Abstract
Background
Weight-loss approaches involving mindfulness have been reported to reduce overeating behavior. We conducted a preliminary evaluation of the feasibility and effectiveness of a mindfulness mobile application (MMA) combined with a comprehensive lifestyle intervention (CLI) focused on weight loss and eating behaviors for people with metabolic syndrome based on post-intervention follow-up data.
Method
Participants were randomly assigned (1:1) to a CLI group or a CLI + MMA group. Participants received weekly CLI for 13 weeks, followed by telephone counseling for 13 weeks. The CLI + MMA group also had access to the MMA. Feasibility was assessed by the number of people who refused to participate, rate of adherence to the MMA, follow-up rate, and participant satisfaction. The preliminary endpoint was weight change (at 26 weeks). Participants completed the Dutch Eating Behavior Questionnaire (DEBQ). A mixed linear model was used for efficacy analysis.
Results
Eight of the 40 participants declined to participate. The MMA was used 4.4 ± 1.7 days per week, but the rate of adherence declined over time. The follow-up rate was 100%, and there was no difference in participant satisfaction between the groups. There was no significant group-by-time interaction for weight loss (p = 0.924), but there was a significant interaction for the DEBQ restrained eating score (p = 0.033).
Conclusions
This study found that CLI plus MMA was highly feasible and moderately acceptable. There were no significant differences in weight loss between the groups, but the CLI + MMA group showed an increase in restrained eating. Further large-scale studies are needed.
Trial Registration
Japanese University Hospital Medical Information Network (UMIN-ICDR). Clinical Trial identifier number UMIN000042626.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Increasing obesity rates are an international problem [1], including in Japan [2]. Obesity is a major cause of metabolic syndrome (MetS) [3]. Reducing obesity and improving MetS can improve hypertension, glucose intolerance, and dyslipidemia, and reduce the morbidity and mortality associated with cardiovascular diseases [4]. Aggressive lifestyle modification focused on weight loss and increased physical activity is the principal treatment for improving MetS [5]. Although intensive lifestyle interventions involving diet and exercise therapy are effective for people with obesity in the short term, maintaining long-term weight loss is difficult [6,7,8]. Different dysfunctional eating behaviors, such as binge eating, emotional eating, external eating, and eating in response to food cravings, have been linked to weight regain after successful weight loss [9]. This highlights the importance of investigating approaches to address associated psychological problems and potentially increase motivation and self-control among patients with obesity (e.g., to limit impulsive and inappropriate use of food) [10]. Psychological interventions, particularly behavioral and cognitive-behavioral strategies, have been reported to be beneficial for weight loss among adults with overweight and obesity, especially when combined with dietary and exercise strategies [11].
Mindfulness is a psychological process in which attention is paid to experiences that occur in the present moment. When developed through meditation and other disciplines, mindfulness can improve emotional control and reduce avoidant reactions to external and internal experiences [12]. Mindfulness-based interventions have been shown to have beneficial effects on weight loss and impaired eating behaviors, including improving the present-moment awareness of the sensory properties of food and reducing further food intake, and supporting decentering strategies that may help individuals resist desired foods [13]. Previous research suggested that mindfulness positively affected weight-related behaviors, such as reducing emotional and binge eating [9, 14,15,16,17,18,19], but had mixed effects on weight loss [14, 16,17,18, 20]. However, few studies have focused on evaluation at follow-up after an active intervention. A systematic review and meta-analysis found that a weight-loss approach involving mindfulness reduced overeating behavior and contributed to maintaining weight loss at follow-up [14]. A small-scale randomized controlled trial (RCT) showed that mindfulness combined with a standard behavioral weight loss program resulted in better weight loss, less overeating behavior, and better adherence to dietary restrictions at the 3-month follow-up after a 3-month active intervention compared with a standard behavioral weight loss program [21]. These studies suggested that mindfulness may be effective for maintaining long-term weight loss and healthy eating behavior after an active intervention.
Mindful eating (derived from mindfulness), when used to address unhealthy eating behavior, incorporates nonjudgmental awareness of physical and emotional sensations associated with eating [22]. Although research on mindful eating has been used in various ways, experimental studies are relatively limited, and it is not yet possible to conclude whether mindful eating strategies impact diet. However, some evidence suggests that certain mindful eating strategies may be promising, such as decentering and attention to the sensory properties of food [23]. A previous review showed that a mindful eating intervention reduced cravings and excess caloric intake and helped maintain continued weight loss [24].
Some studies have reported non-face-to-face weight loss interventions using mindfulness [25, 26]. One such study found that a telephone intervention using a mindfulness-based weight loss program did not improve weight loss compared with a standard weight loss program at the end of the intervention period and at the 6-month follow-up [25]. However, participants who used mindfulness in conjunction with the intervention showed decreased overeating behavior and improved mindful eating practices and mindfulness scale scores [25]. To date, the only published intervention study involving a mindfulness mobile application (MMA) for weight loss involved a general sample of students and reported a comparison with a behavioral self-monitoring electronic diary (e-diary) method [26]. Those results revealed no weight loss in the MMA group at follow-up, although improvements were observed in participants’ stress, eating behavior, mindfulness, and the frequency of mindful eating practices [26]. However, no intervention studies have examined changes in weight and eating behaviors when an MMA is used in addition to diet and exercise therapy. Mobile application-based interventions have been proposed as useful tools for weight loss [27, 28]. These interventions are portable and easy to practice anywhere [12], which may contribute to their potential role in MetS care [29]. Therefore, we aimed to explore the potential effectiveness and feasibility of using an MMA in conjunction with a comprehensive lifestyle intervention (CLI) focused on weight loss and eating behaviors, including at the post-intervention follow-up.
