Abstract
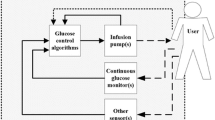
Closed-loop glucose control has the potential to improve the glycemic control in patients with diabetes mellitus type 1. Such an artificial pancreas (AP) should keep the user safe despite all disturbances and faults. The objective of this paper is to analyze those perturbations according to their effects on the glycemic status, and thereby supporting an informed design process of the control system. As suggested by the international standard ISO 14971 for risk management of medical devices, the well proven failure modes and effects analysis (FMEA) was chosen as instrument. An FMEA scheme was modified for this purpose and applied to a single-hormone system with subcutaneous and intraperitoneal routes for glucose sensing and insulin administration. Faults that imply urgent danger and thus require fast detection and diagnosis were identified and distinguished from disturbances that can be sufficiently addressed by basic control functions, e.g. by adaptive control algorithms. Requirements and testing criteria for basic control functions as well as fault detection and diagnosis functions can be derived from the provided overview.

Similar content being viewed by others
References
Kudva YC, Carter RE, Cobelli C, Basu R, Basu A. Closed-loop artificial pancreas systems: physiological input to enhance next-generation devices. Diabetes Care. 2014;37(5):1184–90.
Debono M, Cachia E. The impact of diabetes on psychological well being and quality of life. the role of patient education. Psychol Health Med. 2007;12(5):545–55.
Kropff J, DeVries JH. Continuous glucose monitoring, future products, and update on worldwide artificial pancreas projects. Diabetes Technol Ther. 2016;18(S2):S2–53–63.
Isermann R. Fault-diagnosis systems: an introduction from fault detection to fault tolerance. Berlin Heidelberg: Springer; 2006.
ISO 14971. Medical devices - application of risk management to medical devices. In: ISO Standard. Geneva: ISO; 2007.
Avendaño G. Critical importance of multilateral studies related with adverse events in medical devices. Heal Technol. 2016;6(3):213–27.
Rausand M. Reliability of safety-critical systems : theory and application: Wiley; 2014.
Castle JR, Engle JM, El Youssef J, Massoud RG, Ward WK. Factors influencing the effectiveness of glucagon for preventing hypoglycemia. J Diabetes Sci Technol. 2010;4(6):1305–10.
Medtronic plc, MiniMed® 670G System User Guide, Medtronic plc, 2017.
Welsh JB, Vargas S, Williams G, Moberg S. Designing the modern pump: engineering aspects of continuous subcutaneous insulin infusion software. Diabetes Technol Ther. 2010;12(S1):S37–42.
van Bon AC, Dragt D, DeVries JH. Significant time until catheter occlusion alerts in currently marketed insulin pumps at two basal rates. Diabetes Technol Ther. 2012;14(5):447–8.
McVey E, Keith S, Herr JK, Sutter D, Pettis RJ. Evaluation of intradermal and subcutaneous infusion set performance under 24-hour basal and bolus conditions. J Diabetes Sci Technol. 2015;9(6):1282–91.
Bergenstal RM, Klonoff DC, Garg SK, Bode BW, Meredith M, Slover RH, et al. Threshold-based insulin-pump interruption for reduction of hypoglycemia. The N Engl J Med. 2013;369(3):224–32.
Shah VN, Shoskes A, Tawfik B, Garg SK. Closed-loop system in the management of diabetes: past, present, and future. Diabetes Technol Ther. 2014;16(8):477–90.
Baysal N, Cameron F, Buckingham B, Wilson DM, Bequette BW. Detecting sensor and insulin infusion set anomalies in an artificial pancreas. In: . Washington, DC: ACC. p. 2929–33.
Roberts R, Walsh J, Heinemann L. Help! Someone is beeping. J Diabetes Sci Technol. 2014;8(4):627–9.
Shivers JP, Mackowiak L, Anhalt H, Zisser H. “Turn it off!”: Diabetes device alarm fatigue considerations for the present and the future. J Diabetes Sci Technol. 2013;7(3):789–94.
Georga EI, Protopappas VC, Bellos CV, Fotiadis DI. Wearable systems and mobile applications for diabetes disease management. Heal Technol. 2014;4(2):101–12.
