Abstract
Background
Previous research suggests that socioeconomic status (SES) might be related to the course of quality of life (QoL) in coronary heart disease (CHD) patients. The authors sought to determine whether there are differences in the course of QoL before and after the incidence of CHD among older persons of differing SES.
Method
Two hundred two CHD patients were followed up longitudinally using a community-based survey. Data on patients’ QoL were collected before the diagnosis and at three follow-up assessments.
Results
High SES patients reported better outcomes at the premorbid assessment with fewer depressive feelings and better physical functioning. In physical functioning, similar results were repeated 6 and 12 months after the diagnosis. Additionally, high SES patients showed better role and social functioning 1 year after CHD. A multivariate analysis of variance revealed differential longitudinal pathways in relation to SES in role, social, and physical functioning.
Conclusion
CHD modulates premorbid differences in depressive feelings. Conversely, high SES leads to better outcomes in all functional domains in the long-term after diagnosis. Postmorbid differences in physical functioning are not directly related to CHD, but rather the reestablishment of a premorbid situation. In contrast, socioeconomic inequalities in social and role functioning are a direct response to the impact of the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Previous research has shown that there is an inverse association between socioeconomic status (SES) and the incidence and prevalence of coronary heart disease (CHD) [1, 2] and also between SES and mortality [3, 4]. Less is known about how SES affects patients’ quality of life (QoL) after diagnosis of CHD. Low QoL is a characteristic of aged people of low SES that is not completely explained by their health status [5]. Furthermore, the adverse consequences of CHD in older patients are particularly profound in specific domains of QoL. The impact of heart failure has been found to determine a greater decline in functional status in older patients when compared to a younger group [6]. A prospective study among older patients also showed that the impact of CHD has enduring negative consequences particularly for physical functioning, while its impact on social and psychological domains was significant but less pronounced [7]. In the present study, we build upon these results by examining a potential differential vulnerability effect of SES on the course of different domains of QoL after the emergence of CHD. That is, we evaluate whether older patients with low SES are worse off in terms of QoL once they develop CHD.
Previous research has suggested that low SES may be related to an unfavorable course in several health outcomes (e.g., perceived general health, long-term disability, mobility decline, social isolation, emotional reaction) [8, 9]. The extent to which patients experience these unfavorable outcomes is partly dependent upon the availability of psychosocial coping resources, such as social support and control [10–12]. This finding supports the notion that SES might be related to adverse QoL outcomes after the onset of CHD. Given that adjustment to CHD requires behavioral change, psychosocial resources might be very important in the response to CHD. It might be expected that CHD patients of low SES are more prone to decline in QoL once the disease has been established. Nevertheless, there are no clear indicators describing the impact of SES on QoL in the course of CHD.
In order to study adequately the impact of CHD on the course of QoL, it is important to take into account both the premorbid level of functioning and the multiple assessments after diagnosis. This is of particular relevance if we want to find out whether the differences in QoL due to SES are already present before the incidence of CHD or are a consequence of the disease.
This prospective study examines differences between patients of differing SES in relation to QoL at various assessment points, including a premorbid assessment. We analyze longitudinal changes reported in QoL from the premorbid assessment until 1 year after diagnosis, comparing the course of adaptation in two groups of patients with low and high SES. The emergence of CHD is associated with a greater impairment in functional status, particularly physical functioning [7], than in other QoL domains (such as psychological distress). We, therefore, predict that SES will have a specific impact on functional status up to 1 year after CHD diagnosis. Furthermore, on the basis of indications found in the literature, we expect that patients with high SES will report better outcomes in response to CHD, principally in physical functioning.
Method
Design
This study is part of the Groningen Longitudinal Aging Study (GLAS), a population-based prospective follow-up study of the determinants of health-related QoL of older people [13]. Available data for the present study have been collected and organized since 1993 (T0). A total of 5,279 persons, aged 57 years and older, were recruited to participate in the baseline assessment. These participants were monitored for selected diseases by their general practitioners between 1993 and 1998. After CHD emerged, the patients received a letter from the research team asking them to participate in the follow-up study, covering three follow-up assessments at 2, 6, and 12 months (T1, T2, and T3). This study was approved by the Medical Ethical Committee of the University Medical Center of Groningen.