Methods
Study Design
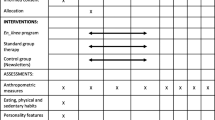
This open-label, parallel, pilot RCT included a 13-week CLI, which comprised a supportive workshop after a physical examination at a city general health center plus telephone counseling every 4 weeks for the following 13 weeks with and without MMA use. The application was provided to all participants, but the provision period was divided into two phases: 1–26 weeks and 27–52 weeks. We compared data between the two groups over 26 weeks. Participants were stratified by sex and randomly assigned to the two groups using a 1:1 ratio. After allocation, participants underwent baseline assessment, and those who did not meet the eligibility criteria were excluded from the analyses. The intervention was provided free of charge. This pilot trial was not designed to have sufficient statistical power to assess the effectiveness of the MMA intervention on weight loss and eating behavior.
Participants
Eligibility criteria were used to select adults aged 20–75 years with MetS, as defined by the International Diabetes Federation (IDF) [30] that had smartphones with mobile applications available. The exclusion criteria were a history of serious heart disease or other conditions that prohibited exercise therapy, severe depression, severe anxiety disorder, severe somatoform disorder, and psychotic symptoms. We recruited 1031 participants (663 females) by mail who met the eligibility criteria from among individuals who underwent physical examinations at a general healthcare center in Kasugai City, Japan. Participants were recruited from April 2020 to January 2021. Three evaluation sessions (baseline, week 13, and week 26) were conducted at the general healthcare center.
Randomization, Blinding, and Allocation Concealment
After orientation, participants who consented to participate in this study were randomly assigned to one of the two groups using the envelope method stratified by sex. The envelopes were opened in sequence in front of the participants. Because this was a pragmatic comparative study rather than a placebo-controlled trial, it was not possible to blind participants or the health workers providing the CLI. However, the risk for detection bias was minimized because all sessions were conducted independently, and the nutritionists and public health nurses in charge of the CLI were not involved in evaluating the results. The statistician always conducted outcome assessments in a separate room and was blinded to group allocation.
Interventions: CLI
The CLI involved a 1-h lesson once a week for 13 weeks from April to June 2021 and was performed with all participants together at designated times. The sessions comprised lectures by public health nurses and nutritionists, nutritional guidance, and lectures and exercise guidance by health exercise instructors. Nutritional guidance was based on the portion control method using the Healthy Plate approach [31], with a daily diet of 1200–1500 kcal plus dairy products and fruits, with a target of 50% carbohydrate, 25–30% protein, and 20–25% fat. The exercise instruction included open-eyed one-legged stands, heel lifts, squats, arm-leg crossing, push-ups, and sit-ups, with an increased load each time. Participants recorded their weight, exercise, meals, and snacks in a notebook each day. They were interviewed and given written feedback on their notebooks by public health nurses and nutritionists when they attended the sessions. As a state of emergency in response to COVID-19 was declared in Aichi Prefecture from May 12 to June 20, 2021 [32], six of the sessions scheduled during this time were canceled. Therefore, only six sessions were held. During the state of emergency, nutritionists and public health nurses called participants once a week to check on their condition. After completion of the active intervention, the nutritionists and public health nurses conducted telephone counseling every 4 weeks from July to September (weeks 14–26) to check whether participants were able to maintain the diet and exercise program and confirm that the MMA group was using the application. These healthcare workers provided instruction to participants based on the transtheoretical model of health behavior change [33].
Experimental Intervention: CLI + MMA
The CLI + MMA group performed the CLI and practiced mindfulness every day using the mobile application. Participants’ MMA use was checked and counseling provided by the nutritionists and public health nurses (who were not experienced in mindfulness practices) when they delivered sessions or telephone counseling. We used the MMA developed by the Relook unit of ARETECO HOLDINGS LTD (https://relook.jp/) for this study, which comprised a 26-week MMA program for weight loss. The present researchers were not involved in the creation of this program. The application was provided free of charge and participants downloaded the application onto their smartphones. Details of the mobile application content are shown in Table 1. The CLI + MMA intervention comprised an average of 453 s (306–889 s) each day, and the application included a reminder notice once-a-day. Participants initially practiced basic mindfulness breathing exercises following audio navigation in Japanese using the mobile application. After practicing mindfulness breathing, participants practiced ways to be mindful in various daily situations. The MMA was provided free of charge to the CLI group for 26 weeks after the evaluation was completed to ensure equality between the two groups.