Brazeau AS, Mircescu H, Desjardins K, Leroux C, Strychar I, Ekoe JM, et al. Carbohydrate counting accuracy and blood glucose variability in adults with type 1 diabetes. Diabetes Res Clin Pract. 2013;99(1):19–23.
van Bon AC, Luijf YM, Koebrugge R, Koops R, Hoekstra JBL, DeVries JH. Feasibility of a portable bihormonal closed-loop system to control glucose excursions at home under free-living conditions for 48 hours. Diabetes Technol Ther. 2014;16(3):131–6.
Turksoy K, Samadi S, Feng J, Littlejohn E, Quinn L, Cinar A. Meal detection in patients with type 1 diabetes: A new module for the multivariable adaptive artificial pancreas control system. IEEE JBHI. 2016;20(1):47–54.
Steil GM. Algorithms for a closed-loop artificial pancreas: the case for proportional-integral-derivative control. J Diabetes Sci Technol. 2013;7(6):1621–31.
Bequette BW. Algorithms for a closed-loop artificial pancreas: The case for model predictive control. J Diabetes Sci Technol. 2013;7(6):1632–43.
Bequette BW. Fault detection and safety in closed-loop artificial pancreas systems. J Diabetes Sci Technol. 2014;8(6):1204–14.
Zhang Y, Jones PL, Jetley R. A hazard analysis for a generic insulin infusion pump. J Diabetes Sci Technol. 2010;4(2):263–83.
Ross P, Milburn J, Reith D, Wiltshire E, Wheeler B. Clinical review: insulin pump-associated adverse events in adults and children. Acta Diabetol. 2015;52(6):1017–24.
Ross P, Gray A, Milburn J, Kumarasamy I, Wu F, Farrand S, et al. Insulin pump-associated adverse events are common, but not associated with glycemic control, socio-economic status, or pump/infusion set type. Acta Diabetol. 2016;53(6):991–8.
Rabbone I, Minuto N, Toni S, Lombardo F, Iafusco D, Marigliano M, et al. Insulin pump breakdown and infusion set failure in Italian children with type 1 diabetes: a 1-year prospective observational study with suggestions to minimize clinical impact. Diabetes Obes Metab. 2018;20(11):2551–6.
Taleb N, Messier V, Ott-Braschi S, Ardilouze J-L, Rabasa-Lhoret R. Perceptions and experiences of adult patients with type 1 diabetes using continuous subcutaneous insulin infusion therapy: Results of an online survey. Diabetes Res Clin Pract. 2018;144:42–50.
Guilhem I, Leguerrier AM, Lecordier F, Poirier JY, Maugendre D. Technical risks with subcutaneous insulin infusion. Diabete Metab. 2006;32(3):279–84.
Heinemann L, Krinelke L. Insulin infusion set: the achilles heel of continuous subcutaneous insulin infusion. J Diabetes Sci Technol. 2012;6(4):954–64.
Deiss D, Adolfsson P, Alkemade-van Zomeren M, Bolli GB, Charpentier G, Cobelli C, et al. Insulin infusion set use: European perspectives and recommendations. Diabetes Technol Ther. 2016;18(9):517–24.
Bequette BW. Continuous glucose monitoring: real-time algorithms for calibration, filtering, and alarms. J Diabetes Sci Technol. 2010;4(2):404–18.
Home PD. Plasma insulin profiles after subcutaneous injection: how close can we get to physiology in people with diabetes? Diabetes Obes Metab. 2015;17(11):1011–20.
Ramkissoon CM, Veh J, Aufderheide B, Bequette BW, Palerm CC, A taxonomy of safety issues to be overcome in the artificial pancreas. (Abstract No. 445) poster presented at ATTD, Paris, 2015.
Blauw H, Keith-Hynes P, Koops R, DeVries JH, A review of safety and design requirements of the artificial pancreas. Annals of Biomedical Engineering, pp. 1–15, 2016.
Ramkissoon CM, Aufderheide B, Bequette BW, Vehi J. A review of safety and hazards associated with the artificial pancreas. Biomedical Engineering, IEEE Reviews. 2017;10:44–62.