Sample
Data for two types of CHD were collected: acute myocardial infarction and congestive heart failure, according to the criteria of the International Classification of Primary Care [14].
Four hundred ninety-four patients with a new episode of acute myocardial infarction or congestive heart failure after the baseline were recruited. Two hundred two patients who completed all follow-up assessments were included in the present study. Figure 1 shows the flowchart of the cases after the baseline assessment. Participants were compared with nonparticipants (patients who dropped out, died, or could not participate to all the assessments for other reasons) at the premorbid stage for sociodemographic characteristics and QoL. The two groups did not significantly differ in most of the measurements (gender, depressive feelings, anxiety, and role and physical functioning), except for the fact that participants were significantly younger (on average, 71.9 versus 74.7 years; F = 15.1, p < 0.001) and reported higher levels of social functioning (on average, 74.8 versus 68.5; F = 5.5, p < 0.05).
Measures
Data at all assessment points were collected through semistructured interviews and by means of self-report questionnaires.
Socioeconomic Status
A weighted sum index combining three major indicators of SES, namely, educational level, income, and occupational prestige, was created at the baseline for the entire GLAS sample.
Educational level is the highest level of education attained by the patients with scores ranging from 1 (elementary school not completed) to 6 (higher education, second phase). The level of education for the respondents is based on the International Standard Classification of Education [15].
The income of the respondents was measured by asking them their net monthly household income. For respondents who were married or living with a partner, the monthly after-tax income for both the respondent and the partner was recorded. This household income was converted to an individual income (six equivalent categories) on a scale ranging from category 1, up to 522 euros per month, to category 6, 795 euros per month or higher.
Occupational prestige was derived by coding the last profession of the respondent according to the classification of the Dutch Central Bureau for Statistics [16]. These nominal codes correspond with the International Standard Classification of Occupations [17]. The occupational codes were converted into prestige scores with an interval level of measurement from 0 to 100 [18]. This scale was developed in The Netherlands on the basis of 116 occupations classified by a random sampling of 500 persons. According to Dahl [19], using the occupation of the male partner for married, divorced, or widowed women provides the best results when researching health among older women, even compared to their own occupational score. Therefore, we used the information of the male partners for female participants who were living with their partners, widowed, or divorced.
To compute an overall index, the scores on all three indicators of SES were transformed into standardized Z scores. We performed an unrotated factor analysis to determine whether the three indicators all loaded on one factor, which turned out to be the case. The factor loadings of the three variables were high and comparable: educational level (0.82), income (0.76), and occupational prestige (0.77). We then multiplied the score for each variable with its factor loading and summed them up to a weighted index for SES. Missing data for income (N = 26) and occupational prestige (N = 14) were replaced by using the mean standardized income score or the mean standardized occupational prestige score calculated for participants with the corresponding value in educational level. The new variable, ranging from −4.36 to 4.64, was finally recoded into low and high SES using the median score of the index as the cut-off point (−0.047). Classification in two categories was preferred over classification in three categories in order to increase power. A closer inspection of the two SES groups on the basis of their composite scores revealed the following composition of the sample. Of the patients in the low SES group, 90% had a lower education (from elementary school to vocational education, lower level), 65% had a small income (less than 658 euros per month), and 91% had low professional prestige (below 50 on the Sixma and Ultee scale). Conversely, 69% of those in the high SES group had a high educational level (from advanced education, higher level to higher education, second phase), 91% had a high income (more than 658 euros per month), and 61% had high job prestige (scoring more than 50 on the Sixma and Ultee scale).
Covariates
Gender, age, and severity of the disease were related to cardiac disease outcome in the present data and in previous research [10, 20]. Disease severity was assessed according to the New York Heart Association (NYHA) classification at the first follow-up assessment [21]. The NYHA classification indicates the severity of cardiac symptoms by the level of complaints of breathlessness in relation to physical activities. It ranges from I (mild symptoms) to IV (severe symptoms).
