Abstract
Imaging of cardiac function and anatomy has advanced at an exponential rate over the past two decades. Our ability to quantitatively assess the degree of myocardial ischemia and accurately define the vascular anatomy using noninvasive techniques is greater than ever before. Current advances is cardiac imaging are allowing us to more safely assess patients for myocardial ischemia and better understand the prognostic implications of our findings. This review summarizes the current state of knowledge in cardiac imaging for the assessment of cardiac ischemia with a focus on the use of cardiac MRI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The last decade has seen exponential growth in the diagnostic modalities available to the clinician for the assessment of coronary artery disease (CAD). While this growth in technology has been accompanied by important advancements in the management of acute coronary syndromes, less progress has been observed in the treatment of chronic stable CAD. This lack of therapeutic progress in the management of chronic forms of coronary disease is disappointing in some respects; however, there is no question that substantial advances have occurred in both our ability to image the disease and our understanding of the significance of the findings that are made. These advances have improved not only our understanding of the prognostic features that are vital in the treatment of CAD, but they also are likely to ultimately result in improved outcomes. This review will attempt to illuminate how recent advances in cardiac imaging, with a focus on cardiac MRI, are likely to translate into improved cardiac care in the future. Fig. 1.
Diagnosis and Prognosis: Two Sides of the Same Coin
The imaging modalities available for the assessment of CAD can be broadly divided into two groups: those that characterize the luminal anatomy of CAD (i.e., CT angiography), and those that characterize the functional consequences of CAD (i.e., stress echocardiography). Imaging modalities that detect anatomical CAD are generally more sensitive to detect coronary artery stenosis; however, imaging modalities that detect functional ischemia may provide more information on the relevance of a stenosis and its impact on prognosis. Cardiac MRI (CMR) is somewhat uniquely placed in that it bridges both the anatomic and functional domains of cardiac imaging (Table 1).
There is an important distinction to be made in the nature of the information obtained from anatomic and functional noninvasive imaging techniques. While anatomic characterization of coronary disease is of great utility in both initial diagnosis of CAD and subsequent planning for revascularization, functional testing represents the more powerful determinant for selecting the appropriate therapy and estimate prognosis. Baseline left ventricular function and objective demonstration of ischemia are strongly associated with outcomes. Mistakenly, noninvasive imaging is often carried out solely to make a determination as to the likelihood of the presence of CAD. If the likelihood is deemed high, the patient is referred for coronary angiography, which then dictates future management based only on the anatomic appearance of the coronary vessel lumen. Except in the most severe forms of CAD [1], evidence advising against revascularization without objective data demonstrating evidence of myocardial ischemia has been available for many years [2]. It is thus necessary to obtain both functional and anatomic information regarding CAD in order to design an appropriate and rational treatment strategy in any given patient.
The rationale against revascularization on the basis of anatomy alone was recently underscored with the publication of the COURAGE trial [3]. This study threw into question the wisdom of basing percutaneous coronary intervention decisions solely on the angiographic appearance of coronary disease. In this large multicenter randomized controlled trial, percutaneous coronary intervention did not reduce the risk of death or myocardial infarction when compared to medical therapy alone. However, a substudy population of this trial, which was further stratified for ischemic burden, did show a trend towards benefit of revascularization when the ischemic burden was high [4]. More recently, evidence has accumulated that demonstrates the value of demonstrating a functional ischemic burden when making revascularization decisions for CAD [5, 6•]. The need for both anatomic and functional imaging modalities in the assessment of cardiac ischemia remains clear.
Ideally, we will reach the point where only patients who are very likely to benefit from invasive revascularization procedures will be exposed to the risks inherent in these techniques. All others will be excluded through the appropriate application of sensitive and specific diagnostic imaging. Clinical research should give guidance for these important questions.
Imaging as an End Point
A functional approach to the diagnosis of CAD relies on imaging modalities that demonstrate myocardial ischemia. These techniques include nuclear imaging, stress echocardiography, PET, and CMR perfusion protocols. The evidence that supports the use of these techniques usually considers the identification of significant CAD (>50% narrowing of a coronary artery) at coronary angiography as the gold standard against which the technique is assessed. Table 2 outlines the sensitivity and specificity of the various imaging modalities. Generally, the performance of these tests can be considered very good, but not diagnostic by itself. Thus, clinical judgment still plays an important role in patient management.