Outcomes
Acceptability, Adherence, and Feasibility
These outcomes were measured by the number of people who refused to consent to the study after receiving orientation, the rate of adherence to the application (number of days application implementation was completed), follow-up rate, participant satisfaction, and number of adverse events. Data on patient adherence to the application were collected by ARETECO HOLDINGS LTD, which was performed automatically by the app and recorded every time a participant completed more than 90% of an application session. ARETECO HOLDINGS LTD provided the research team with a list of codes, which allowed the researchers to see a log of the actual time the application was used. Satisfaction was assessed at week 26, with reference to previous studies [25], to compare the satisfaction of participants in the two groups regarding their overall impression of the program using a 5-point Likert scale (1 = “very dissatisfied” to 5 = “very satisfied”). We also assessed participants’ willingness to recommend the program to friends, and whether the program helped them consume a healthy diet using a 5-point Likert scale (1 = “very negative” to 5 = “very positive”). We systematically tracked adverse events at each weekly session and followed monthly telephone counseling.
Assessment procedures
The primary, secondary, and exploratory outcomes were evaluated at weeks 0, 13, and 26.
Primary Outcome Measures
The primary outcome of using the MMA was the rate of change in body weight. Body weight was measured in units of 0.1 kg, while wearing test clothes.
Secondary Outcome Measures
Eating behavior.
The modified Japanese version of the Dutch Eating Behavior Questionnaire (DEBQ) was used to evaluate eating behavior. The DEBQ has three eating behavior subscales: restrained eating, emotional eating, and external eating [34]. The Japanese version of the DEBQ has been reviewed for reliability [35]. The 10-item restrained eating subscale assesses intentions and behaviors regarding restricting food intake because of weight concerns. The 13-item emotional eating subscale rates overeating behaviors triggered by negative emotions, such as anger, boredom, anxiety, and fear. The 10-item external eating subscale measures eating in response to food-related stimuli, such as the smell and taste of food, seeing other people eating, and seeing food being prepared. Participants responded to each item on a 5-point scale from “never” (1 point) to “always” (5 points). Higher scores indicated greater endorsement of that eating behavior.
Exploratory Outcome Measures
As exploratory outcome measures, we assessed body mass index (BMI), body fat percentage, abdominal circumference, body blood pressure, and blood test parameters (total cholesterol, high-density lipoprotein, low-density lipoprotein, triglyceride, fasting blood sugar, hemoglobin A1c, blood urea nitrogen, creatinine, cystatin C, estimated glomerular filtration rate), self-reported physical activity using the Japanese version of the International Physical Activity Questionnaire (short version) [36], and the Motivation to Live a Healthy Diet scale [37]. Because of the large amount of data collected, this paper only describes the results for body weight and eating behavior, as no association between the other items and the effects of mindfulness was shown.
Statistical Analysis
Statistical analyses were performed using SPSS version 27.0 (IBM Corporation, Armonk, NY, USA). After group allocation and before the intervention, one participant refused to participate in this study. Another participant was excluded because they did not meet the IDF criteria for MetS at the baseline assessment. Therefore, the modified intention-to-treat method was applied to investigate the treatment effects. Continuous variables measured at baseline were described using means and standard deviations and compared between treatment groups using two-sample t-tests. Categorical variables were described using frequencies and percentages, and comparisons between treatment groups were made using Fisher’s exact tests (two-sided). We used linear mixed models to analyze the effects of the intervention on body composition and DEBQ scores, including the endpoint of weight change. The model included fixed effects of group, time, and group-by-time interactions. The linear modeling analysis of participants who completed the MMA on at least 5 out of 7 days (per protocol) supported the results and the conclusions of the linear mixed modeling for the full sample. In this study, we only report the results of the linear mixed modeling for the full sample. It is considered more appropriate to use the standard deviation of the baseline values to reflect clinically meaningful differences based on the distribution of the population [38]. The effect size was calculated as the difference in mean changes at week 26 between the two groups, standardized to the pooled standard deviation of the baseline values. As an additional analysis, the rate of weight loss, changes in DEBQ score, and the frequency of application use were analyzed using Pearson’s product-moment correlation coefficients.
Results
Participant Flow: Screening and Study Acceptability
In total, 40 people attended the study orientation, of which 8 (20%) declined to participate in this study. The remaining 32 participants (80%) were randomly assigned to the study groups: 17 to the CLI + MMA group and 15 to the CLI group. One participant refused to participate in this study because of fear of infection with COVID-19 before the intervention started. Another participant did not meet the inclusion criteria for baseline measurements. These two participants were therefore excluded from the analyses, and background characteristics and results are reported for 30 participants. The enrollment, randomization, and retention processes are shown in Fig. 1.
Participants’ Characteristics
Differences between the two groups at baseline are shown in Table 2. Most participants (83%, n = 25) were female and the mean age was 69.3 ± 5.0 years. Baseline measurements for the two groups showed a significant difference in weight (p = 0.035), with mean weights of 61.7 ± 7.5 kg and 69.3 ± 11.0 kg in the CLI + MMA and CLI groups, respectively.
