Abstract
Inventory is a fundamental process throughout the life cycle of medical devices. The maintenance program for each piece of equipment must comply with current regulations that are constantly evolving. The need to set up an evidence based management of the inventory of thousands of medical devices hosted in the Careggi University Hospital (AOUC), in Florence (Italy), has suggested to conceive a method to group medical devices in sub-classes, in order to monitor their performances and maintenance. The starting point to reach this goal is to establish a suitable nomenclature, a complex system of rules, codes, and definitions employed by healthcare systems and organizations to identify sets of medical devices. This paper describes the literature search performed on both Ovid and Scopus databases, that made it possible to identify several classifications and nomenclatures for medical devices. On the basis of this search, only a few works fulfil the requirement of classifying medical devices for management purposes (e.g., inventories, database, and supply chains). The analysis has shown that it is possible to reduce the number of classes into macro groups when applying the Italian National Classification of Medical Devices (CND). Although the CND nomenclature shows inconsistencies for complex groups it is an effective and successful choice, in terms of efficiency and optimization, also considering that it is the basis for the European Medical Device Nomenclature (EMDN).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
A medical device nomenclature is a complex system of rules, codes, and definitions employed by healthcare systems or organizations to identify sets of medical devices (MD). These naming systems meet various requirements that span from maintenance, procurement, and accounting to stock keeping, regulatory affairs, adverse events reporting, etc. [1]. The need for a global nomenclature for MDs is of great relevance and is involving the most important international players, starting from the World Health Organisation (WHO). In 2019, in the occasion of the 145th WHO Executive Board, the Director-General underlined the need for a standardized nomenclature of MDs “as a common language for recording and reporting medical devices across the whole health system at all levels of health care for a whole range of uses. [...] The lack of a nomenclature system has hampered the development of the evidence- and web-based health technologies database to provide guidance on appropriate medical devices” [2]. Some of the most important nomenclatures and identifiers currently used are: the National Classification of Medical Devices (CND), the European Medical Device Nomenclature (EMDN), the Global Medical Device Nomenclature (GMDN), the Universal Medical Device Nomenclature System (UMDNS), and the Unique Device Identifier (UDI). These systems are briefly illustrated in Sect. 2.1. Very recently, in January 2021, at the 148th WHO Executive Board, it was reported that, after an analysis of existing nomenclature systems, “the WHO analysis concluded that, of the analyzed nomenclatures, the one that complies with the WHO principles for international classification, coding and nomenclature of medical devices mentioned above, is the CND (Italian National Classification, ed). Subject to the Board’s consideration, the Secretariat is of the view that the other three nomenclature systems, including GMDN, which was mentioned as a possible option by some Member States during the discussions at the Executive Board in May 2019), would not be consistent with the WHO principles” [3]. Adriana Velazquez Berumen, group lead of medical devices and in vitro diagnostics at WHO, in the occasion of an online presentation to Low- and Middle-Income Countries (LMICs) on April 29, 2021, underlined how a global nomenclature should include the following characteristics: publicly available; free access; continuous update; expandable as the new technologies develop; flexible structure; based on a tree system; considering all aspects of classification [4]. These aspects are more and more important on a global level, in consideration that regulatory frameworks designed for high-income settings might be very inadequate to LMIC settings [5]. WHO stated the following requirements for a global nomenclature system:
-
(i)
a transparent methodology and processes;
-
(ii)
a transparent mechanism for regular updates (e.g. once per year);
-
(iii)
hierarchies grouped into categories and subcategories to meet stakeholder needs;
-
(iv)
medical devices used outside highly regulated countries;
-
(v)
mutually exclusive terms;
-
(vi)
availability of terms in other languages” [3].
They also cared about the access to information, stating that it should:
-
(i)
be freely available and considered a global public good;
-
(ii)
support unique device identifier system;
-
(iii)
be accessible through simple and intuitive search;
-
(iv)
be available for use in all health-related data base systems.
The aim of this scoping review is to conceive a method to group MDs in sub-classes in order to simplify their maintenance monitoring. The idea of grouping MDs in sub-classes stems from the need to manage about 18,000 MDs of the Careggi University Hospital (AOUC), in Florence (Italy) [6,7,8].
In the late 1990s the coding system, developed by the “Centro di Informazione e Valutazione delle Apparecchiature Biomediche” (CIVAB) in Trieste (Italy) and called CIVAB code, was used for procurement and management of biomedical technologies. It represented a unique classification system for most of the MDs in Italy, but it was replaced by CND starting 2005. Nevertheless, CIVAB is still used by many companies and by the “Ente di Supporto Tecnico Amministrativo Regionale” (ESTAR) [9], to categorize MDs. ESTAR, established for technical, administrative, assessment and support functions for Tuscany’s hospitals (Italy) in October 1st, 2014, is in charge of the clinical engineering service for AOUC. 18,000 AOUC medical devices are today falling into 609 different CIVAB classes. Because their maintenance is too hard to manage and monitor, a new methodology system is required in order to provide the decision makers with evidence from data [10].