More recently, the use of CT has become prevalent in the diagnosis of CAD. Techniques range from coronary calcium scoring to the multislice CT determination of coronary anatomy. These techniques do not depend on the presence of myocardial ischemia for the identification of CAD, and therefore are likely to detect the presence of disease during the earlier stages of atherosclerosis. While the widespread use of CT is likely to remain constrained by the radiation dose, this modality currently offers a diagnostic test of high accuracy.
When considering the value of any imaging technique, it is important to keep in mind the expected outcomes from any given result. The identification of minor vessel irregularities on a multislice CT does not likely carry the same prognostic significance as would the presence of severe inducible wall motion abnormalities identified during stress echocardiography. Indeed, the evidence on clinical outcomes, which support the established methods of ischemia imaging, are a substantial advantage of the older techniques. Newer modalities have not yet sufficiently well demonstrated their prognostic significance, although such studies are underway. More importantly, though, even standard techniques are not backed up by data showing that therapeutic decision-making based on such findings actually improves outcome, regardless of mere diagnostic accuracy and predictive value.
Relevant outcomes in ischemia trials include not only death, but also markers such as resolution of ST elevation, symptoms, arrhythmia, heart failure, hospitalizations, and quality of life. When assessing the utility of an imaging end point, it is important to consider the relationship that the imaging result has with these factors.
Perfusion Imaging
Scintigraphy
There is a substantial body of evidence that supports the use of ischemia imaging as a clinically relevant end point. This is particularly true of the nuclear medicine literature. A meta analysis of single-photon emission CT (SPECT) imaging, which included 69,655 patients referred for risk stratification, concluded that the presence of a moderate or severe perfusion defect was associated with an annual hard event rate of 5.9%, while a normal SPECT scan was associated with an annual risk of death or myocardial infarction (MI) of only 0.85%, a rate which is comparable to that of the general population [7]. Similarly, an abnormal perfusion scan using rubidium positron emission tomography in patients with known or suspected CAD is associated with an annual risk of death of 4.3%, while a normal study is associated with an annual mortality rate of 0.9% [8].
A general limitation of all perfusion techniques may arise from the presence of microvascular disease in diabetes, hypertension, and hypercholesterolemia. Microvascular disease is hypothesized to result in impaired perfusion in the absence of significant epicardial stenosis. This is thought to partially explain (the other reason being the low incidence of disease in the study population) why SPECT’s specificity is never found to be much higher than 75% to 80%. It is of interest that this lower specificity is not reflected in worsened prognostic power, suggesting that microvascular disease remains an important prognostic determinant.
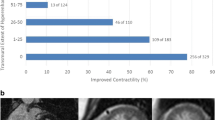
Cardiac MRI
While nuclear perfusion imaging techniques are well established, they are increasingly compromised by concerns about radioactivity as well as more recent concerns surrounding isotope supply problems. Fortunately, the utility of stress perfusion CMR as an evidence-based diagnostic technique is also improving. MR-IMPACT was a multicenter head-to-head comparison of stress perfusion CMR and nuclear perfusion imaging that found the two techniques approximately equivalent in CAD detection [9•]. This study was an important contribution to the field, as it provided strong evidence in support of CMR-based perfusion imaging. A recent meta analysis of the diagnostic performance of stress perfusion CMR which included 2,125 patients enrolled in 26 studies, reported an overall sensitivity of 89% and a specificity of 80% [10••] of CMR stress perfusion when compared to the gold standard of coronary angiography. As discussed above, the relatively low specificity of CMR perfusion protocols is argued to be in part due to its sensitivity in identifying microvascular coronary disease which is not associated with epicardial stenosis [11].
