Abstract
Introduction
Cognitive impairment and depression in patients with heart failure (HF) are common comorbidities and are associated with increased morbidity, readmissions and mortality. Timely recognition of cognitive impairment and depression is important for providing optimal care. The aim of our study was to determine if these disorders were recognised by clinicians and, secondly, if they were associated with hospital admissions and mortality within 6 months’ follow-up.
Methods
Patients (aged ≥65 years) diagnosed with HF were included from the cardiology outpatient clinic of Gelre Hospitals. Cognitive status was evaluated with the Montreal Cognitive Assessment test (score ≤22). Depressive symptoms were assessed with the Geriatric Depression Scale (score >5). Patient characteristics were collected from electronic patient files. The clinician was blinded to the tests and asked to assess cognitive status and mood.
Results
We included 157 patients. Their median age was 79 years (65–92); 98 (62%) were male. The majority had New York Heart Association functional class II. Cognitive impairment was present in 56 (36%) patients. Depressive symptoms were present in 21 (13%) patients. In 27 of 56 patients (48%) cognitive impairment was not recognised by clinicians. Depressive symptoms were not recognised in 11 of 21 patients (52%). During 6 months’ follow-up 24 (15%) patients were readmitted for HF-related reasons and 18 (11%) patients died. There was no difference in readmission and mortality rate between patients with or without cognitive impairment and patients with or without depressive symptoms.
Conclusion
Cognitive impairment and depressive symptoms were infrequently recognised during outpatient clinic visits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
-
Cognitive impairment and depressive symptoms are highly prevalent in older patients with heart failure.
-
Cognitive impairment and depressive symptoms are infrequently recognised during outpatient clinic visits.
-
Timely recognition of cognitive impairment and depressive symptoms is important for providing optimal care.
Introduction
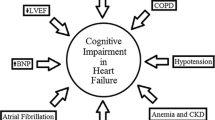
Cognitive impairment and depression are highly prevalent comorbidities in patients with heart failure. A complex interaction exists between heart failure, cognitive impairment and depression. Cognitive impairment and depression in patients with heart failure are known to worsen chronic heart failure and heart failure is known to worsen cognitive impairment and depression. They are also associated with poor outcomes: increased morbidity, readmissions and mortality [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15].
They share a common pathophysiological basis, such as neurohormonal activation and chronic inflammation and have similar risk factors such as hypertension, diabetes, hypercholesterolaemia and smoking [1,2,3,4,5,6,7,8,9,10,11, 16].
Recognition and optimal care
Timely recognition of cognitive impairment and depression is important to break the downwards spiral in which patients may find themselves: the treatment regimen of heart failure can be challenging for patients because of the need for self-management, which can be further complicated by cognitive impairment or depression [17]. Poor self-management may lead to exacerbation of heart failure and, as a consequence, more frequent readmissions and even mortality [12, 18, 19]. These exacerbations may in turn lead to an increase in cognitive problems and depressive symptoms. Optimal treatment of depression and support in the case of cognitive impairment could optimise the treatment of heart failure. Conversely, optimal treatment of heart failure may reduce depression and cognitive problems. Consequently, early recognition is the essential first step in improvement of treatment in heart failure patients; it may provide a unique opportunity to improve outcomes for these patients.
Aim
The aim of our study was to determine if cognitive impairment and depressive symptoms in older patients with heart failure were recognised by their clinicians and, secondly, to establish the association of these disorders with hospital admissions and mortality within 6 months.
Methods
We performed a cross-sectional cohort study at Gelre Hospitals, a medium-sized community teaching hospital with two locations in the Netherlands. Patients aged ≥65 years diagnosed with heart failure who attended the outpatient cardiology clinic between January 2017 and April 2017 and during a second inclusion period between May 2018 and October 2018 were approached for this study. The gap between these periods was due to logistical problems. At the end of their regular appointment with the cardiologist or nurse specialised in heart failure, patients were asked to participate. Exclusion criteria were communication problems such as severe hearing impairment or speech problems, known severe cognitive impairment, or not being physically well enough to perform or complete the tests. After providing written informed consent, each patient was interviewed by a research student, who was not involved in the patient’s care. This research student administered the Montreal Cognitive Assessment test (MoCA) and the Geriatric Depression Scale questionnaire (GDS). Patient characteristics and cardiovascular risk factors were collected from electronic patient records by a research nurse or research student and through the interviews by a research student. Socio-demographic variables were age, sex and years of education. Cardiovascular risk factors were hypertension, hypercholesterolaemia, current smoking, diabetes mellitus and atrial fibrillation as recorded by a cardiologist in patient records. Severity of heart failure was classified by the cardiologist based on the New York Heart Association (NYHA) guideline. Comorbidities were scored with the Charlson Comorbidity Index [20].