Maintenance is a fundamental process throughout the life cycle of MDs and includes both corrective and scheduled maintenance. For each piece of equipment, the maintenance program must comply with current regulations that are constantly evolving. The maintenance planning requires the assessment of a number of parameters, including mode and frequency of use of a medical equipment, its intended use and the associated risks. The maintenance is also a crucial part of the activities of a hospital clinical engineering department (CED), involving significant human and financial resources. The UNI EN 15341:2019 standard [11] comes in support by describing a system for managing maintenance Key Performance Indicators (KPIs), with the aim of measuring the maintenance performance, how it is influenced by key maintenance factors and how to assess and improve efficiency and effectiveness. MDs maintenance must secure the equipment availability and reliability, that is linked to the safety of the device.
In a recent study by Iadanza et al. [10], a new set of technological, organizational, and financial KPIs is proposed in order to achieve an evidence based medical equipment maintenance process. The article is grounded on the Evidence-Based Maintenance (EBM) approach [12,13,14,15], defined as “a continual improvement process that analyses the effectiveness of maintenance resources deployed in comparison to outcomes achieved previously or elsewhere and makes necessary adjustments to maintenance planning and implementation” as reported by Wang B. [16]. The study focused on devices used for intensive care and surgery, including vascular interventions. The final purpose of our research is to further extend this approach by applying the above-mentioned set of KPIs to the whole set of electromedical devices. One of the first problems to solve is reducing the high number of classes from the above-mentioned figure of 609 to a more reasonable and manageable number. Since it is extremely important to use objective and effective grouping criteria, we found it appropriate performing a scoping review in order to set the baseline for our research. The Methods section of this scoping review presents the state-of-the-art nomenclatures aimed to manage MDs, retrieved thanks to a literature performed on two different databases. The Results section illustrates information collected from databases (updated to July 06, 2020) that respected inclusion criteria and whose was aimed to discover MD grouping methods. The Discussion section is divided into two main subsections. The first further analyses the obtained results, focusing on the strengths of the articles that were considered relevant for our work. The second subsection analyzes the conversion from CIVAB to CND nomenclature system on MD systems identified by ESTAR and reported within its own guide.
2 Methods
A literature search on available databases made it possible to identify several classifications and nomenclatures for MDs. At the beginning of this section the most important nomenclatures currently used worldwide are described. Subsequently, the motivations for performing our search in two databases (firstly on Ovid and afterwards on Scopus) are reported.
2.1 Nomenclatures for identification of MDs
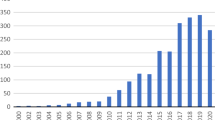
Different nomenclatures are employed by healthcare systems or organizations to identify sets of medical devices. Some important international organizations, such as the WHO [1, 3], the International Federation for Medical and Biological Engineering (IFMBE) [17] and the European Alliance for Medical and Biological Engineering and Science (EAMBES) [18], have recently set up working groups to study the current situation and to contribute to a global standardization. As shown in Fig. 1, many countries adopt nationally developed systems, some countries make use of GMDN and UMDNS, whole many countries in Eastern Europe, Latin America, Africa and Asia are still a proper nomenclature system. As stated in the introduction, each of the existing nomenclature systems have limitations, therefore none of them seems adequately universal, yet. The roadmap to a standardized international classification coding and nomenclature of MDs, should include the opening of closed systems together with the interoperability between different systems, leveraging standard protocols and techniques.
Type of nomenclatures by countries [WHO https://tinyurl.com/ycz72tnt]
In the following some of the main systems are described and briefly discussed.
CND is the Italian classification, also used in Portugal and Greece, which groups MDs into homogeneous categories of products, that are intended to carry out similar therapeutic or diagnostic interventions. Following the criterion of product differentiation based on their intended use and/or on 22 anatomical-functional locations (eight anatomical types, nine functional types, and five special categories), the classification has an alphanumeric structure accomplishing two primary duties: the first is to develop a multi-level hierarchical tree, the second is to aggregate MDs into categories, groups and types [19]. The nomenclature greatly facilitates the data management for MD groups.
GMDN was developed based on the international standard ISO 15225 “Medical devices – Quality management – Medical device nomenclature data structure”[20], by the European Committee for Standardization (CEN) and by MD experts from all over the world (manufacturers, healthcare authorities and regulators). It consists of a poly-hierarchical system in which the product identification consists of: a unique numerical five-digit index GMDN Code that is associated to a GMDN Term Name, indicating the MD name; a GMDN Definition including the intended use(s) and the device category (based on device application, technology, or other common characteristics). The identification of specific MDs that have similar generic features is possible through cross-referencing [21]. The GMDN is made up of 20 main categories and contains primary terms and synonyms for MDs. It is a list of generic terms used to identify all MDs. Such products include those used for the purposes of diagnosis, prevention, monitoring, treatment or alleviation of disease or harm to humans.
