Abstract
Background
Surgery plays an important role in the treatment of neuroblastoma. Perioperative complications may impact the course of neuroblastoma treatment. To date, comprehensive analyses of complications and risk factors have been lacking.
Methods
Patients with retroperitoneal neuroblastoma undergoing tumor resection were retrospectively analyzed between 2014 and 2021. The data collected included clinical characteristics, operative details, operative complications and postoperative outcomes. Risk factors for perioperative complications of retroperitoneal neuroblastoma were analyzed.
Results
A total of 571 patients were enrolled in this study. Perioperative complications were observed in 255 (44.7%) patients. Lymphatic leakage (28.4%), diarrhea (13.5%), and injury (vascular, nerve and organ; 7.5%) were the most frequent complications. There were three operation-related deaths (0.53%): massive hemorrhage (n = 1), biliary tract perforation (n = 1) and intestinal necrosis (n = 1). The presence of image-defined risk factors (IDRFs) [odds ratio (OR) = 2.09, P < 0.01], high stage of the International Neuroblastoma Risk Group staging system (INRGSS) (OR = 0.454, P = 0.04), retroperitoneal lymph node metastasis (OR = 2.433, P = 0.026), superior mesenteric artery encasement (OR = 3.346, P = 0.003), and inferior mesenteric artery encasement (OR = 2.218, P = 0.019) were identified as independent risk factors for perioperative complications.
Conclusions
Despite the high incidence of perioperative complications, the associated mortality rate was quite low. Perioperative complications of retroperitoneal neuroblastoma were associated with IDRFs, INRGSS, retroperitoneal lymph node metastasis and vascular encasement. Patients with high-risk factors should receive more serious attention during surgery but should not discourage the determination to pursue total resection of neuroblastoma.
Video Abstract (MP4 94289 KB)
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroblastoma (NB) is the most common extracranial solid tumor in childhood and is responsible for 15% of all pediatric oncology deaths [1]. High-risk NB still has a poor prognosis, with a 50%–60% 5-year event-free survival rate [2]. A report from the International Society of Pediatric Oncology Europe Neuroblastoma Group High-Risk Neuroblastoma 1 study showed improved event-free and overall survival associated with complete macroscopic excision [3]. NB most commonly develops in the posterior peritoneal region, and the adrenal gland is the most frequent origin [4]. Complete resection of retroperitoneal NB is clearly difficult to achieve when extensive lymph node metastasis and vascular encasement are present. Since Kiely first came up with the technique of dissection in the subadventitial plane, the total resection rate of tumors has been remarkably improved [5, 6].
Pediatric surgeons strive for gross total resection (GTR), but there is a scarcity of data with respect to complications associated with operations for retroperitoneal NB. According to the reports that have been published thus far, lymphatic leakage (LL) and diarrhea are common complications after NB resection, and major vascular injury may lead to serious consequences [7, 8]. The presence of image-defined risk factors (IDRFs) at resection was associated with a greater incidence of intraoperative complications [9, 10]. However, large sample sizes, comprehensive analyses of all complications and risk factor assessments were absent from these studies.
The aim of this study was to determine the incidence of all perioperative complications in patients undergoing retroperitoneal NB resection and identify risk factors associated with significant complications.
Methods
Patients
A total of 594 patients underwent retroperitoneal NB tumor resection from January 2014 to December 2021 in our center, of whom 571 were enrolled in this study and fulfilled the following eligibility criteria: (1) primary retroperitoneal NB; and (2) tumor resection was performed instead of tumor biopsy. Twenty-three cases were excluded due to dysfunction of vital organs and major illnesses such as heart or brain disease (Fig. 1). Informed consent to participate in the study was obtained from participants (or their parent or legal guardian in the case of children under 16).
All patients underwent enhanced computed tomography and vascular three-dimensional reconstruction to determine the presence of IDRFs before the operation. NB was diagnosed in either of the following ways: (1) unequivocal pathologic diagnosis by tumor resection or biopsy; and (2) bone marrow aspirate or trephine biopsy contains unequivocal tumor cells.