Acceptability, Adherence, and Feasibility
After 6 months of evaluation, data were available for all 30 participants (follow-up rate: 100%). No adverse events were observed. The application use logs revealed the application was used 4.4 ± 1.7 days per week on average; however, the number of days of application use decreased over time (Fig. 2). In the first week, the average number of days of application use was 6.63 ± 0.78, which decreased to 4.06 ± 2.56 in week 13, and 2.00 ± 2.34 in week 26. The number of participants who did not use the MMA by intervention week was 0 at week 1, but increased to two of 16 (17.5%) at week 13, and eight of 16 (50%) at week 26. Sixteen CLI + MMA participants (response rate = 100%) and 14 CLI participants (response rate = 100%) reported satisfaction with their participation in the 6-month survey. The CLI + MMA and CLI groups had similar mean program satisfaction ratings for overall impressions of the program (CLI + MMA: 3.4 ± 0.9; CLI: 3.5 ± 1.2), recommending the program to friends who wanted to lose weight (CLI + MMA: 3.4 ± 1.0; CLI: 3.5 ± 1.0), and helping them to eat healthily (CLI + MMA: 3.8 ± 0.7; CLI: 3.4 ± 0.9).
Weight Loss
Compared with baseline, the mean weight loss at week 26 was significantly reduced by 2.1 kg (standard error (SE) 0.6, p = 0.004; 3.2%, SE 0.9) in the CLI group and 2.3 kg (SE 0.2, p < 0.001; 3.7%, SE 0.4) in the CLI + MMA group. There was no significant group-by-time interaction between mindfulness use and weight loss (p = 0.924). These results are shown in Table 3 and Fig. 3.
DEBQ
Analysis of DEBQ results showed the restrained eating score significantly increased from 3.27 (SE 0.17) to 3.64 (SE 0.16) at week 26 in the CLI + MMA group (p = 0.010), but no change was observed in the CLI group (baseline: 3.54, SE 0.14; week 26: 3.42, SE 0.16). The group-by-time interaction was significant (p = 0.033) (Fig. 3B and Table 3). The DEBQ emotional eating score showed a decreasing trend in the CLI + MMA group from 1.96 (SE 0.19) to 1.79 (SE 0.15) at week 26, but the difference was not significant (p = 0.311). There was no change in emotional eating score in the CLI group (baseline: 2.10, SE 0.22; week 26: 2.02, SE 0.25) and no significant group-by-time interaction (p = 0.419). The external eating score showed a decreasing trend in the CLI + MMA group from 2.97 (SE 0.18) to 2.68 (SE 0.16) at week 26, but this difference was not significant (p = 0.098). No changes were observed in the CLI group (baseline: 2.84, SE 0.15; week 26: 2.87, SE 0.18) and the group-by-time interaction was not significant (p = 0.269) (Table 3).
Mechanisms/Moderators
We examined potential mechanisms for mindfulness treatment by correlating the change between baseline and follow-up at week 26 (follow-up score minus baseline score) for the rate of weight loss and restrained eating scores (Fig. 4A). Overall, an increase in restrained eating scores was correlated with higher rates of weight loss (Pearson’s correlation coefficient: 0.474; Fig. 4A), especially in the CLI + MMA group (Pearson’s correlation coefficient: 0.634; Fig. 4A, black dots) compared with the CLI group (Pearson’s correlation coefficient: 0.417; Fig. 4A, orange dots). We also investigated mindfulness engagement to test whether more engagement with the MMA was associated with more weight loss. In the CLI + MMA group, the number of days spent using the MMA was significantly and positively associated with increased weight loss (Pearson’s correlation coefficient: 0.598, p = 0.014; Fig. 4B).
Discussion
The present study showed the combination of CLI and MMA did not affect participants’ satisfaction with the program over 26 weeks. The high follow-up rate in this study allowed us to successfully track participants, but the rate of adherence to the MMA was low. No adverse events were observed. The preliminary results indicated that the MMA intervention did not result in greater weight loss at 6 months, but significantly increased restrained eating behavior compared with the CLI group. A positive relationship was found between the rate of weight loss and increased restrained eating scores. There was also a positive relationship between the rate of weight loss and frequency of using MMA. These results suggested the MMA was potentially effective for people with MetS.
Weight loss results did not significantly differ between the CLI + MMA and CLI groups at follow-up from the end of the CLI. Overall, both groups exhibited modest weight loss (3.5% of body weight, 2.2 kg on average). These effects on body weight were consistent with the results of previous meta-analyses, which reported small effect sizes for weight loss with mindfulness-based interventions [17,18,19]. A meta-analysis demonstrated moderate effects on weight loss with these interventions, but the level of evidence was limited because of methodological weaknesses and variability [20]. The present study was designed with the CLI group as the target group, and the results were similar to those of the most recent meta-analysis in that the interventions in both groups resulted in the same amount of weight loss [17]. Regarding the persistence of intervention effects on weight loss, weight regain after an active intervention is common, with around half of the lost weight being regained within 2 years [39]. Carriere et al. conducted a systematic review and meta-analysis that revealed a difference in weight at follow-up with and without the intervention [14]. However, there is variability in the timing of weight-related assessments among studies [40], and it is unclear when weight regain occurs. A small-scale RCT examining a mindfulness intervention reported weight gain in the CLI group after 12 weeks of follow-up [21]. However, in the present study, both the CLI + MMA and CLI groups exhibited no weight gain. This discrepancy could be attributed to differences in study methodology, as well as differences in the average age and ethnicity of the sample. In this study, we continued regular telephone-based counseling after the active intervention. Continued biweekly or monthly behavioral counseling after initial weight loss is known to be an effective approach for preventing weight regain [41]. Therefore, the follow-up period in our study might have been insufficient to assess the impact of the MMA itself on weight, meaning the results do not preclude the possibility that the MMA intervention may help weight loss. Further large-scale, long-term follow-up studies are needed to confirm our findings.