Outcome Measures
Five indicators representing the three domains of QoL (psychological, physical, and social) were used at both baseline and follow-up assessments.
Depressive feelings and anxiety were assessed with the two subscales of the Hospital Anxiety and Depression Scale (HADS) [22]. Both the anxiety (Cronbach’s α = 0.83 at baseline) and depressive feelings (Cronbach’s α = 0.71 at baseline) subscales were composed of seven items varying from 0 to 21 (higher scores indicating more symptoms). HADS has been validated for an older Dutch population [23].
The participants’ social functioning, role functioning, and physical functioning were quantified using three subscales of the Medical Outcomes Study Short Form 20 (MOS SF-20) [24]. The social functioning subscale measures the extent to which health interferes with normal social activities such as having contacts and visiting friends (one item). The role functioning subscale measures the extent to which health interferes with usual daily activities such as housework or the professional job (two items, Cronbach’s α = 0.87 at baseline). The physical functioning subscale provides a global indication for physical limitations such as walking uphill or eating and dressing (six items, Cronbach’s α = 0.79 at baseline). All three subscales range from 0 to 100 and higher scores indicate better functioning. The psychometric properties of the Dutch version of the MOS were approved in a previous study [25].
Statistical Analysis
In order to examine the relationship between SES and psychological distress, as well as role, social, and physical functioning at different assessment points, mean values of the considered variables were compared between the two socioeconomic groups using a one-way analysis of variance (one-way ANOVA) with SES as an independent factor. A multivariate analysis of variance (MANOVA) investigated the similarities or differences between the paths of adaptation of the two levels of SES. All the results were controlled for covariates. All analyses were performed using SPSS version 14.0.
Results
Characteristics of the Patients
In Table 1, the characteristics of the sample are presented. The sample is almost equally distributed in terms of gender and SES with an average age of 72 years (the age of the present sample ranges between 58 and 96 years). The severity of the disease 2 months after diagnosis is assessed for the whole sample around class 2, which means that patients have CHD resulting in slight limitation of activity. A closer inspection of the two SES groups shows a different composition with respect to gender: patients with low SES are predominantly women, while the high SES group is mostly composed of men. Furthermore, patients with low SES are slightly older and their cardiac symptoms are severer than for the patients with high SES.
Differences Between High and Low SES
Table 2 shows the mean levels of psychological distress and social, role, and physical functioning at the different assessment points for the two SES groups separately. Cross-sectional differences for the two SES groups are noticeable for depressive feelings (T0), role (T3), social (T3), and physical functioning (T0, T2, and T3). Thus, inequalities between patients of high and low SES in physical functioning in the short- and long-term after diagnosis were already present at the baseline. In contrast, disparities between high and low SES in role and social functioning are only significant 1 year after diagnosis and appear to be the result of a different response to the disease. Finally, premorbid differences in depressive feelings between the SES groups disappeared after the emergence of the CHD.
Difference in the Course of Adaptation Between High and Low SES
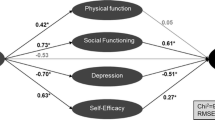
In Fig. 2, the results of MANOVA are presented, revealing differences in the way the two groups responded over time. Whereas for psychological domains we did not find substantial divergences in the way the two SES groups responded to CHD, we did find a difference in relation to patients’ functioning. High and low SES patients differ in terms of their trajectories of change over time in regard to role (p < 0.05), social (p < 0.05), and particularly physical (p < 0.001) functioning.