Cognitive status was evaluated with the MoCA [21], a screening instrument for mild cognitive dysfunction that assesses different cognitive domains: attention and concentration, executive functions, memory, language, visuo-constructional skills, conceptual thinking, and orientation. The maximum score is 30 points; a score of 26 or higher is considered normal. We used a cutoff score of ≤22, because we aimed to identify clinically relevant cognitive impairment that may have an impact on a patient’s self-management skills [22, 23].
Depressive symptoms were assessed with the GDS‑2 and GDS-15 [24]. The GDS‑2 is a questionnaire that broadly distinguishes patients with depressive symptoms from patients without symptoms. It is a self-rated screening instrument that consists of two questions regarding feelings of depression and anhedonia in the past month. If a participant answered one of these two questions in the affirmative, the symptoms were further assessed with the GDS-15. This is a 15-item form and a score >5 indicates depressive symptoms.
The cardiologist or nurse was blinded to the test results and was asked to assess whether the patient had cognitive problems or depressive symptoms.
The number of hospital admissions, the number of heart-failure-related admissions and mortality in the 6 months following inclusion were recorded.
The investigation conformed to the principles outlined in the Declaration of Helsinki.
Analysis
We calculated proportions for categorical variables and means and standard deviations for continuous variables that were normally distributed. For variables that were not normally distributed, we generated medians and interquartile ranges. We compared the characteristics of patients with and without cognitive impairment using the chi-square test, unpaired t-test or Mann-Whitney U test where applicable. All analyses were performed using SPSS software version 20.
Results
A total of 224 patients were asked to participate in our study, of whom 157 agreed. Their baseline characteristics are listed in Tab. 1. Median age was 79 years (range 65–92) and 98 (62%) of participants were male. The majority had NYHA functional class II. The median Charlson Comorbidity Index score was 3 (range 1–9). The median MoCA score was 24, and ranged from 11 to 30 with clustering of the scores around the median (Fig. 1). Cognitive impairment (defined as MoCA score ≤22) was present in 56 of 157 (36%) patients; 109 (69%) scored below the generally used cutoff of 26. In 72 (46%) patients the GDS-15 was performed, after initial assessment by the GDS‑2. The median score on the GDS-15 was 3.5 (range 0–13). Twenty-one patients (13%) had depressive symptoms. Six of these patients had cognitive impairment. During 6 months’ follow-up 44 (28%) patients were readmitted. Twenty-four (15%) patients were readmitted for heart-failure-related reasons and 18 (11%) patients died. There was no difference in overall readmissions and heart-failure-related readmissions between patients with or without cognitive impairment (p = 0.62 and p = 0.84 respectively) and patients with or without depressive symptoms (p = 0.95 and p = 0.61respectively). Cognitive impairment and depressive symptoms were not associated with mortality (p = 0.83 and p = 0.24 respectively).
Recognition of cognitive impairment and depressive symptoms
Of the 56 patients with cognitive impairment, 29 (52%) were not recognised as such by the clinician during the visit at the outpatient clinic. The sensitivity of assessment of cognitive impairment by the clinician was 48%. The specificity was 84% (Fig. 2).
Of the 21 patients with symptoms of depression, 11 (52%) were not recognised as such by the clinician. The sensitivity of the assessment of symptoms of depression by the clinician was 48%, the specificity was 85% (Fig. 3).
Discussion
In this study of older patients with heart failure, we found that cognitive impairment and depressive symptoms were poorly recognised by clinicians during visits to the outpatient clinic. Half of the patients with cognitive impairment and depressive symptoms were not recognised.
Recognition of cognitive impairment and depressive symptoms in patients with heart failure has not received much attention in previous studies. One study in outpatient heart failure patients showed an even poorer recognition of cognitive impairment than our study: cardiologists failed to recognise cognitive impairment in 88% of patients [25]. The difference could be a result of the fact that most of the patients in our study visited the heart failure nurse, who had more time to assess social factors during routine care. Another study, in line with our results, showed that 42% of patients with depressive symptoms were not recognised as such by clinicians in routine care [26].
An explanation for poor recognition of cognitive impairment and depressive symptoms could be that heart failure, cognitive decline and depression share certain symptoms such as loss of energy or decreased physical activities. A cardiologist might attribute these symptoms to heart failure, whereas they could be due to cognitive decline or depression as well [12, 26]. In addition, cardiologists are not routinely trained to diagnose cognitive impairment or affective disorders.
