Abstract
Background
Despite proven clinical benefits, only a minority of patients complete outpatient cardiac rehabilitation (CR) after acute myocardial infarction (AMI). The main purpose of this study was to evaluate to what extent and at which time patients drop out of CR, and to assess which patient-related characteristics can predict dropout.
Methods
In a retrospective cohort study, we selected patients who had been hospitalised with an AMI in our centre in 2015 or 2016. Patients were selected pseudonymously based on reimbursement codes in the electronic health record. We extracted baseline characteristics and data on CR referral, enrolment and completion for each patient. Multivariable logistic regression was used to assess which characteristics predicted referral and dropout.
Results
The 666 patients included were predominantly male (66%), with a mean age of 69.0 years. Of the 640 eligible patients, 201 (31%) were not referred for CR. Enrolment after referral was 94%. Nonreferral was independently associated with older age, female sex, traveling distance, non-ST-elevation myocardial infarction (NSTEMI; as compared with STEMI), no coronary revascularisation and prior manifestations of coronary artery disease. Of the 414 enrolled patients, 24% did not complete their CR programmes (i.e. dropped out). Older age and worse exercise capacity at baseline were independently associated with dropout. The ability of the multiple regression models to predict nonreferral and noncompletion was good to fair, with an area under the receiver operating characteristic curves of 0.86 and 0.71, respectively.
Conclusion
The main reason for not participating in or not completing CR after AMI was nonreferral. To optimise CR utilisation, improvement of referral rates should be prioritised.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
-
The main reason for not participating in or not completing cardiac rehabilitation (CR) after acute myocardial infarction was nonreferral.
-
Although dropout after referral was lower, more than half of discharged patients ultimately did not complete a CR programme.
-
To optimise CR utilisation, improvement of referral rates should have priority, focusing on elderly patients and women, and on patients with non-ST-elevation myocardial infarction, without coronary revascularisation or with prior manifestations of coronary artery disease.
-
Alternative models of CR, such as cardiac telerehabilitation, should be considered to improve CR enrolment and completion.
Introduction
Cardiac rehabilitation (CR) reduces cardiovascular morbidity and mortality and increases quality of life in patients after acute myocardial infarction (AMI) [1,2,3]. Therefore, CR is strongly recommended in American and European guidelines [4,5,6,7]. Still, less than half of eligible patients with AMI or other manifestations of coronary artery disease (CAD) participate in outpatient CR [8]. Low participation rates are caused by suboptimal referral by medical professionals and unsatisfactory enrolment of patients after referral [9]. After enrolment, up to one-third of participants do not complete their CR programmes [10]. Even though low CR participation and completion rates are well studied and improved uptake has been proven beneficial in cost-benefit analyses [11, 12], detailed recommendations on strategies to improve these rates are lacking in current guidelines.
Not participating or not completing CR is associated with a wide range of factors at the patient level, healthcare professional level and (healthcare) system level [13, 14]. Examples of these factors include demographic or disease-specific factors (patient level), physician CR endorsement (professional level) and financial or geographic factors (system level). While not participating and dropout of CR are associated with a doubled risk for cardiovascular events or death [15], nonparticipation and dropout are more often seen in older and high risk patients (i.e. patients with cardiovascular risk factors or lower socioeconomic status) [16,17,18]. As this may even further increase their cardiovascular risks, it is of eminent importance to understand why and at which times during a CR programme these patients drop out.
Despite a growing body of evidence on interventions to increase CR utilisation, the percentage of participating patients has not increased in Europe in the past 7 years [8]. To identify the weakest link in the CR care pathway—and thus the primary target for improvement—it is important to chart the entire pathway, and not to solely focus on CR referral or completion. Therefore, the objective of this study was to evaluate at which time (from hospital discharge to CR completion) patients drop out of CR, and to assess which patient-related characteristics can predict dropout.