Regarding eating behavior, we found restrained eating behavior was significantly increased in the CLI + MMA group. Several meta-analyses reported that mindfulness improved binge eating behavior [9, 14,15,16,17,18,19]. Daubenmier et al. measured the effect of mindfulness using the DEBQ as an evaluation item [42], and revealed a small effect on restrained eating behavior, but large effects on emotional eating and external eating behavior [42]. In the present study, the effects on restrained and external eating behavior were large, and the effects on emotional eating behavior were small. Compared with the previous study, participants in our study reported healthier eating behaviors in their baseline assessment (our study: restrained eating 3.27, emotional eating 1.95, external eating 2.97; Daubenmier et al. [42]: restrained eating 2.79, emotional eating 3.42, external eating 3.57). In addition, participants in the present study were older and had a lower BMI than those in the previous study [42]. Further research is needed to elucidate this issue in more depth.
The MMA used in this study appeared to be feasible, as most participants with MetS found it acceptable and the loss to follow-up was small. However, the average adherence to the application declined over time. The overall average length of time the MMA was used each day was 453 s (range 306–889 s) (Fig. 2). Maintaining adherence is important in weight management [27], and our sensitivity analysis showed a correlation between adherence to the MMA and weight loss (Fig. 4B). A systematic review and meta-analysis of home practice in mindfulness-based cognitive therapy and mindfulness-based stress reduction showed the pooled estimate for participants’ home practice was 64% of the assigned amount, equating to about 30 min/day, 6 days/week [43]. Similarly, a systematic review of cancer survivors’ adherence to home mindfulness practice found the pooled adherence rate for participants’ home practice was 60% of the assigned amount (27 min/day during the intervention period), although survivors tended to practice less as time passed [44]. A possible reason for this difference in adherence is that adherence to an application partly depends on users’ characteristics [45]. Participants in our study may not have been aware of the importance of mindfulness. In addition, the healthcare workers who checked MMA adherence were not familiar with mindfulness, which might have made it difficult to follow the transtheoretical model of health behavior change [33]. This study also included participants that were older than expected. Application-based studies with older participants have used devices with easy-to-use touch screens of about 7 in. [46] or incorporating multiple alarm functions per day [46, 47]. Creative strategies to increase adherence to such applications should be considered in further studies to comprehensively evaluate the benefit of the MMA for individuals with MetS.
The strength of the present study was our finding that increased restrained eating behavior may be associated with weight loss during CLI. Restraint theory suggests that cognitive control of human eating behavior leads to reduced sensitivity to internal cues for satiety, which can result in disinhibited eating (i.e., overeating) in situations where cognitive control is undermined [48]. However, there is little experimental evidence from non-clinical samples that increased eating restraint is related to disinhibited eating or an increased cognitive bias for food [49]. When those who reported trying to lose weight via dieting were compared with those who were not dieting, the former group showed a reduced frequency of binge eating [50]. Another study found current ongoing dieters did not show activation in the prefrontal cortex and orbitofrontal cortex regions related to cognitive control [51]. It is possible that participants in the present study had lost weight because they were ongoing dieters during CLI. In this study, the correlation between weight and restrained eating was higher in the CLI + MMA group compared with the CLI group (Fig. 4A). Mindfulness decreases default mode network and frontoparietal network connectivity, and changes in medial prefrontal-amygdala connectivity are critically implicated in the regulation of emotion, which may be related to improved emotional regulation [52, 53]. Although there is a possibility of confounding bias from other factors that contribute to weight loss, our findings regarding the MMA warrant further research.
The present study also had several limitations that should be considered. As expected in a pilot feasibility study, the sample size was too small to draw definitive conclusions. Furthermore, 92% of the sample were women, which limited the generalizability of the findings to men. A third limitation was the choice of a control intervention. We compared a CLI group as the control group because of the feasibility of the study. Although this was a proprietary program in the public interest and not a scientifically proven effective program for weight loss, similar interventions throughout Japan have shown some effectiveness [54]. Fourth, the randomization was not successful as the control group was significantly heavier than the intervention group at baseline. Fifth, this study was conducted during the COVID-19 pandemic [32]. In addition to the fact that the planned interventions could not be implemented, the restrictions on daily life caused by COVID-19 measures also affected eating and physical activity [55], which could have influenced the outcomes in our study.
The present study showed that the MMA was highly feasible and moderately acceptable for use by people with MetS. The average duration of MMA use in the present study was 453 s (range 306–889 s) per day. This was a short duration compared with traditional mindfulness interventions, which typically involve face-to-face group exercises lasting 2–2.5 h per session [56]. We found the effects of the MMA included improved eating behavior, which suggested that this low-intensity application was effective for modifying some behaviors and attitudes related to problem eating behavior. Further large-scale studies are needed to confirm our results. We also found an association between adherence to the MMA and weight loss. This could be attributable to the characteristics of the application or the relationship between participants and the healthcare workers delivering the program. However, it was difficult to fully examine this important factor using the data collected in this study. Further studies focused on this aspect may inform development of more effective interventions.
