Abstract
Atrial fibrillation (AF) is associated with short-term mortality after ST-elevation myocardial infarction (STEMI), but there is limited data on the temporal association between AF and mortality after STEMI. A total of 830 patients were included (age: 62 ± 12 years, 76 % male). Patients with new-onset AF < 30 days after STEMI were divided among three subgroups: AF on the day of admission, AF 24–72 h and AF > 72 h after admission. Thirty-day mortality was assessed by telephone and via the municipal population registry. Twenty patients died < 30 days after admission. In 41 patients, AF was detected on the day of admission, in 14 patients 24–72 h after admission and in 18 patients > 72 h after admission. Mortality was higher in patients with AF on the day of admission (7.3 vs 2.2 %, p = 0.036) and 24–72 h after admission (14.3 vs 1.4 %, p < 0.001), but not in patients with AF > 72 h after admission (0 vs 1.1 %, p > 0.999). Age (odds ratio (OR) 1.123, p < 0.001), Killip class (adjusted OR 8.341, p < 0.001), AF on the day of admission (OR 3.585, p = 0.049) and 24–72 h after admission (OR 11.515, p = 0.003) were, amongst other variables, associated with an increased 30-day mortality. In conclusion, only new-onset incident AF during the first 72 h after admission was associated with 30-day mortality in STEMI patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atrial fibrillation (AF) is common in the setting of ST-elevation myocardial infarction (STEMI) [1–4] and is associated with an increased re-infarction rate, cardiogenic shock and pulmonary oedema [5]. AF is also an independent predictor of both short-[6, 7] and long-term mortality [5, 7–12]. However, there are only limited data on the temporal association between new-onset AF and short-term mortality. The present study was aimed at assessing the impact of different AF episode timings on 30-day mortality in patients who underwent primary percutaneous coronary intervention (PPCI) in the setting of STEMI.
Methods
Our population consisted of patients with a STEMI, who were admitted for PPCI and included in the ongoing tirofiban in myocardial infarction evaluation (On-TIME) II study [13, 14], a prospective, multicentre, placebo-controlled, randomised, clinical trial. The rationale, design and primary results of On-TIME II have been previously described [13]. Briefly, enrolment was from June 2006 to November 2007. Eligible patients were aged 21–85 years with symptoms of acute myocardial infarction of more than 30 min but less than 24 h and ST-segment elevation of more than 1 mV in two adjacent electrocardiograph (ECG) leads. Exclusion criteria were severe renal dysfunction (glomerular filtration rate < 30 ml/min or serum creatinine > 200 mmol/l (> 2.5 mg/dl)), therapy resistant cardiogenic shock (systolic blood pressure ≤ 80 mmHg for > 30 min), persistent severe hypertension (systolic pressure > 180 mmHg or diastolic pressure > 110 mmHg), or a contraindication to anticoagulation or increased risk of bleeding. Also, patients with a left bundle branch block, pregnant and/or breastfeeding women, and patients with a life expectancy of less than 1 year were excluded. For the present study, patients with a known history of AF were excluded. From each patient, written informed consent for participation in the On-TIME II study was obtained. The local ethics committees approved the study protocol.
Treatment
All patients were planned to undergo PPCI and were treated according to the On-TIME II study protocol, randomly assigned to (prehospital) treatment with tirofiban (25 μg/kg bolus and 0.15 μg/kg/min maintenance infusion for 18 h) or placebo. PPCI was performed with standard techniques, if the coronary anatomy was suitable for angioplasty. Additional treatment with stents and devices was at the discretion of the treating cardiologist. All patients were treated with optimal drug therapy including angiotensin-converting enzyme inhibitors, β-blockers, aspirin and a statin. Final discharge and admission duration was at the discretion of the treating cardiologist.
Endpoints
The primary endpoint of the On-TIME II trial was the extent of residual ST-segment deviation at 1 h after PCI. For the present study, all-cause mortality was the primary endpoint of this study. To assess mortality, all patients visited the outpatient clinic 30 days after admission. When patients did not visit the outpatient clinic, an attempt was made to contact the patient and general practitioner to determine whether the patient was still alive. Furthermore, the municipal population registries, which keep records of all deaths in participating countries, were checked in all patients > 30 days after the STEMI. The occurrence of AF was defined as an episode of AF/atrial flutter/atrial tachycardia > 30 s, either on a telemetry strip or on a 12-lead ECG, in accordance with European guidelines [15] within 30 days after admission. Patients were on telemetry during the first 48 h after admission, and an ECG was performed once every 24 h, or whenever deemed necessary. Whenever a patient experienced symptoms and was not on telemetry, an ECG was performed immediately.
