Abstract
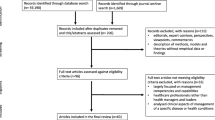
There exist a sizable body of research addressing the evaluation of eHealth/health information technology (HIT) readiness using standard readiness model in the domain of Information Systems (IS). However, there is a general lack of reliable indicators used in measuring readiness assessment factors, resulting in limited predictability. The availability of reliable measuring tools could help improve outcomes of readiness assessments. In determining the predictive relevance of developed HIT model we collected quantitative data from clinical and non-clinical (administrators) staff at Komfo Anokye Teaching Hospital (KATH), Kumasi Ghana using the traditional in-person distribution of paper-based survey, popularly known as drop and collect survey (DCS). We then used PLS-SEM path analysis to measure the predictive relevance of a block of manifest indicators of the readiness assessment factors. Three important readiness assessment factors are thought to define and predict the structure of the KATH HIT/eHealth readiness survey data (Technology readiness (TR); Operational resource readiness (ORR); and Organizational cultural readiness (OCR). As many public healthcare organizations in Ghana have already gone paperless without any reliable HIT/eHealth guiding policy, there is a critical need for reliable HIT/eHealth regulatory policies readiness (RPR) and some improvement in HIT/eHealth strategic planning readiness (core readiness). The final model (R2 = 0.558 and Q2 = 0.378) suggest that TR, ORR, and OCR explained 55.8% of the total amount of variance in HIT/eHealth readiness in the case of KATH and the relevance of the overall paths of the model was predictive. Fit values (SRMR = 0.054; d_ULS = 6.717; d_G = 6.231; Chi2 = 6,795.276; NFI = 0.739). Generally, the GoF for this SEM are encouraging and can substantially be improved.



Similar content being viewed by others
Notes
eHealth, HIT and digital health are uses interchangeably in this paper.
Information quality relates to the quality of output in the context of content, presentation, and relevance of information (Ibid).
Service quality denotes the overall support offered to system users to help in achieving their goals of using the IS (Ibid).
Medical doctors, pharmacists, RNs, Lab technicians.
Administrative officers.
References
Acquah-Swanzy, M. Evaluating electronic health record systems in Ghana: the case of Effia Nkwanta regional hospital. 2015, UiT Norges arktiske universitet.
Adebayo K, Ofoegbu E. Issues on E-health adoption in Nigeria. International Journal of Modern Education and Computer Science. 2014;6:36.
Adebesin F. et al. Barriers & challenges to the adoption of E-Health standards in Africa; 2013.
Sullivan GM. A primer on the validity of assessment instruments. ACGME Suite 2000. 2011;515–9.
Akosua A, Aseweh A. Financing public healthcare institutions in Ghana. Journal of Health Organization and Management. 2011;25:128–41.
Al-Adwan A, Berger H. Exploring physicians’ behavioural intention toward the adoption of electronic health records: an empirical study from Jordan. Int J Healthc Technol Manag. 2015;15:89–111.
Al Sallakh M, Rodgers S, Lyons R, Sheikh A, Davies G. Socioeconomic deprivation and inequalities in asthma care in Wales. Lancet. 2017;390:S19.
Alarcón D, Sánchez J. Assessing convergent and discriminant validity in the ADHD-R IV rating scale: user-written commands for Average Variance Extracted (AVE), Composite Reliability (CR), and Heterotrait-Monotrait ratio of correlations (HTMT). Spanish Stata Meeting; 2015.
Albers S. PLS and success factor studies in marketing. Handbook of partial least squares; 2010. p. 409–25.
Arpaci I. A theoretical framework for IT consumerization: factors influencing the adoption of BYOD. Handbook of research on technology integration in the global world. IGI Global; 2019.
Bagozzi R, Yi Y. On the evaluation of structural equation models. J Acad Mark Sci. 1988;16:74–94.
Bangert D, Doktor R. The role of organizational culture in the management of clinical e-health systems. System Sciences, 2003. Proceedings of the 36th Annual Hawaii International Conference on, 2003. IEEE, 9 pp.