Surgery
Localized NB in stage L1 could be operated on by a minimally invasive approach, while laparotomy surgery was recommended for tumors with IDRFs. Chemotherapy should be administered to lower the IDRFs if it is present before surgery. Tumor excision was attempted after 2–4 cycles of chemotherapy if necessary, depending on the response. All procedures were performed by the same group of surgeons, all of whom were senior pediatric oncology surgeons with more than 10 years of practice. The detailed protocol, including inductive chemotherapy, surgery and consolidation therapy, of each International Neuroblastoma Risk Group (INRG) was based on the CCCG-NB-2015 Regimen [11].
Removal of all macroscopic tumors, including metastatic lymph nodes and suspicious lesions on imaging, was defined as GTR, and incomplete tumor removal (residual macroscopic tumor, tumor removal less than 90%) was defined as partial resection (PR). The basic principles of surgical resection include the accurate and safe display of vital vascular anatomy with optimal exposure of the tumor to achieve GTR as much as possible while avoiding unnecessary organ removal.
Outcomes
The primary outcome was the occurrence of direct, common and major complications, including hemorrhage (20 mL/kg or more), vascular injury, unplanned organ resection, secondary hypertension, LL, diarrhea, important structural injury, and any organ failure. The secondary outcome measured included individual complications (minor complications), including wound complications, abdominal infection, intestinal obstruction, and hypoglycemia.
LL was defined as (1) the milky-white drain fluid lasted up to 48 hours; (2) the drain output was more than 100 mL/day and did not decrease 48 hours after the operation; and (3) the triglyceride of the drainage fluid was greater than 1.13 mmol/L, and meeting any of the criteria, the diagnosis could be made.
Diarrhea was defined as three or more loose stools per day lasting for more than 3 days. Intestinal obstruction was considered a minor complication in this cohort, as no patients underwent surgery due to postoperative intestinal obstruction; nevertheless, all of these individuals improved with conservative care and did not suffer significantly.
Risk factors
Age, sex, maximum tumor diameter at operation, location, tumor origin, Shimada classification, IDRFs, INRG stage, INRG risk group, MYCN status, retroperitoneal lymph node metastasis, operation style, operation time, surgical excision and avascular encasement were evaluated as potential risk factors for complications. Vascular encasement in this study was defined as having tumors wrapping more than 75% of the surrounding blood vessels, including the aorta, celiac trunk, superior mesenteric artery, renal artery, and inferior mesenteric artery.
Statistical analysis
For statistical analysis, IBM SPSS software (Version 26.0.0; Armonk, NY, IBM Corp.) was used. The relationship between patient characteristics and perioperative complications was evaluated using Chi-squared test. Univariable analysis produced significant variables, and risk factors related to postoperative complications were finally filtered out by multivariable conditional logistic regression. A probability of type I error of 5% (P < 0.05) was used to determine statistical significance.
Results
Patients
The key characteristics of the patients who were eligible for the criteria are listed in Table 1.
Operative factors
Laparotomy was performed in 498 patients and minimally invasive in 73 patients, including laparoscopic surgery in 59 patients and DaVinci robotic surgery in 14 patients. The tumors in 524 cases were GTR, while 49 cases were PR.
Perioperative complications
Perioperative complications were observed in 255 (44.7%) of 571 patients. Primary complications occurred in 234 (41.0%) patients, while minor complications occurred in 31 (5.4%). The incidence of intraoperative and postoperative complications was 6.8% and 39.6%, respectively. There were 3 (0.53%) operation-related deaths: massive hemorrhage (n = 1), biliary tract perforation (n = 1), and intestinal necrosis (n = 1).
LL (28.4%), diarrhea (13.5%), and injury (vascular, nerve and organ; 7.5%) were the most frequent complications. Vascular injury occurred in 19 (3.3%) patients, including the aorta, renal artery, superior mesenteric artery, inferior mesenteric artery, and splenic artery. All other complications (hypertension, unplanned organ resection, infection or minor complications) occurred in < 4.2% of patients. All complications and their incidences are illustrated in Table 2.