Methods
Study design
In this retrospective cohort study, we selected patients who had been hospitalised with an AMI in our Department of Cardiology between 1 January 2015 and 31 December 2016. Patients were selected pseudonymously based on reimbursement codes in the electronic health record (EHR) and data were extracted using the EHR Data Platform version 1.2.10 from CTcue (Amsterdam, the Netherlands) [19]. The study design was approved by the Medical Ethics Review Committee of Máxima Medical Center Veldhoven, the Netherlands.
Study population and follow-up
We selected patients who had been hospitalised in our centre with a non-ST-elevation myocardial infarction (NSTEMI) or ST-elevation myocardial infarction (STEMI). Patients who already participated in outpatient CR at the time of hospitalisation, were excluded from all analyses, as this would likely influence participation in a new CR programme. Follow-up after the index event (i.e. hospitalisation for AMI) was maximised at 12 months, to minimise the possibility of incorrectly attributing components of a second CR programme to the index event.
Cardiac rehabilitation programme
During the study period, patients with AMI were semiautomatically referred for CR at the time of hospital discharge by the treating physician via the EHR. When the EHR registered that a patient was hospitalised with an AMI, the physician received an automatic notification that CR was advised for that patient. At discharge, the physician then created a partly prefilled CR referral form in the EHR, containing relevant clinical characteristics, in order to refer the patient. This semiautomatic referral strategy was combined with advice (liaison) by nurses on the ward.
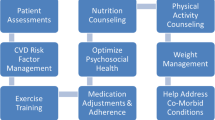
Following the current Dutch CR guideline [20], patients referred for CR after AMI were offered an individualised outpatient programme of 12 weeks, consisting of one or more group-based therapies (i.e. exercise training, education, relaxation therapy, psychoeducative prevention therapy, smoking cessation therapy) and/or individual treatment by a psychologist, dietician or social worker. The content of a patient’s programme was based on an individual needs assessment [21]. After 3 months, the programme was evaluated at the outpatient clinic.
Data extraction
For each patient, demographic, geographic and clinical characteristics were collected at baseline (i.e. hospitalisation or, if applicable, start of the CR programme). For patients attending the programme, data from the individual needs assessment [21] were also collected. This included data on exercise testing, marital and employment status, and questionnaires on health-related quality of life (Kwaliteit van Leven bij Hartpatiënten, a validated Dutch translation of the MacNew Heart Disease Health-Related Quality of Life Questionnaire), anxiety (Generalized Anxiety Disorder 7‑item Scale) and depression (Patient Health Questionnaire-9) [21].
Outcome measures
Outcome measures were CR referral, enrolment (attending the intake procedure), attendance at one or more therapies, and programme completion (attending the evaluation procedure after 12 weeks).
Statistical analysis
Continuous variables are reported as mean ± standard deviation when normally distributed or as median and interquartile range when not normally distributed. Categorical variables are presented as number and percentage. If the presence or absence of cardiovascular risk factors or prior manifestations of CAD was not documented (i.e. data were missing), we assumed they were absent. We analysed differences in baseline characteristics between patients for the outcome measures using the chi-squared test or (if the expected cell count for a variable was less than five) the Fisher’s exact test for categorical variables, and the independent samples t-test or (if the variable was not normally distributed) the Mann-Whitney U test for continuous variables. Statistical tests were two-tailed, and p-values were considered statistically significant when p < 0.05.
Variables for which a statistically significant between-group difference (p < 0.05) was found in univariate analysis, were used in multivariable logistic regression analyses to assess which variables were associated with the outcome measures (complete-case analysis). Because of the explorative design of the study, we used backwards stepwise multivariable logistic regression to calculate the odds ratio and 95% confidence interval for each variable. For each multivariable model, we plotted a receiver operating characteristic (ROC) curve and calculated the area under the curve to assess its discriminative ability. Statistical analyses were performed using SPSS Statistics version 22 (IBM Corp. Armonk, NY, USA).