In contrast to our expectations and previous research our study showed no association between cognitive impairment and depressive symptoms and the number of hospital readmissions or mortality during 6 months’ follow-up [12, 18, 19]. This might be due to the relatively small sample size and because previous studies investigated a hospitalised population and had a longer follow-up period.
Suggestions for clinical practice and for future research
The high prevalence of cognitive problems and depressive symptoms, as well as the poor recognition of these conditions, may lead to suboptimal treatment in a large proportion of older heart failure patients. In addition, suboptimal heart failure treatment can accelerate cognitive decline and worsen depressive symptoms. One of the theories is that, in heart failure patients, low-grade hypoxia, neurohormones and elevated inflammatory cytokines play an important role in development of anatomical brain changes and cognitive dysfunctions [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15]. Timely recognition may allow adjustment of medication (e.g. statins may not be beneficial in patients with poor prognosis) and lifestyle regimes, simplification of dietary restrictions and better coordination of appointments. In patients with cognitive impairment or depression extra attention should be given to treatment adherence (e.g. medication, fluid restriction). We also recommend that a proxy accompanies the patient to all hospital appointments. These measures may prevent unnecessary hospital admissions and preserve quality of life. Recognition of cognitive impairment is also important in the decision-making process, for example decisions regarding possible implantable cardioverter defibrillator implantation or valve replacement and advance care planning [2, 3, 26,27,28].
Working towards better recognition starts with awareness and education: cognitive impairment and depressive symptoms are important comorbidities in heart failure. Physicians and nurses should be trained in signalling clinical signs of cognitive impairment and depressive symptoms in patients with heart failure. Barriers to improving recognition and heart failure management could be the physician’s available time, limited geriatric or mental health knowledge, and restricted availability of geriatric or mental health resources [12, 26].
Future research with larger study population sizes and longer follow-up is needed to confirm the current findings. Also, studies are needed to identify the best way to screen for cognitive problems and depression in outpatients with heart failure. As a part of normal care, periodic screening for cognitive decline and depressive symptoms in older patients with heart failure could be introduced in the heart failure care service. Formal cognitive testing, through history-taking by proxy and neuropsychological assessment, should be performed in patients showing symptoms of or screened positive for cognitive impairment. A diagnostic interview should be performed in patients screened positive for depressive symptoms. In all of the suggested strategies a two-step approach between cardiology, geriatric medicine, primary care and mental health care is paramount.
Study strengths and limitations
The MoCA and GDS are merely screening instruments to assess cognition and mood. We were unable to formally diagnose mild cognitive impairment, dementia or depression in our study. These screening instruments are, however, well suited to screen for problems that indicate a need for further assessment. We deliberately chose a stricter cutoff score of 22 for the MoCA, to make sure that we established the possibility of clinically relevant cognitive impairment that may have an impact on a patient’s self-management skills. Lower cutoffs are supported by previous studies for use in older outpatient populations [22, 23].
Selection bias in this study is possible, as patients with more severe cognitive impairment or depression might be less inclined to participate in the study. This may have led to an underestimation of the prevalence of cognitive impairment and depressive symptoms. However, in a recent meta-analysis the prevalence of cognitive impairment in heart failure cohorts [43% (95% confidence interval 30–55)] was in line with the prevalence in our study (36%) [16]. The prevalence of depressive symptoms in this study (13%) is lower than that described in previous studies (20–42%) [7, 13, 14, 26]. This difference can, in addition to possible selection bias, be explained by a difference in populations. Previous research included only younger patients, patients with higher NYHA class and inpatients. In these populations, a higher prevalence of depressive symptoms is to be expected.
The relatively small study population resulted in low numbers of outcomes during follow-up, which prohibited multivariable regression analyses with adjustment for confounders such as age and comorbidity.
Conclusion
Cognitive impairment and depressive symptoms in patients with heart failure are frequently present but infrequently recognised by clinicians. The lack of good recognition of these common comorbidities may lead to suboptimal treatment.
References
Alagiakrishnan K, Mah D, Ahmed A, et al. Cognitive decline in heart failure. Heart Fail Rev. 2016;21:661–73.
Festen S, de Rooij S. Heart failure and brain failure: two of a kind? Eur J Heart Fail. 2015;17:539–40.
Ampadu J, Morley J. Heart failure and cognitive dysfunction. Int J Cardiol. 2015;178:12–23.
Daskalopoulou M, George J, Walters K, et al. Depression as a risk factor for the initial presentation of twelve cardiac, cerebrovascular, and peripheral arterial diseases: data linkage study of 1.9 million women and men. PloS One. 2016;11:e153838.
Gullestad L, Ueland T, Vinge LE, et al. Inflammatory cytokines in heart failure: mediators and markers. Cardiology. 2012;122:23–35.
