Abstract
Background
After coronary artery bypass grafting (CABG), healthcare utilisation is high and is partly unplanned. eHealth applications have been proposed to reduce healthcare consumption and to enable patients to get actively involved in their recovery. This way, healthcare expenses can be reduced and the quality of care can be improved.
Objectives
We aim to evaluate whether the use of an eHealth programme can reduce unplanned healthcare utilisation and improve mental and physical health in the first 6 weeks after discharge in patients who underwent CABG. In addition, patient satisfaction and use of the eHealth programme will be evaluated.
Methods
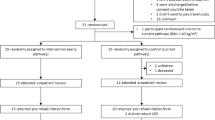
For this single-centre randomised controlled trial, at least 280 patients referred for CABG will be included at the preoperative outpatient clinic and randomised to an intervention or control group. The intervention group will have access to an eHealth programme, which consists of online educational videos developed by the Dutch Heart Foundation and postoperative video consultations with a physician. The control group will receive standard care and will not have access to the eHealth programme. The primary endpoint is healthcare utilisation; other endpoints include anxiety, duration of recovery, quality of life and patient satisfaction. Participants will complete several questionnaires at 6 time points during the study.
Results
Patient enrolment started in February 2020 and completion of the follow-up period is expected in August 2021.
Conclusion
This randomised trial was initiated to test the hypothesis that patients who are partaking in our eHealth programme use less unplanned care and experience a better quality of life, less anxiety and a faster recovery than controls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronary artery bypass graft grafting (CABG) is the most prevalent cardiac surgery performed in the Netherlands, with roughly 7000 procedures annually [1]. The care chain of CABG is costly, and several quality improvement initiatives have been successfully implemented that sought to contain costs and to improve patient outcomes [2, 3]. Despite the positive effects of these initiatives on costs, mortality, postoperative morbidity and process measures such as in-hospital length of stay, healthcare utilisation in the first 30 days after CABG remains an issue, placing a significant burden on the healthcare system. Readmissions after CABG are commonly reported and the readmission rate can be as high as 34% in the first 30 days [4, 5].
Insight into unplanned healthcare utilisation during this period is scarce (apart from readmissions), but it is reasonable to expect a short hospital stay after CABG is counterbalanced by the use of other healthcare services, especially because planned care is not initiated until 6 weeks after discharge. In this period, patients commonly experience psychological symptoms (e.g. anxiety, depression), have to deal with uncertainty and worry about what to expect (e.g. what level of postoperative pain is normal, is physical exercise allowed?) [6]. Recall of information provided perioperatively is often incomplete and patients do not always know who to contact in case of complaints. They will then search for (sometimes unreliable) information on surgery or recovery and reach out to different healthcare providers, who have a varying degree of expertise in CABG care. Conflicting advice on recovery can further increase fear and insecurity, which will eventually hamper the recovery process and contribute to unplanned healthcare utilisation [7, 8].
We hypothesise that restructuring the postoperative period with an eHealth strategy will reduce unplanned healthcare utilisation through improved mental and physical health and faster recovery. In the IMPROV-ED trial, we aim to evaluate whether the use of an eHealth programme that consists of educational videos developed by the Dutch Heart Foundation (Hartstichting) and video consultations, is more effective than standard care in the reduction of unplanned healthcare utilisation and the improvement of patient outcomes in the first 6 weeks after CABG. In addition, a process and patient satisfaction evaluation of the newly developed eHealth strategy will be conducted.
Methods
Study setting
This randomised trial is conducted at the Catharina Hospital in the Netherlands. The trial will be reported in accordance with relevant sections from the Standard Protocol Items: Recommendations for Interventional Trials [9], and the Consolidated Standards of Reporting Trials of Electronic and Mobile Health Applications and Online Telehealth. The study was approved by the local medical ethics committee (registration number R19.100) and is registered in the Netherlands Trial Registry (www.trialregister.nl, number NL8510).
Recruitment and allocation
All patients planned for preoperative outpatient counselling for CABG will be contacted by telephone in the week of their scheduled appointment. Patient eligibility for the trial will be assessed according to prespecified inclusion criteria (Tab. 1). Eligible patients will be informed about the study protocol by one of the investigators after their scheduled appointment. If the patient is willing to participate, the informed consent form is signed. At inclusion, patients are randomised to either the intervention or control group in a ratio 1:1 using block randomisation, with a block size of four.
Interventions
Control group
Patients randomised to the control group will receive standard care according to the local protocol. One month prior to surgery, patients are invited to the preoperative outpatient clinic, where they are individually counselled by a physician and a nurse practitioner. They are also handed information brochures after a nurse-led group session during which they receive information on the CABG care process at our hospital.
