Abstract
Aim
This study sought to assess whether radial artery access improves clinical outcomes in patients presenting with acute myocardial infarction compared with femoral artery access.
Methods
This is a single-centre, prospective observational registry of all STEMI and NSTEMI patients who underwent coronary angiography and/or primary PCI in the period January 2010 to December 2013. Primary endpoint was 30-day all-cause mortality. Choice of access was left to the discretion of the cardiologist. Differences in the risk of death at 30 days between patients undergoing transradial intervention versus transfemoral intervention was assessed on an intention-to-treat comparison.
Results
Retrospective analysis of prospectively collected data was performed in 3580 patients with an acute coronary syndrome who underwent coronary angiography, of which 1310 had radial artery access. PCI was performed in 77 % of the patients. Before propensity score matching, patients who underwent transradial intervention and those intended to undergo transfemoral approach differed significantly in intra-aortic balloon pump use (1.7 % vs. 6.7 %, p < 0.001), and Killip class (Killip 1: 10.8 % vs. 17.3 %, p < 0.001). 30-day mortality rates were 1.7 % in the transradial group and 4.6 % in the transfemoral group (p < 0.001). After matching on the propensity score, the hazard ratio for 30-day mortality in the transradial group was 0.56 (95 % CI: 0.29–1.07, p = 0.08).
Conclusion
This registry-based study showed that radial access is associated with improved outcome in patients with an acute coronary syndrome. However, this difference was no longer significant after multivariate and propensity score adjustment for differences in baseline characteristics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In patients with acute coronary syndrome (ACS), early and complete restoration of blood flow has been shown to improve long-term outcomes [1, 2]. For both diagnostic coronary angiography and percutaneous coronary intervention (PCI) a transradial approach to vascular access (transradial intervention) is rapidly becoming preferable to traditional transfemoral intervention [3, 4]. Myocardial infarction (MI) and PCI-related bleeding have been strongly associated with early and late mortality [5–9]. The use of radial access has been demonstrated to be feasible in the ACS setting and, compared with femoral access, a reduction in vascular complications and bleeding has been suggested [10, 11]. Whether this evident reduction in access-site bleeding may also have a positive impact on prevention of further cardiovascular events remains to be defined. The available clinical evidence summarised in a recent meta-analysis seems to suggest that the radial approach could also be associated with improved outcome [12]. It is possible that mortality and ischaemic events may also be reduced by this technique. The primary aim of this observational study was to evaluate the effect of radial artery access on 30-day all-cause mortality in an unselected all-comer ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation myocardial infarction (NSTEMI) population who were undergoing coronary angiography in a high-volume cardiothoracic centre.
Methods
All consecutive STEMI and NSTEMI patients undergoing coronary angiography at Isala, Zwolle in the Netherlands between January 2010 and December 2013 were included. STEMI patients were defined as those presenting with ischaemic symptoms >30 min with ST-segment elevation of >2 mm in two contiguous precordial leads or >1 mm in two contiguous limb leads or new left bundle branch block. NSTEMI was defined by the presence of ischaemic chest pain (or another complaint suggestive of ischaemia, such as shortness of breath of collapse), the notable absence of ST-segment elevation on electrocardiography, and the presence of either ST-segment depression or T‑wave inversion on electrocardiography and/or elevated cardiac biomarkers. All STEMI patients were directly transported to the catheterisation laboratory on arrival, and acute coronary angiography was performed with subsequent primary PCI when indicated. All NSTEMI patients were treated according to the current NSTEMI-ACS guidelines [13]. The decision to use radial or femoral access was at the discretion of the treating cardiologist. Patients who had a crossover of access were excluded from analysis. All patients were pre-treated with aspirin, heparin, and clopidogrel (600 mg loading dose), or ticagrelor (180 mg loading dose) during transportation to the hospital, or these drugs were administered in the emergency room. The use of glycoprotein (GP) IIb/IIIa inhibitors or bivalirudin was left to the operator’s discretion. There were no exclusion criteria with regard to age, sex, ischaemic time, cardiac history, or renal failure.
Study design
This was a prospective observational cohort study. Baseline demographics, clinical presentation, procedure details and procedural complications were collected by the performing physician at the end of each procedure. Post-procedural complications, clinical data and discharge medications were updated on discharge. Follow-up data of mortality during index hospital admission (in-hospital) and 30-day mortality were collected at the routine outpatient visit or by telephone interview of the patient by research personnel. The primary outcome measure was 30-day all-cause mortality.
