Abstract
Background
Computer software for absorbed dose quantification has been used widely in nuclear medicine. Different software tools have been written to improve the dose assessment, especially in therapeutic nuclear medicine. Some software tools focusing on computational phantom models from the international commission of radiation protection and units (ICRP) whilst others on Monte Carlo simulated models. While many studies have investigated therapeutic nuclear medicine dosimetry. The authors have noticed that very few papers compare the therapeutic software tools to each other, hence a doctor of philosophy study was embarked on. The aim of our study was therefore to validate our in-house developed software tool Masterdose using the commercial software OLINDA/EXM 1.0 that was available in our department.
Methods
Methodology was based on clinical patient data treated for neuroendocrine tumours with 177Lutetium (Lu)-DOTATATE at a South African hospital. All patients underwent the same SPECT acquisition protocol and were corrected for scatter, partial volume, collimator-detector response, gamma camera calibration and attenuation. Correction factors were applied to images to convert counts to activity. The first cycle of peptide receptor radionuclide therapy (PRRT) for 11 single photon emission computed tomography (SPECT) patients were compared on the Masterdose and OLINDA/EXM 1.0 software tools at 1, 24, 72 and 168 h. Cumulated activity and the absorbed dose were compared for the two software tools. The absorbed dose difference was then compared using statistical Bland-Altman analysis.
Results
Masterdose and OLINDA/EXM 1.0 had different peptide receptor radionuclide therapy methodologies. This led to different results obtained for the software tools. Cumulated activities of Masterdose and DTK was 10.5% and 10.9% for the kidneys and tumours respectively. On average tumour absorbed doses were nine-times that of the kidneys. Bland–Altman analysis show a non-systematic difference between the two software.
Conclusion
On average the relative percentage difference between the cumulated activities and absorbed dose of the two software were 10.7%.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Radionuclides are used for therapeutic procedures in nuclear medicine, this treatment has been termed radiopharmaceutical therapy, which differs from external beam radiation therapy, since it uses radiolabelled therapeutic pharmaceutical agents [1]. It is therefore important to perform valid quantification of radionuclide dose in organs and tissues. Internal dosimetry is essential to evaluate the risk and benefit of these nuclear medicine procedures. Computer programs are needed to measure the dose to organs and tissues. Nuclear medicine has benefitted from advances in computer software and this gain was at a rapid pace [2]. Dose quantification using personal computer software in nuclear medicine was first developed in the early 1990’s and was distributed to two thousand users worldwide [3]. Electronic dose calculations were formed by the Radiation Dose Assessment Resource (RADAR) group [4]. This data can be downloaded from the internet website www.doseinfo-radar.com. The MIRD committee of the United States Society of Nuclear Medicine developed the MIRD formulism which has gained acceptance in nuclear medicine [5,6,7]:
where:
\(\overline D\;(r_T,T_D)\) is the mean absorbed dose in Gy,
à is the time-integrated activity (TIA) in Bq.s,
rTrepresents the target region,
rs represents the source organ,
and the 'S-value' which is the cumulated activity in the source organ in Gy/Bq.s
The formulism requires knowledge of the cumulated activities, which are numerical values obtained from quantified nuclear medicine images. The ‘S-value’ are Monte Carlo calculation estimates using anthropomorphic phantoms and are radionuclide specific. Fisher-Snyder [8, 9], developed the first anthropomorphic phantom of the human body through a combination of geometric shapes, spheres, cylinders, cones, etc. Cristy et al. [10], then developed a series of phantoms, which represented children and adults of both genders. Stabin et al. [11], developed the female phantom, at three stages of pregnancy and non-pregnant. Other models for organs and structures include the brain [12], eye [13], peritoneal cavity [13], prostate gland [11], bone [12], rectum [14] and tumours [15]. The specific absorbed fractions from the models were “electronically published” by Stabin et al. [16]. This software was written in basic programming language using Visual Basic from Microsoft Corporation, which was later migrated to Windows software [16].