UMDNS was developed in the US by the Emergency Care Research Institute (ECRI) as an interrelated vocabulary, which makes use of terms naming the different MDs. It is a polyhierarchical system where the difference between the levels is a single term. The UMDNS nomenclature is made up by two elements: preferred terms and entry terms. Each preferred term has a definition that describes the applications of the MD, its materials and technologies. A five-digit code is assigned (Universal Medical Device Code - UMDC), using a consecutive-numbering system without an intrinsic meaning. Entry terms, on the other hand, represent lexical variants, apparent synonyms, or acronyms of the preferred terms. Maintenance is performed by a core group of ECRI nomenclature specialists, both for internal use and for support to the external clients and licensees [21].
The CIVAB coding system represents a unique recognition system of the largest part of biomedical technologies on the domestic market. The code consists of eight alpha-numeric digits. Three identify the technology class, other three digits are reserved for the manufacturing company, while the last two indicate the specific model. CIVAB has not been updated since 2010.
The UDI system is a unique numeric or alphanumeric code used to identify and track MDs through the healthcare supply chain. It consists of two parts [22]. The first mandatory one is called Device Identifier (UDI-DI): it is the fixed portion of the UDI and identifies the specific version or model of the device. The last (optional) is called Production Identifier (UDI-PI): it is the variable portion of the UDI, and identifies the lot or batch number, within which each device was manufactured, the specific date in which each device was manufactured, the expiration date of each device, the serial number of each device, etc.
The WHO noted that countries that make use of an official nomenclature, have been using the following types of systems: 26% national system (e.g. CND in Italy), 12% UMDNS, 10% GMDN, and 3% more than one system [21]. Several countries have their own country-based nomenclature system, but the two most widely used nomenclature systems for MDs are the GMDN and the UMDNS [21]. According to Article 26 of Regulation 745/2017 on MDs and to Article 23 of Regulation 746/2017 on in-vitro diagnostic medical devices (IVD) [23], the European Commission Medical Device Coordination Group (MDCG) decided to use the CND as nomenclature for the European EUDAMED database (used by manufacturers to register their MDs), because of its features in terms of structure, purpose, usability and updating methodology. The EMDN is going to be the official nomenclature in the European Union (EU) [24].
2.2 Databases and literature search
2.2.1 Ovid technologies
Ovid Technologies is a provider of bibliographic and full-text database in medical and academic fields. It is interface to MEDLINE, the world’s largest and oldest medical database, produced by the US National Library of Medicine, and it provides the user with a convenient and powerful set of tools for performing literature searches.
Literature search methods and selection criteria
At first we performed a search to identify relevant scientific literature on the following bibliographic databases: the Ovid MEDLINE database (1946–June 06th, 2020) and the Journals@Ovid Full Text database (June 06th, 2020). The search was completed on June 06th, 2020. The main search concepts were nomenclature, classification and medical equipment management. The search strategy comprised keywords such as MD/s, medical equipment, inventory, taxonomy, classification/s, nomenclature, health technology assessment, health technology management, management, clinical engineering, and more. Conference abstracts and proceeding papers were excluded from the search results. The results were obtained by limiting the search to a span of twenty years, from 2000 to 2020, and just to papers in English. We considered only publications describing nomenclature, MDs classification management, or both. Publications describing only pharmaceutical nomenclature methods or other techniques were not considered. Furthermore, the articles focusing on IVD were excluded.
2.2.2 Elsevier scopus
After the search on the Ovid database, given the relatively small number of management-related papers reached, we opted for a second search on the Scopus database from Elsevier, which indexes a wider range of biomedical engineering and management journals, if compared to Ovid which is focused on medical journals. We then merged the search results from both databases. Three more articles, [25,26,27], known to the authors but not captured by the search, were manually added.
Literature search methods and selection criteria
Search was completed on June 06th, 2020. The main search topics included: nomenclature, classification and medical equipment management.
The search strategy was comprised of keywords such as:MD/s, medical equipment, inventory, UDI, GMDN, CND, UMDNS, classification/s, health technology assessment, health technology management, and clinical engineering. The search was limited to the period of time from 2000 to 2020, English or Italian languages, and to the following types of documents: article, review, book chapter, and book. The included subject areas were: medicine, engineering, computer science, business management and accounting, psychology, decision sciences, environmental science, agricultural and biological sciences, and mathematics. We adopted the same selection criteria described for Ovid search. In fact, we considered the publications that describe nomenclature and classification management of MDs, following the EU Regulation 2017/745 [28].
2.2.3 Grey literature
Together with the bibliographic research, one more document were included: a technical-inventory guideline developed by ESTAR.