Statistical analysis
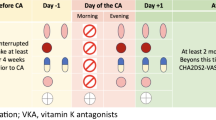
Continuous variables were expressed as mean with standard deviation (SD). Patients in whom AF was detected < 24 h after admission were categorised to the ‘AF on the day of admission’ subgroup. Patients in whom AF was detected 24–72 h after admission were categorised to the ‘AF 24–72 h after admission’ subgroup. Patients in whom AF was detected > 72 h but < 30 days after admission were categorised to the ‘AF > 72 h after admission’ subgroup, as displayed in Fig. 1. Baseline characteristics between 30-day mortality yes and no groups were compared with a Mann–Whitney U test in case of continuous variables and chi-square test in case of dichotomous or categorical data, except for data with > 20 % cells with a value < 5, in which case a Fisher’s exact test was used. A univariate analysis was performed for the association between patient characteristics, biomarkers, AF and mortality with a binary logistic regression model. A multivariate model was not created due to the limited number of endpoints in this study. However, for each AF episode timing, we performed a multivariate analysis with the Zwolle risk score [16]. The Zwolle risk score is a composite score of 6 clinical variables: Killip class, TIMI flow post-PPCI, age, 3-vessel disease, anterior infarction and ischaemia time, and allows identification of STEMI patients at high risk of 30-day mortality. The difference between patient age in smoking versus non-smoking patients was assessed with a Mann–Whitney U test. Statistical analysis was performed using IBM SPSS statistics version 20 (IBM inc., Armonk, NY, USA). A p-value of ≤ 0.05 was considered statistically significant.
Results
A total of 984 patients were admitted with the diagnosis of STEMI. Of these patients, 861 underwent PPCI. Baseline characteristics of the whole study population have been previously reported [14]. A total of 31 patients had a history of AF and were subsequently excluded; 30-day follow-up was present in 830 patients, who were included in the analysis for the current study. Baseline characteristics of the study population are displayed in supplemental Table 1.
Mortality and baseline characteristics
A total of 20 patients died < 30 days after STEMI, 5 patients died < 24 h after admission, 3 patients died 24–72 h after admission and 12 patients died > 72 h after admission. AF was detected in a total of 73 patients: in 41 patients on the day of admission, in 14 patients 24–72 h after admission and in 18 patients > 72 h after admission, as displayed in Fig. 1. Patients who died were significantly older (74.2 vs 61.8 years, p < 0.001), less often smokers (21.1 vs 49.3 %, p = 0.015), with more often a history of diabetes (35.0 vs 10.1 %, p < 0.001) and hypertension (55.0 vs 32.7 %, p = 0.037), more often a Killip class > 1 (50.0 vs 10.7 %, p < 0.001), more often a previous infarction (25.0 vs 7.8 %, p = 0.006), a lower systolic (109.1 vs 131.4 mmHg, p < 0.001) and diastolic blood pressure on admission (63.3 vs 76.9 mmHg, p = 0.001), received the tirofiban study medication less often (20.0 vs 49.6 %, p = 0.009) and more often a TIMI grade flow < 3 post PPCI (40.0 vs 8.2 %, p < 0.001), as displayed in supplemental Table 1.
Atrial fibrillation on day of admission
Mortality in patients in whom AF was detected on the day of admission was significantly higher compared with patients who were AF-free (7.3 vs 2.2 %, p = 0.036), as displayed in Table 1. In univariate analysis, age (odds ratio (OR) 1.123, p < 0.001), smoking (OR 0.275, p = 0.023), diabetes (OR 4.774, p = 0.001), hypertension (OR 2.514, p = 0.043), Killip class > 1 (OR 8.314, p < 0.001), previous myocardial infarction (OR 3.942, p = 0.010), systolic (OR 0.641, p < 0.001) and diastolic (OR 0.530, p < 0.001) blood pressure on admission, tirofiban study medication (OR 0.254, p = 0.015) and TIMI grade post PPCI < 3 (OR 7.444, p < 0.001) were associated with 30-day mortality. AF on the day of admission was also significantly associated with 30-day mortality (OR 3.585, p = 0.049). In multivariate analysis, AF on the day of admission was not associated with short-term mortality (adjusted OR 3.537, p = 0.116). The analysis is displayed in Table 2.