Major bleeding was defined as either intracranial bleeding or overt bleeding with a decrease in haemoglobin ≥5 g/dl (≥3.1 mmol/l) or a decrease in haematocrit ≥15 % within 30 days after admission. Minor bleeding was defined as identified bleeding with a decrease in haemoglobin ≥3 g/dl (≥1.9 mmol/l), or >10 % decrease in haematocrit [14].
Statistics
Because the patients were not randomly assigned to undergo transradial intervention, a propensity score analysis was performed by using a logistic regression model for transradial versus transfemoral intervention to adjust for differences in baseline characteristics [15]. This analysis included a number of clinical, angiographic, and procedural variables: age, sex, hypertension, STEMI, out-of-hospital cardiac arrest (OHCA), ischaemic time (onset of symptoms to angiogram), year of procedure, previous coronary artery bypass grafting (CABG), PCI performed, P2Y12 inhibitors during acute phase, heparin during acute phase, GP IIb/IIIa inhibitors during acute phase, intra-aortic balloon pump (IABP), Killip >1, previous PCI, family history, previous MI, previous cerebrovascular accident. Patients in the transradial group were matched to patients in the transfemoral group with the closest propensity score. Only pairs of patients in which the difference between propensity scores was <0.2 were selected. After all the propensity score matching was performed, we compared the baseline covariates between the two intervention groups. Continuous variables were compared using the paired T‑test or the Wilcoxon signed-rank test, as appropriate, and categorical variables were compared using McNemar’s test. The statistical significance and the effect of treatment on outcomes were estimated using appropriate statistical methods for matched data. In the propensity score-matched cohort, the risks of each outcome were compared using Cox regression models which accounted for the clustering of matched pairs. Survival curves were also constructed with Kaplan-Meier estimates and compared by the Klein-Moeschberger test. Also the propensity score that was generated in the whole patient population was incorporated into subsequent proportional hazards models as a covariate. To avoid over-adjustment, the multivariable Cox regression analysis was performed using only the two variables ‘propensity score’ and ‘treatment.’ All reported p values are two-sided, and p values of <0.05 were considered to indicate statistical significance. IBM SPSS software (version 20, SPSS Inc, Chicago, USA) was used for statistical analyses.
Results
A total of 3580 STEMI and NSTEMI patients were studied. The percentage of patients undergoing transradial intervention increased from 19 % in 2010 to 74.5 % in 2013. The rate of crossover from primarily intended transradial to transfemoral intervention was 4 % in 2010, to 3 % in 2011, 2.2 % in 2012 and 4.6 % in 2013. Baseline, clinical and angiographic characteristics are shown in Table 1 and 2.
Unadjusted outcomes
Before propensity score matching, patients who underwent transfemoral intervention and those intended to undergo the transradial approach differed significantly in clinical and procedural characteristics (Table 1). Patients with previous CABG (5.2 % in the transradial vs. 7.5 % in the transfemoral group; p = 0.008), GP IIb/IIIa inhibitors in the pre-hospital phase (28.9 % in the transradial vs. 33.4 % in the transfemoral group; p = 0.006), patients with IABP (1.7 % in the transradial vs. 6.6 % in the transfemoral group; p < 0.001) and patients with Killip class >1 (10.8 % in the transradial vs. 17.3 % in the transfemoral group; p < 0.001) were more likely to be treated by transfemoral intervention. The unadjusted rate of death in the first 30 days after treatment was lower among patients undergoing transfemoral intervention (1.7 % in the transradial vs. 4.6 % in the transfemoral group; p < 0.001). There was no significant difference in MI (0.6 % in the transradial vs. 0.9 % in the transfemoral group; p = 0.216) and stroke (0 % in the transradial vs. 0.3 % in the transfemoral group; p = 0.093). The rate of overall bleeding was significantly reduced in the transradial group at 30 days (10.9 % vs. 13.6 % in the transfemoral group; p = 0.02). The rate of major bleeding was also significantly reduced in the transradial group at 30 days (4.7 % vs. 7.8 % in the transfemoral group; p = 0.001). There was no significant difference in minor bleeding between the transradial and the transfemoral group (6.2 % in the transradial vs. 5.8 % in the transfemoral group; p = 0.643).
