Abstract
Background
The aim of this study was to identify similarities and differences in the unmet supportive care needs (USCN) of families of children with major chronic health conditions (CHCs) using a universal need assessment tool.
Methods
A cross-sectional online survey involving parents of children with congenital heart disease (CHD), type 1 diabetes mellitus (T1D), cancer, and asthma diagnosed within the last 5 years recruited via social media and support organizations. Thirty-four items assessing the USCN across six domains (care needs, physical and social needs, informational needs, support needs, financial needs, child-related emotional needs) were responded to on a 4-point Likert scale [no need (1) to high need (4)]. Descriptive statistics identified the level of need, and linear regressions identified factors associated with higher need domain scores. Due to small numbers, the asthma group was excluded from comparisons across CHCs.
Results
One hundred and ninety-four parents completed the survey (CHD: n = 97, T1D: n = 50, cancer: n = 39, and asthma: n = 8). Parents of children with cancer were most likely to report at least one USCN (92%), followed by parents of children with T1D (62%). The five most commonly reported USCN across CHCs were drawn from four domains: child-related emotional, support, care, and financial. Three need items were included in the top five needs for all conditions. A higher USCN was associated with a greater frequency of hospital visits and the absence of parental support.
Conclusions
Using a universal need assessment tool, this is one of the first studies to characterize USCN in families of children diagnosed with common CHCs. While proportions endorsing different needs varied across conditions, the most endorsed needs were similar across the illness groups. This suggests that support programs or services could be shared across different CHCs.
Video Abstract
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic health conditions (CHCs) are those that last longer than a year, require regular medical attention, and cause limitations in daily life [1, 2]. In Australia, the prevalence of chronic disease is increasing, with recent data (2020–2021) indicating that approximately 44% of children have at least one CHC (inclusive of mental health conditions) [3, 4]. A CHC in childhood can have a lasting negative impact on educational, social, and emotional outcomes [5]. Medical care for children with CHC may include complex and/or ongoing treatment, with families requiring diligence, energy, and skills to manage their child’s health (e.g., ensuring medications taken as prescribed) [6]. Additionally, parents need to provide physical, emotional, and practical support to their child while maintaining work, family, and social roles [7,8,9].
Although the medical care of children with different chronic conditions varies, there is similarity in patterns of parental adjustment and experiences [9,10,11,12,13,14,15,16]. For instance, a systematic review identified common experiences of parents of children with different long-term conditions relating to a lack of information and support, managing emotional and physical burdens, mastering technical aspects of the child’s care, coordinating services and seeking social support systems [14]. A systematic review exploring father’s experiences caring for a child with a chronic illness found increased anxiety and depression, lower self-esteem and a need for social and informational support regardless of the health condition [16].
Supportive care needs (SCN) refer to the services or support that people with a health condition or those caring for them may need [17, 18]. The SCN framework, originally developed in relation to cancer care, classifies needs into a number of different domains, including physical, emotional, social, psychological, informational, spiritual, health care, and practical care [17, 19]. A gap in the support parents need and the support they receive reflects unmet supportive care needs (USCN), highlighting areas where further services are required [20,21,22,23,24]. Determining the USCN of parents caring for children with a CHC can help to develop programs and services to enhance parents wellbeing and assist children in their adjustment to their health condition [8, 25,26,27]. The SCN framework and concept have been extended to consider the needs of carers and families of children with life-limiting and rare conditions, including pediatric cancers [19, 23, 25, 28,29,30,31,32].
Research has demonstrated the universality of need domains across different groups [28, 31, 33]. However, as the majority of research examining USCN in families of children with a CHC has focused on cancer, our understanding of similarity and differences in specific needs across childhood CHCs is limited [26, 33]. Furthermore, the lack of a consistent method to assess unmet needs across different conditions [33] makes it difficult to determine whether there exists a common pattern of needs across families of children with different CHCs. To start to address this gap, this study aimed to use a universal need assessment to (1) characterize the unmet SCN across different common childhood CHCs; (2) compare frequencies of moderate/high needs across conditions; and (3) determine associations between level of need and parental demographic characteristics, child-specific factors, and illness-related variables.