Barzekar H, Karami M. Organizational factors that affect the implementation of information technology: perspectives of middle managers in Iran. Acta Informatica Medica. 2014;22:325.
Bedeley R, Palvia P. A study of the issues of e-health care in developing countries: The case of Ghana; 2014:2.
Bentler P, Bonett D. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88:588.
Bland JM, Altman D. Statistics notes: Cronbach’s alpha. BMJ. 1997;314:572.
Bollen K. A new incremental fit index for general structural equation models. Sociol Methods Res. 1989;17:303–16.
Brown S. Drop and collect surveys: a neglected research technique? Market Intell Plan. 1987;5:19–23.
Byrne B. Structural equation modeling with EQS and EQS/Windows: basic concepts applications and programming. Thousand Oaks: Sage; 1994.
Cain M, Zhang Z, Yuan K. Univariate and multivariate skewness and kurtosis for measuring nonnormality: prevalence, influence and estimation. Behav Res Methods. 2016; 1–20.
Chin W. Commentary: issues and opinion on structural equation modeling. 1998, JSTOR 3.
Cohen J. Statistical power analysis for the behavioral sciences. Hilsdale: Lawrence Earlbaum Associates; 1988. p. 2.
Dansky K, Gamm L, Vasey J, Barsukiewicz C. Electronic medical records: are physicians ready? J Healthc Manag. 1999;44:440–54.
Delone W, Mclean E. Information systems success: the quest for the dependent variable. Inf Syst Res. 1992;3:60–95.
Delone W, Mclean E. The DeLone and McLean model of information systems success: a ten-year update. J Manag Inf Syst. 2003;19:9–30.
Delone W, Mclean E. Measuring e-commerce success: applying the DeLone & McLean information systems success model. Int J Electron Commer. 2004;9:31–47.
Dewi MAA, Hidayanto AN, Purwandari B, Kosandi M, Budi NFA. Smart City readiness model using Technology-Organization-Environment (TOE) framework and its effect on adoption decision. PACIS; 2018. p. 268.
Dwivedi Y, Wade M, Schneberger S. Information systems theory: explaining and predicting our digital society. New York: Springer Science & Business Media; 2012.
Eden K, Totten A, Kassakian S, Gorman P, Mcdonagh M, Devine B, Pappas M, Daeges M, Woods S, Hersh W. Barriers and facilitators to exchanging health information: a systematic review. Int J Med Inform. 2016;88:44–51.
Eigner I, Hamper A, Wickramasinghe N, Bodendorf F. Success factors for National eHealth Strategies: a comparative analysis of the Australian and German eHealth system. Int J Networking Virtual Organ. 2019;21:399–424.
Faber S, Van Geenhuizen M, De Reuver M. eHealth adoption factors in medical hospitals: a focus on the Netherlands. Int J Med Inform. 2017;100:77–89.
Fanta GB, Pretorius L. A conceptual framework for sustainable eHealth implementation in resource-constrained settings. S Afr J Ind Eng. 2018;29:132–47.
Fanta G, Pretorius L, Erasmus L. A system dynamics model of eHealth acceptance: a sociotechnical perspective. International Association For Management Of Technology IAMOT; 2016; p. 259–72.
Fanta G, Pretorius L, Erasmus L. Organizational dynamics of sustainable eHealth implementation: a case study of Ehmis. 2017 Portland International Conference on Management of Engineering and Technology (PICMET), 2017. IEEE, p. 1–9.
Fornell C, Larcker D. Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. 1981;18:39–50.
Freeze R, Alshare K, Lane P, Wen H. Is success model in e-learning context based on students’ perceptions. J Inf Syst Educ. 2019;21:4.
Fricker S, Thümmler C, Gavras A. Requirements engineering for digital health. Cham: Springer; 2015.
Garson G. Partital least sqaures: ression & structural equation models. Asheboro: G. David Garson and Statistical Associates Publishing; 2016.
Gefen D, Straub D, Boudreau M. Structural equation modeling and regression: guidelines for research practice. Commun Assoc Inf Syst. 2000;4:7.
Gholamhosseini L, Ayatollahi H. The design and application of an e-health readiness assessment tool. Health Information Management Journal. 2017;46:32–41.