Propensity score-adjusted outcomes
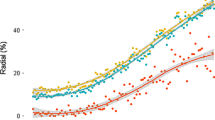
After propensity score matching was performed, there were 781 matched pairs of patients (Table 3). The adjusted outcomes based on propensity score analysis showed no significant difference for mortality (HR 0.56 95 % CI [0.29–1.07], p = 0.08) at 30 days in both groups (Fig. 1a). There was also not a significant difference for MI (HR 0.75 95 % CI [0.26–2.15], p = 0.59) (Fig. 1b) and for composite death, MI, and stroke (HR 0.64 95 % CI [0.37–1.13], p = 0.12) (Fig. 1c). Major bleeding (HR 0.61 [0.25–1.47], p = 0.27) and minor bleeding (HR 0.75 [0.32–1.77], p = 0.51) showed no significant differences. Although not statistically significant, there was a trend towards a favourable outcome for transradial intervention for all endpoints.
Kaplan-Meier curves for outcomes in the propensity score-matched cohort of patients. Patients who underwent transradial or transfemoral intervention were matched for propensity scores. Propensity matching for the entire cohort created 781 matched pairs of patients. (a) Outcomes for overall 30-day mortality; (b) outcomes for myocardial infarction; (c) outcomes for 30-day mortality, myocardial infarction, or stroke
A subgroup analysis comparing STEMI vs. NSTEMI patients showed that the transradial approach was associated with significantly lower mortality at 30 days in STEMI patients (1.7 % in the transradial vs. 5.6 % in the transfemoral group; p < 0.001) and a non-significant difference in NSTEMI patients (1.6 % in the transradial vs. 2.2 % in the transfemoral group; p = 0.47). A subgroup analysis comparing OHCA vs. no-OHCA patients showed that that transradial intervention was associated with significantly lower mortality at 30 days in no-OHCA patients (transradial: 1.3 % vs. transfemoral: 2.7 %, p = 0.009), and a non-significant difference in OHCA patients (transradial: 14.3 %, transfemoral: 21.3 %, p = 0.34). There was no significant interaction between the type of MI, OHCA and vascular access site, (Fig. 2).
Discussion
This prospective observational cohort study, based on a large and unselected cohort of patients, showed that transradial intervention was associated with reduced mortality at 30 days; however, this difference was no longer significant after multivariate and propensity score adjustment. There was a trend towards a favourable outcome for the transradial approach for all endpoints. Transfemoral intervention is currently considered the gold standard access site worldwide [3]; however, access-site complications remain frequent in clinical practice. Theoretically, transradial intervention may improve the survival rate by minimising access site-related complications and their negative prognostic consequences [16]. It would be difficult to reduce bleeding complications in a setting of patients with high thrombotic risk where aggressive antithrombotic and antiplatelet therapy drives gastrointestinal, intracranial and other non-access-site bleeding [17]. Transradial intervention may be underutilised in high-risk ACS patients who may derive greater benefit from this approach. The RIVAL (Radial Versus Femoral Access for Coronary Intervention) study was a large randomised trial of radial and femoral artery access in patients with ACS. It failed to show a significant reduction in death, MI, or bleeding despite significant reductions in vascular access complications. In the subgroup of STEMI patients, however, transradial intervention significantly reduced the primary outcome of death, MI, or stroke and secondary outcomes mainly by a reduction in mortality with a directionally consistent reduction in MI [10, 18]. The RIFLE-STEACS was a large randomised clinical trial comparing the radial and femoral approaches performed in patients with STEMI only and showed that radial access was associated with significantly lower morbidity and cardiac mortality [19]. Subgroup analysis in our study showed no significant interaction in clinical outcome between STEMI vs. NSTEMI for patients treated with transradial vs. transfemoral intervention. The recently published MATRIX trial (Minimising Adverse Haemorrhagic Events by Transradial Access Site and Systemic Implementation of Angiox) randomised 8404 patients undergoing angioplasty. This large trial included STEMI and NSTEMI patients. After 30 days, the use of radial access for coronary angiography followed by percutaneous coronary intervention, if indicated, significantly reduced the rate of net adverse clinical events, defined as the composite of major adverse cardiovascular events or major bleeding [20]. Systematic reviews have repeatedly demonstrated that transradial intervention in unselected populations for coronary angiography resulted in an absolute reduction in bleeding complications, leading to reduced ischaemic endpoints and death [21]. Especially in high-risk populations, such as patients with extreme obesity, reductions resulted in an absolute reduction in vascular complications [22, 23]. Selecting a transradial approach for coronary angiography or PCI may be an important intervention for reducing procedural morbidity in patients considered at high risk for access site complications. The radial access route is still not widely utilised despite current evidence. The radial approach is a specific skill and involves a learning curve [24, 25]. There are a few known complications, such as upper extremity dysfunction after transradial intervention, radial artery spasm, intimae damage and occlusion, or vascular anomalies with consequent failure to reach the ascending aorta. These are obstacles that can be overcome with appropriate training [11, 26, 27].