Kowalski AJ. Can we really close the loop and how soon? Accelerating the availability of an artificial pancreas: a roadmap to better diabetes outcomes. Diabetes Technol Ther. 2009;11(S1):S113–9.
Feng J, Turksoy K, Cinar A. Performance assessment of model-based artificial pancreas control systems. In: Kirchsteiger H, Jørgensen JB, Renard E, del Re L, editors. Prediction methods for blood glucose concentration. Lecture notes in bioengineering. Cham: Springer; 2016. pp. 243–65.
Guenego A, Bouzillé G, Breitel S, Esvant A, Poirier J-Y, Bonnet F, et al. Insulin pump failures: Has there been an improvement? Update of a prospective observational study. Diabetes Technol Ther. 2016;18(12):820–4.
Schaepelynck P, Darmon P, Molines L, Jannot-Lamotte M, Treglia C, Raccah D. Advances in pump technology: insulin patch pumps, combined pumps and glucose sensors, and implanted pumps. Diabete Metab. 2011;37:S85–93.
Liebl A, Hoogma R, Renard E, Geelhoed-Duijvestijn PH, Klein E, Diglas J, et al. A reduction in severe hypoglycaemia in type 1 diabetes in a randomized crossover study of continuous intraperitoneal compared with subcutaneous insulin infusion. Diabetes Obes Metab. 2009;11(11):1001–8.
Blanke M, Kinnaert M, Lunze J, Staroswiecki M. Diagnosis and fault-tolerant control, 2nd edn. Berlin Heidelberg: Springer; 2006.
Vaddiraju S, Burgess DJ, Tomazos I, Jain FC, Papadimitrakopoulos F. Technologies for continuous glucose monitoring: current problems and future promises. J Diabetes Sci Technol. 2010;4(6):1540–62.
Klueh U, Kaur M, Qiao Y, Kreutzer DL. Critical role of tissue mast cells in controlling long-term glucose sensor function in vivo. Biomaterials. 2010;31(16):4540–51.
El-Laboudi A, Sharma S, Oliver N, Hussein T, Patel D, Johnston D, et al. Development of a novel microprobe array continuous glucose sensor for type 1 diabetes: Interference studies. Vienna: ATTD; 2014.
Facchinetti A, Favero S, Sparacino G, Cobelli C. An online failure detection method of the glucose sensor-insulin pump system: Improved overnight safety of type-1 diabetic subjects. IEEE Trans Biomed Eng. 2013;60(2):406–16.
Zhao C, Fu Y. Statistical analysis based online sensor failure detection for continuous glucose monitoring in type i diabetes. Chemom Intell Lab Syst. 2015;144:128–37.
Klueh U, Liu Z, Feldman B, Henning TP, Cho B, Ouyang T, et al. Metabolic biofouling of glucose sensors in vivo: role of tissue microhemorrhages. J Diabetes Sci Technol. 2011;5(3):583–95.
Klueh U, Frailey JT, Qiao Y, Antar O, Kreutzer DL. Cell based metabolic barriers to glucose diffusion: macrophages and continuous glucose monitoring. Biomaterials. 2014;35(10):3145–53.
King BR, Goss PW, Paterson MA, Crock PA, Anderson DG. Changes in altitude cause unintended insulin delivery from insulin pumps mechanisms and implications. Diabetes Care. 2011;34(9):1932–3.
Gibney M, Xue Z, Swinney M, Bialonczyk D, Hirsch L. Reduced silent occlusions with a novel catheter infusion set (bd flowsmart): Results from two open-label comparative studies. Diabetes Technol Ther. 2016;18(3):136–43.
Kerr D, Morton J, Whately-Smith C, Everett J, Begley JP. Laboratory-based non-clinical comparison of occlusion rates using three rapid-acting insulin analogs in continuous subcutaneous insulin infusion catheters using low flow rates. J Diabetes Sci Technol. 2008;2(3):450–5.
Schmid V, Hohberg C, Borchert M, Forst T, Pfützner A. Pilot study for assessment of optimal frequency for changing catheters in insulin pump therapy-trouble starts on day 3. J Diabetes Sci Technol. 2010;4(4):976–82.
