Abstract
Background
High sedentary time (ST) and low physical activity may increase cardiovascular risk, potentially though cardiac-autonomic dysregulation. This study investigated associations of statistically exchanging device-measured ST and physical activity with measures of cardiac-autonomic regulation in previously pregnant women.
Method
This cross-sectional, secondary analysis included 286 women (age = 32.6 ± 5.7 years; 68% white) measured 7–15 years after delivery. ST and light (LPA), moderate (MPA), vigorous (VPA), and moderate-to-vigorous (MVPA) intensity physical activity were measured by ActiGraph GT3X. ST was further partitioned into long (≥ 30 min) and short (< 30 min) bouts. MVPA was also partitioned into long (≥ 10 min) and short (< 10 min) bouts. Cardiac-autonomic regulation was assessed by heart rate variability (HRV) (resting heart rate, natural log transformed standard deviation of normal R-R intervals [lnSDNN], natural log-transformed root mean square of successive differences [lnRMSSD]) from a 5-min seated ECG. Progressive isotemporal substitution models adjusted for confounders. Sensitivity analyses removed women with related underlying medical conditions and who did not meet respiration rate criteria.
Results
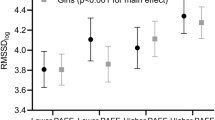
Initial analyses found no significant associations with HRV when exchanging 30 min of ST and physical activity (p > 0.05). Yet, replacing long- and short-bout ST with 30 min of long-bout MVPA yielded significantly higher (healthier) lnRMSSD (B = 0.063 ± 0.030 and B = 0.056 ± 0.027, respectively; both p < 0.05). Sensitivity analyses strengthened these associations and yielded further associations of higher lnSDNN and lnRMSSD when replacing 30 min of short-bout MVPA with equivalent amounts of long-bout MVPA (B = 0.074 ± 0.037 and B = 0.091 ± 0.046, respectively).
Conclusion
Replacing ST with long-bout MVPA is a potential strategy to improve cardiac-autonomic function in previously pregnant women.

Similar content being viewed by others
References
Hansen B, Kolle E, Dyrstad S, Holme I, Anderssen S. Accelerometer-determined physical activity in adults and older people. Medicine & Science in Sports & Exercise 2012;44(2):266–72.
Tremblay MS, Aubert S, Barnes JD, et al. Sedentary behavior research network (SBRN)–terminology consensus project process and outcome. Int J Behav Nutr Phys Act. 2017;14(1):75.
Dunstan DW, Thorp AA, Healy GN. Prolonged sitting: is it a distinct coronary heart disease risk factor? Curr Opin Cardiol. 2011;26(5):412–9.
Ekelund U, Steene-Johannessen J, Brown WJ, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. The Lancet. 2016;388(10051):1302–10.
Pandey A, Salahuddin U, Garg S, et al. Continuous dose-response association between sedentary time and risk for cardiovascular disease: a meta-analysis. JAMA cardiology. 2016;1(5):575–83.
Committee PAGA. 2018 Physical activity guidelines advisory committee scientific report.: US Department of Health and Human Services, 2018.
Canadian 24-Hour Movement Guidelines for Adults Aged 18–64: an integration of physical activity, sedentray behavior, and sleep. In: Physiology CSfE, ed. 2020;2.
Berntson GG, Thomas Bigger Jr J, Eckberg DL, et al. Heart rate variability: origins, methods, and interpretive caveats. Psychophysiology. 1997;34(6):623–48.
Fang S-C, Wu Y-L, Tsai P-S. Heart rate variability and risk of all-cause death and cardiovascular events in patients with cardiovascular disease: a meta-analysis of cohort studies. Biol Res Nurs. 2020;22(1):45–56.
Horiuchi M, Takiguchi C, Kirihara Y, Horiuchi Y. Impact of wearing graduated compression stockings on psychological and physiological responses during prolonged sitting. Int J Environ Res Public Health. 2018;15(8):1710.
Horiuchi M, Thijssen DH. Ischemic preconditioning prevents impact of prolonged sitting on glucose tolerance and markers of cardiovascular health, but not cerebrovascular responses. American J Physiol-Endocrinol Metabolism 2020.
dos Santos RR, Rosa EC, Rosa T, et al. Sedentary behavior: a key component in the interaction between an integrated lifestyle approach and cardiac autonomic function in active young men. Int J Environ Res Public Health. 2019;16(12):2156.
Dempsey PC, Matthews CE, Dashti SG, et al. Sedentary behavior and chronic disease: mechanisms and future directions. J Phys Act Health. 2020;17(1):52–61.
Oliveira C, Silveira EA, Rosa L, et al. Risk factors associated with cardiac autonomic modulation in obese individuals. J Obesity 2020;2020
Spina G, Gonze B, Barbosa A, Sperandio E, Dourado V. Presence of age-and sex-related differences in heart rate variability despite the maintenance of a suitable level of accelerometer-based physical activity. Brazilian J Medical and Biol Res 2019;52(8).