Methods
Sample and setting
This study comprised an online cross-sectional survey involving a convenience sample of Australian parents of children with common CHCs. The survey was open between November 2020 and October 2022. Inclusion criteria were as follows: (1) Australian parents of children diagnosed with one of the following CHCs: congenital heart disease (CHD), type 1 diabetes mellitus (T1D), cancer, or asthma; (2) children aged between 0 and 18 years; and (3) receiving treatment or managing their condition in the last 5 years. Exclusion criteria included children with a genetic, developmental, cognitive, or mental health condition.
Measures
Parents completed an online survey consisting of items measuring the USCN, child-illness factors, and demographic characteristics of the child and family.
Unmet supportive care needs survey
Given that there currently exists no universal instrument to assess USCN in families of children with different CHCs [33], our approach was guided by Denham et al.’s (2020) framework for assessing USCN in carers of adults with mixed CHCs [34]. We developed a set of items drawing on USCN scales developed for cancer: eight items from the Family Inventory of Needs–Pediatric II [35] and thirteen items from the Cancer Survivors Unmet Needs scale [36]. Fourteen additional items derived from the CHC literature were included in the survey. Items were designed to cover five domains identified, with the addition of items assessing financial needs [28, 33]. To ensure appropriateness and acceptability to CHCs included in our study, the wording of each item was reviewed, and cancer-specific wording was changed to ensure inclusivity. The initial scale consisted of 35 items with respondents indicating their level of need for help in the past month on a four-point Likert scale ranging from no need (1), low need (2), moderate need (3) and high need (4). The USCN survey takes approximately 10 minutes to complete. An exploratory principal component analysis with varimax rotation was conducted (Supplementary tables, Part 1) to determine whether the USCN items could be classified into domains as suggested by others [17, 28, 31]. The scree plot and the eigenvalue > 1 criteria were used to identify the number of factors to retain. Items were eligible to be assigned to a factor if factor loadings were > 0.30. This analysis yielded six factors (termed “domains”) accounting for 70% of the total variance. Cronbach’s alpha coefficient revealed very good internal consistency for the domain subscales derived from identified factors.
Items were rearranged to provide a clear factor solution that was conceptually and clinically relevant [29]. Although items 20, 16, 19 and 33 had greater loadings under other factors, they were retained under factor 4 due to their conceptual or clinical similarity with items on this factor and were primarily designed to assess support needs. Additionally, item 18 did not load conceptually well on any domains and was excluded from subsequent analysis. The domains identified for the 34 items were (1) care needs (7 items, 50.72% variance, α = 0.87); (2) physical and social needs (7 items, 4.67% variance, α = 0.92); (3) informational needs (4 items, 4.10% variance, α = 0.88); (4) support needs (9 items, 3.71% variance, α = 0.90); (5) financial needs (3 items, 3.45% variance, α = 0.87); and (6) child-related emotional needs (4 items, 3.08% variance, α = 0.87) (Supplementary tables, Part 1).
Parent and child characteristics
The child’s condition, parent demographic characteristics and treatment-related information were collected. Parent demographic characteristics included age, gender, marital status (partnered vs. other), employment (working vs. not working), and education (up to secondary vs. post-secondary education). Questions also assessed access to a support person such as a partner, friend, or sibling (yes vs. no). Several support organizations for each condition are available and provide free services (e.g., peer support groups, helpline). Respondents indicated that the number of support services (among those listed for each CHC) used was tallied and standardized as the mean score. Child characteristics included sex, current age, disease type, and age at diagnosis and treatment or management (e.g., surgery). Number of hospital visits for professional consultations over the past 12 months was collected with responses recoded into never/once a year, two, and three or more times a year.
Procedure
Parents were invited to participate through multiple avenues, including advertising on social media platforms and through charity support group organizations. For the latter, organizations specific to the condition (e.g., Redkite, Heart Kids, Diabetes Australia, and Asthma Australia) were contacted, and the study was advertised either through their websites or via email. All invitations provided parents with background information about the study and the link to the online survey. Upon giving consent, parents completed the survey in Qualtrics. Ethics approval was obtained from the institutional review board of Deakin University, Australia (HEAG-H_53_2020).