After surgery, patients have an in-hospital physiotherapist consultation. Before discharge, a resident or nurse provides brief information about the permitted level of physical activity and the medication schedules and answers remaining questions patients might have. Outpatient postoperative follow-up is scheduled for 6 weeks after discharge. Structured guidance to improve general condition and strength by a physiotherapist is offered (cardiac rehabilitation). Patients have no planned care in the first 6 weeks after discharge.
Intervention group
Aside from standard care as described in the previous section, patients in the intervention group will have access to educational videos and will be invited to two video consultations. Access will be granted through a link sent by email. The educational videos will be made available directly after randomisation for the duration of the study, via a secure online portal. The portal provides an orderly index in which patients can navigate by means of preformulated questions stratified in three categories: treatment, recovery and healthy living (Fig. 1). Each question will be accompanied by an educational video, which provides information and practical advice if applicable (Fig. 2).
The aim of the videos is to prepare patients, and their caregivers and family members for the surgery and offer guidance during the recovery process. The videos were developed by the Dutch Heart Foundation and were made available specifically for this study. Videos contain spoken text with animations (Figs. 3 and 4); all information is in Dutch. A nurse practitioner experienced in care for cardiothoracic surgery patients will conduct the video consultations with patients on their recovery and any complaints. Supervision will be provided by a cardiothoracic surgeon. The nurse practitioner will be told the study’s aim is to ‘improve the current follow-up procedure’ and that he or she will therefore be blinded for the specific outcomes.
Outcomes
Primary outcome measure
The primary outcome is the volume of unplanned healthcare utilisation (resources used per patient). Healthcare utilisation is defined as a composite endpoint of all emergency department visits, outpatient clinic visits, rehospitalisation, patient-initiated telephone consultations with a physician or nurse, and visits to a general practitioner, allied health professionals and psychologists.
An adaptation of the Institute for Medical Technology Assessment Medical Consumption Questionnaire (iMCQ) will be used to determine the volume of healthcare utilisation and the reasons thereof. This generic questionnaire aims to determine the costs of healthcare based on care consumption and is applicable to the Dutch healthcare system [10]. The questionnaire answers will result in absolute frequencies of visits for the relevant care activities. When patients report the use of healthcare, their healthcare provider will be contacted to validate the date and the reason for the healthcare encounter. This information will be crossvalidated with the subjects’ self-reports.
Secondary outcome measures
Secondary outcome measure are defined as the individual care activities of unplanned healthcare utilisation, a composite endpoint of consultations with a general practitioner, allied health professionals and psychologists plus patient-initiated telephone consultations with a physician or nurse, and a composite endpoint of in-hospital care (emergency department visits, outpatient clinic visits, rehospitalisation).
Tertiary outcome measures
Tertiary outcome measures are the patients’ quality of life and their mental and physical status. To assess these domains, the 36-Item Short Form Health Survey (SF-36) [11], the anxiety subscale of the Hospital Anxiety and Depression Scale (HADS) [12] and an adaptation of the Recovery Index-10 (RI-10) [13] will be used at different time points during follow-up (Tab. 2).
The SF-36 is routinely used at our facility and has been validated in multiple patient populations, including cardiac surgery patients [14,15,16,17,18]. This questionnaire assesses health-related quality of life in the previous 4 weeks. The HADS questionnaire is widely validated and is most commonly used to assess depression or anxiety. The RI-10 is a short, Dutch-language, 10-item questionnaire measuring postoperative domains on a 5-point scale over the last 7 days. It has been validated in gynaecology patients, but the general nature of the questions suits our patient population [19].
Process measures
The performance of the eHealth strategy on several domains will be structurally evaluated using qualitative and quantitative measures [20, 21]. The process evaluation will assess participant attitude, eligibility, access, usage and engagement of the eHealth strategy (Tab. 3), in order to make recommendations on the development and subsequent implementation of eHealth strategies. Data will originate from the internet usage log of the portal and the patient satisfaction questionnaire.
Patient and procedural data
Patient characteristics (age, sex, comorbidities), procedural characteristics (in-hospital complications, length of stay, duration of surgery), follow-up data (mortality, reoperations, deep sternal wound infections, stroke, recurrent myocardial infarction within 30 days) and sociodemographic information will be collected and analysed to provide insight into our patient population and to adjust endpoints if necessary. Patient, procedural and follow-up data are routinely collected at our facility and are defined by the Netherlands Heart Registry [22]. Sociodemographic data are part of the iMCQ.