Hojbjerre L, Skov-Jensen C, Kaastrup P, Pedersen PE, Stallknecht B. Effect of steel and teflon infusion catheters on subcutaneous adipose tissue blood flow and infusion counter pressure in humans. Diabetes Technol Ther. 2009;11(5):301–6.
Heinemann L. Insulin absorption from lipodystrophic areas: A (neglected) source of trouble for insulin therapy? J Diabetes Sci Technol. 2010;4(3):750–3.
Ward WK, Castle JR, El Youssef J. Safe glycemic management during closed- loop treatment of type 1 diabetes: the role of glucagon, use of multiple sensors, and compensation for stress hyperglycemia. J Diabetes Sci Technol. 2011;5(6):1373–80.
Ramkissoon CM, Vehí J. Emotions and diabetes. In: Ortuño F, Rojas I, editors. Bioinformatics and biomedical engineering. IWBBIO 2015. Lecture notes in computer science. Cham: Springer; 2015. pp. 720–27.
Salai M, Vassányi I, Kósa I, Stress detection using low cost heart rate sensors. Journal of Healthcare Engineering. 2016;2016:13. https://doi.org/10.1155/2016/5136705.
Dassau E, Bequette BW, Buckingham BA, Doyle FJ III. Detection of a meal using continuous glucose monitoring implications for an artificial β-cell. Diabetes Care. 2008;31(2):295–300.
Lee H, Bequette BW. A closed-loop artificial pancreas based on model predictive control: Human-friendly identification and automatic meal disturbance rejection. Biomed Signal Process Control. 2009;4(4):347–54.
Lee H, Buckingham BA, Wilson DM, Bequette BW. A closed-loop artificial pancreas using model predictive control and a sliding meal size estimator. J Diabetes Sci Technol. 2009;3(5):1082.
Cameron F, Niemeyer G, Buckingham BA. Probabilistic evolving meal detection and estimation of meal total glucose appearance. J Diabetes Sci Technol. 2009;3(5):1022–30.
Hughes CS, Patek SD, Breton M, Kovatchev BP. Anticipating the next meal using meal behavioral profiles: A hybrid model-based stochastic predictive control algorithm for t1dm. Comput Methods Prog Biomed. 2011;102(2):138–48.
Cameron F, Niemeyer G, Bequette BW. Extended multiple model prediction with application to blood glucose regulation. J Process Control. 2012;22(8):1422–32.
Riddell MC, Zaharieva DP, Yavelberg L, Cinar A, Jamnik VK. Exercise and the development of the artificial pancreas: One of the more difficult series of hurdles. J Diabetes Sci Technol. 2015;9(6):1217–26.
Shetty VB, Fournier PA, Davey RJ, Retterath AJ, Paramalingam N, Roby HC, Cooper MN, Davis EA, Jones TW. Effect of exercise intensity on glucose requirements to maintain euglycaemia during exercise in type 1 diabetes. J Clin Endocrinol Metab. 2016;101(3):972–80.
Ding S, Schumacher M. Sensor monitoring of physical activity to improve glucose management in diabetic patients: A review. Sensors (Basel). 2016;16(4).
Hinshaw L, Dalla Man C, Nandy DK, Saad A, Bharucha AE, Levine JA, et al. Diurnal pattern of insulin action in type 1 diabetes: implications for a closed-loop system. Diabetes. 2013;62(7):2223.
Baysal N, Cameron F, Stenerson M, Buckingham B, Wilson D, Mayer-Davis E, Maahs D, Bequette B. Using activity monitors to improve CGM sensor anomaly detection. Presented at ATTD, Paris, vol. 15, No S1, pp. A2, 2013.
Rausand M, Høyland A. System reliability theory: models, statistical methods, and applications, 2nd edn. Hoboken: John Wiley & Sons; 2004.
Kölle K, Fougner AL, Carlsen SM, Ellingsen R, Stavdahl Ø. Failure analysis of an artificial pancreas — double subcutaneous vs. double intraperitoneal approach, (Abstract No. 334) poster presented at ATTD, Milano, 2016.
ISO/TR 12489, Petroleum, petrochemical and natural gas industries – Reliability modelling and calculation of safety systems, ISO Standard, 2013.