2.3 Screening procedure for inclusion, and information collection
According to the scoping review protocol by Tricco et al. [29], two reviewers (S.C. and C.L.) independently screened titles and abstracts, reviewed the full texts using the same selection criteria and compared their lists of included and excluded studies. These reviewers collected data information and conducted a descriptive analysis of the methods used to classify MDs. The data extracted were reviewed, categorized, and organized to synthesize different methodologies. Extracted information includes the study characteristics (e.g., first author name, publication year, and reference number), and title. Additional extracted information is the type of nomenclature and the conceptual framework used to classify health technologies. All information were arranged in a table: each row is assigned to a document; the different columns report the main characteristics of each document, its aims and a brief analysis of the content. Results were then compared and interpreted to identify and find strategies or patterns for managing the medical equipment or techniques, described in the included studies. A third reviewer (E.I.) intervened in case of disagreement and verified all decisions made by the other reviewers, in order to ensure data accuracy.
3 Results
The process of selection applied to the products obtained by the literature search is described in Fig. 2. The main characteristics and key considerations about each analysed document are reported in Table 1, whose columns are organised as follows: first author and year of publication; title of the paper; source database; aims; analysis of results; treated nomenclatures. All the articles are ordered by publication date and range from 2013 to 2019. A total of 15 articles and one technical documents were included for review. The query strings used in the selection process are included in the supplementary materials. In the following subsections, the results are grouped by source.
3.1 Ovid
A total of 1,989 articles have been identified in the Ovid literature search. Following the screening of titles and abstracts, 1,937 articles were excluded, and 52 potentially relevant reports were retrieved for full-text review. Among these potentially relevant articles, 46 publications were excluded due to non-compliance with the inclusion criteria. Six publications met the inclusion criteria and were included in the review. See left branch in Fig. 2.
3.1.1 Aims
We found five articles dealing with UDI nomenclature framework [30,31,32,33,34], and one with GMDN [35].
In Sherwin’s work [34], the authors examine some of the key problems in managing MD inventory tracking.
Ibey et al. [33] describe the procedures used by a clinical engineering team in order to put in place a management system for MDs.
In the work from Henschke et al. [35], the aim is to develop a taxonomy model that provides researchers and policy makers with an orientation tool to approach the assessment of different use and regulations of MDs.
Drozda et al. [32] report the Food and Drug Administration (FDA) strategy defined for the MDs post-market surveillance, in 2012. This strategy is divided in four parts, where the first concerns the UDI use to register MDs. FDA and Medical Device Epidemiology Network carried out a pilot project in order to incorporate UDI into electronic information systems of cardiac catheterizing laboratories.
In a recent paper [30], it is proposed a possible approach for the implementation of UDI and traceability in Europe for a standalone MD software, in order to trace the system’s lifecycle and improve its overall quality.
In Camus’ work [31], UDI system and EUDAMED databank are described in depth: all the steps to push the French ecosystem towards the new European MD regulation are explained.
3.2 Scopus
Following the research on Ovid, a new literature search has been performed on Scopus. A total of 2,613 articles have been identified. Following the screening of titles and abstracts, 2,541 were excluded, and 72 potentially relevant articles were retrieved for full-text review. Among them, 66 publications did not match the inclusion criteria and were excluded (see central branch in Fig. 2). Three relevant articles were manually retrieved (via Scopus and PUBMED) and are treated as “SCOPUS” for simplicity: [25,26,27]. Nine publications met the inclusion criteria and were included in this scoping review. The description of the objectives is reported below.
3.2.1 Aims
Four different standard nomenclatures are treated in the selected works: four articles deal with GMDN [26, 36,37,38], four with UDI [36, 39,40,41], three refer to UMDNS [25, 27, 37, 38].
The aim of Bliznakov’s work [37] is to develop a global information system, which includes software modules, in order to manage every aspect of MDs.
The article from Mobarek [27] analyses the different phases of the design, the implementation and the evaluation of a Fully Automated CE Technical Management System, for the Ministry Of Health (MOH) in Jordan.
Bliznakov et al. [25] describe an equipment inventory development of the MDs used in the Peripheral Healthcare System (PHS) of Crete. Their process has led to creation of an electronic database.
A work by Hefflin et al. [38] presents the MD nomenclature perspective. The authors take into consideration the UMDNS and GMDN.
Anand et al. [36] report a detailed GMDN description and its integration within the UDI system.
The article by White et al. [26] describes in depth the structure and integration of GMDN by the use of Systemized Nomenclature of Medicines, Clinical Terms (SNOMED-CT).
A paper by Brown et al. [40] describes the UDI system and its implementation steps.
In the recent paper by Jiang et al. [41], the authors use The Observational Health Data Sciences and Informatics (OHDSI) vocabulary in order to prototype the UDI vocabulary for the use inside Global Unique Device Identification Database (GUDID) with the purpose of naming MDs.