Data collection
Data will be collected using paper questionnaires at the following time points: 1 month before surgery (T0), 1 week after surgery (T1), 2 weeks after surgery (T2), 3 weeks after surgery (T3), 6 weeks after surgery (T4), 2 months after surgery (T5) and 6 months after surgery (T6) (Tab. 2). If patients do not return two subsequent questionnaires, they will be contacted and kindly requested to fill in and return the next questionnaires. Video consultation will be scheduled for 1 and 3 weeks after surgery.
Statistical considerations
Data analysis
Descriptive statistics will be used to summarise baseline characteristics of the study population. Healthcare utilisation will be expressed as mean ± standard deviation (resource use per patient) and absolute and relative frequencies (users per resource). Mann-Whitney U test and Fisher exact test will be used to compare the intervention and control group. Multivariate regression analysis will be performed to adjust the outcomes for confounding factors based on univariate analysis (p < 0.1), literature review and expert opinion.
The primary analysis will be an intention-to-treat analysis. In the secondary analysis, we will compare the control group with the intervention group that used the educational videos at least once and completed the video consultations (‘users only’). A p-value <0.05 will be considered statistically significant and all analyses will be performed using SPSS 25 (SPSS Inc., Chicago, IL, USA).
Sample size calculation
Studies on eHealth in CABG patients and the effect on healthcare utilisation are scarce and report users per resource [23]. Our primary objective is to reduce healthcare utilisation per patient. To our knowledge, in one study, healthcare utilisation per patient was estimated using the iMCQ at 0.88 ± 0.15.[24] Under the assumption of a small or medium effect of our eHealth strategy (d = 0.35), an α of 0.05 and a power of 0.80, a total sample size of 260 patients is required. The total study population is set at 280 patients (140 patients per arm) to account for loss to follow-up and nonadherence to the intervention.
Expected results
The IMPROV-ED trial will be carried out to evaluate whether an eHealth initiative consisting of online education and video consultation can reduce healthcare utilisation by improving quality of life, decreasing anxiety and accelerating recovery within the first 6 weeks after discharge for CABG.
Discussion
The IMPROV-ED trial is of clinical significance for several reasons. First, we will evaluate the influence of an eHealth strategy on healthcare utilisation, anxiety, quality of life and recovery. Positive results will yield a new postoperative protocol that will lead to better patient outcomes and reduced costs [25]. In addition, the process and patient satisfaction evaluation will show the readiness of CABG patients for structured eHealth initiatives and will evaluate the currently used content and mode of administration, given the broad applicability of eHealth in general and the multitude of devices available [26,27,28]. Second, the control arm of the trial will provide the first detailed insight into unplanned, transmural healthcare utilisation in the early postoperative period after CABG and will thereby show how to further improve post-CABG protocols, aside from eHealth, through multidisciplinary regional collaboration.
eHealth strategies in CABG patients have been successfully applied to guide secondary prevention [29], to improve recovery [30, 31], and to assess physical functioning and quality of life [32,33,34]. Although evidence on the effect of eHealth on healthcare utilisation in CABG patients is minimal, it is reasonable to expect a positive effect based on reduction of healthcare utilisation by eHealth strategies in other populations [8, 23, 35, 36]. According to post-CABG protocols, patients are expected to adopt new behaviours (e.g. relieve stress on the sternum, gradually increase in physical exercise, follow healthy diet) and to deal with the emotions and worries that go with cardiac surgery through self-management, and, thus, to take responsibility for their own recovery [6]. eHealth has shown to be a useful method for patients to enhance their self-management through better understanding of their disease, increased independence and improved acceptance to adhere to lifestyle advice [37]. The educational videos in our eHealth strategy facilitate self-management. By means of video consultation, the physician can guide and supervise the patient’s progress and maintain a good patient-physician relationship, which has been shown to enhance the patient’s self-management skills [37].
The message and content of the educational videos were designed in such a way that they provide health information for patients with low/inadequate health literacy (approximately 36.4% of the general population in the Netherlands [38]), without compromising health communication to patients with adequate health literacy. Meppelink et al. have assessed the features of health information (written vs spoken text vs animations vs illustrations) and concluded that spoken text combined with animation is the most effective way to communicate health information and that it suits both patients with low health literacy and those with adequate health literacy [39]. In addition, to prevent cognitive overload, it is advised to only offer information when it is applicable to the patient’s situation instead of presenting all the information at once, especially to not overburden low health literate patients [40]. We therefore decided to divide the information into the three main phases of CABG recovery (Fig. 2).