The prognostic evidence supporting stress perfusion CMR is more limited than the diagnostic characterization of the test, but is increasing. Jahnke et al. [12] performed stress perfusion CMR studies on 513 patients with known or suspected CAD. During a median follow-up of 2.3 years, a positive scan was associated with a hazard ratio of 12.5 (CI = 3.6–43) for cardiac events [12]. A recent study of 103 patients presenting to the emergency department with low-risk chest pain demonstrated that a normal adenosine CMR stress perfusion study was associated with no subsequent events over a mean follow-up of 277 days in this population [13].
A significant issue with CMR stress perfusion imaging is the difficulty in obtaining adequate first-pass perfusion images in the transit time available. A novel solution to this problem has recently been presented in animal model work by Spuentrup et al. [14]. They have identified a gadolinium-containing contrast agent with a high affinity for myocardial collagen. This agent allows CMR imaging to occur up to an hour after contrast injection while still retaining differential distribution of the contrast agent between normal and ischemic myocardium.
While CMR appears to be capable of replicating the subjective perfusion findings of the nuclear techniques, without the risks associated with radioactive tracers, CMR is capable of much more objective results in the determination of myocardial ischemia.
The capacity of CMR to quantitate myocardial blood flow has been elegantly demonstrated by Kurita et al. [15•], who compared myocardial blood flow at stress and rest in normal and stenotic coronary arteries using both Doppler flow wires and with quantitative first-pass perfusion imaging of the regional myocardium. Their results showed a strong correlation between the two techniques and determined that quantitative first-pass stress perfusion CMR was capable of identifying physiologically relevant reduction in blood flow with a sensitivity of 88% and a specificity of 90% when compared to the flow wire as gold standard.
More recently, a comparison of fractional flow reserve (FFR), as determined by flow wire, to stress myocardial perfusion imaging has been performed in 103 patients with suspected angina [16]. In this study, FFR was recorded in all patents’ major epicardial coronary arteries, and stress perfusion CMR was also performed. Myocardial perfusion scans identified perfusion defects in 121 of 300 coronary artery segments, of which 110 were likely subtended by vessels that had an FFR < 0.75 (indicating likely ischemia downstream). A total of 168 of 179 normally perfused segments had an FFR > 0.75. The sensitivity and specificity of stress perfusion CMR for the detection of functionally significant coronary heart disease were 91% and 94%, respectively, with positive and negative predictive values of 91% and 94% in this study.
The utility of quantifying perfusion CMR for research purposes is clear; however, given the time and effort required to produce these results, it has become standard practice in clinical settings to assess myocardial perfusion images subjectively. However, quantitative perfusion imaging by CMR does offer some clinical advantages over subjective evaluation. Perfusion reserve quantitation is capable of differentiating moderate from severe stenoses in patients. Quantitative techniques have also been shown to differentiate triple-vessel from single-vessel CAD, whereas this is difficult by subjective assessment [17••]. This has important implications for assessment of prognosis, and adoption of quantitative methods in CMR perfusion imaging will need to be considered as stress perfusion CMR becomes a more widespread modality in routine clinical assessment.
In addition to the ability of CMR to provide quantitative information about myocardial perfusion, it offers well-established and robust imaging of previous myocardial infarction [18, 19]. The combination of stress perfusion imaging and infarct visualization has been used to characterize the differences in appearance of ST elevation and non-ST elevation MI that may underlie the divergent natural histories of these injuries [20]. Whether the combination of infarct imaging by late enhancement combined with stress perfusion imaging provides complementary prognostic information in assessing cardiovascular risk has long been of interest [21•]. Data have recently become available addressing this question: 254 patients who were referred for assessment of symptomatic ischemia were imaged using both techniques and subsequently followed for a median of 17 months, with the primary end point being a composite of death and MI. Both the presence of infarct and reversible perfusion defects were associated with a threefold increase in cardiac death or acute MI (death/MI) when adjusted for each other and for the effects of patient age and gender (adjusted hazard ratio, 3.31; P < 0.02; and hazard ratio, 3.43; P < 0.01, respectively). In patients without a history of MI who had negative perfusion scan, infarct presence was associated with an 11-fold hazard increase in death/MI. Patients with neither perfusion defects nor infarct had a 98.1% negative annual event rate for death/MI. For association with major adverse cardiac events, stress perfusion imaging was the strongest multivariable variable (hazard ratio, 10.92; P < 0.0001). Although further follow-up with greater patient numbers is required, it appears that the easily accomplished combination of these two techniques in one scanning session is likely to provide a powerful prognostic tool.