To serve as quality check, a few studies have highlighted the need for development of in-house dosimetry software tools to validate results of commercially available ones [17,18,19,20,21]. An advantage of available dosimetry software packages is that they include image functionality or large databases for S-values. The disadvantage, however, is the exclusion of features for objective calculations of activity to administer, pertaining organ doses and its standard error [19]. Another disadvantage is that most software packages are only commercially available. Whether in-house or commercial, the demand for patient-specific dosimetry necessitates the development of computer software. While many studies have investigated therapeutic dosimetry using in-house or commercial software, comparison of these software is still an open issue. The importance of comparing software tools for accurate absorbed dose calculations are therefore not highlighted in current literature. Authors believe that software comparison studies will assist in predicting possible organ under dosage or over dosage for consequent therapy efficacy or radiation induced toxicity, respectively. Computed absorbed doses can play a role in the amount of activity injected and the actual activity distribution in the organ. The aim of our study was therefore to validate an in-house developed software tool Masterdose using a commercial software tool OLINDA/EXM 1.0 for targeted peptide receptor radionuclide 177Lu-DOTATATE therapy.1
2 Materials and methods
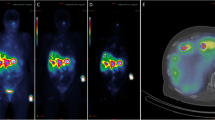
We validated the clinical workflow for Masterdose and OLINDA/EXM 1.0; which included gamma camera acquisition calibration, SPECT acquisition, activity quantification, image volume of interest (VOI) segmentation, time-integrated activity curve (TIAC) fits and absorbed dose calculations as demonstrated in Fig. 1. The challenge in validating Masterdose using OLINDA/EXM 1.0, is that the two software did not address the same dosimetry workflow chain steps, this was similar to what was experienced by Mora-Ramirez et al. [22]. The OLINDA/EXM 1.0 does not propose steps for image quantification. In order to proceed in this study, the Dosimetry Toolkit® (DTK) on the Xeleris® software by GE Healthcare [23] was used to quantify counts and then transferred to OLINDA/EXM 1.0. To reduce uncertainties in each dosimetry workflow step and allow fair comparison, this study only compared the cumulated activity and absorbed dose for the two software tools.
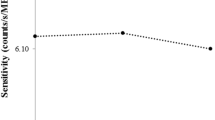
All SPECT quantification were performed using full rotation mode (3600) with 30 s per projection. All acquisitions were performed with a 128 × 128 matrix which had pixel size of 4 × 4 mm2 and the energy discriminatory window was ± 15%. The ordered subsets expectation maximisation (OSEM) algorithm was used for SPECT reconstruction. This algorithm had default settings of eight subsets, four iterations and a Hann filter with a cut-off of 0.85. Gamma camera acquisition calibration, either SPECT or planar, was performed using the same acquisition protocol as the patients. A total of 11 SPECT images in DICOM format with a biopsy proven well-differentiated neuroendocrine tumour (NET) was loaded on each software tool and the kidney with spherical tumour delineated manually or automatically. Most “fine-tuning” of the organs were done manually, the time activity curves created, fitting models applied and the mass dependent S-value time-integrated activity curve (TIAC) calculated. This was done for the first peptide receptor radionuclide 177Lu-DOTATATE patient cycle. All patients were scheduled to receive an activity of 7.4 GBq of peptide receptor 177Lu-DOTATATE in 50 mL of saline for the cycle. All patients were also pre-treated with 1500–2000 mL of lysine amino acid mixture over a period of four hours as well as intravenous injections of 8 mg each of Ondansetron and Corticosteroids prior to administration of peptide receptor 177Lu-DOTATATE therapy. Quantified counts on the kidneys and tumours were compared for the time-points of 1, 24, 72 and 168 h. Peptide receptor radionuclide lutetium-177 therapeutic methods to correct for scatter, partial volume, collimator-detector response, attenuation and correction factor (CF) as discussed in the literature, were applied to all DICOM images [20, 21].
The relative percentage difference (RPD), as demonstrated in Eq. (2), was then used to determine differences in the cumulated activity:
where; QMasterdose = cumulated activity on Masterdose, QDTK = cumulated activity on DTK
Bland–Altman analysis was also used to compare the absorbed dose difference between Masterdose and OLINDA/EXM 1.0. This was done by plotting the difference between the two software on the Y-axis and the mean on the X-axis. The bias (b) was calculated as the mean of the difference between Masterdose and OLINDA/EXM 1.0, with the lower and upper limits of agreement were calculated using Eqs. (3) and (4).
where, LL and UL = lower limit and upper limit of agreement respectively, SD = standart deviation.
The S-values and organ masses from OLINDA/EXM 1.0 were incorporated into Masterdose, hence no comparative analysis performed and is demonstrated in the Appendix Tables 4, 5, 6 and 7.