In a recent work by Aronson et al. [39], the authors analyse the definition of the MDs, the MDs classification, and the MDs regulation through risk classification for into the EU and United States (US) framework.
3.3 Grey literature
ESTAR guideline
The ESTAR technical guideline was built as a tree-system where the main device is the trunk tree (called father) and the linked equipment is the branch tree (called child). Father and son are both inventoried assets. Moreover, all illegitimate children are non-electromedical devices and are inventoried for economic aims and linked to their own father. All MDs were inventoried following CIVAB coding. Electromedical devices (including non-electromedical devices necessary for the main asset) equipped with autonomous power supply (even powered by isolating transformer) are inventoried. Accessories or components powered by the main device but moved by other equipment, have to be inventoried according to the tree-system. Some specific pieces of equipment disconnected from his father must be inventoried as well.
4 Discussion
4.1 Analysis of results
Our research has shown that only a few documents satisfy the need to classify MDs for management purposes. Taking into account the objectives of this paper, some of these articles offer discussion points that we will analyze below. A synthesis is reported in the fifth column of Table 1: “Analysis of results”.
Bliznakov et al. [37] develop a system which aims to manage biomedical technology in support of the CED, made by three software modules: PRAXIS, The Vigilance Information Exchange Module (VIEM), and The Quality Control Protocols Module (QCPM). PRAXIS is composed by sub-modules, in which one is the inventory. The system supports codes and classification of device groups, according to the UMDNS nomenclature system. Alternatively, the system can also support the GMDN nomenclature system. The VIEM module consists of three levels:
-
In the Top Level, devices are grouped into 12 categories divided on the basis of knowledge sets or professional disciplines;
-
The Middle Level is the nomenclature level and its groups MDs by similar intended use;
-
In the Lowest Level, the make and model devices are specified.
In the fully-automated clinical engineering management system [27], a type of CMMS, each element of the management plan is associated to a unique code. In particular, two different codes are assigned to each MD: the inventory number and the class number. Devices are classified inside the inventory, according to the UMDNS. The whole inventory control system is identified thanks to a unique barcode system (GS1). The device inventory number consists of basic equipment information, equipment class number, location, and manufacturer.
Bliznakov et al. describe an MD inventorying procedure applied in Crete (Greece) [25]. Inventories applied in local hospitals were uneven due to lack of information on codification and standard nomenclature, of computer systems and software and most of times deficiency in staff experience. In order to supervise the management system, the authors describe data collection software guidelines and divide the inventory into five categories: device groups, device types, manufacturers, suppliers, and departments [37]. Where possible, MDs have been classified according to the UMDNS code. This document is a conference paper that contains updates to a previous work [37].
In the paper by Hefflin et al. [38] different aspects of MD nomenclature features are analyzed. The UMDNS and GMDN codes are examined.
In Anand’s work [36], an attempt to understand the GMDN logic is made, in order to regulate MD worldwide and find a method to reduce the error registrations. In addition to the GMDN system aspects, authors explain the GMDN and CEN relationship development process, benefits and structural considerations. The integration of the GMDN and UDI systems is discussed as well.
The aim of Shenwin’s work [34] is to track and define an inventory for constantly monitoring mobile MDs. They present a Real Time Location System (RTLS) technology which uses Radio Frequency Identification (RFID). The RTLS system allows a high level of service. For the implementation of this system, they divide the equipment that has to be tracked into three overlapping categories: Highly mobile devices, Most-wanted devices and High-cost devices. Authors use UDI in order to keep track of the equipment and have a universal mobile device registry.
In Brown’s work [40], authors provide a background of the UDI code system, and the FDA perspective about its implementation. In addition, they addresse the hospital benefits of using UDI, which incorporates a new labeling process and data entry requirements.
Henschke’s aim is to develop a taxonomic model in which devices are evaluated according to their risk class in a logic of HTA [35]. The model structure is a \(9\times6\) matrix; to develop the model the authors used:
-
the current EU regulatory framework for MDs, consisting of three directives (93/42/EEC [42], 90/385/EEC [43], 98/79/EC [44]);
-
the international classification for medical devices, used by the GMDN;
-
the OECD Classification of Health Care Functions, that is the International Classification for Health Accounts (ICHA) code for Functions of HealthCare (HC), which considers reimbursement aspects;
-
the work by Perleth’s [45];
-
color-coding.
In the work carried out by Ibey et al. [33], the computerized maintenance management system (CMMS) team develops a guideline which addresses the assets into CMMS, following a new decision-making criterion. The authors label the MDs using the UDI nomenclature as stated by the FDA. All the new assets, entered into the CMMS, adhere to a strict UDI naming convention.