Data analysis
Descriptive statistics were used to examine parents demographic characteristics and USCN. The level of need (low, moderate, or high need) endorsed across all items was assessed to identify the proportions reporting no need on all items, low but no moderate/high needs across items, at least one moderate but no high need, or at least one high level need. Need items were binary coded (no/low and moderate/high), and Chi-square analyses assessed differences in the likelihood of indicating a moderate/high need across health conditions. Percentages of moderate/high needs were used to rank the top 5 USCN items. Standardized USCN domain scores were calculated by summing scores for items within the domain, subtracting the number of domain items (indicated as m), then multiplying the resulting value by 100/[m × (k − 1)], where k is the maximum response value for each item (i.e., 4; high need) [37]. Standardized domain scores have possible values ranging between 0 and 100, with higher scores indicating greater USCN in that domain. Multiple linear regression analyses examined relationships between each standardized USCN domain score and parents demographic characteristics, child’s age and illness characteristics after controlling for the child’s CHC. Regression analyses were conducted in Stata v17 [38], and all other analyses were conducted in SPSS v28 [39]. Due to low numbers, respondents representing children with asthma were excluded from statistical analyses comparing responses across CHCs. Data from this group are reported in Supplementary tables, Part 2. To assess the impact of including the asthma group in regression analyses, sensitivity analyses involving repeating the multiple regression analyses without the asthma group were conducted.
Results
Sample characteristics
Of those accessing the survey site, only 65% completed the survey, and incomplete responses were removed. A total of 201 parents completed the survey. Seven did not meet the inclusion criteria regarding child diagnosis (presence of genetic/developmental conditions) and were removed. Surveys were completed on average approximately 3.3 years post diagnosis of children’s condition, although this varied by condition from around 6 months post-diagnosis for T1D, 1 year for cancer and 5 years for CHD. Of the 194 eligible parents, most were mothers (93%), had a partner (86%) and were aged between 25 and 56 years [mean age = 39, standard deviation (SD) = 6]. With respect to the children with CHCs, 52% were males, aged between 1 and 16 years (mean age = 7, SD = 4). Fifty percent of children had CHD, 26% had T1D, 20% had cancer and 4% had asthma (Table 1 and Supplementary tables, Part 2). Most children with T1D (72%) attended health care professionals three or more times a year, as did 59% of children with cancer and 34% of children with CHD.
Prevalence of unmet supportive care needs
Most parents reported at least one unmet need, with 27% reporting at least one moderate and 61% reporting at least one high USCN (Table 2). Parents of children with cancer were most likely to have at least one high USCN (92%), followed by parents of children with T1D (62%). Half of the parents of children with CHD reported at least one high USCN (50%). Mean scores from the standardized domain scales indicate child-related emotional needs the highest and informational needs the lowest USCN across CHCs (Table 2, and Supplementary tables, Part 2).
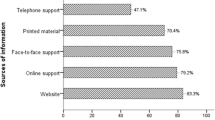
Commonly reported unmet supportive care needs
Table 3 shows the proportion of parents endorsing “moderate/high” need for each individual need item and displays the top 5 (i.e., most commonly endorsed) USCN for each CHC (except asthma, due to low numbers) and across the overall sample. For most items, the proportions endorsing moderate/high need differed by CHC, with parents of children with cancer significantly more likely to report moderate/high need across the items. The financial items were the exception to this pattern, with more parents of children with T1D and CHD than cancer reporting moderate/high needs. The five most commonly reported USCN in the overall sample were drawn from four need domains: child-related emotional (items ranked 1 and 4), support (items ranked 2 and 3), financial (rank 4), and care (rank 5). Despite the group differences in proportions endorsing moderate/high need on the individual items, the five most commonly endorsed need items were similar across CHCs. Three USCN items were in the top 5 for all CHCs: items “worry about your child’s future” (rank 1), “reducing any stress, you may be experiencing” (rank 2 or 3) and “managing your tiredness or lack of energy” (rank 2, 4 or 5) (Supplementary tables, Part 3).