Risk factors
Univariable analysis
The relationship between factors and perioperative complications was analyzed (Table 1). Complications were more likely to be associated with larger tumor size, adrenal primary tumor, Shimada classification as NB, presence of IDRFs, high stage of INRG staging system (INRGSS), high-risk group of INRG, MYCN amplification, retroperitoneal lymph node metastasis, laparotomy surgery, long period of operations, GTR, and vascular encasement.
LL and diarrhea were more likely to be associated with larger tumor size, Shimada classification as NB, presence of IDRFs, high stage of INRGSS, high-risk group of INRG, MYCN amplification, retroperitoneal lymph node metastasis, laparotomy surgery, long period of operations, and vascular encasement (Table 3). There was PR in 6.2% in the absence of complications compared with 11.5% in their presence (P = 0.025).
Multivariate analysis
The multivariate analyses of risk factors for perioperative complications are presented in Table 4. The presence of IDRFs [odds ratio (OR) = 2.09, 95% confidence interval (CI) = 1.387–3.15, P < 0.01], high stage of INRGSS (OR = 0.454, 95% CI = 0.213–0.968, P = 0.04), retroperitoneal lymph node metastasis (OR = 2.433, 95% CI = 1.115–5.31, P = 0.026), superior mesenteric artery encasement (OR = 3.346, 95% CI = 1.505–7.439, P = 0.003), and inferior mesenteric artery encasement (OR = 2.218, 95% CI = 1.14–4.312, P = 0.019) were identified as independent risk factors for perioperative complications.
Retroperitoneal lymph node metastasis, superior mesenteric artery encasement, and inferior mesenteric artery encasement were identified as independent risk factors for LL (Table 4). Inferior mesenteric artery encasement was identified as an independent risk factor for diarrhea (Table 4).
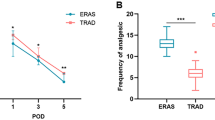
Survival analysis
Five-year event-free survival (5-year EFS; 0.750 ± 0.027) and 5-year overall survival (5-year OS; 0.820 ± 0.025) were significantly higher without complications than with complications (5-year EFS: 0.523 ± 0.043; 5-year OS: 0.682 ± 0.044; P < 0.001; Table 5).
Discussion
In the present study, we analyzed the incidence of all perioperative complications and risk factors for perioperative complications in patients who underwent tumor resection for NB. IDRFs, high stage of INRGSS, retroperitoneal lymph node metastasis, and vascular encasement were significant risk factors for perioperative complications, yet MYCN amplification and tumor size were not significant risk factors. Furthermore, despite the high incidence of perioperative complications, the associated mortality rate was quite low.
Surgery plays an important role in the treatment of NB and is associated with improved survival [3, 12]. Compared with tumor PR, patients who underwent GTR had significantly decreased mortality at 3 years and 5 years [13]. However, there are conflicting viewpoints. Gehad reported that the extent of tumor resection had no impact on EFS and OS, and the concept of accepting incomplete resection to avoid serious complications was successful [14].
Theoretically, the incidence of complications increased with the extent of tumor resection. However, this was not the case in the present study. In fact, the surgeon was forced to terminate the procedure due to severe complications during the operation, such as vascular injury and bleeding. As a result, GTR is not achievable, which increases the incidence of complications in patients with PR. The reported incidence of complications of NB ranged from 20% to 50%, depending on sample size, surgeon’s experience, and the definition criteria for complications. In this study, the overall complication rate was 44.7%. LL, diarrhea, and injury were the most frequent complications in the cohort.
As of yet, there is no official definition of LL, and each study differs in its definition. The occurrence of LL was closely related to the scope of lymph node dissection, and skeletonization resection around the superior mesenteric artery was identified as a significant risk factor. Prophylactic mesenteric lymphatic ligation contributed to its effectiveness in the prevention of chylous fistulae [15]. In our experience, another way to prevent LL was to suture the side peritoneum in a meticulous manner so that the retroperitoneal area was completely isolated from the abdominal cavity. The side peritoneum was often removed along with the tumor. In that case, the mesocolon could be sutured to the liver and lateral abdominal wall on the right side, while the stomach and descending colon could be sutured to the diaphragm and lateral abdominal wall on the left side to close the posterior peritoneum. When LL occurred, encapsulated effusion formed in the enclosed space behind the peritoneum and no longer increased once the tension reached a certain level.