Results
In 2015 and 2016, 666 patients were hospitalised with a NSTEMI (65%) or STEMI (35%). Patients were predominantly male (66%), with a mean age of 69.0 ± 12.8 years. Twenty patients died during hospitalisation and 6 already participated in outpatient CR at the time of hospitalisation. Data of the remaining 640 patients were analysed.
Dropout during CR
In total, 201 out of the 640 included patients (31%) were not referred for CR. Of the 439 referred patients, 25 (6%) did not enrol. Of the 414 enrolled patients, 43 (10%) did not attend any therapies, and of the 371 patients attending one or more therapies, 58 (16%) did not attend the evaluation procedure. A total of 313 patients (49% of eligible patients and 71% of those referred) completed a CR programme (Fig. 1).
Predictors of referral
Patients who were not referred for CR were older, more often female, had a longer traveling distance to the CR centre, more often presented with NSTEMI (as compared with STEMI), were less often revascularised and more often had prior manifestations of CAD (Tab. 1). All these variables were independently associated with nonreferral (Tab. 2). The chance of nonreferral was 1.7 times higher in women, 2.2 times higher for patients with NSTEMI and 11 times higher for patients who were not revascularised. The area under the ROC curve for the multiple regression model including these variables was 0.86, indicating good discriminatory ability (Fig. 2a).
Predictors of enrolment
Of the referred patients, 6% did not enrol in CR and did not attend the intake procedure at the outpatient clinic. Median waiting time (time between hospital discharge date and date of planned intake procedure) in the entire cohort was 11 days, without between-group differences for patients who enrolled or did not enrol. There were also no between-group differences in waiting time for patients who completed or did not complete CR (Tab. 1). Patients who did not enrol were older and were less often revascularised. The area under the ROC curve for this model was 0.76, indicating fair discriminatory ability (Fig. 2b).
Predictors of completion
Of the patients enrolled in CR, 24% did not complete their CR programmes (i.e. dropped out). Patients who dropped out were older and more often had hypertension, diabetes mellitus and prior manifestations of CAD (Tab. 1). They also had worse exercise capacity at baseline, were less often employed and had a worse quality of life. Characteristics independently associated with dropout were older age and worse exercise capacity (Tab. 2). The area under the ROC curve for this model was 0.71, indicating fair discriminatory ability (Fig. 2c).
Attendance at group-based and individual therapies
Of the 414 patients enrolled in CR, 47% attended the education sessions, 90% attended the exercise training programme, 9% attended relaxation therapy and 5% attended psychoeducative prevention therapy. Regarding individual therapies, 25% visited a dietician (at least one visit) and 8% visited a psychologist (at least one visit).
Discussion
In this study, nonreferral was the most important reason for not completing a CR programme after AMI. One-third of patients were not referred, and although dropout after referral was lower, more than 50% of discharged patients ultimately did not complete a CR programme. We found older age, female sex, traveling distance, NSTEMI, no coronary revascularisation and prior manifestations of CAD to be independently associated with nonreferral, which is in line with previous studies [22, 23].
The reason why several subgroups of patients are referred less often is only partly understood. Several studies have suggested that some physicians believe women or elderly patients will benefit less from CR [24, 25]. For patients with NSTEMI or without coronary revascularisation, the perceived benefit of CR may also be lower. In this case, however, limited capacity at CR facilities or lack of reimbursement for specific subgroups may also lead to lower referral rates [24], although the available evidence provides no reason for not referring these subgroups [26]. For elderly patients, transport and mobility issues may influence CR participation or willingness to be referred, as do social obligations, providing informal care or a belief that they may not benefit from CR. Widespread implementation of fully automatic referral strategies (including a mandatory justification in case a patient is not referred) may reduce selective referral, leading to improved referral rates. Besides, education of both patients and healthcare professionals on the benefits of CR may improve their motivation and attitudes towards CR and may reduce prejudices that CR is less effective in certain subgroups.