Limitations
Several limitations of the present analysis should be considered. First, this is a single-centre, non-randomised, prospective observational study and therefore it was not possible to account for all confounding influences. We used propensity score matching to make the patient groups comparable according to the measured confounders, and we successfully eliminated the observed differences. However, we cannot fully exclude the possibility of confounding by baseline factors that we did not study. Second, we also could not control for differences in the skill of the operators. It is conceivable that a radial approach may be preferentially selected by more skilled angiographers.
Conclusion
In this single-centre registry, the use of radial access for all consecutive STEMI and NSTEMI patients undergoing coronary angiography and PCI when appropriate showed that radial access was associated with improved outcome. However, this difference was no longer significant after multivariate and propensity score adjustment for differences in baseline characteristics.
References
ten Berg JM, van ’t Hof AWJ, Dill T, et al. On-TIME 2 study group. Effect of early, pre-hospital initiation of high bolus dose tirofiban in patients with ST-segment elevation myocardial infarction on short- and long-term clinical outcome. J Am Coll Cardiol. 2010;55:2446–55.
Zeymer U, Schroder R, Machnig T, Neuhaus KL. Primary percutaneous transluminal coronary angioplasty accelerates early myocardial reperfusion compared to thrombolytic therapy in patients with acute myocardial infarction. Am Heart J. 2003;146:686–91.
Valgimigli M, Saia F, Guastaroba P, et al., REAL Registry Investigators. Transradial versus transfemoral intervention for acute myocardial infarction: a propensity score-adjusted and –matched analysis from the REAL (REgistro regionale AngiopLastiche dell’Emilia-Romagna) multicenter registry. J Am Coll Cardiol Interv. 2012;5:23–35.
Fefer P, Matetzky S, Gannot S, et al. Predictors and outcomes associated with radial versus femoral access for intervention in patients with acute coronary syndrome in a real-world setting: results from the Acute Coronary Syndrome Israeli Survey (ACSIS). J Invasive Cardiol. 2010;2014(26):398–402.
Mehran R, Pocock S, Nikolsky E, et al. Impact of bleeding on mortality after percutaneous coronary intervention results from a patient-level pooled analysis of the REPLACE-2 (randomized evaluation of PCI linking angiomax to reduced clinical events), ACUITY (acute catheterization and urgent intervention triage strategy), and HORIZONS-AMI (harmonizing outcomes with revascularization and stents in acute myocardial infarction) trials. JACC Cardiovasc Interv. 2011;4:654–64.
Kinnaird TD, Stabile E, Mintz GS, et al. Incidence, predictors, and prognostic implications of bleeding and blood transfusion following percutaneous coronary interventions. Am J Cardiol. 2003;92:930–5.
Rao SV, Jollis JG, Harrington RA, et al. Relationship of blood transfusion and clinical outcomes in patients with acute coronary syndromes. JAMA. 2004;292:1555–62.
Ndrepepa G, Berger PB, Mehilli J, et al. Periprocedural bleeding and 1‑year outcome after percutaneous coronary interventions: appropriate- ness of including bleeding as a component of a quadruple end point. J Am Coll Cardiol. 2008;51:690–7.
Pocock SJ, Mehran R, Clayton TC, et al. Prognostic modeling of individual patient risk and mortality impact of ischemic and hemorrhagic complications: assessment from the acute catheterization and urgent intervention triage strategy trial. Circulation. 2010;121:43–51.
Mehta SR, Jolly SS, Cairns J, et al., RIVAL Investigators. Effects of radial versus femoral artery access in patients with acute coronary syndromes with or without ST-segment elevation. J Am Coll Cardiol. 2012;60:2490–9.