Limitations
The addition of our eHealth strategy to the postoperative protocol might yield additional costs in comparison to standard care. We believe that these additional costs will be balanced by reduced healthcare utilisation and will therefore result in less total costs and better patient outcomes. Another potential limitation is that we will only include patients that have sufficient computer and digital literacy skills and have access to a computer or tablet, which might diminish generalisability of our study protocol. Moreover, as in most eHealth research, our trial is not fully blinded, which could lead to bias when patients report healthcare utilisation.
References
Nederlandse Hart Registratie. Nederlandse Hart Registratie 2018. 2018;(april 2019):249. Available from: https://nederlandsehartregistratie.nl/wp-content/uploads/2018/12/NHR_Publicatie_Registratie_2018.pdf
Ferguson TB, Peterson ED, Coombs LP, et al. Use of continuous quality improvement to increase use of process measures in patients undergoing coronary artery bypass graft surgery: a randomized controlled trial. J Am Med Assoc. 2003;290:49–56.
Swaminathan M, Phillips-Bute BG, Patel UD, et al. Increasing healthcare resource utilization after coronary artery bypass graft surgery in the United States. Circ Cardiovasc Qual Outcomes. 2009;2:305–12.
Hannan EL, Zhong Y, Lahey SJ, et al. 30-Day readmissions after coronary artery bypass graft surgery in New York State. JACC Cardiovasc Interv. 2011;4:569–76.
Shah RM, Zhang Q, Chatterjee S, et al. Incidence, cost, and risk factors for readmission after coronary artery bypass grafting. Ann Thorac Surg. 2019;107:1782–9.
Lie I, Bunch EH, Smeby NA, Arnesen H, Hamilton G. Patients’ experiences with symptoms and needs in the early rehabilitation phase after coronary artery bypass grafting. Eur J Cardiovasc Nurs. 2012;11:14–24.
Pedoto A, Perrino AC. Delayed recovery following thoracic surgery: persistent issues and potential interventions. Curr Opin Anaesthesiol. 2019;32:3–9.
Talboom-Kamp EP, Verdijk NA, Harmans LM, Numans ME, Chavannes NH. An eHealth platform to manage chronic disease in primary care: an innovative approach. Interact J Med Res. 2016;5:e5.
Chan AW, Tetzlaff JM, Altman DG, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158:200–7.
Bouwmans C, Hakkaart-van Roijen L, Koopmanschap M, Krol M, Severens H, Brouwer W. Productivity costs questionnaire. 2013. https://docplayer.nl/60086739-Medical-consumption-questionnaire-productivity-and-health-research-group.html, last access: 15-04-2020, Productivity and Health Research Group. Inst Med Technol Earsmus Univ Rotterdam.
Sanderman R, van der Zee KI. Het meten van de algemene gezondheidstoestand met de Rand-36. 2012. https://www.umcg.nl/SiteCollectionDocuments/research/institutes/SHARE/assessmenttools/handleiding_rand36_2e_druk.pdf, last access: 15-04-2020, Res Inst SHARE.
Spinhoven P, Ormel J, Sloekers PPA, Kempen GIJM, Speckens AEM, Van Hemert AM. A validation study of the hospital anxiety and depression scale (HADS) in different groups of Dutch subjects. Psychol Med. 1997;27:363–70.
Kluivers KB, Hendriks JCM, Mol BWJ, et al. Clinimetric properties of 3 instruments measuring postoperative recovery in a gynecologic surgical population. Surgery. 2008;144:12–21.
Jensen BØ, Hughes P, Rasmussen LS, Pedersen PU, Steinbrüchel DA. Health-related quality of life following off-pump versus on-pump coronary artery bypass grafting in elderly moderate to high-risk patients: a randomized trial. Eur J Cardiothorac Surg. 2006;30:294–9.
Goldsmith IRA, Lip GYH, Patel RL. A prospective study of changes in the quality of life of patients following mitral valve repair and replacement. Eur J Cardiothorac Surg. 2001;20:949–55.
Hansen L, Winkel S, Kuhr J, Bader R, Bleese N, Riess FC. Factors influencing survival and postoperative quality of life after mitral valve reconstruction. Eur J Cardiothorac Surg. 2010;37:635–44.
Santini F, Montalbano G, Messina A, et al. Survival and quality of life after repair of acute type A aortic dissection in patients aged 75 years and older justify intervention. Eur J Cardiothorac Surg. 2006;29:386–91.
Koertke H, Hoffmann-Koch A, Boethig D, et al. Does the noise of mechanical heart valve prostheses affect quality of life as measured by the SF-36® questionnaire? Eur J Cardiothorac Surg. 2003;24:52–8.
van der Meij E, Huirne JA, Bouwsma EV, et al. Substitution of usual perioperative care by eHealth to enhance postoperative recovery in patients undergoing general surgical or gynecological procedures: study protocol of a randomized controlled trial. JMIR Res Protoc. 2016;5:e245.