The participation rate in our cohort was 58% (371 out of 640 eligible patients started one or more therapies), which is higher than it was in recent studies [8, 18]. This may be due to differences in the definition of participation and the methods of data collection (e.g., EHR or survey data), and the possibility that participation rates have increased over time. Completion rates in our population were comparable to those in previous studies, although different definitions of completion were used [10, 18]. We found older age and worse exercise capacity at baseline to be independently associated with CR dropout. Low exercise capacity may be caused by comorbidity, which we could only partially correct for in our analyses. However, as low exercise capacity is associated with worse prognosis [27], it is even more important for these patients to participate in a multidisciplinary secondary prevention programme.
Although it seems that improving referral should have priority when aiming to increase CR utilisation, optimisation of enrolment, adherence and completion should not be overlooked. A recent Cochrane review, however, has only found limited evidence for interventions improving participation in and adherence to CR [28]. Home-based CR or cardiac telerehabilitation (CTR) is a safe and (cost-)effective alternative to centre-based CR [29], and future research should indicate whether implementation of CTR indeed leads to increased participation and completion rates. Still, budget ceilings may limit this potential increase in CR utilisation, even with full reimbursement for CR. Updated economic analyses, such as those by Frederix [11] and De Gruyter [12], are therefore needed to convince health insurers and policy makers of the benefits and return on investment of CR.
Strengths and limitations
This study is the first to assess CR participation and dropout in the entire care pathway from hospital discharge after AMI to CR completion. Another strength is the fact that our data reflect referral, enrolment and completion in actual practice instead of being part of a prospective trial, in which selection bias may occur.
However, due to the retrospective nature of our study and the use of CTcue, we could not register data on socioeconomic status, contraindications or physician endorsement for CR, and reasons for nonreferral or dropout. Second, data on cardiovascular risk factors could not be reliably collected for patients who were not referred; therefore, these data were not used in analyses evaluating referral.
Conclusion
For patients discharged after AMI, the main reason for not participating in CR was nonreferral. To optimise CR utilisation, improvement of referral rates should have priority, focusing on elderly patients and women, and on patients with NSTEMI, without coronary revascularisation or with prior manifestations of CAD. To improve CR enrolment and completion, alternative models of CR, such as CTR, should be considered.
References
Anderson L, Thompson DR, Oldridge N, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2016;1:CD1800.
de Vries H, Kemps HM, van Engen-Verheul MM, et al. Cardiac rehabilitation and survival in a large representative community cohort of Dutch patients. Eur Heart J. 2015;36:1519–28.
Rauch B, Davos CH, Doherty P, et al. The prognostic effect of cardiac rehabilitation in the era of acute revascularisation and statin therapy: a systematic review and meta-analysis of randomized and non-randomized studies—the cardiac rehabilitation outcome study (CROS). Eur J Prev Cardiol. 2016;23:1914–39.
Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European society of cardiology (ESC). Eur Heart J. 2018;39:119–77.
Roffi M, Patrono C, Collet JP, et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European society of cardiology (ESC). Eur Heart J. 2016;37:267–315.
O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. J Am Coll Cardiol. 2013;61(4):e78–e140.
Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes. J Am Coll Cardiol. 2014;64(24):e139–e228.
Kotseva K, Wood D, De Bacquer D. Determinants of participation and risk factor control according to attendance in cardiac rehabilitation programmes in coronary patients in Europe: EUROASPIRE IV survey. Eur J Prev Cardiol. 2018;25:1242–51.
Ades PA, Keteyian SJ, Wright JS, et al. Increasing cardiac rehabilitation participation from 20 % to 70 %: a road map from the million hearts cardiac rehabilitation collaborative. Mayo Clin Proc. 2017;92:234–42.
McDonall J, Botti M, Redley B, et al. Patient participation in a cardiac rehabilitation program. J Cardiopulm Rehabil Prev. 2013;33:185–8.
Frederix I, Vandijck D, Hens N, et al. Economic and social impact of increased cardiac rehabilitation uptake and cardiac telerehabilitation in Belgium—a cost-benefit analysis. Acta Cardiol. 2018;73:222–9.