Diarrhea, one of the paraneoplastic syndromes, is due to hypersecretion of vasoactive intestinal peptide by the tumor and will disappear after tumor resection [16]. In contrast, postoperative diarrhea has rarely been reported. In fact, diarrhea was fairly routine after retroperitoneal NB resection, occurring in up to 13.5% of our cohort, and was significantly related to tumor dissection around the aorta and inferior mesenteric artery. It was inferred that the accompanying excision of sympathetic nerve fibers leading to autonomous nerve dysfunction might be the culprit. This type of diarrhea was characterized by being refractory to medication and having a long duration. The symptoms become favorable when the autonomous nervous system gradually achieves equilibrium. However, it was the detail of the operational method with retaining as many nerve fibers as possible that counts.
Vascular injury is always a concern in retroperitoneal NB surgery due to the tumor's proclivity for encasing visceral vessels. Massive hemorrhage, transfusion requirements, renal hypertension and unscheduled nephrectomy were all not uncommon following high-risk NB resection. A critical step for avoiding and minimizing injury to these vessels is their identification before they pass through the tumor, most often at their take-off from the aorta or vena cava [17]. Additionally, 3D-printed models could be of great assistance to pediatric surgeons in understanding the spatial relationships of tumors with adjacent anatomic structures, especially vessels [18]. Do not panic if vascular injury occurred during the operation. Perfusion can be sustained in most cases with primary suture and vascular anastomosis or prosthetic vascular graft repair.
Catecholamines released by the NB were a significant cause of preoperative hypertension, while postoperative hypertension was most likely renovascular. If postoperative hypertension is not actively treated, it might lead to cardiovascular or cerebrovascular problems and interfere with the effectiveness of chemotherapy. The majority of individuals could return to normal with hypotensors. Percutaneous transluminal angioplasty was considered for refractory hypertension that failed antihypertensive medications [19], and nephrectomy was often employed as a last resort.
Unscheduled organ excision primarily involved the kidney. Tumor invasion of the kidney and wrapping around the kidney or renal pedicle did not mean the need for nephrectomy, and when these occurred in our cohort, the kidney could be saved while the tumor was removed. The most frequent cause for organ removal was accidental blood vessel damage, which should be removed when there was postoperative organ atrophy or refractory symptoms such as resistant hypertension.
In 2009, the INRG created a new staging system that relies on preoperative imaging for staging [20, 21]. Central to the INRGSS are IDRFs combined with clinical data to provide upfront risk stratification. IDRFs are a consensus of radiologic findings across multiple organ systems that can be applied consistently to diagnostic imaging to describe organ, nerve, and vessel involvement [22]. Evidently, there was a direct correlation between IDRFs and complications, and complications were more likely to occur when more IDRFs were involved [10]. The presence of IDRFs as a risk factor for perioperative complications requires surgeons to pay more attention to patients with IDRFs during surgery, and this should not discourage the determination to pursue total resection of NB.
MYCN amplification is one of the strongest independent adverse prognostic factors, accounting for 20% to 25% of NB and is strongly associated with advanced-stage disease [23,24,25]. MYCN-amplified NB was sensitive to chemotherapy and could considerably lower IDRFs after chemotherapy. In patients with localized NB harboring MYCN amplification, extended surgery of the primary tumor site improved the local control rate and survival [12].
We observed that MYCN-amplified NB was extremely invasive to the vascular adventitia and adjacent tissues, fusing tumors, vessels, and surrounding tissue into a sticky mass, making the surgery more challenging and potentially increasing the occurrence of complications. Unexpectedly, MYCN amplification was not a significant risk factor for perioperative complications in the study, which should be due to the high incidence of LL and diarrhea. It was recommended that GTR should be carried out on MYCN-amplified NB, and suspicious adjacent tissue should be excised as much as possible, which may prevent local recurrence and improve prognosis to some extent.