In the work by Drozda et al. [32], the UDI implementation has affected lots of operational processes in several functional areas, such as: supply, labor, revenue, inventory management, and system design. The UDI data, electronically captured via bar-code, using the Global Trade Identification Number (GTIN) GS1, has been combined into a rich dataset, which also includes device attributes and patients’ data electronically recorded. Prototypes of UDI coronary stents were created, which can be linked to device attributes contained in the FDA Global UDI Database and to additional key clinical attributes contained in the Mercy Supplemental UDI Database.
Bianchini et al. [30] go through the UDI regulatory framework of US to apply UDI code to EUDAMED databank. The aim is to solve and identify the main problems related to the production of standalone Software as a MD (SaMD). The authors identified several critical points during the European UDI system implementation: labeling, assignment criteria, privacy and compliance with international standards.
Camus et al. in [31] analyze the UDI nomenclature, the GMDN code, and the EUDAMED databank. They provide some insights and recommendations aimed to apply new MD European regulation to the French system.
White et al. analyze the United Kingdom (UK) MD nomenclature status in 2013 [26]. The authors describe the GMDN and SNOMED-CT structure and the integration of GMDN with SNOMED.
In their paper [41], Jiang et al. propose a framework for building a UDI research database for MD evaluation, using the OHDSI common data model (CDM) [46]. The framework comprises three modules: UDI Vocabulary, ETL (Extract, Transform, and Load) for the UDI-Enabled Device Data, and Analytic methods for MD evaluation. They collected the Class III device dataset from the GUDID website.
Aronson et al. [39] examine the current regulatory processes of the US and EU, such as the MD classification. In the US, the FDA provides a Product Code (PC) to the MD: it is made up of 18 fields i.e. 18 characteristics, in order to label, track and classify the device. Furthermore, the MDs are organized into 19 medical specialties panels, and their descriptions are available on the Code of Federal Regulations (CFR) Title 21, parts 862 to 892. The CFR provides a general description for each classified MD, including the intended use, the device class (i.e., Class I, II, III), and information related to marketing requirements. In the European context, the corresponding PC is UDI indentifier according to Regulation (EU) 2017/745 of April 5, 2017. The new Regulation establishes an electronic system for the unique device identification in the EUDAMED database, which enables unique identification in the EU market and facilitates their traceability.
4.2 Analysis of the classification methods
The analysis just performed shows that only a few works fulfil the requirement of classifying MDs with management objective.
The strength of Heneske’s work [35] is the need to adopt different methodological groups depending on the nature of the device. Indeed, within this taxonomic model, the devices are evaluated based on the risk class and HTA logic. The matrix model is not without limitations because the color-coding is based on assumptions, and the risk assessment is addressed on a specific product without valuing the context of use. Nevertheless, the newly developed taxonomy combines the two worlds and allows CED to consider device risk in more detail.
Bliznakov’s teamwork [25, 37], has grouped MDs in order to develop Web-Praxis system. At the top-level, the strength is the possibility to apply to our needs the 12 or more categories based on the knowledge set of authors and professional discipline. Moreover, the middle-level can be applied to our aim because MDs are grouped with the same or similar intended uses or common technologies in order to indent device types with common features or functions.
In Aronson’s work [39], an interesting aspect concerns the PC used by the FDA. Specifically, an important strength that can be applied to our work is the possibility to divide the MDs into 19 “panels” (medical specialties). The PC is made up of seven alphanumeric symbols as follows: two digits for the Industry Code, one for the Class, and two for the Product. Unfortunately, the latter two are assigned randomly.
Among the nomenclatures examined and analyzed, the CND classification is the most suitable for our purpose. It is based on anatomical systems and it presents some strengths. CND code structure can group devices into homogeneous categories, as opposed to CIVAB nomenclature where there is no grouping system. Furthermore, CND is going to be the EMDN base nomenclature, and it allows clinical engineers to monitor how devices are used, even enabling an analysis of failures by being able to compare individual categories.
In the next future, the most effective and successful choice in terms of efficiency and optimization, is to adopt the EMDN nomenclature, following the European trend proposed by MDCG.
5 Conclusions
We performed this study with the final goal of identifying the best-suited method for grouping MDs into classes. We screened all available articles on both Ovid and Scopus databases. We found few articles addressing nomenclature systems on OVID due to its prevalent focus on medical and health journals. Then, we performed a second query on Scopus. Despite the presence of more technological and management journals, we found only nine papers matching our search criteria. On the basis of our search, only a few works fulfil the requirement of classifying MDs with management objective (e.g., inventories, database, and supply chains).