Atrial fibrillation 24–72 h after admission
Mortality in patients in whom AF was detected 24–72 h after admission was significantly higher compared with patients who were AF-free (14.3 vs 1.4 %, p < 0.001), as displayed in Table 1. In univariate analysis, age (OR 1.111, p < 0.001), diabetes (OR 5.911, p = 0.001), Killip class > 1 (OR 7.275, p < 0.001), previous myocardial infarction (OR 4.300, p = 0.015), systolic (OR 0.708, p = 0.005) and diastolic blood pressure on admission (OR 0.611, p = 0.009), tirofiban study medication (OR 0.254, P = 0.035), culprit vessel (OR 4.317, p = 0.026), TIMI grade flow < 3 post PPCI (OR 4.061, p = 0.019) and AF 24–72 h after admission (OR 11.515, p = 0.003) were significantly associated with 30-day mortality. In multivariate analysis, AF 24–72 h after admission was independently associated with 30-day post-infarction mortality (adjusted OR 13.476, p = 0.006). The analysis is displayed in Table 3.
Atrial fibrillation > 72 h after admission
Mortality in patients in whom AF was detected > 72 h after admission did not differ among patients with AF compared with those without AF (0 vs 1.1 %, p > 0.999), as displayed in Table 1. In univariate analysis, age (OR 1.106, p = 0.002), diabetes (OR 6.333, p = 0.002), Killip class > 1 (OR 5.939, p = 0.003), previous myocardial infarction (OR 5.913, p = 0.005), culprit vessel (OR 5.298, p = 0.034) and TIMI grade flow < 3 post PPCI (OR 5.583, p = 0.006) were significantly associated with 30-day post-infarction mortality. No multivariate analysis was performed for AF > 72 h after admission. The analysis is displayed in supplemental Table 2.
Discussion
The current study reports the temporal association between new-onset AF and 30-day post-infarction mortality. AF on the day of admission and AF 24–72 h after admission were significantly associated with 30-day post-infarction mortality. In contrast, patients in whom AF was detected > 72 h after admission did not show an increased post-infarction mortality.
Predictors of mortality
In previous studies, age, diabetes, hypertension, Killip class, previous myocardial infarction, blood pressure on admission, culprit vessel and TIMI grade flow have been associated with short-term post-infarction mortality [17–20]. Furthermore, smoking was associated with reduced short-term mortality [18]. The present study is in line with these previous studies. Furthermore, many studies have reported the independent association between AF and short- and long-term mortality in both the otherwise healthy population [21, 22] and in STEMI patients [6, 12, 23]. Several factors may predispose to AF in the setting of STEMI. Peri-infarction AF has been associated with an increased left ventricular diastolic dysfunction and end-diastolic pressure, which may increase atrial stretch and atrial pressure [24, 25]. Furthermore, atrial dysfunction, atrial ischaemia, pericarditis, congestive heart failure due to ischaemia and enhanced sympathetic tone may also play an important role in the genesis of post-infarction AF [26–28]. Finally, a previous study has reported that an irregular ventricular rate decreases cardiac output and increased pulmonary capillary wedge pressure and right atrial pressure, independent of heart rate [29].
Previous studies
Of note, a study [23] comparing prognosis of AF before and after PPCI reported that only AF post-PPCI was associated with an increase in long-term mortality. However, several differences between the present study and this study are apparent: the present study investigated the impact of AF on short-term mortality, whereas the patients in the study by Beukema et al. [23] were followed-up for 481 days post-PPCI. Furthermore, pre-PPCI AF was associated with an increase in mortality, but only after adjustment for several confounders, AF pre-PPCI was not associated with long-term mortality. The authors did not categorise the AF occurrence in the groups specified in the present study. Of note, this study was conducted in patients at a relatively short distance to the PCI centres [30], and therefore these results may not be applicable in countries with a longer ischaemic time.