Turksoy K, Quinn L, Littlejohn E, Cinar A. Monitoring and fault detection of continuous glucose sensor measurements. Chicago: ACC; 2015. p. 5091–6.
Feng J, Turksoy K, Samadi S, Hajizadeh I, Cinar A. Hybrid sensor error detection and functional redundancy for artificial pancreas control systems. Trondheim: IFAC DYCOPS-CAB; 2016.
Turksoy K, Roy A, Cinar A. Real-time model-based fault detection of continuous glucose sensor measurements. IEEE Trans Biomed Eng. 2017;64(7):1437–45.
Bondia J, Tarín C, García-Gabin W, Esteve E, Fernández-Real JM, Ricart W, et al. Using support vector machines to detect therapeutically incorrect measurements by the MiniMed CGMSQR. J Diabetes Sci Technol. 2008;2(4):622–9.
Tarin C, Traver L, Bondia J, Vehí J. A learning system for error detection in subcutaneous continuous glucose measurement using support vector machines. Yokohama: CCA; 2010. p. 1614–9.
Leal Y, Ruiz M, Lorencio C, Bondia J, Mujica L, Vehi J. Principal component analysis in combination with case-based reasoning for detecting therapeutically correct and incorrect measurements in continuous glucose monitoring systems. Biomed Signal Process Control. 2013;8(6):603–14.
Leal Y, Gonzalez-Abril L, Lorencio C, Bondia J, Vehi J. Detection of correct and incorrect measurements in real-time continuous glucose monitoring systems by applying a postprocessing support vector machine. IEEE Trans Biomed Eng. 2013;60(7):1891–9.
Cameron F, Buckingham B, Wilson D, Bequette B, Extending threshold based detection of infusion set failures. presented at DMT, Bethesda, 2012.
Herrero P, Calm R, Veh J, Armengol J, Georgiou P, Oliver N, et al. Robust fault detection system for insulin pump therapy using continuous glucose monitoring. J Diabetes Sci Technol. 2012;6(5):1131–41.
Del Favero S, Monaro M, Facchinetti A, Tagliavini A, Sparacino G, Cobelli C. Real-time detection of glucose sensor and insulin pump faults in an artificial pancreas. Cape Town: IFAC World Congress; 2014. p. 1941–6.
Finan DA, Zisser H, Jovanovi L, Seborg DE, Bevier WC. Automatic detection of stress states in type 1 diabetes subjects in ambulatory conditions. Ind Eng Chem Res. 2010;49(17):7843–8.
Rojas R, Garcia-Gabin W, Bequette BW. Multivariate statistical analysis to detect insulin infusion set failure. San Francisco: ACC; 2011. p. 1952–7.
Rojas R, Garcia-Gabin W, Bequette BW. Mean glucose slope – principal component analysis classification to detect insulin infusion set failure. Milano: IFAC World Congress; 2011. p. 14127–32.
Vega-Hernandez O, Campos-Cornejo F, Campos-Delgado DU, Espinoza-Trejo DR. Increasing security in an artificial pancreas: diagnosis of actuator faults. Mexico City: PAHCE; 2009. p. 137–42.
Howsmon DP, Baysal N, Buckingham BA, Forlenza GP, Ly TT, Maahs DM, et al. Real-time detection of infusion site failures in a closed-loop artificial pancreas. Journal of Diabetes Science and Technology. 2018;12(3):599–607.
Kölle K, Fougner AL, Unstad KAF, Stavdahl Ø, Fault detection in glucose control: Is it time to move beyond CGM data? IFAC-PapersOnLine, 2018.
Harvey RA, Dassau E, Zisser H, Seborg DE, Doyle FJ. Design of the glucose rate increase detector a meal detection module for the health monitoring system. J Diabetes Sci Technol. 2014;8(2):307–20.
Turksoy K, Hajizadeh I, Samadi S, Feng J, Sevil M, Park M, et al. Real-time insulin bolusing for unannounced meals with artificial pancreas. Control Eng Pract. 2017;59(C):159–64.