Difference in the course of adaptation between socioeconomic groups. T0 baseline premorbid measurement, T1 2 months after the diagnosis, T2 6 months after the diagnosis, T3 12 months after the diagnosis. MANOVA: *p < 0.05; **p < 0.00. Results have been adjusted for age, gender, and severity of the disease (NYHA class). Higher scores indicate better functioning except for depressive feelings and anxiety
Discussion
The results of this prospective study show that differences between socioeconomic groups are present at different time periods, prediagnosis and postdiagnosis, in five domains of QoL. In all cases, high SES was associated with more favorable outcomes than low SES. Furthermore, after diagnosis, CHD patients with high SES exhibit higher levels of social functioning, role functioning, and physical functioning than patients with low SES. Differences in social and role functioning may result from a differentiated response to the disease, while differences in physical functioning could be related to the premorbid situation. Confirming our expectations, high SES predicts better outcomes in the functional domains of QoL up to 1 year after the diagnosis of CHD. Differences in psychological distress were limited to depressive feelings at the premorbid measurement, therefore, unrelated to CHD.
The novel aspect of our research is the inclusion of patients’ premorbid data. This approach allowed us to investigate the specific mechanisms of the process of adjustment to CHD, which otherwise would have remained undiscovered, leading to potentially erroneous interpretations.
A possible limitation of the study is the high level of subject attrition because we selected only those patients who replied through the four assessments. Patients with poorer health may have dropped out of the study, biasing our sample toward CHD patients with milder disease or lower anxiety and depression. That might also explain the paucity of differences between socioeconomic groups in the psychological domains. The participants in our study might have responded more quickly and actively to the condition, enhancing their chances of survival. As we illustrated in the methodological section, the study participants were younger and socially more active than nonparticipants.
In order to accurately describe the clinical profile of the patients, additional biomedical data should be incorporated in this study. For instance, the left ventricular ejection fraction (LVEF) is a sensitive measure of disease severity which can be employed complementarily to the NYHA. LVEF represents the fraction of blood pumped out of the left ventricle during each heartbeat, which is substantially limited in CHD patients. Because in the present dataset information on disease severity were only gathered through the NYHA classification, further studies on QoL in CHD, including records of patients’ LVEF and other clinical variables, would be recommendable.
Another limitation may have been the varying time intervals between baseline assessment and diagnosis in our sample, which ranged from 1 to 58 months. If patients of one socioeconomic group were registered for a diagnosis of CHD a long time after the first interview, they could report more changes in QoL compared to the others who entered the study shortly after the baseline. However, we calculated and compared the mean time between baseline and diagnosis for both socioeconomic groups and found no statistically significant difference between them (26 months for the low SES and 28 months for the high one). Additionally, we checked the correlations between the time elapsed since the diagnosis and the outcome variables after the diagnosis. There were no significant correlations with the outcome variables of interest. Therefore, we do not consider such a time factor to be a confounder in the present study.
Status inconsistency (i.e., discrepancies between the three indicators of SES) is associated with CHD and might have obscured results showing socioeconomic disparities in psychological domains [26]. However, educational level, job prestige, and income are moderately correlated with each other (r values between 0.37 and 0.42, all p < 0.001). In addition, the factor loadings of the three indicators were similar, indicating that they contribute to SES in a similar way. In other words, although we cannot exclude the presence of status inconsistency, such a phenomenon should be of limited importance in the present study.
Similarly to status inconsistency, downward mobility (i.e., decrease in SES over time) is associated with health problems and incidence of CHD and might represent a possible bias in our study. Because SES was only measured at the premorbid assessment, we could not gauge downward mobility in the present research. However, considering that the mean age of the sample was 72 years (the youngest patient was 57 years old), implying that most of the participants were already retired, it is quite unlikely that such patients would have experienced a collapse in their career or retirement funds at this specific moment of their life. For these reasons, we exclude downward mobility as a possible limitation of the study.
Our results indicate that cross-sectional differences between SES after the onset of CHD are regulated by distinct mechanisms. Interestingly, the significant differences in depressive feelings between SES groups observed at prediagnosis (patients with low SES reported higher depressive feelings) disappeared after the emergence of the CHD and did not reappear throughout the study. The emergence of the disease appeared to modulate differences that were previously present between SES groups.