Gil-Garcia J. Using partial least squares in digital government research, in Handbook of research on public information technology. 2008, IGI Global. p. 239-253. 4.
Gorla N, Somers T, Wong B. Organizational impact of system quality, information quality, and service quality. J StrategInfSyst. 2010;19:207–28.
Gregory M, Tembo S. Implementation of E-health in developing countries challenges and opportunities: a case of Zambia. Science and Technology. 2017;7:41–53.
Grisot M, Vassilakopoulou P. Re-infrastructuring for eHealth: dealing with turns in infrastructure development. Comput Supported Coop Work. 2017;26:7–31.
Hair J Jr, Black W, Babin B, Anderson R. Multivariate data analysis; a global perspective (Ed.). New Jersey: Pearson Education Inc.; 2010, p. 5.
Hair F Jr, Sarstedt M, Hopkins L, Kuppelwieser V. Partial least squares structural equation modeling (PLS-SEM): an emerging tool in business research. Eur Bus Rev. 2014;26:106–21.
Hair J Jr, Hult GT, Ringle C, Sarstedt M. A primer on partial least squares structural equation modeling (PLS-SEM). Thousand Oaks: Sage Publications; 2016.
Hair J, Hollingsworth C, Randolph A, Chong A. An updated and expanded assessment of PLS-SEM in information systems research. Industrial Management & Data systems. 2017;117:442–58.
Hao J, Shi H, Shi V, Yang C. Adoption of automatic warehousing systems in logistics firms: a technology–organization–environment framework. Sustainability. 2020;12:5185.
Harding K, Biks GA, Adefris M, Loehr J, Gashaye K, Tilahun B, Volynski M, Garg S, Abebaw Z, Dessie K. A mobile health model supporting Ethiopia’s eHealth strategy. Digital Medicine. 2018;4:54.
Henseler J, Ringle C, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J Acad Mark Sci. 2015;43:115–35.
Henseler J, Hubona G, Ray P. Using PLS path modeling in new technology research: updated guidelines. Industrial Management & Data Systems. 2016;116:2–20.
Herath TC, Herath HS, D’Arcy J. Organizational adoption of information security solutions: an integrative lens based on innovation adoption and the technology-organization-environment framework. ACM SIGMIS Database: the DATABASE for Advances in Information Systems. 2020;51:12–35.
Hu L, Bentler P. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6:1–55.
Hue TT. The determinants of innovation in vietnamese manufacturing firms: an empirical analysis using a technology–organization–environment framework. Eurasian Business Review. 2019;9:247–67.
Hulland J. Use of partial least squares (PLS) in strategic management research: a review of four recent studies. Strat Manag J. 1999;20:195–204.
Hung S-Y, Hung W-H, Tsai C-A, Jiang S-C. Critical factors of hospital adoption on CRM system: organizational and information system perspectives. Decis Support Syst. 2010;48:592–603.
Jaana M, Tamim H, Paré G, Teitelbaum M. Key IT management issues in hospitals: results of a Delphi study in Canada. Int J Med Inform. 2011;80:828–40.
Jalghoum Y, Tahtamouni A, Khasawneh S, Al-Madadha A. Challenges to healthcare information systems development: the case of Jordan. International Journal of Healthcare Management; 1–9; 2019.
Kline R. Principles and practice of structural equation modeling. New York: Guilford Publications; 2015.
Koivumäki T, Pekkarinen S, Lappi M, Väisänen J, Juntunen J, Pikkarainen M. Consumer adoption of future MyData-based preventive eHealth services: an acceptance model and survey study. Journal of Medical Internet Research. 2017;19:E429.
Kupek E. Beyond logistic regression: structural equations modelling for binary variables and its application to investigating unobserved confounders. BMC Med Res Methodol. 2006;6:13.
Kwao L, Millham R, Opanin Gyamfi E. An integrated success model for adopting biometric authentication technique for District Health Information Management System 2, Ghana. Ghana (February 20, 2020); 2020. 5.