Clinical implications
The present study showed a clear temporal association between AF and short-term mortality. More specifically, patients who develop AF on the day of admission and especially 24–72 h after admission should be considered high-risk patients. In contrast, patients who develop AF > 72 h after admission show a mortality rate no greater than other STEMI patients and possibly should not be considered high-risk patients. Although this study does not provide any evidence, underlying pathophysiological mechanisms may be different in the AF subgroups. Hypothetically, patients who develop AF on the day of admission or 24–72 h after admission are haemodynamically compromised, with a lower blood pressure and a higher Killip class, factors contributing to an increased 30-day mortality. In contrast, AF > 72 h after admission may be more closely associated with atrial fibrosis, and thereby not directly impacting 30-day mortality.
Limitations
Current study is a substudy of the On-TIME II study and therefore, a predefined power assessment was not made for the relation of incident AF and short-term mortality. Only a multivariate analysis with the Zwolle risk score could be performed. The results of the multivariate analysis should be interpreted with caution due to the limited number of endpoints in this study. Although all variables were prospectively registered, the present study is a post-hoc cross-sectional analysis. Future studies with a larger patient population may be necessary to further elucidate the temporal association between AF and mortality. Patients with asymptomatic AF before inclusion in the study may have influenced the data. All patients were kept on telemetry for at least 48 h but thereafter, an ECG was performed once daily. This may have caused several asymptomatic AF episodes not to have been documented, which may have impacted the present study’s outcome. Furthermore, the AF episode in regard to the onset of ischaemia was not registered.
Conclusion
Post-infarction AF occurring during the first 72 h after admission for STEMI was an important risk factor for mortality. In contrast, AF detected > 72 h after STEMI was not associated with 30-day mortality.
References
Goldberg RJ, Seeley D, Becker RC, et al. Impact of atrial fibrillation on the in-hospital and long-term survival of patients with acute myocardial infarction: a community-wide perspective. Am Heart J. 1990;119:996–1001.
Pedersen OD, Bagger H, Kober L, et al. The occurrence and prognostic significance of atrial fibrillation/-flutter following acute myocardial infarction. TRACE Study group. TRAndolapril Cardiac Evalution. Eur Heart J. 1999;20:748–54.
Pizzetti F, Turazza FM, Franzosi MG, et al. Incidence and prognostic significance of atrial fibrillation in acute myocardial infarction: the GISSI-3 data. Heart. 2001;86:527–32.
Wann LS, Curtis AB, Ellenbogen KA, et al. 2011 ACCF/AHA/HRS focused update on the management of patients with atrial fibrillation (update on dabigatran): a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2011;57:1330–7.
Mehta RH, Dabbous OH, Granger CB, et al. Comparison of outcomes of patients with acute coronary syndromes with and without atrial fibrillation. Am J Cardiol. 2003;92:1031–6.
Consuegra-Sanchez L, Melgarejo-Moreno A, Galcera-Tomas J, et al. Short- and long-term prognosis of previous and new-onset atrial fibrillation in ST-segment elevation acute myocardial infarction. Rev Esp Cardiol. 2015;68:31–8.
Podolecki T, Lenarczyk R, Kowalczyk J, et al. Effect of type of atrial fibrillation on prognosis in acute myocardial infarction treated invasively. Am J Cardiol. 2012;109:1689–93.
Lehto M, Snapinn S, Dickstein K, et al. Prognostic risk of atrial fibrillation in acute myocardial infarction complicated by left ventricular dysfunction: the OPTIMAAL experience. Eur Heart J. 2005;26:350–6.
Sakata K, Kurihara H, Iwamori K, et al. Clinical and prognostic significance of atrial fibrillation in acute myocardial infarction. Am J Cardiol. 1997;80:1522–7.
Kober L, Swedberg K, McMurray JJ, et al. Previously known and newly diagnosed atrial fibrillation: a major risk indicator after a myocardial infarction complicated by heart failure or left ventricular dysfunction. Eur J Heart Fail. 2006;8:591–8.
Jabre P, Jouven X, Adnet F, et al. Atrial fibrillation and death after myocardial infarction: a community study. Circulation. 2011;123:2094–100.
Jabre P, Roger VL, Murad MH, et al. Mortality associated with atrial fibrillation in patients with myocardial infarction: a systematic review and meta-analysis. Circulation. 2011;123:1587–93.
Hof AW van ’t, Hamm C, Rasoul S, et al. Ongoing tirofiban in myocardial infarction evaluation (On-TIME) 2 trial: rationale and study design. EuroIntervention. 2007;3:371–80.