Niemelä M, Kiviniemi A, Kangas M, et al. Prolonged bouts of sedentary time and cardiac autonomic function in midlife. Translational Sports Medicine. 2019;2(6):341–50.
McGregor DE, Carson V, Palarea-Albaladejo J, Dall PM, Tremblay MS, Chastin SF. Compositional analysis of the associations between 24-h movement behaviours and health indicators among adults and older adults from the Canadian health measure survey. Int J Environ Res Public Health. 2018;15(8):1779.
Ryan DJ, Wullems JA, Stebbings GK, Morse CI, Stewart CE, Onambele-Pearson GL. Segregating the distinct effects of sedentary behavior and physical activity on older adults’ cardiovascular profile: part 2—isotemporal substitution approach. J Phys Act Health. 2018;15(7):537–42.
Alansare A, Alford K, Lee S, Church T, Jung HC. The effects of high-intensity interval training vs. moderate-intensity continuous training on heart rate variability in physically inactive adults. Int J environmental res public health 2018;15(7):1508.
Raffin J, Barthélémy J-C, Dupré C, et al. Exercise frequency determines heart rate variability gains in older people: a meta-analysis and meta-regression. Sports Med. 2019;49(5):719–29.
Grässler B, Thielmann B, Böckelmann I, Hökelmann A. Effects of different training interventions on heart rate variability and cardiovascular health and risk factors in young and middle-aged adults: a systematic review. Front physiol 2021;12
Rosenberger ME, Fulton JE, Buman MP, et al. The 24-hour activity cycle: a new paradigm for physical activity. Med Sci Sports Exerc. 2019;51(3):454.
Mekary RA, Willett WC, Hu FB, Ding EL. Isotemporal substitution paradigm for physical activity epidemiology and weight change. Am J Epidemiol. 2009;170(4):519–27.
Hallal PC, Andersen LB, Bull FC, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. The lancet. 2012;380(9838):247–57.
Gooding HC, Gidding SS, Moran AE, et al. Challenges and opportunities for the prevention and treatment of cardiovascular disease among young adults: report from a National Heart, Lung, and Blood Institute working group. J Am Heart Assoc 2020;9:e016115
Green AN, McGrath R, Martinez V, Taylor K, Paul DR, Vella CA. Associations of objectively measured sedentary behavior, light activity, and markers of cardiometabolic health in young women. Eur J Appl Physiol. 2014;114(5):907–19.
Chastin SF, De Craemer M, De Cocker K, et al. How does light-intensity physical activity associate with adult cardiometabolic health and mortality? Systematic review with meta-analysis of experimental and observational studies. Br J Sports Med. 2019;53(6):370–6.
Catov JM, Snyder GG, Bullen BL, Barinas-Mitchell EJ, Holzman C. Women with preterm birth have evidence of subclinical atherosclerosis a decade after delivery. J Womens Health. 2019;28(5):621–7.
Catov JM, Wu CS, Olsen J, Sutton-Tyrrell K, Li J, Nohr EA. Early or recurrent preterm birth and maternal cardiovascular disease risk. Ann Epidemiol. 2010;20(8):604–9.
Winship C, Radbill L. Sampling weights and regression analysis. Sociological Methods & Research. 1994;23(2):230–57.
Migueles JH, Cadenas-Sanchez C, Ekelund U, et al. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sports Med. 2017;47(9):1821–45.
Sasaki JE, John D, Freedson PS. Validation and comparison of ActiGraph activity monitors. J Sci Med Sport. 2011;14(5):411–6.
Matthews CE, Ainsworth BE, Thompson RW, Bassett DR Jr. Sources of variance in daily physical activity levels as measured by an accelerometer. Med Sci Sports Exerc. 2002;34(8):1376–81.
Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167(7):875–81.
Credeur DP, Miller SM, Jones R, et al. Impact of prolonged sitting on peripheral and central vascular health. Am J Cardiol. 2019;123(2):260–6.
Alansare AB, Kowalsky RJ, Jones MA, Perdomo SJ, Stoner L, Gibbs BB. The effects of a simulated workday of prolonged sitting on seated versus supine blood pressure and pulse wave velocity in adults with overweight/obesity and elevated blood pressure. J Vascular Res 2020;1–12.
Jakicic JM, Kraus WE, Powell KE, et al. Association between bout duration of physical activity and health: systematic review. Med Sci Sports Exerc. 2019;51(6):1213.
Tarvainen MP, Niskanen J-P, Lipponen JA, Ranta-Aho PO, Karjalainen PA. Kubios HRV–heart rate variability analysis software. Comput Methods Programs Biomed. 2014;113(1):210–20.