Zwaan EM, Koopman AG, Holtzer CA, et al. Revealing the impact of local access-site complications and upper extremity dysfunction post transradial percutaneous coronary procedures. Neth Heart J. 2015;23:514–24.
Bertrand OF, Bélisle P, Joyal D, et al. Comparison of transradial and femoral approaches for percutaneous coronary interventions: a systematic review and hierarchical Bayesian meta-analysis. Am Heart J. 2012;163:632–48.
Hamm CW, Bassand JP, Agewall S, et al., ESC Committee for Practice Guidelines. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: the task force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2011;32:2999–3054.
Hermanides RS, Ottervanger JP, ten Berg JM, et al., On-TIME 2 Trial Investigators. Net clinical benefit of prehospital glycoprotein IIb/IIIa inhibitors in patients with ST-elevation myocardial infarction and high risk of bleeding: effect of tirofiban in patients at high risk of bleeding using CRUSADE bleeding score. J Invasive Cardiol. 2012;24:84–9.
Austin PC. Some methods of propensity-score matching had superior performance to others: results of an empirical investigation and Monte Carlo simulations. Biom J. 2009;51:171–84.
Applegate RJ, Sacrinty MT, Kutcher MA, et al. Trends in vascular complications after diagnostic cardiac catheterization and percutaneous coronary intervention via the femoral artery, 1998 to 2007. Jacc Interv. 2008;1:317–26.
Verheugt FW, Steinhubl SR, Hamon M, et al. Incidence, prognostic impact, and influence of antithrombotic therapy on access and nonaccess site bleeding in percutaneous coronary intervention. JACC Cardiovasc Interv. 2011;4:191–7.
Jolly SS, Yusuf S, Cairns J, et al., RIVAL trial group. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet. 2011;377:1409–20.
Romagnoli E, Biondi-Zoccai G, Sciahbasi A, et al. Radial versus femoral randomized investigation in ST-segment elevation acute coronary syndrome: The RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) study. J Am Coll Cardiol. 2012;60:2481–9.
Valgimigli M, Gagnor A, Calabró P, et al., MATRIX Investigators. Radial versus femoral access in patients with acute coronary syndromes undergoing invasive management: a randomised multicentre trial. Lancet. 2015;385:2465–76.
Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am Heart J. 2009;157:132–40.
Fetterly KA, Lennon RJ, Bell MR, Holmes DR Jr., Rihal CS. Clinical determinants of radiation dose in percutaneous coronary interventional procedures: influence of patient size, procedure complexity, and performing physician. JACC Cardiovasc Interv. 2011;4:336–43.
Benamer H, Louvard Y, Sanmartin M, et al. A multicentre comparison of transradial and transfemoral approaches for coronary angiography and PTCA in obese patients: the TROP registry. EuroIntervention. 2007;3:327–32.
Rao SV, Ou FS, Wang TY, et al. Trends in the prevalence and outcomes of radial and femoral approaches to percutaneous coronary intervention: a report from the National Cardiovascular Data Registry. JACC Cardiovasc Interv. 2008;1:379–86.
Ball WT, Sharieff W, Jolly SS, et al. Characterization of operator learning curve for transradial coronary interventions. Circ Cardiovasc Interv. 2011;4:336–41.
Eccleshall SC, Banks M, Carroll R, Jaumdally R, Fraser D, Nolan J. Implementation of a diagnostic and interventional transradial programme: resource and organisational implications. Heart. 2003;89:561–2.
Azzano A, Vermeersch P. The tricky charm of the radial access. Neth Heart J. 2015;23:508–9.
Acknowledgements
We thank Vera Derks for her excellent editorial assistance.
Funding
None.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
S. Kilic, R.S. Hermanides, J.P. Ottervanger, E. Kolkman, J.H.E. Dambrink, V. Roolvink, A.T.M. Gosselink, E. Kedhi and A.W.J. van ’t Hof declare that they have no competing interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kilic, S., Hermanides, R.S., Ottervanger, J.P. et al. Effects of radial versus femoral artery access in patients with acute myocardial infarction: A large centre prospective registry. Neth Heart J 25, 33–39 (2017). https://doi.org/10.1007/s12471-016-0887-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12471-016-0887-6