Landis-Lewis Z, Manjomo R, Gadabu O, Kam M, Simwaka B, Zickmund S, Chimbwandira F, Douglas G, Jacobson R. Barriers to using eHealth data for clinical performance feedback in Malawi: a case study. Int J Med Inform. 2015;84:868–75.
Lee K, Che S. Introduction to partial least square: common criteria and practical considerations. Advanced materials research. Trans Tech Publ; 2013. p. 1766–9.
Lennon M, Bouamrane M-M, Devlin A, O'Connor S, O'Donnell C, Chetty U. et al. Readiness for delivering digital health at scale: lessons from a longitudinal qualitative evaluation of a national digital health innovation program in the United Kingdom. Journal of Medical Internet Research. 2017;19:E42.
Li J, Talaei-Khoei A, Seale H, Ray P, Macintyre C. Health care provider adoption of eHealth: systematic literature review. Interactive Journal of Medical Research. 2013;2:e7.
Lin H-F. Understanding the determinants of electronic supply chain management system adoption: using the technology–organization–environment framework. Technol Forecast Soc Chang. 2014;86:80–92.
Lomax R, Schumacker R. A beginner’s guide to structural equation modeling. New York: Routledge Academic; 2012.
Long L-A, Pariyo G, Kallander K. Digital technologies for health workforce development in low-and middle-income countries: a scoping review. Global Health: Science and Practice. 2018;6:S41–8.
Lowry P, Gaskin J. Partial least squares (PLS) structural equation modeling (SEM) for building and testing behavioral causal theory: when to choose it and how to use it. IEEE Trans Prof Commun. 2014;57:123–46 (139).
Matar N, Alnabhan M. Evaluating E-Health services and patients requirements in Jordanian Hospitals. Int Arab J E-Technol. 2014;3:250–7.
Maunder K, Walton K, Williams P, Ferguson M, Beck E. A Framework for eHealth readiness of dietitians. Int J Med Inform. 2018;115:43–52.
Mcgowan J, Cusack C, Bloomrosen M. The future of health it innovation and informatics: a report from AMIA’s 2010 policy meeting. J Am Med Inform Assoc. 2012;19:460–7.
Mertes A, Brüesch C. Stakeholder participation in eHealth policy: a Swiss case study on the incorporation of stakeholder preferences. IRSPM 22nd Annual Conference, Edinburgh, Scotland, 11–13 April 2018. International Research Society for Public Management; 2018. p. 1–23.
Mettler T, Vimarlund V. Evaluation of E-Health strategies: a portfolio approach. The 15th International Symposium for Health Information Management Research (ISHIMR 2011), Sept 8–9, Zurich; 2011.
Moss S. Fit indices for structural equation modeling. Website: https://www.psych-it.com.au/Psychlopedia/article.asp; 2009.
Nunnally J. Psychometric theory. New York: Mcgraw-Hill; 1978.
Ojo A. Validation of the DeLone and McLean information systems success model. Healthcare Informatics Research. 2017;23:60–6.
Oliveira T, Martins M. Information technology adoption models at firm level: review of literature. European Conference on Information Management and Evaluation. Academic Conferences International Limited; 2011. p. 312.
Omotosho A, Ayegba P, Emuoyibofarhe J, Meinel C. Current state of ICT in healthcare delivery in developing countries. International Journal of Online Engineering. 2019;15:91–107.
Pan M-J, Jang W-Y. Determinants of the adoption of enterprise resource planning within the technology-organization-environment framework: Taiwan’s communications industry. J Comput Inf Syst. 2008;48:94–102.
Party AW. WP 131, 11. Working document on the processing of personal data relating to health in electronic health records (EHR). Adopted on 2007 (WP 131); 2007.
Ramayah T, et al. Testing a confirmatory model of facebook usage in smartPLS using consistent PLS. IJBI, 2017;3(2):1-14. 6.
Ribes D, Polk J. Flexibility relative to what? Change to research infrastructure. J Assoc Inf Syst. 2014;15:1.
Sanchez G. Pls path modeling with R. Berkeley: Trowchez Editions; 2013.
Scherer R, Siddiq F, Tondeur J. The technology acceptance model (TAM): a meta-analytic structural equation modeling approach to explaining teachers’ adoption of digital technology in education. Comput Educ. 2019;128:13–35.