Factors associated with unmet supportive care needs
After controlling for the child’s diagnosis, only two factors were related to multiple USCN domains: number of times the child attended a hospital/health professional and the absence of a support person (Table 4). A greater number of medical appointments was significantly associated with higher scores for all domains. Except for child-related emotional needs, the absence of a support person was related to higher scores on all domains (Table 4). Children’s age, age at diagnosis, gender, parents age, and employment status were not related to any USCN domains. Other variables were related to one or two USCN domains. The use of support services and parent marital status were positively associated with care needs [B = 0.1, standard error (SE) = 0.9, P < 0.05] and financial needs (B = 14.0, SE = 6.8, P < 0.05). Parent education was negatively related to care needs (B = − 10.6, SE = 3.8, P < 0.01). Sensitivity analyses found no difference in regression results when the asthma group was excluded from the analyses.
Discussion
Using a universal need assessment tool developed for use in families of children affected by some of the most common CHCs, this is one of the first studies to characterize similarities and differences in the SCN of families of children living with a number of different CHCs. With over 60% of parents reporting at least one high USCN, the results suggest that many parents of children with common CHCs experience a gap in the support they need and the support they receive. The proportion of parents identifying a moderate/high need for each item differed between CHCs, with the cancer group having the highest needs, reflecting the different treatment protocols and prognoses of the CHCs included in this study. However, we also found that the types of needs most commonly experienced were similar across CHCs, with “worry about their child’s future”, additional support to help “reduce their own stress”, and “manage tiredness” as key issues for parents. These findings suggest that some areas of support could be generalized across CHCs. A greater frequency of visits to hospital/medical appointments was associated with a higher need across domains, suggesting the role that medical demands, treatment or lack of health information and self-care skills have in generating unmet needs for parents [14, 40, 41]. Additionally, we found that the absence of a support person was associated with a higher USCN in five of the six domains. Previous studies have also shown that the lack of a support person can contribute to greater care burdens for parents [42, 43]. These findings provide suggestions for factors that might help identify parents who require additional assistance regardless of their child’s health condition.
The high prevalence of unmet needs across conditions indicates that many parents require more support than they are currently accessing. While pediatric health services in Australia provide psychology and social work services, access may be hindered due to variations in the type of services available, eligibility criteria, a lack of coordinated care, and limited information about services [44]. Community-based support organizations for each condition provide access to additional support services. However, the use of these services was relatively low in our study, with the highest usage found among parents of children with T1D. As others have noted, work to identify, and implement effective strategies to better link parents to relevant services in the community and at health services is needed [10, 15, 26].
Apart from the literature relating to pediatric cancer, few studies have assessed the unmet SCN of families of children with CHD, T1D or other conditions to compare our findings [33]. We found that parents need for additional support was high across all CHCs. Previous pediatric cancer and CHD studies reported high levels of emotional needs in parents, with most reporting needs regarding managing anxiety, stress, or grief [19, 25, 30, 32, 45, 46]. Our study also found that needs relating to managing concerns about the future or illness progression were common across CHCs. While this domain has been identified by others examining the needs of families of children with cancer [32], our recent systematic review suggests that child-related emotional concerns are often combined with general parental emotional concerns, including feelings of anxiety, depression, and grief [33]. The integration of needs relating to the carer’s own emotional state and concerns about the patient’s disease progression into a single emotional need domain is also seen in the adult carer USCN literature [24, 29, 47]. Although the need domains identified in our study are broadly consistent with the SCN framework, the high frequency of financial needs in the T1D group suggests that work is required to ensure that all relevant unmet need domains are captured by assessment tools. In addition, although needs relating to school, communication and lifestyle management have been identified [48,49,50], their relevance across childhood CHCs is less well understood and requires further investigation.
Regardless of the child’s condition, two commonly reported USCN in our study were reducing parents stress and managing tiredness. Stress in parents caring for a child with a CHC is common and is unrelated to illness duration or severity [12]. Many factors have been associated with parenting stress, including treatment adherence/management responsibilities, frequent hospitalizations, communication with health care providers, disruption of a normal family life, and lack of resources or social support [12, 51]. Need items reflecting these factors were reported as unmet in our study. Our findings suggest that many parents of children with CHCs require more assistance in managing the stress they experience.