Mahmoudi Z, Nørgaard K, Poulsen NK, Madsen H, Jørgensen JB. Fault and meal detection by redundant continuous glucose monitors and the unscented kalman filter. Biomedical Signal Processing and Control. 2017;38:86–99.
Ramkissoon CM, Herrero P, Bondia J, Vehi J. Meal detection in the artificial pancreas: Implications during exercise. IFAC PapersOnLine. July 2017;50(1):5462–7.
Ramkissoon CM, Herrero P, Bondia J, Vehí J. Unannounced meals in the artificial pancreas: detection using continuous glucose monitoring. Sensors. 2018;18(3):884. https://www.mdpi.com/1424-8220/18/3/884.
Weimer J, Chen S, Peleckis A, Rickels MR, Lee I. Physiology-invariant meal detection for type 1 diabetes. Diabetes Technol Ther. 2016;18(10):616–24.
Kölle K, Fougner AL, Stavdahl Ø, Meal detection based on non-individualized moving horizon estimation and classification. In 2017 IEEE Conference on Control Technology and Applications (CCTA), 2017, pp. 529–535.
Samadi S, Turksoy K, Hajizadeh I, Feng J, Sevil M, Cinar A. Meal detection and carbohydrate estimation using continuous glucose sensor data. IEEE Journal of Biomedical and Health Informatics. 2017;21(3):619–27.
Samadi S, Rashid M, Turksoy K, Feng J, Hajizadeh I, Hobbs N, Lazaro C, Sevil M, Littlejohn E, Cinar A, Automatic detection and estimation of unannounced meals for multivariable artificial pancreas system. Diabetes Technology and Therapeutics. 2018;20(3):235–46.
Heinemann L, Fleming GA, Petrie JR, Holl RW, Bergenstal RM, Peters AL. Insulin pump risks and benefits: A clinical appraisal of pump safety standards, adverse event reporting, and research needs a joint statement of the european association for the study of diabetes and the american diabetes association diabetes technology working group. Diabetes Care. 2015;38(4):716–22.
Zhang Y, Jetley R, Jones PL, Ray A. Generic safety requirements for developing safe insulin pump software. J Diabetes Sci Technol. 2011;5(6):1403–19.
Richter S, Sereseanu A. Developing effective risk assessment criteria in regulated environments, vol. 2. Warsaw: IDAACS; 2015. p. 564–9.
Patek SD, Magni L, Dassau E, Hughes-Karvetski C, Toffanin C, De Nicolao G, et al. Modular closed-loop control of diabetes. IEEE Trans Biomed Eng. 2012;59(11):2986–99.
Venkatasubramanian V, Rengaswamy R, Kavuri S, Yin K. A review of process fault detection and diagnosis: Part III: Process history based methods. Comput Chem Eng. 2003;27(3):327–46.
Baysal N, Cameron F, Buckingham BA, Wilson DM, Chase HP, Maahs DM, et al. A novel method to detect pressure- induced sensor attenuations (PISA) in an artificial pancreas. J Diabetes Sci Technol. 2014;8(6):1091–6.
Castle JR, Pitts A, Hanavan K, Muhly R, El Youssef J, Hughes-Karvetski C, et al. The accuracy benefit of multiple amperometric glucose sensors in people with type 1 diabetes. Diabetes Care. 2012;35(4):706–10.
Shah R, Kristensen J, Wolfe K, Aasmul S, Bansal A, Orthogonally redundant sensor systems and methods. US Generic US20 130 060 105 A1, 2013.
Doyle FJ III, Huyett LM, Lee JB, Zisser HC, Dassau E. Closed-loop artificial pancreas systems: engineering the algorithms. Diabetes Care. 2014;37(5):1191–7.
Howsmon D, Bequette BW. Hypo- and hyperglycemic alarms devices and algorithms. J Diabetes Sci Technol. 2015;9(5):1126–37.
Walsh J, Roberts R, Morris R, Heinemann L. Device connectivity the next big wave in diabetes. J Diabetes Sci Technol. 2015;9(3):701–5.
ISO 14155, Clinical investigation of medical devices for human subjects – Good clinical practice, ISO Standard, 2011.
Cobelli C, Renard E, Kovatchev B. Artificial pancreas: past, present, future. Diabetes. 2011;60(11):2672–82.