Lilford RJ, Foster J, Pringle M. Evaluating eHealth: how to make evaluation more methodologically robust. PLoS Med. 2009;6:e1000186.
Cissell WB. Process evaluation for public health interventions and research. Health Educ Res. 2004;19:739.
Nederlandse Hart Registratie. NHR Handboek. 2019. Available from: www.nederlandsehartregistratie.nl.
Van der Meij E, Anema JR, Otten RHJ, Huirne JAF, Schaafsma FG. The effect of perioperative e‑health interventions on the postoperative course: a systematic review of randomised and non-randomised controlled trials. PLoS One. 2016;11:1–24.
Pattamatta M, Smeets BJJ, Evers SMAA, Peters EG, Luyer MDP, Hiligsmann M. Quality of life and costs of patients prior to colorectal surgery. Expert Rev Pharmacoecon Outcomes Res. 2020;20:193–8.
Porter M. What is value in health care?—Supplementary appendix 2. N Engl J Med. 2010;363:1–3.
Piepoli MF, Hoes AW, Agewall S, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice. The sixth joint task force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice. G Ital Cardiol (Rome). 2017;18:547–612.
Frederix I, Caiani EG, Dendale P, et al. ESC e‑cardiology working group position paper: overcoming challenges in digital health implementation in cardiovascular medicine. Eur J Prev Cardiol. 2019;26:1166–77.
Pagliari C, Sloan D, Gregor P, et al. What is eHealth (4): a scoping exercise to map the field. J Med Internet Res. 2005;7:e9.
Brørs G, Pettersen TR, Hansen TB, et al. Modes of e‑Health delivery in secondary prevention programmes for patients with coronary artery disease: a systematic review. BMC Health Serv Res. 2019;19:364.
Miller C, Zimmerman L, Barnason S, Nieveen J. Impact of an early recovery management intervention on functioning in postoperative coronary artery bypass patients with diabetes. Heart Lung. 2007;36:418–30.
Zimmerman L, Barnason S, Nieveen J, Schmaderer M. Symptom management intervention in elderly coronary artery bypass graft patients. Outcomes Manag. 2004;8:5–12.
Körtke H, Stromeyer H, Zittermann A, et al. New East-Westfalian postoperative therapy concept: a telemedicine guide for the study of ambulatory rehabilitation of patients after cardiac surgery. Telemed J E Health. 2006;12:475–83.
Barnason S, Zimmerman L, Nieveen J, et al. Influence of a symptom management telehealth intervention on older adults’ early recovery outcomes after coronary artery bypass surgery. Heart Lung. 2009;38:364–76.
Torrance GW. Preferences for health outcomes and cost-utility analysis. Am J Manag Care. 1997;3:S8–S20.
Lorig KR, Ritter P, Stewart AL, et al. Chronic disease self-management program: 2‑year health status and health care utilization outcomes. Med Care. 2001;39:1217–23.
Steventon A, Bardsley M, Billings J, et al. Effect of telehealth on use of secondary care and mortality: findings from the Whole System Demonstrator cluster randomised trial. BMJ. 2012;344:e3874.
Lorig KR, Holman HR. Self-management education: History, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26:1–7.
Sørenson K, Van den Broucke S, Fullam J, et al. (HLS-EU). Consortium Health Literacy Project Europe. Health Literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;25:1053–8.
Meppelink CS, Van Weert JCM, Haven CJ, Smit EG. The effectiveness of health animations in audiences with different health literacy levels: an experimental study. J Med Internet Res. 2015;17:e11.
Heijmans M, Zwikker H, van der Heide I, Rademakers J. NIVEL Kennisvraag 2016: zorg op maat. Hoe kunnen we de zorg beter laten aansluiten bij mensen met lage gezondheidsvaardigheden? Utrecht: NIVEL; 2016.
Acknowledgements
The Dutch Heart Foundation provided the online educational videos and contextMe provided the platform by which video consultation was facilitated.
Funding
This work was supported by the Dutch Heart Foundation and contextMe. Each party was responsible for the quality assurance, maintenance and dispersion of its intellectual property. Thus, neither sponsor provided reimbursement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
G.J. van Steenbergen, D. van Veghel, J. ter Woorst, D. van Lieshout and L. Dekker declare that they have no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van Steenbergen, G.J., van Veghel, D., ter Woorst, J. et al. IMPROV-ED trial: eHealth programme for faster recovery and reduced healthcare utilisation after CABG. Neth Heart J 29, 80–87 (2021). https://doi.org/10.1007/s12471-020-01508-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12471-020-01508-9