Conclusion
This study is the first pilot RCT to examine the efficacy of MMA combined with diet and exercise therapy for MetS. This pilot study found that MMA with CLI was highly feasible and moderately acceptable, but low adherence to the application suggests that the intervention should include additional steps to improve engagement with the application. We found no difference in the effects on weight loss between the study groups, although use of the MMA might have contributed to an increase in restrained eating. Further large-scale studies building on this study are needed to demonstrate the effectiveness of MMA interventions.
Data Availability
The datasets generated and analyzed during the current study are not publicly available due to confidentiality but are available from the corresponding author on reasonable request.
References
Collaboration NCDRF. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387(10026):1377–96. https://doi.org/10.1016/S0140-6736(16)30054-X.
Funatogawa I, Funatogawa T, Nakao M, Karita K, Yano E. Changes in body mass index by birth cohort in Japanese adults: results from the National Nutrition Survey of Japan 1956–2005. Int J Epidemiol. 2009;38(1):83–92. https://doi.org/10.1093/ije/dyn182.
Muller MJ, Lagerpusch M, Enderle J, Schautz B, Heller M, Bosy-Westphal A. Beyond the body mass index: tracking body composition in the pathogenesis of obesity and the metabolic syndrome. Obes Rev. 2012;13(Suppl 2):6–13. https://doi.org/10.1111/j.1467-789X.2012.01033.x.
Eberly LE, Prineas R, Cohen JD, et al. Metabolic syndrome: risk factor distribution and 18-year mortality in the multiple risk factor intervention trial. Diabetes Care. 2006;29(1):123–30. https://doi.org/10.2337/diacare.29.1.123.
Bassi N, Karagodin I, Wang S, et al. Lifestyle modification for metabolic syndrome: a systematic review. Am J Med. 2014;127(12):1242 e1–10. https://doi.org/10.1016/j.amjmed.2014.06.035.
Butryn ML, Webb V, Wadden TA. Behavioral treatment of obesity. Psychiatr Clin North Am. 2011;34(4):841–59. https://doi.org/10.1016/j.psc.2011.08.006.
Look ARG. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity (Silver Spring). 2014;22(1):5–13. https://doi.org/10.1002/oby.20662.
Bray GA, Kim KK, Wilding JPH, World Obesity F. Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes Rev. 2017;18(7):715–23. https://doi.org/10.1111/obr.12551.
O’Reilly GA, Cook L, Spruijt-Metz D, Black DS. Mindfulness-based interventions for obesity-related eating behaviours: a literature review. Obes Rev. 2014;15(6):453–61. https://doi.org/10.1111/obr.12156.
Pellegrini M, Carletto S, Scumaci E, Ponzo V, Ostacoli L, Bo S. The use of self-help strategies in obesity treatment. a narrative review focused on hypnosis and mindfulness. Curr Obes Rep. 2021;10(3):351–64. https://doi.org/10.1007/s13679-021-00443-z.
Shaw K, O'Rourke P, Del Mar C, Kenardy J. Psychological interventions for overweight or obesity. Cochrane Database Syst Rev. 2005(2):CD003818. https://doi.org/10.1002/14651858.CD003818.pub2.
Creswell JD. Mindfulness interventions. Annu Rev Psychol. 2017;68:491–516. https://doi.org/10.1146/annurev-psych-042716-051139.
Tapper K. Can mindfulness influence weight management related eating behaviors? If so, how? Clin Psychol Rev. 2017;53:122–34. https://doi.org/10.1016/j.cpr.2017.03.003.
Carriere K, Khoury B, Gunak MM, Knauper B. Mindfulness-based interventions for weight loss: a systematic review and meta-analysis. Obes Rev. 2018;19(2):164–77. https://doi.org/10.1111/obr.12623.
Godfrey KM, Gallo LC, Afari N. Mindfulness-based interventions for binge eating: a systematic review and meta-analysis. J Behav Med. 2015;38(2):348–62. https://doi.org/10.1007/s10865-014-9610-5.
Katterman SN, Kleinman BM, Hood MM, Nackers LM, Corsica JA. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: a systematic review. Eat Behav. 2014;15(2):197–204. https://doi.org/10.1016/j.eatbeh.2014.01.005.
Daniela M, Robinson L, Gordon G, Werthmann J, Campbell IC, Schmidt U. The outcomes of mindfulness-based interventions for obesity and binge eating disorder: a meta-analysis of randomised controlled trials. Appetite. 2021;166:105464. https://doi.org/10.1016/j.appet.2021.105464.
Ruffault A, Czernichow S, Hagger MS, et al. The effects of mindfulness training on weight-loss and health-related behaviours in adults with overweight and obesity: a systematic review and meta-analysis. Obes Res Clin Pract. 2017;11(5 Suppl 1):90–111. https://doi.org/10.1016/j.orcp.2016.09.002.
Rogers JM, Ferrari M, Mosely K, Lang CP, Brennan L. Mindfulness-based interventions for adults who are overweight or obese: a meta-analysis of physical and psychological health outcomes. Obes Rev. 2017;18(1):51–67. https://doi.org/10.1111/obr.12461.
Olson KL, Emery CF. Mindfulness and weight loss: a systematic review. Psychosom Med. 2015;77(1):59–67. https://doi.org/10.1097/PSY.0000000000000127.