We observed differences in physical functioning 6 and 12 months after CHD diagnosis but, crucially, this difference existed premorbidly. This finding may be important for understanding the impact of CHD on physical functioning, especially in research which does not include premorbid measures. In the present study, we found that differences in physical functioning are not a direct consequence of CHD but rather the reestablishment of a premorbid situation. On the other hand, socioeconomic inequalities in social and role functioning only emerged 1 year after the diagnosis. In this case, the observed differences represent a differential response to the impact of the disease.
A few recommendations can be derived from the results of this study. The research on social inequalities in health among aged people is still scarce, while it should be of primary concern considering the substantial impact of this age group on health care use [27]. More investments are needed to alleviate the unfavorable situation of disadvantaged groups on specific aspects of QoL, ensuring that health care services respond appropriately and promptly to the needs of different socioeconomic groups. Moreover, this study suggests that interventions for older patients with low SES should be primarily focused on domains such as role and social activities where differences according to SES are a direct consequence of CHD. More generally, the physical domain should be of particular clinical concern as well due to the fact that socioeconomic differences in physical functioning are already present at the premorbid stage and remain substantial after the onset of the disease.
Two main issues which could not be directly addressed in the present research should be integrated into future studies. First, more light should be shed on the role of psychological resources (such as control beliefs) in the explanation of socioeconomic differences in adaptation to CHD in old age [10]. A higher risk of heart disease, associated with persons of low SES, is better explained by differences in control beliefs than by the classical coronary risk factors (e.g., smoking, hypertension) [28]. One may wonder whether psychological resources could help to explain the differences in outcomes of QoL after the onset of CHD for different socioeconomic groups. Secondly, it would be useful to expand our approach to include research on other conditions, in order to determine which outcomes are disease-specific and which represent a more general response to the onset of diseases.
References
Marmot MG, Smith GD, Stansfeld S, Patel C, North F, Head J, et al. Health inequalities among British civil-servants: the Whitehall II study. Lancet 1991;337:1387–93.
Nordstrom CK, Roux AVD, Sharon AJB, Gardin JM. The association of personal and neighborhood socioeconomic indicators with subclinical cardiovascular disease in an elderly cohort. The cardiovascular health study. Soc Sci Med 2004;59:2139–47.
Bernheim SM, Spertus JA, Reid KJ, Bradley EH, Desai RA, Peterson ED, et al. Socioeconomic disparities in outcomes after acute myocardial infarction. Am Heart J 2007;153:313–9.
Mackenbach JP, Cavelaars AEJM, Kunst AE, Groenhof F. Socioeconomic inequalities in cardiovascular disease mortality: an international study. Eur Heart J 2000;21:1141–51.
Breeze E, Jones DA, Wilkinson P, Bulpitt CJ, Grundy C, Latif AM, et al. Area deprivation, social class, and quality of life among people aged 75 years and over in Britain. Int J Epidemiol 2005;34:276–83.
Masoudi FA, Rumsfeld JS, Havranek EP, House JA, Peterson ED, Krumholz HM, et al. Age, functional capacity, and health-related quality of life in patients with heart failure. J Card Fail 2004;10:368–73.
van Jaarsveld CHM, Ranchor AV, Sanderman R, Ormel J, Kempen GIJM. The role of premorbid psychological attributes in short- and long-term adjustment after cardiac disease. A prospective study in the elderly in The Netherlands. Soc Sci Med 2005;60:1035–45.
Koster A, Bosma H, Kempen GIJM, van Lenthe FJ, van Eijk JTM, Mackenbach JP. Socioeconomic inequalities in mobility decline in chronic disease groups (asthma/COPD, heart disease, diabetes mellitus, low back pain): only a minor role for disease severity and comorbidity. J Epidemiol Community Health 2004;58:862–9.
van der Meer JBW, Mackenbach JP. Course of health status among chronically ill persons: differentials according to level of education. J Clin Epidemiol 1998;51:171–9.
Barbareschi G, Sanderman R, Kempen GIJM, Ranchor AV. The mediating role of perceived control on the relationship between socioeconomic status and functional changes in older patients with coronary heart disease. J Gerontol B Psychol Sci Soc Sci 2008;63:353–361.