Reports showed that operative complications had no significant adverse effect on EFS or OS [3], but this was not the case in this study. It is important to consider that the complication rate was associated with a high stage of INRGSS and risk group of INRG. In addition, any perioperative complication would result in delays in the timely delivery of systemic therapy and/or the ability to deliver full-dose therapies.
In conclusion, despite the high incidence of perioperative complications, the associated mortality rate was quite low. The presence of IDRFs, high-stage INRGSS, retroperitoneal lymph node metastasis, superior mesenteric artery encasement, and inferior mesenteric artery encasement were significant risk factors for perioperative complications of retroperitoneal NB. Surgery for retroperitoneal NB has always been a challenge for pediatric oncologists. To improve clinical outcomes for these patients, surgeons take on the challenge of eliminating these tumors. Future large-sample and multicenter studies are expected to explore additional information, develop a more intuitive understanding of the complications and risk factors for NB surgery, and assist surgeons in providing better management for NB patients.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Maris JM, Hogarty MD, Bagatell R, Cohn SL. Neuroblastoma. Lancet. 2007;369:2106–20.
Croteau N, Nuchtern J, LaQuaglia MP. Management of neuroblastoma in pediatric patients. Surg Oncol Clin N Am. 2021;30:291–304.
Holmes K, Pötschger U, Pearson ADJ, Sarnacki S, Cecchetto G, Gomez-Chacon J, et al. Influence of surgical excision on the survival of patients with stage 4 high-risk neuroblastoma: a report from the HR-NBL1/SIOPEN study. J Clin Oncol. 2020;38:2902–15.
Twist CJ, Schmidt ML, Naranjo A, London WB, Tenney SC, Marachelian A, et al. Maintaining outstanding outcomes using response- and biology-based therapy for intermediate-risk neuroblastoma: a report from the Children’s Oncology Group Study ANBL0531. J Clin Oncol. 2019;37:3243–55.
Kiely EM. The surgical challenge of neuroblastoma. J Pediatr Surg. 1994;29:128–33.
Kiely E. A technique for excision of abdominal and pelvic neuroblastomas. Ann R Coll Surg Engl. 2007;89:342–8.
Rees H, Markley MA, Kiely EM, Pierro A, Pritchard J. Diarrhea after resection of advanced abdominal neuroblastoma: a common management problem. Surgery. 1998;123:568–72.
Froeba-Pohl A, Muehling J, Vill K, Grote V, Komm T, Seitz D, et al. Lymphatic leakage after surgery for neuroblastoma: a rare complication? Eur J Pediatr Surg. 2021;31:140–6.
Phelps HM, Ndolo JM, Van Arendonk KJ, Chen H, Dietrich HL, Watson KD, et al. Association between image-defined risk factors and neuroblastoma outcomes. J Pediatr Surg. 2019;54:1184–91.
Temple WC, Vo KT, Matthay KK, Balliu B, Coleman C, Michlitsch J, et al. Association of image-defined risk factors with clinical features, histopathology, and outcomes in neuroblastoma. Cancer Med. 2021;10:2232–41.
Pediatric Oncology Committee CACAOG, Chinese Association of Pediatric Surgeons. Expert consensus on diagnosing and treating of neuroblastoma in children: CCCG⁃NB-2015 Regimen. Chin J Pediatr Surg. 2015;36:3–7 (in Chinese).
Fischer J, Pohl A, Volland R, Hero B, Dübbers M, Cernaianu G, et al. Complete surgical resection improves outcome in INRG high-risk patients with localized neuroblastoma older than 18 months. BMC Cancer. 2017;17:520.
Yang X, Chen J, Wang N, Liu Z, Li F, Zhou J, et al. Impact of extent of resection on survival in high-risk neuroblastoma: a systematic review and meta-analysis. J Pediatr Surg. 2019;54:1487–94.