Spadaro KC, Davis KK, Sereika SM, Gibbs BB, Jakicic JM, Cohen SM. Effect of mindfulness meditation on short-term weight loss and eating behaviors in overweight and obese adults: a randomized controlled trial. J Complement Integr Med. 2017;15(2). https://doi.org/10.1515/jcim-2016-0048.
Framson C, Kristal AR, Schenk JM, Littman AJ, Zeliadt S, Benitez D. Development and validation of the mindful eating questionnaire. J Am Diet Assoc. 2009;109(8):1439–44. https://doi.org/10.1016/j.jada.2009.05.006.
Tapper K. Mindful eating: what we know so far. Nutr Bull. 2022;47(2):168–85. https://doi.org/10.1111/nbu.12559.
Dunn C, Haubenreiser M, Johnson M, et al. Mindfulness approaches and weight loss, weight maintenance, and weight regain. Curr Obes Rep. 2018;7(1):37–49. https://doi.org/10.1007/s13679-018-0299-6.
Carpenter KM, Vickerman KA, Salmon EE, Javitz HS, Epel ES, Lovejoy JC. A randomized pilot study of a phone-based mindfulness and weight loss program. Behav Med. 2019;45(4):271–81. https://doi.org/10.1080/08964289.2017.1384359.
Lyzwinski LN, Caffery L, Bambling M, Edirippulige S. The mindfulness app trial for weight, weight-related behaviors, and stress in university students: randomized controlled trial. JMIR Mhealth Uhealth. 2019;7(4):e12210. https://doi.org/10.2196/12210.
Ghelani DP, Moran LJ, Johnson C, Mousa A, Naderpoor N. Mobile apps for weight management: a review of the latest evidence to inform practice. Front Endocrinol. (Lausanne). 2020;11:412. https://doi.org/10.3389/fendo.2020.00412.
Flores Mateo G, Granado-Font E, Ferre-Grau C, Montana-Carreras X. Mobile phone apps to promote weight loss and increase physical activity: a systematic review and meta-analysis. J Med Internet Res. 2015;17(11):e253. https://doi.org/10.2196/jmir.4836.
Wong EML, Leung DYP, Tam HL, Wang Q, Yeung KW, Leung AYM. The effect of a lifestyle intervention program using a mobile application for adults with metabolic syndrome, versus the effect of a program using a booklet: a pilot randomized controlled trial. Clin Interv Aging. 2021;16:633–44. https://doi.org/10.2147/CIA.S303920.
Oda E. Metabolic syndrome: its history, mechanisms, and limitations. Acta Diabetol. 2012;49(2):89–95. https://doi.org/10.1007/s00592-011-0309-6.
Yamauchi K. Evidence-based lifestyle improvement, efficacy and practice of the Japanese portion control method (Healthy Plate) with behavioral therapy. J Japan Ass Diabet Informatics. 2016;14:56–62 (in Japanese).
Office for Novel Coronavirus Disease Control, Cabinet Secretariat, Government of Japan. Extension of the period for declaring a state of emergency for novel coronavirus infection. https://corona.go.jp/news/news_20200421_70.html. Accessed March 22, 2022. (in Japanese)
Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38–48. https://doi.org/10.4278/0890-1171-12.1.38.
Van Strien T, Frijters JE, Bergers GP, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int J Eat Disord. 1986;5(2):295–315.
Kato Y, Roth R. The difference of eating behavior between Austrian and Japanese university students. J Yasuda Women’s University. 2009;37:209–20 (in Japanese).
Murase N, Katsumura T, Ueda C, Inoue S, Shimomitsu T. Validity and reliability of Japanese version of International Physical Activity Questionnaire. J Health Welfare Stat. 2002;49(11):1–9 (in Japanese).
Kato Y, Nishida M, Tanaka Y, Kawabata T. The relationship between motivation for healthy eating and attitudes toward childhood eating habits among university students. Japanese J School Health. 2013;54(6):507–19 (in Japanese).
Morris SB. Estimating effect sizes from pretest-posttest-control group designs. Organ Res Methods. 2008;11(2):364–86.
Stelmach-Mardas M, Mardas M, Walkowiak J, Boeing H. Long-term weight status in regainers after weight loss by lifestyle intervention: status and challenges. Proc Nutr Soc. 2014;73(4):509–18. https://doi.org/10.1017/S0029665114000718.
Mason AE, Epel ES, Aschbacher K, et al. Reduced reward-driven eating accounts for the impact of a mindfulness-based diet and exercise intervention on weight loss: data from the SHINE randomized controlled trial. Appetite. 2016;100:86–93. https://doi.org/10.1016/j.appet.2016.02.009.
Alamuddin N, Bakizada Z, Wadden TA. Management of obesity. J Clin Oncol. 2016;34(35):4295–305. https://doi.org/10.1200/JCO.2016.66.8806.
Daubenmier J, Kristeller J, Hecht FM, et al. Mindfulness intervention for stress eating to reduce cortisol and abdominal fat among overweight and obese women: an exploratory randomized controlled study. J Obes. 2011;651936. https://doi.org/10.1155/2011/651936.