Isermann R, Ball P. Trends in the application of model-based fault detection and diagnosis of technical processes. Control Eng Pract. 1997;5(5):709–19.
IEC 60050, International Electrotechnical Vocabulary, IEC Standard.
IEC 61508-4, Functional Safety of Electrical/Electronic/Programmable Electronic Safety- Related Systems. Part 4: Definitions and Abbreviations, IEC Standard, 2010.
Acknowledgements
The study was financed by The Liaison Committee for Education, Research and Innovation in Central Norway (project no. 46075403), and partly by the Research Council of Norway (project no. 248872) and the Centre for Digital Life Norway. The authors would like to thank Sverre C. Christiansen for invaluable input.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Author disclosure statement
An abstract and a poster with preliminary results from this paper were presented at the ATTD conference in Milano, February 2016. All authors expect M. A. Lundteigen are members of the Artificial Pancreas Trondheim (APT) research group (http://www.apt-norway.com/) which focuses on the double intraperitoneal approach for an artificial pancreas. R. Ellingsen is a shareholder and board member of GlucoSet, a company in the glucose monitoring field.
Conflict of interest
The authors declare that they have no conflict of interest.
Terminology
- Adverse event
-
Any untoward medical occurrence, unintended disease or injury, or untoward clinical signs (...) in subjects, users or other persons, whether or not related to the investigational medical device [110]
- Artificial pancreas
-
Closed-loop control of blood glucose in diabetes, is a system combining a glucose sensor, a control algorithm, and an insulin infusion device [111]
- Disturbance
-
An unknown (or uncontrolled) input acting on a system [112]
- Error
-
Discrepancy between a computed, observed or measured value or condition, and the true, specified or theoretically correct value or condition [113]
- Failure mode
-
Manner in which a failure occurs [113] (Fault modes rather than failure modes are actually analyzed in an FMEA, but the term failure modes and effects analysis is the common name of this methodology [7].)
- Failure
-
The termination of the ability of an item to perform a required function [113]
- Fault detection
-
Event by which the presence of a fault becomes apparent [113]
- Fault diagnosis
-
Action to identify and characterize the fault [113]
- Fault identification
-
Determination of the size and time-variant behaviour of a fault. Follows fault isolation [112]
- Fault isolation
-
Determination of the kind, location and time of detection of a fault. Follows fault detection [112]
- Fault tolerance
-
Ability of an item to perform a required function in the presence of certain given sub-item faults [113]
- Fault
-
Inability to perform as required, due to an internal state [113]
- Harm
-
Physical injury or damage to persons, property, and livestock [113]
- Hazard
-
Potential source of harm [113]
- Hazardous event
-
Event that can cause harm [113]
- Hazardous situation
-
Circumstance in which persons, property and livestock or the environment are exposed to at least one hazard [113]
- Intended use
-
Use of a product, process or service in accordance with the information for use provided by the supplier [113]
- Perturbation
-
An input acting on a system, which results in a temporary departure from the current state [112]
- Random hardware failure
-
Failure, occurring at a random time, which results from one or more of the possible degradation mechanisms in the hardware [114]
- Reasonably foreseeable misuse
-
Use of a product, process or service in a way not intended by the supplier, but which may result from readily predictable human behaviour [113]
- Reliability
-
Ability to perform as required, without failure, for a given time interval, under given conditions [113]
- Residual
-
A fault indicator, based on a deviation between measurements and model-equation-based computations. [112]
- Risk analysis
-
Systematic use of available information to identify hazards and to estimate the risk [113]
- Risk
-
Combination of the probability of occurrence of harm and the severity of that harm [113]
- Safety
-
Freedom from unacceptable risk to the outside from the functional and physical units considered [113]
- Systematic failure
-
Failure that consistently occurs under particular conditions of handling, storage or use [113]
Rights and permissions
About this article
Cite this article
Kölle, K., Fougner, A.L., Lundteigen, M.A. et al. Risk analysis for the design of a safe artificial pancreas control system. Health Technol. 9, 311–328 (2019). https://doi.org/10.1007/s12553-018-0269-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12553-018-0269-8