Gallo LC, Bogart LM, Vranceanu AM, Matthews KA. Socioeconomic status, resources, psychological experiences, and emotional responses: a test of the reserve capacity model. J Pers Soc Psychol 2005;88:386–99.
Mickelson KD, Kubzansky LD. Social distribution of social support: the mediating role of life events. Am J Community Psychol 2003;32:265–81.
Kempen GIJM, Ormel J, Brilman EI, Relyveld J. Adaptive responses among Dutch elderly: the impact of eight chronic medical conditions on health-related quality of life. Am J Public Health 1997;87:38–44.
Lamberts H, Wood M. International classification of primary care. Oxford: Oxford University Press; 1987.
UNESCO. International Standard Classification of Education (ISCED). Paris: ISCED; 1976.
Centraal Bureau voor de Statistiek. Beroepenclassificatie 1984 [Job classification 1984]. Voorburg: CBS; 1984.
International Labor Office. International Standard Classification of Occupations: ISCO-88. International Labor Office: Geneva; 1990.
Sixma H, Ultee W. An occupational prestige scale for the Netherlands in the eighties. In: Bakker BFM, Dronkers J, Ganzeboom HBG, editors. Social stratification and mobility in the Netherlands. A collection of recent contributions to the study of social inequality in a modern Western society: data, trends, and comparisons. Amsterdam: SISWO-publication 291; 1984.
Dahl E. Inequality in health and the class position of women: the Norwegian experience. Sociol Health Illn 1991;13:492–505.
van Jaarsveld CHM, Sanderman R, Miedema I, Ranchor AV, Kempen GIJM. Changes in health-related quality of life in older patients with acute myocardial infarction or congestive heart failure: a prospective study. J Am Geriatr Soc 2001;49:1052–8.
New York heart Association. The criteria committee of the New York Heart Association. In disease of the heart and blood vessels; nomenclature and criteria for diagnosis. Boston: Little Brown; 1964.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70.
Spinhoven P, Ormel J, Sloekers PPA, Kempen GIJM, Speckens AEM, van Hemert AM. A validation study of the hospital anxiety and depression scale (HADS) in different groups of Dutch subjects. Psychol Med 1997;27:363–70.
Stewart AL, Hays RD, Ware JE. The Mos short-form general health survey: reliability and validity in a patient population. Med Care 1988;26:724–32.
Kempen GIJM. Het meten van de gezondheidstoestand van ouderen; een toepassing van een Nederlandse versie van de MOS-schaal [The assessment of the health status of elderly; a Dutch version of the MOS scale]. Tijdschr Gerontol Geriatr 1992;23:132–40.
Peter R, Gassler H, Geyer S. Socioeconomic status, status inconsistency and risk of ischaemic heart disease: a prospective study among members of a statutory health insurance company. J Epidemiol Community Health 2007;61:605–11.
Artazcoz L, Rueda S. Social inequalities in health among the elderly: a challenge for public health research. J Epidemiol Community Health 2007;61:466–7.
Bosma H, van Jaarsveld CHM, Tuinstra J, Sanderman R, Ranchor AV, van Eijk JTM, et al. Low control beliefs, classical coronary risk factors, and socioeconomic differences in heart disease in older persons. Soc Sci Med 2005;60:737–45.
Acknowledgments
The research reported was part of GLAS. GLAS and its substudies are financially supported by the Dutch government (through NESTOR), the University of Groningen, the Faculty of Medical Sciences in Groningen, the Dutch Cancer Society (KWF Kankerbestrijding), and the Netherlands Organisation for Scientific Research (NWO). We thank Dr. Ellen van Jaarsveld for her contribution during the construction of the database. We thank Dr. Tim Fawcett, Dr. Kristin Mc Gee, and Dr. Juliet Foster for their comments on the text.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Barbareschi, G., Sanderman, R., Kempen, G.I.J.M. et al. Socioeconomic Status and the Course of Quality of Life in Older Patients with Coronary Heart Disease. Int.J. Behav. Med. 16, 197–204 (2009). https://doi.org/10.1007/s12529-008-9010-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-008-9010-8