The analysis that we performed has shown that it is possible to reduce the number of classes into group systems. The method locally developed by ESTAR in Italy is a valid tool able to reduce the number of device classes and to perform an effective control, thanks to its hierarchical structure which highlights the relationships between the devices belonging to the same system. Furthermore, it shares analogies to the national italian classification (CND). The limits of the ESTAR methodology can be overcome by the contemporary use of the CND code, replacing the old CIVAB coding system. Based on this literature analysis, we think that adopting the EMDN nomenclature, following the MDCG directive for the EUDAMED database, is at the moment the most effective and successful choice for European healthcare structures. The European Commission is, at the date we are writing, holding a month-long online consultation on the European Medical Device Nomenclature (EMDN) English version, aimed to collect feedback from users by 4 June 2021 [4]. We believe that the dissemination of the findings from this scoping review can bring positive relapses also in re-framing the existing nomenclature systems, in the light of a future global system, as proposed by WHO in its roadmap [4]. Finally, CEDs should start planning all the needed steps to put in place such a migration, to pursue a proper Evidence Based Management system.
References
World Health Organization: Standardization of medical devices nomenclature. https://apps.who.int/gb/ebwha/pdf_files/EB145/B145_3-en.pdf?ua=1 (2019). Accessed 20 May 2021.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L, et al. Prisma extension for scoping reviews (prisma-scr): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
World Health Organization: Standardization of medical devices nomenclature. https://apps.who.int/gb/ebwha/pdf_files/EB148/B148_13-en.pdf (2021). Accessed 20 May 2021.
World Health Organization: Health product and policy standards. https://www.who.int/teams/health-product-and-policy-standards/access-to-assistive-technology-medical-devices/medical-devices/nomenclature. Accessed 20 May 2021.
Perleth M, Busse R, Schwartz FW. Regulation of health-related technologies in germany. Health Policy. 1999;46(2):105–26.
Ibey AA, King D, Hsieh T, Hutnan T, Dixon J, Soet R. What constitutes a clinical engineering asset? J Clin Eng. 2015;40(3):165–8.
Miniati R, Dori F, Iadanza E, Fregonara MM, Gentili GB. Health technology management: a database analysis as support of technology managers in hospitals. Technol Health Care. 2011;19(6):445–54.
Ministero della Salute. Classificazione nazionale dei dispositivi medici (cnd). http://www.salute.gov.it/portale/temi/p2_6.jsp?lingua=italiano&id=328&area=dispositivi-medici&menu=classificazione. Accessed 20 May 2021.
Sherwin J. The essentials of medical device inventory tracking. Biomed Instrum Technol. 2013;47(5):382–6.
Iadanza E, Marzi L, Dori F, Gentili GB, Torricelli M. Hospital health care offer. A monitoring multidisciplinar approach. In World Congress on Medical Physics and Biomedical Engineering 2006. Springer, 2007. p. 3685–8.
U.S. Food & Drug Administration. Udi basics. https://www.fda.gov/medical-devices/unique-device-identification-system-udi-system/udi-basics. Accessed 20 May 2021.
Wang B, Fedele J, Pridgen B, Williams A, Rui T, Barnett L, Granade C, Helfrich R, Stephenson B, Lesueur D, et al. Evidence-based maintenance: part ii: comparing maintenance strategies using failure codes. J Clin Eng. 2010;35(4):223–30.
Wang B, Fedele J, Pridgen B, Williams A, Rui T, Barnett L, Granade C, Helfrich R, Stephenson B, Lesueur D, et al. Evidence-based maintenance: part iii, enhancing patient safety using failure code analysis. J Clin Eng. 2011;36(2):72–84.
Wang B, Rui T, Koslosky J, Fedele J, Balar S, Hertzler LW, Poplin B. Evidence-based maintenance: part iv-comparison of scheduled inspection procedures. J Clin Eng. 2013;38(3):108–16.
White J, Carolan-Rees G. Current state of medical device nomenclature and taxonomy systems in the uk: spotlight on gmdn and snomed ct. JRSM Short Reports. 2013;4(7):1–7.
Wang B, Fedele J, Pridgen B, Williams A, Rui T, Barnett L, Granade C, Helfrich R, Stephenson B, Lesueur D, et al. Evidence-based maintenance: part i: measuring maintenance effectiveness with failure codes. J Clin Eng. 2010;35(3):132–44.
Health Technology Assessment Division. https://ifmbe.org/organisation-structure/divisions/htad/. Accessed 20 May 2021.
European Alliance for Medical and Biological Engineering and Science. https://eambes.org/. Accessed 20 May 2021.
Mobarek I, Al Tarawneh W, Langevin F, Ibbini M. Fully automated clinical engineering technical management system. J Clin Eng. 2006;31(1):46–60.
Jiang G, Yu Y, Kingsbury PR, Shah N. Augmenting medical device evaluation using a reusable unique device identifier interoperability solution based on the ohdsi common data model. Stud Health Technol Inform. 2019;264:1502–3.
World Health Organization: Nomenclature of medical devices. https://www.who.int/medical_devices/priority/mde_nomenclature/en/ (2019). Accessed 20 May 2021.
Wang B. Evidence-Based Maintenance of Medical Equipment. An outcomes-based method of keeping medical equipment safe and reliable: Independently published; 2019.