Parsons CE, Crane C, Parsons LJ, Fjorback LO, Kuyken W. Home practice in mindfulness-based cognitive therapy and mindfulness-based stress reduction: a systematic review and meta-analysis of participants’ mindfulness practice and its association with outcomes. Behav Res Ther. 2017;95:29–41. https://doi.org/10.1016/j.brat.2017.05.004.
Baydoun M, Moran C, McLennan A, Piedalue KL, Oberoi D, Carlson LE. Mindfulness-based interventions in cancer survivors: a systematic review of participants’ adherence to home practice. Patient Prefer Adherence. 2021;15:1225–42. https://doi.org/10.2147/PPA.S267064.
Zhao J, Freeman B, Li M. Can mobile phone apps influence people’s health behavior change? An evidence review. J Med Internet Res. 2016;18(11):e287. https://doi.org/10.2196/jmir.5692.
Mira JJ, Navarro I, Botella F, et al. A Spanish pillbox app for elderly patients taking multiple medications: randomized controlled trial. J Med Internet Res. 2014;16(4):e99. https://doi.org/10.2196/jmir.3269.
van Het Reve E, Silveira P, Daniel F, Casati F, de Bruin ED. Tablet-based strength-balance training to motivate and improve adherence to exercise in independently living older people: part 2 of a phase II preclinical exploratory trial. J Med Internet Res. 2014;16(6):e159. https://doi.org/10.2196/jmir.3055.
Herman CP, Mack D. Restrained and unrestrained eating. J Pers. 1975;43(4):647–60. https://doi.org/10.1111/j.1467-6494.1975.tb00727.x.
Watson P, Le Pelley ME. A meta-analysis of the relationship between eating restraint, impaired cognitive control and cognitive bias to food in non-clinical samples. Clin Psychol Rev. 2021;89:102082. https://doi.org/10.1016/j.cpr.2021.102082.
Lowe MR. Commentary on: What is restrained eating and how do we identify it?: unveiling the elephant in the room. Appetite. 2022;168:105221. https://doi.org/10.1016/j.appet.2021.105221.
Ely AV, Childress AR, Jagannathan K, Lowe MR. Differential reward response to palatable food cues in past and current dieters: a fMRI study. Obesity (Silver Spring). 2014;22(5):E38-45. https://doi.org/10.1002/oby.20599.
Sezer I, Pizzagalli DA, Sacchet MD. Resting-state fMRI functional connectivity and mindfulness in clinical and non-clinical contexts: a review and synthesis. Neurosci Biobehav Rev. 2022;135:104583. https://doi.org/10.1016/j.neubiorev.2022.104583.
Chumachenko SY, Cali RJ, Rosal MC, et al. Keeping weight off: mindfulness-based stress reduction alters amygdala functional connectivity during weight loss maintenance in a randomized control trial. PLoS One. 2021;16(1):e0244847. https://doi.org/10.1371/journal.pone.0244847.
Nakao YM, Miyamoto Y, Ueshima K, et al. Effectiveness of nationwide screening and lifestyle intervention for abdominal obesity and cardiometabolic risks in Japan: the metabolic syndrome and comprehensive lifestyle intervention study on nationwide database in Japan (MetS ACTION-J study). PLoS One. 2018;13(1):e0190862. https://doi.org/10.1371/journal.pone.0190862.
Deschasaux-Tanguy M, Druesne-Pecollo N, Esseddik Y, et al. Diet and physical activity during the coronavirus disease 2019 (COVID-19) lockdown (March-May 2020): results from the French NutriNet-Sante cohort study. Am J Clin Nutr. 2021;113(4):924–38. https://doi.org/10.1093/ajcn/nqaa336.
Mason AE, Epel ES, Kristeller J, et al. Effects of a mindfulness-based intervention on mindful eating, sweets consumption, and fasting glucose levels in obese adults: data from the SHINE randomized controlled trial. J Behav Med. 2016;39(2):201–13. https://doi.org/10.1007/s10865-015-9692-8.
Acknowledgements
The mindfulness mobile application was provided free of charge by Relook unit of ARETECO HOLDINGS LTD (Tokyo, Japan). We thank Benjamin Knight, MSc., and Audrey Holmes, MA, from Edanz (https://jp.edanz.com/ac) for editing drafts of this manuscript.
Funding
This work was supported by a JSPS KAKENHI Grant (Number JP19K19352). The funding body had no role in the design of the study, collection, analysis, and interpretation of the data, or in the writing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
The study protocol was approved by Nagoya University (approval number 2020–0617). All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in this study.
Statement Regarding the Welfare of Animals
Not applicable.
Conflict of Interest
The authors declare that they have no competing interests.
The mobile application for mindfulness used in this study was provided free of charge by Relook unit of ARETECO HOLDINGS LTD (Tokyo, Japan). ARETECO HOLDINGS LTD provided us with mindfulness technology and information owned solely by Relook unit of ARETECO HOLDINGS LTD. ARETECO HOLDINGS LTD did not intervene in any way in the design or preparation of the study protocol or the evaluation, including statistical analysis of the data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Matsuhisa, T., Fujie, R., Masukawa, R. et al. Impact of a Mindfulness Mobile Application on Weight Loss and Eating Behavior in People with Metabolic Syndrome: a Pilot Randomized Controlled Trial. Int.J. Behav. Med. 31, 202–214 (2024). https://doi.org/10.1007/s12529-023-10173-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-023-10173-2