3 Results
The 177Lu-DOTATATE patient data used in this study is given in Table 1.
The patient population presented in this study had advanced disease. These patients had prior surgeries, chemotherapy and biological therapies with further treatment options being limited. The Eastern Cooperative Oncology Group (ECOG) [24] performance status mean was 0. Demonstrating that all patients were fully active and able to carry all pre-disease performance without restriction.
The organ masses after manual delineation on CT for the kidneys are demonstrated in Table 2. Men organ mass was larger than that of women, as reported by similar studies [25, 26]. Kidney masses have been shown to vary up to a factor of three between patients.
Table 3 gives the dosimetry analysis of computational software tools. Of note is the varying TIAC fitting used by the different software.
Computer software tools are needed due to the difficult nature in measuring absorbed dose to organs and tissues [27]. Both software tools were able to create a TIAC.
The cumulated activities from Masterdose and OLINDA/EXM1.0 are demonstrated in Fig. 2a and b.
The largest cumulated activities were found in tumours compared to the kidneys for both software. The tumour uptake was on average nine-times that of the kidneys for both software. The VOIs delineation, quantification steps and fitting parameters have a direct impact on the results displayed in Fig. 2. On average the RPD between the cumulated activities of Masterdose and DTK was 10.5% and 10.9% for the kidneys and tumours respectively.
The absorbed doses for Masterdose and OLINDA/EXM 1.0 are demonstrated in Fig. 3a and b.
On average the RPD between the absorbed doses of Masterdose and OLINDA/EXM 1.0 was 10.5% and 10.9% for the kidneys and tumours respectively. Following the similar trend by the cumulated activities.
The Bland–Altman analysis for the kidney and tumour absorbed doses are demonstrated in Figs. 4 and 5.
For the kidneys, a particular trend is seen that the calculated absorbed doses were almost consistently higher that the bias or systematic error of 0.2 Gy. However, the tumour Bland–Altman analysis show a non-systematic difference, as calculated absorbed doses were distributed evenly around the bias of 1.9 Gy. None of the cases quantified received a kidney absorbed dose of 23.0 Gy, which is considered the external radiotherapy limit [28].
4 Discussion
There was a lack of standardized peptide receptor radionuclide therapy methodology between the Masterdose and OLINDA/EXM 1.0 software tools. According to GE recommendations, planar acquisition should be performed to obtain the CF [23]. Therefore Masterdose used a SPECT CF and OLINDA/EXM a planar CF. The relative percentage difference in the accumulated activity could be attributed to the different CFs used. Using a planar CF for SPECT cases, even though recommended by the vendor, is not ideal, the in-air CF for DTK did not adequately approximate patient scatter and attenuation conditions. The Masterdose SPECT calibration factor correctly accounted for scatter and attenuation corrections since the volumetric phantom “mimicked” the patient. Similar studies deemed an overall percentage difference of less than 10% between software dose as acceptable [25, 26]. Comparison of software in this study was just outside this limit, however, one should consider use of CFs as discussed extensively earlier as a large contribution to this error. Although not explicitly studied in this research, the authors could have used a SPECT generated CF for the DTK software, going against vendor recommendations, as performed by Mora-Ramirez et al. [22]. This would have produced an RDP of 3.2% between Masterdose and OLINDA/EXM 1.0, which would be well within the 10%.
The largest cumulated activities were found in tumours compared to the kidneys for both software. The tumour uptake was on average nine-times that of the kidneys for both software, demonstrating the therapeutic clinical environment. Clinicians could therefore have escalated absorbed doses to the tumours whilst sparing the kidneys. The VOIs delineation, quantification steps and fitting parameters have a direct impact on the results displayed in Fig. 2. Although not explicitly investigated in this comparison of software, studies have shown that trapezoid methods will be influenced by random and systematic errors [29]. The selection of four data time points in our study assisted in reducing these types of errors, as trapezoidal curve fitting improves with more data points. Mora-Ramirez et al. [22] made the observation that it is difficult to compare time-activity curve fitting performances of software at this stage, due to non-identical activity maps. This prevented authors from implementing the same approach for the software compared and is a development which needs to be addressed in the near future. Therefore, this study did not compare the fitting performance of the trapezoidal and mono-exponential function, which could have added to the RPD of software comparison.