De Gruyter E, Ford G, Stavreski B. Economic and social impact of increasing uptake of cardiac rehabilitation services—a cost benefit analysis. Heart Lung Circ. 2016;25:175–83.
Grace SL, Gravely-Witte S, Brual J, et al. Contribution of patient and physician factors to cardiac rehabilitation enrollment: a prospective multilevel study. Eur J Cardiovasc Prev Rehabil. 2008;15:548–56.
Clark AM, King-Shier KM, Duncan A, et al. Factors influencing referral to cardiac rehabilitation and secondary prevention programs: a systematic review. Eur J Prev Cardiol. 2013;20:692–700.
Pardaens S, Willems AM, Clays E, et al. The impact of drop-out in cardiac rehabilitation on outcome among coronary artery disease patients. Eur J Prev Cardiol. 2017;24:1490–7.
De Vos C, Li X, Van Vlaenderen I, et al. Participating or not in a cardiac rehabilitation programme: factors influencing a patient’s decision. Eur J Prev Cardiol. 2013;20:341–8.
Wittmer M, Volpatti M, Piazzalonga S, et al. Expectation, satisfaction, and predictors of dropout in cardiac rehabilitation. Eur J Prev Cardiol. 2012;19:1082–8.
Sunamura M, Ter Hoeve N, Geleijnse ML, et al. Cardiac rehabilitation in patients who underwent primary percutaneous coronary intervention for acute myocardial infarction: determinants of programme participation and completion. Neth Heart J. 2017;25:618–28.
CTCUE. EHR data platform making medical data searchable and accessible, using a privacy by design approach. 2013. https://ctcue.com. Accessed 16 Nov 2018.
Netherlands Society of Cardiology/Netherlands Heart Foundation. Multidisciplinary guidelines for cardiac rehabilitation. Utrecht: Netherlands Society of Cardiology; 2011.
Netherlands Society of Cardiology. Beslisboom Poliklinische Indicatiestelling Hartrevalidatie 2012. Utrecht: Netherlands Society of Cardiology; 2012.
Cortes O, Arthur HM. Determinants of referral to cardiac rehabilitation programs in patients with coronary artery disease: a systematic review. Am Heart J. 2006;151:249–56.
Hermann M, Witassek F, Erne P, et al. Referral for cardiac rehabilitation after acute myocardial infarction: Insights from nationwide AMIS Plus registry 2005–2017. Int J Cardiol. 2018;261:1–5.
van Engen-Verheul M, de Vries H, Kemps H, et al. Cardiac rehabilitation uptake and its determinants in the Netherlands. Eur J Prev Cardiol. 2013;20:349–56.
Beckstead JW, Pezzo MV, Beckie TM, et al. Physicians’ tacit and stated policies for determining patient benefit and referral to cardiac rehabilitation. Med Decis Making. 2014;34:63–74.
Knuuti J, Wijns W, Saraste A, et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41:407–77.
Vanhees L, Fagard R, Thijs L, et al. Prognostic significance of peak exercise capacity in patients with coronary artery disease. J Am Coll Cardiol. 1994;23:358–63.
Karmali KN, Davies P, Taylor F, et al. Promoting patient uptake and adherence in cardiac rehabilitation. Cochrane Database Syst Rev. 2014;6:CD7131.
Anderson L, Sharp GA, Norton RJ, et al. Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst Rev. 2017;6:CD7130.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
R.W.M. Brouwers, V.J.G. Houben, J.J. Kraal, R.F. Spee and H.M.C. Kemps declare that they have no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Brouwers, R.W.M., Houben, V.J.G., Kraal, J.J. et al. Predictors of cardiac rehabilitation referral, enrolment and completion after acute myocardial infarction: an exploratory study. Neth Heart J 29, 151–157 (2021). https://doi.org/10.1007/s12471-020-01492-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12471-020-01492-0