The need for financial support/assistance was endorsed by many families and was a top 5 unmet needs for families of children with T1D and CHD. Financial burden has been identified previously [46, 52,53,54,55,56]. Studies have shown that many mothers of children with one of our health conditions restrict their hours of paid work to care for their child [54], which may add to the financial impact of these conditions. In addition, ongoing costs associated with T1D management may contribute to a significant financial burden for families [54]. Similarly, in CHD, lack of insurance coverage and disease complexity/treatment costs over time can contribute to increased financial burden [55, 56]. While parents of children with cancer also experience financial burden [57] in our study, the proportions reporting a financial need were less than T1D and CHD parents. In the Australian context, this finding may reflect that pediatric cancer care is primarily delivered in the public hospital system, which reduces out-of-pocket costs for families. While there is government assistance for T1D care, including devices, this funding may not cover all costs. The lifelong need for T1D care may place additional stress on parents. With few studies examining the financial needs of parents of children with CHCs, our study suggests that work is needed to identify the type and drivers of financial needs parents have.
Although parents of children with CHD were less likely to experience moderate/high needs than parents of children with cancer or T1D, our study found that 80% experienced at least one moderate/high need for additional support. Previous research in parents of children with CHD found similar results, with 59% having at least one need and 40% of parents reporting a need for psychosocial care [45, 46]. Despite differences in the timing of our survey and treatment stage (from diagnosis to 5 years post-treatment), the level of USCN found in previous studies is similar to the levels reported here. Additional work is required to identify and classify the unique needs of parents across the trajectory of CHD care.
This is one of the few studies to use the same assessment tool to examine unmet needs across different CHCs post-acute treatment, allowing comparison of type and extent of needs across conditions. The initial psychometric evaluation of this newly established assessment tool showed good reliability but requires further validation. Recruitment via online platforms (including social media platforms associated with condition-specific support services and charity organizations) and selection bias (mostly mothers) may limit the potential generalizability of the findings. It is possible that those who engage with these platforms may have greater needs [58]. Recruitment of parents of children at various stages of care and during the coronavirus disease 2019 (COVID-19) pandemic might have caused this disparity and elevated needs. The sample size of parents of children with different CHCs varied considerably, with low numbers for asthma. While this may reflect a lack of need among these different groups, it is also possible that the timing of the survey influenced participation with parents focusing on managing their child’s health during the COVID-19 pandemic [59, 60]. Finally, our survey was based on measures developed for cancer populations. While the similarities in the ranking of needs across the CHCs suggest the utility of this approach, further work is needed to determine a suitable tool to assess USCN across multiple CHCs. The findings from this study suggest that this work is warranted.
In conclusion, our results show that a significant number of parents caring for a child with a CHC have a moderate/high level of needs, demonstrating a gap in the support services they require and receive. As there is a lack of intervention studies addressing the USCN of pediatric CHCs, future research should develop and test interventions. The similarity of the top ranked needs across CHCs suggests that support programs, particularly those that aim to help parents address their fatigue and stress, could be shared across health conditions. To assist this work, research is also needed to develop a standardized measure for assessing the USCN of parents across multiple CHCs.
Data availability
Due to ethical and privacy reasons data is not publicly available. Datasets generated during the current study will be accessible from corresponding author upon reasonable request.
Change history
19 June 2023
The original version is updated due to missing of video abstract.
References
Bernell S, Howard SW. Use your words carefully: what is a chronic disease? Front Public Health. 2016;4:159.
Centers For Disease Control And Prevention. About chronic diseases. https://www.cdc.gov/chronicdisease/about/index.htm. 2021. Accessed 27 Jan 2022.
Australian Bureau of Statistics. Health conditions prevalence. https://www.abs.gov.au/statistics/health/health-conditions-and-risks/health-conditions-prevalence/2020-21. 2022. Accessed 2 Nov 2022.
Australian Institute of Health and Welfare. Health of children. https://www.aihw.gov.au/reports/children-youth/health-of-children. 2022. Accessed 2 Nov 2022.
Miller GF, Coffield E, Leroy Z, Wallin R. Prevalence and costs of five chronic conditions in children. J Sch Nurs. 2016;32:357–64.