It should be noted that only self-absorbed doses were reported in this study. Self-absorbed dose is the dominant contributor for 177Lu according to the ICRP [30]. The electron emission dominates the self-absorbed dose of 177Lu, due to its short range in soft tissue and bone. Absorbed doses were spread throughout the Bland–Altman plot, with only three kidney and one tumour calculated absorbed doses within correlation of agreement. All absorbed doses were within the limits of agreement of 0.5 Gy and 3.9 Gy for the kidneys and tumours respectively.
5 Conclusion
The Masterdose and OLINDA/EXM 1.0 software tools compared have different therapeutic approaches. This led to variations in the radiopharmaceutical therapeutic approach and affected the clinical evidence derived from this paper. Our paper has estimated uncertainties during the CF, and activity quantification of Masterdose and OLINDA/EXM 1.0.
Data availability
The authors make this data available to the journal.
Code availability
This study was part of a PhD, the code can only be made available after 5 years.
References
Wahl RL, Ahuja S, Clarke B. Current Landscape of Radiopharmaceutical Therapies: SNMMI Therapy Task Force Survey. J Nucl Med. 2021;62(5):11N-16N.
Mattsson S, Johansson L, Leide Svegborn S, et al., ICRP. Radiation dose to patients from radiopharmaceuticals. A compendium of current information related to frequently used substances. ICRP publication 128. Ann. ICRP 2015:44(2S).
Stabin MG. MIRDOSE: personal computer software for internal dose assessment in nuclear medicine. J Nucl Med. 1996;37:538–46.
Stabin M, Wendt RE, Flux GD. RADAR Guide: Standard Methods for Calculating Radiation Doses for Radiopharmaceuticals, Part 2-Data Analysis and Dosimetry. J Nucl Med. 2022;63(3):485–92.
Bolch WE, Eckerman KF, Sgouros G, Thomas SR. MIRD pamphlet No. 21: a generalized schema for radiopharmaceutical dosimetry-standardization of nomenclature. J Nucl Medicine. 2009;50(3):477–84.
Quantitative nuclear medicine imaging: concepts, requirements and methods. Vienna: International Atomic Energy Agency, 2014. IAEA human health series, ISSN 2074–7667; no. 9.
Lassmann M, Chiesa C, Flux G, Bardiès M. EANM Dosimetry Committee guidance document: good practice of clinical dosimetry reporting. Eur J Nucl Med Mol Imaging. 2010. https://doi.org/10.1007/s00259-010-1549-3.
Snyder W, Ford M, Warner G, Fisher H Jr: MIRD Pamphlet no 5—estimates of absorbed fractions for monoenergetic photon sources uniformly distributed in various organs of a heterogeneous phantom J. Nucl. Med. 1969 (Suppl 3) 5.
Dunford CL, Burrows TW. Online nuclear data service. Upton, NY: Brookhaven National Laboratory. 1999:NNDC/ONL 99/3,IAEA NDS-150,Rev 99/3.
Cristy M, Eckerman K. Specific absorbed fractions of energy at various ages from internal photons sources ORNL/TM-8381 V1-V7 (Oak Ridge, TN: Oak Ridge National Laboratory), 1987. https://www.osti.gov/servlets/purl/6233638.
Stabin M. A model of the prostate gland for use in internal dosimetry. J Nucl Med. 1994;35:516–20.
Eckerman K, Stabin M. Electron absorbed fractions and dose conversion factors for marrow and bone by skeletal regions. Health Phys. 2000;78:199–214.
Holman B, Zimmerman R, Shapiro J, Kaplan M, Jones A, Hill T. Biodistribution and dosimetry of n-isoproyl p-123I iodoamphetamine in the primate. J Nucl Med. 1983;24:922–31.
Mardirossian G, Tagesson M, Blanco P, Bouchet LG, Stabin M, Yoriyaz H, Baza S, Ljungberg M, Strand S, Brill A. A new rectal model for dosimetry applications. J Nucl Med. 1999;40:1524–31.
Stabin M, Konijnenberg M. Re–evaluation of absorbed fractions for photons and electrons in small spheres. J Nucl Med. 2000;41:149–60.
Stabin MG, da Luz CQPL. New decay data for internal and external dose assessment. Health Phys. 2002;83:471–5.