Ahmed G, Fawzy M, Elmenawi S, Elzomor H, Yosif Y, Elkinaai N, et al. Role of surgery in localized initially unresectable neuroblastoma. J Pediatr Urol. 2018;14:231–6.
Chui CH. Mesenteric lymphatic ligation in the prevention of chylous fistulae in abdominal neuroblastoma surgery. Pediatr Surg Int. 2014;30:1009–12.
Han W, Wang HM. Refractory diarrhea: a paraneoplastic syndrome of neuroblastoma. World J Gastroenterol. 2015;21:7929–32.
Davidoff AM, Fernandez-Pineda I. Complications in the surgical management of children with malignant solid tumors. Semin Pediatr Surg. 2016;25:395–403.
Anand S, Krishnan N, Goel P, Dhua AK, Jain V, Yadav DK, et al. Utility of three-dimensional printing for preoperative assessment of children with extracranial solid tumors: a systematic review. Pediatr Rep. 2022;14:32–9.
Alexander A, Richmond L, Geary D, Salle JL, Amaral J, Connolly B. Outcomes of percutaneous transluminal angioplasty for pediatric renovascular hypertension. J Pediatr Surg. 2017;52:395–9.
Monclair T, Brodeur GM, Ambros PF, Brisse HJ, Cecchetto G, Holmes K, et al. The International Neuroblastoma Risk Group (INRG) staging system: an INRG Task Force report. J Clin Oncol. 2009;27:298–303.
Spencer B, Patel A, Cilley R, Grant CN. Surgical management in pediatric neuroblastoma diagnosis and treatment: a 20-year, single-center experience. World J Pediatr. 2022;18:120–5.
Ryan AL, Akinkuotu A, Pierro A, Morgenstern DA, Irwin MS. The role of surgery in high-risk neuroblastoma. J Pediatr Hematol Oncol. 2020;42:1–7.
Thompson D, Vo KT, London WB, Fischer M, Ambros PF, Nakagawara A, et al. Identification of patient subgroups with markedly disparate rates of MYCN amplification in neuroblastoma: a report from the International Neuroblastoma Risk Group project. Cancer. 2016;122:935–45.
Brodeur GM, Bagatell R. Mechanisms of neuroblastoma regression. Nat Rev Clin Oncol. 2014;11:704–13.
Somasundaram DB, Aravindan S, Gupta N, Yu Z, Baker A, Aravindan N. ALK expression, prognostic significance, and its association with MYCN expression in MYCN non-amplified neuroblastoma. World J Pediatr. 2022;18:285–93.
Acknowledgements
Special thanks to Yi Jin and Yan Huang for helping with the image processing for this study. We thank all the members of clinical team who provided care for patients.
Funding
This work was supported by General Program of National Natural Science Foundation of China (No. 32270853), and Key Program of Natural Science Foundation of Zhejiang Province (No. HDMZ23H160029).
Author information
Authors and Affiliations
Contributions
HM and CJB contributed equally to this work and should be considered co-first authors. HM drafted the initial manuscript and was the surgeon who treated the patient. CJB helped to review and edit the literature, and CJB was the surgeon who treated the patient. WX, TYB, WJY, CJJ, GZH, XJN, and PWX contributed to data acquisition, analysis and interpretation. MJQ and TT helped to review and edit the literature. WJH was the guarantor and designed the study, helped to review and edit the literature, and was the surgeon who treated the patient. All authors issued final approval for the version to submitted and published.
Corresponding authors
Ethics declarations
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Children’s Hospital, Zhejiang University School of Medicine (2022-IRB-271). Informed consent to participate in the study have been obtained from participants (or their parent or legal guardian in the case of children under 16).
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article. The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
He, M., Cai, JB., Wu, X. et al. Perioperative complication incidence and risk factors for retroperitoneal neuroblastoma in children: analysis of 571 patients. World J Pediatr 20, 250–258 (2024). https://doi.org/10.1007/s12519-023-00773-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-023-00773-z