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 2003;42(6):1206–52.
de Geus EJ, Gianaros PJ, Brindle RC, Jennings JR, Berntson GG. Should heart rate variability be “corrected” for heart rate? Biological, quantitative, and interpretive considerations. Psychophysiology. 2019;56(2): e13287.
Kluttig A, Schumann B, Swenne CA, et al. Association of health behaviour with heart rate variability: a population-based study. BMC Cardiovasc Disord. 2010;10(1):1–11.
Laborde S, Mosley E, Thayer JF. Heart rate variability and cardiac vagal tone in psychophysiological research–recommendations for experiment planning, data analysis, and data reporting. Front Psychol. 2017;8:213.
Sandercock G, Bromley PD, Brodie DA. Effects of exercise on heart rate variability: inferences from meta-analysis. Med Sci Sports Exerc. 2005;37(3):433–9.
Reimers AK, Knapp G, Reimers C-D. Effects of exercise on the resting heart rate: a systematic review and meta-analysis of interventional studies. J Clin Med. 2018;7(12):503.
May R, McBerty V, Zaky A, Gianotti M. Vigorous physical activity predicts higher heart rate variability among younger adults. J Physiol Anthropol. 2017;36(1):1–5.
Alansare AB, Gibbs BB, Catov JM, et al. Association of physical activity and sedentary time with cardio-autonomic regulation in women. J Women's Health 2021.
Quinn TD, Kline CE, Nagle E, Radonovich LJ, Alansare A, Gibbs BB. Cardiovascular responses to physical activity during work and leisure. Occup Environ Med. 2022;79(2):94–101.
Pope ZC, Gabriel KP, Whitaker KM, et al. Association between objective activity intensity and heart rate variability: cardiovascular disease risk factor mediation (CARDIA). Med Sci Sports Exerc. 2020;52(6):1314–21.
Kiviniemi AM, Tulppo MP, Eskelinen JJ, et al. Cardiac autonomic function and high-intensity interval training in middle-age men. Med Sci Sports Exerc. 2014;46(10):1960–7.
Falconer CL, Page AS, Andrews RC, Cooper AR. The potential impact of displacing sedentary time in adults with type 2 diabetes. Med Sci Sports Exerc. 2015;47(10):2070.
Evenson KR, Herring AH, Wen F. Accelerometry-assessed latent class patterns of physical activity and sedentary behavior with mortality. Am J Prev Med. 2017;52(2):135–43.
Katzmarzyk PT, Powell KE, Jakicic JM, et al. Sedentary behavior and health: update from the 2018 physical activity guidelines advisory committee. Med Sci Sports Exerc. 2019;51(6):1227.
Routledge FS, Campbell TS, McFetridge-Durdle JA, Bacon SL. Improvements in heart rate variability with exercise therapy. Can J Cardiol. 2010;26(6):303–12.
Stanton AM, Handy AB, Meston CM. The effects of exercise on sexual function in women. Sexual medicine reviews. 2018;6(4):548–57.
Wang M, Zhou R, Xiong W, et al. Oxytocin mediated cardioprotection is independent of coronary endothelial function in rats. Peptides. 2020;130: 170333.
Stanley J, Peake JM, Buchheit M. Cardiac parasympathetic reactivation following exercise: implications for training prescription. Sports Med. 2013;43(12):1259–77.
Thosar SS, Johnson BD, Johnston JD, Wallace JP. Sitting and endothelial dysfunction: the role of shear stress. Medical science monitor: international medical j exp clin res 2012;18(12):RA173.
Howard BJ, Fraser SF, Sethi P, et al. Impact on hemostatic parameters of interrupting sitting with intermittent activity. Med Sci Sports Exerc. 2013;45(7):1285–91.
Koster A, Shiroma EJ, Caserotti P, et al. Comparison of sedentary estimates between activPAL and hip-and wrist-worn ActiGraph. Med Sci Sports Exerc. 2016;48(8):1514.
Acknowledgements
We would like to thank Samantha Bryan for her help in managing the data and providing guidance on analysis. The results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
Funding
This POUCHmoms Study was supported by the National Heart, Lung, and Blood Institute (R01-HL103825). The POUCH Study was supported by the Perinatal Epidemiological Research Initiative Program Grant from the March of Dimes Foundation (20FY01-38 and 20FY04-37), the Eunice Kennedy Shriver National Institute for Child Health and Human Development and the National Institute of Nursing Research (R01-HD34543), the Thrasher Research Foundation (02816–7), and the Centers for Disease Control and Prevention (U01-DP000143-01).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Alansare, A.B., Gibbs, B.B., Holzman, C. et al. Isotemporal Associations of Device-Measured Sedentary Time and Physical Activity with Cardiac-Autonomic Regulation in Previously Pregnant Women. Int.J. Behav. Med. 30, 497–508 (2023). https://doi.org/10.1007/s12529-022-10113-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-022-10113-6