Mirzaei S, Sohlberg A, Knoll P, et al. Easy-to-use online software package for internal dose assessment after radionuclide treatment in clinical routine. Clin Nucl Med. 2013;38(9):686–90.
Visser E, Postema E, Boerman O, et al. Software package for integrated data processing for internal dose assessment in nuclear medicine (SPRIND). Eur J Nucl Med Mol Imaging. 2007;34:413–21.
Marie-Paule G, Daphnée V, Erin M, et al. TestDose: A nuclear medicine software based on Monte Carlo modeling for generating gamma camera acquisitions and dosimetry. Med Phys. 2015;42:6885–94.
Van Wyk B, Hasford F, Nyakale N, Vangu M. An image-based notion for therapeutic planar organ activity dosimetry in a developing country: Masterdose software. Hell J Nucl Med. 2022;25(1):71–82.
Stabin MG, Sparks RB, Crowe E. OLINDA/EXM: The Second-Generation Personal Computer Software for Internal Dose Assessment in Nuclear Medicine. J Nucl Med. 2005;46:1023–7.
Mora-Ramirez E, Santoro L, Cassol E, Ocampo-Ramos JC, Clayton N, Kayal G, et al. Comparison of commercial dosimetric software platforms in patients treated with 177Lu-DOTATATE for peptide receptor radionuclide therapy. Med Phys. 2020;47(9):4602–15.
GE Healthcare. Organ dose estimates for radio-isotope therapy treatment planning purposes. Dosimetry toolkit package. White paper. 2011.
Zubrod C, et al. Appraisal of methods for the study of chemotherapy in man: Comparative therapeutic trial of nitrogen mustard and thiophosphoramide. J Chronic Dis. 1960;11:7–33.
Grimes J. Patient-specific internal dose calculation techniques for clinical use in targeted radionuclide therapy. University of British Columbia; 2013. https://open.library.ubc.ca/soa/cIRcle/collections/ubctheses/24/items/1.0073590.
Mora-Ramirez E, Santoro L, Trauchessec D, Chouaf S. Dosimetric estimations using commercial workstations for peptide receptor radionuclide therapy (PRRT) patients treated with 177Lu-DOTATATE. Eur J Nucl Med Mol Imaging. 2017;44S810.
Simulation, analysis, and modeling software. https://tegvirginia.com/software/saam-ii/. Accessed 19/03/2021.
International Commission on Radiation Units and Measurements. Report 44: Tissue Substitutes in Radiation Dosimetry and Measurement. Bethesda, MD: ICRU; 1989.
Sjogreen Gleisner K, Chouin N, Gabina P, Cicone F, Gnesin S, Stokke C, Konijnenberg M, Cremonesi M, Verburg F, Bernhardt P, Eberlein U, Gear J. EANM dosimetry committee recommendations for dosimetry of 177Lu-labelled somatostatin-receptor-and PSMA-targeting ligands. Eur J Nucl Med Mol Imaging. 2002;49:1778–809.
Eckerman E, Endo A. ICRP Publication 107: Nuclear decay data for dosimetric calculations. Ann ICRP. 2008;38(3).
Acknowledgements
The authors would like to express their sincere gratitude to the nuclear medicine departments at Witwatersrand University-Donald Gordon Medical Centre and Inkosi Albert Luthuli Central Hospital. Special thanks go to Monageng Motsabi for assisting with and “fine-tuning” the Masterdose software, and from whom the name of the software probably comes from, due to us calling each other “Master”.
Funding
Open access funding provided by Sefako Makgatho Health Sciences University. Sincere gratitude to the research department at Sefako Makgatho University for making funding available for the research.
Author information
Authors and Affiliations
Contributions
Bronwin Van Wyk performed the software validation; Francis Hasford, Nozipho Nyakale and Mboyo-Di-Tamba Vangu interpreted and supervised the manuscript findings. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Sefako Makgatho Health Sciences University Research Ethics Committee approved this study, SMUREC Ethics Reference Number: SMUREC//M/114/2018: PG.
Consent to participate
Not applicable.
Consent for publication
All authors consent to the publication.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Van Wyk, B., Hasford, F., Nyakale, N. et al. Validation of an in-house developed therapeutic dosimetric software tool for the treatment of 177Lutetium-DOTATATE peptide receptor radionuclide therapy. Health Technol. 14, 277–289 (2024). https://doi.org/10.1007/s12553-024-00818-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12553-024-00818-x