Rohan JM, Winter MA. Ethical considerations in pediatric chronic illness: the relationship between psychological factors, treatment adherence, and health outcomes. Paediatr Respir Rev. 2021;39:48–53.
Hjelmstedt SK, Forinder UM, Lindahl Norberg AM, Hovén EIM. A balancing act: working and caring for a child with cancer. J Child Fam Stud. 2021;30:1881–94.
Kimbell B, Lawton J, Boughton C, Hovorka R, Rankin D. Parents’ experiences of caring for a young child with type 1 diabetes: a systematic review and synthesis of qualitative evidence. BMC Pediatr. 2021;21:160.
Nayeri ND, Roddehghan Z, Mahmoodi F, Mahmoodi P. Being parent of a child with congenital heart disease, what does it mean? A qualitative research. BMC Psychol. 2021;9:33.
Bradshaw S, Bem D, Shaw K, Taylor B, Chiswell C, Salama M, et al. Improving health, wellbeing and parenting skills in parents of children with special health care needs and medical complexity-a scoping review. BMC Pediatr. 2019;19:301.
Tong HJ, Qiu F, Fan L. Parents’ experience of caring for children with type 1 diabetes in mainland China: a qualitative study. World J Clin Cases. 2021;9:2478–86.
Cousino MK, Hazen RA. Parenting stress among caregivers of children with chronic illness: a systematic review. J Pediatr Psychol. 2013;38:809–28.
Herzer M, Godiwala N, Hommel KA, Driscoll K, Mitchell M, Crosby LE, et al. Family functioning in the context of pediatric chronic conditions. J Dev Behav Pediatr. 2010;31:26–34.
Smith J, Cheater F, Bekker H. Parents’ experiences of living with a child with a long-term condition: a rapid structured review of the literature. Health Expect. 2015;18:452–74.
Smith S, Tallon M, Clark C, Jones L, Mörelius E. “You never exhale fully because you’re not sure what’s next”: parents’ experiences of stress caring for children with chronic conditions. Front Pediatr. 2022;10:902655.
Spurr S, Danford CA, Roberts KJ, Sheppard-LeMoine D, Machado Silva-Rodrigues F, Darezzo RNM, et al. Father’s experiences of caring for a child with a chronic illness: a systematic review. Children (Basel). 2023;10:197.
Fitch MI. Supportive care framework. Can Oncol Nurs J. 2008;18:6–24.
National Cancer Institute. Supportive care. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/supportive-care. 2022. Accessed 7 Sep 2022.
Kerr LM, Harrison MB, Medves J, Tranmer JE, Fitch MI. Understanding the supportive care needs of parents of children with cancer: an approach to local needs assessment. J Pediatr Oncol Nurs. 2007;24:279–93.
Campbell HS, Sanson-Fisher R, Taylor-Brown J, Hayward L, Wang XS, Turner D. The cancer support person’s unmet needs survey: psychometric properties. Cancer. 2009;115:3351–9.
Collier J, Pattison H, Watson A, Sheard C. Parental information needs in chronic renal failure and diabetes mellitus. Eur J Pediatr. 2001;160:31–6.
Cruz AC, Aranha GA, Silva CMC, Pedreira MLG. The complexity of having a child with a congenital heart defect in a developing country: a qualitative study of parental needs. J Pediatr Nurs. 2022;64:e159–65.
Kerr LM, Harrison MB, Medves J, Tranmer J. Supportive care needs of parents of children with cancer: transition from diagnosis to treatment. Oncol Nurs Forum. 2004;31:E116–26.
Sklenarova H, Krümpelmann A, Haun MW, Friederich HC, Huber J, Thomas M, et al. When do we need to care about the caregiver? Supportive care needs, anxiety, and depression among informal caregivers of patients with cancer and cancer survivors. Cancer. 2015;121:1513–9.
Aziza YDA, Wang ST, Huang MC. Unmet supportive care needs and psychological distress among parents of children with cancer in Indonesia. Psychooncology. 2019;28:92–8.
Leeman J, Crandell JL, Lee A, Bai J, Sandelowski M, Knafl K. Family functioning and the well-being of children with chronic conditions: a meta-analysis. Res Nurs Health. 2016;39:229–43.