Hof AW Van’t, Ten Berg J, Heestermans T, et al. Prehospital initiation of tirofiban in patients with ST-elevation myocardial infarction undergoing primary angioplasty (On-TIME 2): a multicentre, double-blind, randomised controlled trial. Lancet. 2008;372:537–46.
Calkins H, Kuck KH, Cappato R, et al. 2012 HRS/EHRA/ECAS Expert Consensus Statement on Catheter and Surgical Ablation of Atrial Fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. Europace. 2012;14:528–606.
Luca G De, Suryapranata H, Hof AW van ’t, et al. Prognostic assessment of patients with acute myocardial infarction treated with primary angioplasty: implications for early discharge. Circulation. 2004;109:2737–43.
Lee KL, Woodlief LH, Topol EJ, et al. Predictors of 30-day mortality in the era of reperfusion for acute myocardial infarction. Results from an international trial of 41,021 patients. GUSTO-I Investigators. Circulation. 1995;91:1659–68.
Canto JG, Kiefe CI, Rogers WJ, et al. Atherosclerotic risk factors and their association with hospital mortality among patients with first myocardial infarction (from the National Registry of Myocardial Infarction). Am J Cardiol. 2012;110:1256–61.
Schmidt M, Jacobsen JB, Lash TL, et al. 25 year trends in first time hospitalisation for acute myocardial infarction, subsequent short and long term mortality, and the prognostic impact of sex and comorbidity: a Danish nationwide cohort study. BMJ. 2012;344:e356.
Vogt A, Essen R von, Tebbe U, et al. Impact of early perfusion status of the infarct-related artery on short-term mortality after thrombolysis for acute myocardial infarction: retrospective analysis of four German multicenter studies. J Am Coll Cardiol. 1993;21:1391–5.
Wolf PA, Mitchell JB, Baker CS, et al. Impact of atrial fibrillation on mortality, stroke, and medical costs. Arch Intern Med. 1998;158:229–34.
Benjamin EJ, Wolf PA, D’Agostino RB, et al. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998;98:946–52.
Beukema RJ, Elvan A, Ottervanger JP, et al. Atrial fibrillation after but not before primary angioplasty for ST-segment elevation myocardial infarction of prognostic importance. Neth Heart J. 2012;20:155–60.
Shelton RJ, Clark AL, Goode K, et al. The diagnostic utility of N-terminal pro-B-type natriuretic peptide for the detection of major structural heart disease in patients with atrial fibrillation. Eur Heart J. 2006;27:2353–61.
Celik S, Erdol C, Baykan M, Kaplan S, Kasap H. Relation between paroxysmal atrial fibrillation and left ventricular diastolic function in patients with acute myocardial infarction. Am J Cardiol. 2001;88:160–2, A5.
Crenshaw BS, Ward SR, Granger CB, Stebbins AL, Topol EJ, Califf RM. Atrial fibrillation in the setting of acute myocardial infarction: the GUSTO-I experience. Global Utilization of Streptokinase and TPA for Occluded Coronary Arteries. J Am Coll Cardiol. 1997;30:406–13.
Corradi D, Callegari S, Maestri R, Benussi S, Alfieri O. Structural remodeling in atrial fibrillation. Nat Clin Pract Cardiovasc Med. 2008;5:782–96.
Zicha S, Tsuji Y, Shiroshita-Takeshita A, Nattel S. Beta-blockers as antiarrhythmic agents. Handb Exp Pharmacol. 2006;171:235–66.
Clark DM, Plumb VJ, Epstein AE, Kay GN. Hemodynamic effects of an irregular sequence of ventricular cycle lengths during atrial fibrillation. J Am Coll Cardiol. 1997;30:1039–45.
Postma S, Dambrink JH, Boer MJ de, et al. The influence of residential distance on time to treatment in ST-elevation myocardial infarction patients. Neth Heart J. 2014;22:513–9.
Acknowledgements
The On-TIME II study was supported by Merck&Co (Whitehouse Station, USA). We thank Ms. Petra Koopmans for verifying the statistical analysis.
Funding
None.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Gal, P., Parlak, E., Demirel, F. et al. Prognostic significance of incident atrial fibrillation following STEMI depends on the timing of atrial fibrillation. Neth Heart J 23, 430–435 (2015). https://doi.org/10.1007/s12471-015-0709-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12471-015-0709-2