Hefflin BJ, Gross TP, Richardson EA, Coates VH. Medical device nomenclature. Medical Device Epidemiology and Surveillance. 2007. p. 87.
European Commission. The European Medical Device Nomenclature (EMDN). https://ec.europa.eu/docsroom/documents/28668/ attachments/1/translations/en/renditions/native. Accessed 20 May 2021.
Bliznakov Z, Malataras P, Pallikarakis N. Medical equipment inventorying and installation of a web-based management system–pilot application in the periphery of crete, greece. In 11th Mediterranean Conference on Medical and Biomedical Engineering and Computing 2007. Springer, 2007. p. 1092–5.
World Health Organization. Global atlas of medical devices. World Health Organization. 2017. p. 70–5.
Ohdsi. OHDSI Common Data Model. https://github.com/OHDSI/CommonDataModel/wiki. Accessed 20 May 2021.
The European Parliament and the Council of the European Union. Eu regulation 2017/745. https://eur-lex.europa.eu/legal-content/en/TXT/?uri=celex%3A32017R0745. Accessed 20 May 2021.
UNI EN 15341. Maintenance - Maintenance Key Performance Indicators. 2019.
Bianchini E, Francesconi M, Testa M, Tanase M, Gemignani V. Unique device identification and traceability for medical software: a major challenge for manufacturers in an ever-evolving marketplace. J Biomed Inform. 2019;93:103150.
Camus D, Thiveaud D, Josseran A, Barthélémy C-E, Chambrin P-Y, Hebbrecht G, Lafont J, Mazaud P, Pazart L, Soly P, et al. New european medical device regulation: How the french ecosystem should seize the opportunity of the eudamed and the udi system, while overcoming the constraints thereof. Therapies. 2019;74(1):73–85.
European Commission. Mdcg 2018-2. future eu medical device nomenclature. description of requirements. https://ec.europa.eu/docsroom/documents/39009/attachments/1/translations/en/renditions/native. Accessed Feb 2018.
ISO. ISO 15225: Medical devices – Quality management – Medical device nomenclature data structure.
The Council of the European Communities. Council directive 90/385/eec. https://eur-lex.europa.eu/legal-content/EN/ALL/?uri=celex:31990L0385. Accessed 20 May 2021.
Iadanza E, Gonnelli V, Satta F, Gherardelli M. Evidence-based medical equipment management: a convenient implementation. Med Biol Eng Comput. 2019;57(10):2215–30.
Anand K, Veermaram C, Saini S, Singh B. Global medical device nomenclature: The concept for reducing device-related medical errors. J Young Pharm. 2010;2(4):403–9.
Bliznakov Z, Pappous G, Bliznakova K, Pallikarakis N. Integrated software system for improving medical equipment management. Biomed Instrum Technol. 2003;37(1):25–33.
Henschke C, Panteli D, Perleth M, Busse R. Taxonomy of medical devices in the logic of health technology assessment. Int J Technol Assess Health Care. 2015;31(5):324–30.
Aronson JK, Heneghan C, Ferner RE. Medical devices: definition, classification, and regulatory implications. Drug Saf. 2020;43(2):83–93.
Brown C, Kaushiva A, Chi L. Fundamentals of unique device identification. J Clin Eng. 2015;40(1):35–6.
Luschi A, Marzi L, Miniati R, Iadanza E. A custom decision-support information system for structural and technological analysis in healthcare. In XIII Mediterranean Conference on Medical and Biological Engineering and Computing 2013. Springer, 2014. p. 1350–3.
The Council of the European Union. Directive 93/42/cee. https://eur-lex.europa.eu/legal-content/en/TXT/?uri=celex%3A31993L0042. Accessed 20 May 2021.
Drozda JP Jr, Dudley C, Helmering P, Roach J, Hutchison L. The mercy unique device identifier demonstration project: implementing point of use product identification in the cardiac catheterization laboratories of a regional health system. In Healthcare. Elsevier, 2016;4(2):116–9.
The European Parliament and the Council of the European Union. Directive 98/79/ec. https://eur-lex.europa.eu/legal-content/it/TXT/?uri=CELEX:31998L0079. Accessed 20 May 2021.
Regione Toscana. Ente di supporto tecnico amministrativo regionale. https://www.regione.toscana.it/estar. Accessed 20 May 2021.
Pecchia L, Piaggio D, Maccaro A, Formisano C, Iadanza E. The inadequacy of regulatory frameworks in time of crisis and in low-resource settings: personal protective equipment and covid-19. Heal Technol. 2020;10(6):1375–83.
Funding
Open access funding provided by Università degli Studi di Firenze within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Iadanza, E., Cerofolini, S., Lombardo, C. et al. Medical devices nomenclature systems: a scoping review. Health Technol. 11, 681–692 (2021). https://doi.org/10.1007/s12553-021-00567-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12553-021-00567-1