Tikkanen AU, Oyaga AR, Riaño OA, Álvaro EM, Rhodes J. Paediatric cardiac rehabilitation in congenital heart disease: a systematic review. Cardiol Young. 2012;22:241–50.
Gill FJ, Hashem Z, Stegmann R, Aoun SM. The support needs of parent caregivers of children with a life-limiting illness and approaches used to meet their needs: a scoping review. Palliat Med. 2021;35:76–96.
Girgis A, Lambert S, Lecathelinais C. The supportive care needs survey for partners and caregivers of cancer survivors: development and psychometric evaluation. Psychooncology. 2011;20:387–93.
Ji Q, Currin-McCulloch JA, Zhang A, Streeter CL, Jones BL, Chen Y. Assessing the needs of parents of children diagnosed with cancer in China: a psychometric study developing a needs assessment tool. J Pediatr Oncol Nurs. 2018;35:6–15.
Pelentsov LJ, Laws TA, Esterman AJ. The supportive care needs of parents caring for a child with a rare disease: a scoping review. Disabil Health J. 2015;8:475–91.
Zucchetti G, Candela F, Ciappina S, Mastrazzo C, Roccia E, Bertolotti M, et al. Validation of a tool to assess the multidimensional needs of the parents of children with cancer. Cancer Nurs. 2022;45:141–7.
Thomas S, Ryan N, Byrne L, Hendrieckx C, White V. Unmet supportive care needs of families of children with chronic illness: a systematic review. Deakin Univeristy. 2023 (Under review).
Denham AMJ, Wynne O, Baker AL, Spratt NJ, Turner A, Magin P, et al. An online survey of informal caregivers’ unmet needs and associated factors. PLoS One. 2020;15:e0243502.
Monterosso L, Kristjanson LJ, Dadd G. Content validity and reliability testing of the FIN-PED II: a tool to measure care needs of parents of children with cancer. J Nurs Meas. 2006;14:31–44.
Hodgkinson K, Butow P, Hunt GE, Pendlebury S, Hobbs KM, Lo SK, et al. The development and evaluation of a measure to assess cancer survivors’ unmet supportive care needs: the CaSUN (Cancer Survivors Unmet Needs measure). Psychooncology. 2007;16:796–804.
McElduff P, Boyes A, Zucca A, Girgis A. Supportive care needs survey: a guide to administration, scoring and analysis. Newcastle: Centre for Health Research & PsychoOncology; 2004.
Stata statistical software: release 17. TX, United States: StataCorp LLC; 2021.
IBM Spss statistics for windows. Armonk. New York: IBM Corp; 2021.
Miller AR, Recsky MA, Armstrong RW. Responding to the needs of children with chronic health conditions in an era of health services reform. CMAJ. 2004;171:1366–7.
Greenfield G, Okoli O, Quezada-Yamamoto H, Blair M, Saxena S, Majeed A, et al. Characteristics of frequently attending children in hospital emergency departments: a systematic review. BMJ Open. 2021;11:e051409.
Collins A, Burchell J, Remedios C, Thomas K. Describing the psychosocial profile and unmet support needs of parents caring for a child with a life-limiting condition: a cross-sectional study of caregiver-reported outcomes. Palliat Med. 2020;34:358–66.
Javalkar K, Rak E, Phillips A, Haberman C, Ferris M, Van Tilburg M. Predictors of caregiver burden among mothers of children with chronic conditions. Children. 2017;4:39.
Children’s Health Queensland Hospital and Health Service. Supporting the long-term developmental needs of children with congenital heart disease and their families. Queensland: Queensland Government; 2018. https://www.childrens.health.qld.gov.au/chq/health-professionals/qcyc-network/. Accessed 19 Jan 2023
Levert EM, Helbing WA, Dulfer K, van Domburg RT, Utens EM. Psychosocial needs of children undergoing an invasive procedure for a CHD and their parents. Cardiol Young. 2017;27:243–54.
Wray J, Maynard L. The needs of families of children with heart disease. J Dev Behav Pediatr. 2006;27:11–7.
Rietveld MJA, Peters EJ, Husson O, van Amstel FKP, Kamm Y, Sijtsema S, et al. Psychometric properties of the 45-item supportive care needs survey—partners and caregivers-Dutch (SCNS-P&C45-D) in partners of patients with breast cancer. J Patient Rep Outcomes. 2019;3:1.