Cacciatore F, Testa G, Langellotto A, et al. Role of ventricular rate response on dementia in cognitively impaired elderly subjects with atrial fibrillation: a 10-year study. Dement Geriatr Cogn Disord. 2012;34:143–8.
Freedland K, Rich M, Skala J, et al. Prevalence of depression in hospitalized patients with congestive heart failure. Psychosom Med. 2003;65:119–28.
Almeida O, Beer C, Lautenschlager N, et al. Two-year course of cognitive function and mood in adults with congestive heart failure and coronary artery disease: the heart-mind study. Int Psychogeriatr. 2012;24:38–47.
Joynt K, Whellan D, O’Connor C. Why is depression bad for the failing heart? A review of the mechanistic relationship between depression and heart failure. J Card Fail. 2004;10:258–71.
Rutledge T, Reis V, Linke S, et al. Depression in heart failure: a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48:1527–37.
Huynh Q, Negishi K, Blizzard L, et al. Predictive score for 30-day readmission or death in heart failure. JAMA Cardiol. 2016;1:362–4.
Liguori I, Russo G, Curcio F, et al. Depression and chronic heart failure in the elderly: an intriguing relationship. J Geriatr Cardiol. 2018;15:451–9.
Haworth J, Moniz-Cook E, Clark A, et al. Prevalence and predictors of anxiety and depression in a sample of chronic heart failure patients with left ventricular systolic dysfunction. Eur J Heart Fail. 2005;7:803–8.
Sokoreli I, de Vries J, Riistama J, et al. Depression as an independent prognostic factor for all-cause mortality after a hospital admission for worsening heart failure. Int J Cardiol. 2016;220:202–7.
Vogels R, Scheltens P, Schroeder-Tanka J, et al. Cognitive impairment in heart failure: a systematic review of the literature. Eur J Heart Fail. 2007;9:440–9.
Cannon J, Moffitt P, Perez-Moreno A, et al. Cognitive impairment and heart failure: systematic review and meta-analysis. J Card Fail. 2017;23:464–75.
Chang L, Wu S, Chiang C, et al. Depression and self-care maintenance in patients with heart failure: a moderated mediation model of self-care confidence and resilience. Eur J Cardiovasc Nurs. 2017;16:435–43.
Dodson J, Truong T, Towle V, et al. Cognitive impairment in older adults with heart failure: prevalence, documentation, and impact on outcomes. Am J Med. 2013;126:120–6.
Agarwal K, Kazim R, Xu J, et al. Unrecognized cognitive impairment and its effect on heart failure readmissions of elderly adults. J Am Geriatr Soc. 2016;64:2296–301.
Quan H, Li B, Couris C, et al. Updating and validating the Charlson Comorbidity Index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173:676–82.
Nasreddine Z, Phillips N, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–9.
Gallagher R, Sullivan A, Burke R, et al. Mild cognitive impairment, screening, and patient perceptions in heart failure patients. J Card Fail. 2013;19:641–6.
Lee J, Lee D, Cho S, et al. Brief screening for mild cognitive impairment in elderly outpatient clinic: validation of the Korean version of the Montreal Cognitive Assessment. J Geriatr Psychiatry Neurol. 2008;21:104–10.
Skeikh J, Yesavage J. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol. 1986;5:165–73.
Hanon O, Vidal J, de Groote P, et al. Prevalence of memory disorders in ambulatory patients aged ≥70 years with chronic heart failure (from the EFICARE study). Am J Cardiol. 2014;113:1205–10.
Cully J, Jimenez D, Ledoux T, et al. Recognition and treatment of depression and anxiety symptoms in heart failure. Prim Care Companion J Clin Psychiatry. 2009;11:103–9.
Havakuk O, King K, Grazette L, et al. Heart failure-induced brain injury. J Am Coll Cardiol. 2017;69:1609–16.
Čelutkienė J, Vaitkevičius A, Jakštienė S, et al. Expert opinion-cognitive decline in heart failure: more attention is needed. Card Fail Rev. 2016;2:106–9.
Acknowledgements
B. Goudzwaard, M. van Nistelrooy, H. Zeilstra, V. Paques and E. van der Heul collected study data. H. van der Zaag advised on statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
F.M.M. Oud, P.E. Spies, R.L. Braam and B.C. van Munster declare that they have no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oud, F.M.M., Spies, P.E., Braam, R.L. et al. Recognition of cognitive impairment and depressive symptoms in older patients with heart failure. Neth Heart J 29, 377–382 (2021). https://doi.org/10.1007/s12471-020-01527-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12471-020-01527-6