Schreiber J, Nora A, Stage F, Barlow E, King J. reporting structural equation modeling and confirmatory factor analysis results: a review. J Educ Res. 2006;99:323–38.
Scott R, Mars M. Principles and framework for eHealth strategy development. Journal of Medical Internet Research. 2013;15:e155.
Shim M, Jo H. What quality factors matter in enhancing the perceived benefits of online health information sites? Application of the updated DeLone and McLean information systems success model. Int J Med Inform. 2020;137:104093.
Singeh FW, Abrizah A, Kiran K. Bringing the digital library success factors into the realm of the technology-organization-environment framework. The Electronic Library. 2020;7.
Sullivan G. A primer on the validity of assessment instruments. Chicago: The Accreditation Council for Graduate Medical Education Suite; 2011.
Sunny S, Patrick L, Rob L. Impact of cultural values on technology acceptance and technology readiness. Int J Hosp Manag. 2019;77:89–96.
Teo T, Lin S, Lai K-H. Adopters and non-adopters of e-procurement in Singapore: an empirical study. Omega. 2009;37:972–87.
Tornatzky L, Fleischer M. The process of technology innovation. Lexington: Lexington Books; 1990.
Urbach N, Ahlemann F. Structural equation modeling in information systems research using partial least squares. JITTA: Journal of Information Technology Theory and Application. 2010;11:5.
Van Velsen L, Evers M, Bara C-D, Den Akker H, Boerema S, Hermens H. Understanding the acceptance of an ehealth technology in the early stages of development: an end-user walkthrough approach and two case studies. JMIR Formative Research. 2018;2:E10474.
Veinot T, Ancker J, Bakken S. Health informatics and health equity: improving our reach and impact. J Am Med Inform Assoc. 2019;26:689–95.
Venkatesh V, Bala H. Technology acceptance model 3 and a research agenda on interventions. Decision Sciences. 2008;39:273–315.
Vinzi V, Chin W, Henseler J, Wang H. Handbook of partial least squares. Berlin: Springer; 2010.
Wang C, Ku E. eHealth in kidney care. Nat Rev Nephrol. 2020;1–3.
William C. 22 Privacy and security: privacy of personal eHealth data in low-and middle-income countries. Global health informatics: principles of EHealth and MHealth to improve quality of care, p. 269.
World Health Organization. Country coorperation strategy brief, Ghana. WHO; 2014.
Yusif S, Soar J. Preparedness for e-Health in developing countries: the case of Ghana. JHIDC. 2014;8:18–37.
Yusif S, Hafeez-Baig A, Soar J. E-health readiness assessment factors and measuring tools: a systematic review. Int J Med Inform. 2017;107:56–64.
Yusif S, Hafeez-Baig A, Soar J. An exploratory study of the readiness of public healthcare facilities in developing countries to adopt Health Information Technology (HIT)/e-Health: the case of Ghana. Journal of Healthcare Informatics Research; 2020.
Yusif S, Hafeez-Baig A, Soar, J. A model for evaluating ehealth preparedness–a case study approach. Transforming Government: People, Process and Policy; 2020.
Zakaria N, Yusof S, Zakaria N. Managing ICT in healthcare organization: culture, challenges, and issues of. Handbook of research on advances in health informatics and electronic healthcare applications: global adoption and impact of information communication technologies: global adoption and impact of information communication technologies; 2009, p. 153.
Zayyad M, Toycan M. Factors affecting sustainable adoption of e-health technology in developing countries: an exploratory survey of nigerian hospitals from the perspective of healthcare professionals. PeerJ. 2018;6:E4436.
Acknowledgments
The authors wish to acknowledge the support of the Australian Government Research Training Program (AGRTP)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Appendix 2
Appendix 3
Appendix 4
Rights and permissions
About this article
Cite this article
Yusif, S., Hafeez-Baig, A., Soar, J. et al. PLS-SEM path analysis to determine the predictive relevance of e-Health readiness assessment model. Health Technol. 10, 1497–1513 (2020). https://doi.org/10.1007/s12553-020-00484-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12553-020-00484-9