Karst JS, Hoag JA, Chan SF, Schmidt DJ, Anderson LJ, Englebert NE, et al. Assessment of end-of-treatment transition needs for pediatric cancer and hematopoietic stem cell transplant patients and their families. Pediatr Blood Cancer. 2018;65:e27109.
Lesch W, Specht K, Lux A, Frey M, Utens E, Bauer U. Disease-specific knowledge and information preferences of young patients with congenital heart disease. Cardiol Young. 2014;24:321–30.
McNelis AM, Musick B, Austin JK, Larson P, Dunn DW. Psychosocial care needs of children with recent-onset asthma. J Spec Pediatr Nurs. 2007;12:3–12.
Golfenshtein N, Srulovici E, Medoff-Cooper B. Investigating parenting stress across pediatric health conditions—a systematic review. Issues Compr Pediatr Nurs. 2016;39:41–79.
Dodgson JE, Garwick A, Blozis SA, Patterson JM, Bennett FC, Blum RW. Uncertainty in childhood chronic conditions and family distress in families of young children. J Fam Nurs. 2000;6:252–66.
Helgeson VS, Becker D, Escobar O, Siminerio L. Families with children with diabetes: implications of parent stress for parent and child health. J Pediatr Psychol. 2012;37:467–78.
Katz ML, Laffel LM, Perrin JM, Kuhlthau K. Impact of type 1 diabetes mellitus on the family is reduced with the medical home, care coordination, and family-centered care. J Pediatr. 2012;160:861–7.
Ludomirsky AB, Bucholz EM, Newburger JW. Association of financial hardship because of medical bills with adverse outcomes among families of children with congenital heart disease. JAMA Cardiol. 2021;6:713–7.
McClung N, Glidewell J, Farr SL. Financial burdens and mental health needs in families of children with congenital heart disease. Congenit Heart Dis. 2018;13:554–62.
Pelletier W, Bona K. Assessment of financial burden as a standard of care in pediatric oncology. Pediatr Blood Cancer. 2015;62(Suppl 5):S619–31.
Frey E, Bonfiglioli C, Brunner M, Frawley J. Parents’ use of social media as a health information source for their children: a scoping review. Acad Pediatr. 2022;22:526–39.
Guido A, Marconi E, Peruzzi L, Dinapoli N, Tamburrini G, Attinà G, et al. Psychological impact of COVID-19 on parents of pediatric cancer patients. Front Psychol. 2021;12:730341.
McLoone J, Wakefield CE, Marshall GM, Pierce K, Jaffe A, Bye A, et al. It’s made a really hard situation even more difficult: the impact of COVID-19 on families of children with chronic illness. PLoS One. 2022;17:e0273622.
Acknowledgements
The investigators acknowledge the contribution of Redkite, Heart Kids, Diabetes Australia, and Asthma Australia in promoting the study to their members. We also thank the social media support groups for allowing us to advertise the study to their members. Finally, we wish to thank the parents and carers who took part in this study for sharing their experiences with us.
Funding
Open access funding is enabled and organized by CAUL and its Member Institutions. The lead author is funded by a Deakin University PhD Scholarship.
Author information
Authors and Affiliations
Contributions
TS contributed to conceptualization, methodology, data curation, formal analysis, writing of the original draft, funding acquisition, reviewing, and editing. BLK, RNP, HC, and WV contributed to conceptualization, methodology, resources, supervision, reviewing and editing. All authors have read and approved the submitted version.
Corresponding authors
Ethics declarations
Ethical approval
Ethics approval was obtained from Institutional Review Board of Deakin University (HEAG-H_53-2020). Informed consent to participate in the study have been obtained from all the participants.
Conflict of interest
There are no potential conflicts of interest to disclose. No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Thomas, S., Byrne, L.K., Ryan, N.P. et al. Unmet supportive care needs in families of children with chronic health conditions: an Australian cross-sectional study. World J Pediatr 19, 1181–1191 (2023). https://doi.org/10.1007/s12519-023-00730-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-023-00730-w