CMR Perfusion without Contrast: BOLD Imaging and Spin Labeling
The safe, noninvasive properties of CMR represent an important advantage of the technique. This benefit is somewhat compromised by the intravenous use of gadolinium-containing contrast agents, especially in patients with renal failure [22, 23]. Two strategies are under investigation that may eliminate the need for contrast agents in perfusion CMR protocols of the future.
The first approach is the extension of spin labeling blood flow techniques from the great vessels to the coronary artery bed. Ideally, this method could provide direct quantitation of coronary blood flow in individual epicardial vessels. This technique is made more challenging by cardiac and respiratory motion during image acquisition. Nonetheless, some progress has been made using navigator sequences to control for vessel motion [24•].
The second technique takes advantage of the variable paramagnetic properties of hemoglobin in the oxygenated and deoxygenated states to directly quantitate the oxygen status of the myocardium. This technique is very attractive, as it offers a direct measure of the oxygenation state of the tissue, hence a direct look at ischemia. Interestingly, the ability to determine oxygenation state independently of blood flow may allow us to differentiate true ischemia from the surrogate marker of relative blood flow [25•]. Blood oxygen level–dependent (BOLD) imaging has been shown to be feasible in CMR, but challenges remain [26, 27]. Current 1.5-T magnets display a limited signal-to-noise ratio, which has hampered the application of BOLD imaging in the determination of myocardial ischemia in patients. Nevertheless, BOLD imaging has been successfully combined with myocardial perfusion studies in a large animal model in order to calculate myocardial oxygen supply and demand parameters [28•]. The MRI data obtained in this study correlate well with PET values obtained for myocardial blood flow, myocardial oxygen consumption, and oxygen extraction fraction.
More recently, application of BOLD imaging on 3-T magnets has met with some success. Manka et al. [29•] performed BOLD imaging on a series of 46 patients who subsequently underwent coronary angiography to determine ischemic territories. They report significantly lower T2* values in ischemic segments of myocardium compared to normal and nonischemic segments. Under adenosine stress, T2* values increased significantly in normal segments only.
Jahnke et al. [30••] also recently reported on a series of 50 patients with suspected or known CAD who underwent CMR at 3.0-T followed by invasive X-ray angiography within 48 h. BOLD imaging was performed at rest and under adenosine stress, followed by stress and rest first-pass perfusion and delayed enhancement imaging. Quantitative coronary X-ray angiography was used for coronary stenosis definition. The image quality of BOLD CMR at rest and during adenosine stress was considered good to excellent in 90% and 84% of the patients, respectively, and BOLD signal differed significantly between normal myocardium, myocardium supplied by a stenotic coronary artery, and infarcted myocardium (P < 0.001). These results are encouraging, and are likely to be expanded upon as 3-T systems become more readily available.
Assessment of Ischemia-Induced Contractile Dysfunction
Dobutamine is both an inotropic and chronotropic agent whose use in pharmacologic stress protocols with echocardiographic and CMR-based imaging of the left ventricular cavity is well established. Exercise as a stress is also used in echocardiography, but its use is more problematic in CMR.
The format of the pharmacologic stress studies is identical regardless of the imaging modality: left ventricular wall motion is analyzed at baseline, and subsequently at increasing doses of dobutamine, and if required, atropine—in order to achieve a target cardiac workload. Areas of myocardial ischemia declare themselves as workload increases, and oxygen demand exceeds supply resulting in the development of wall motion abnormalities (WMA). Pooled analysis of 13 stress echocardiography studies including 32,739 patients revealed an annual hard event rate (death or MI) of 1.2% for a normal stress echocardiogram as compared with 7.0% for an abnormal study [31]. These event rates are similar to those identified with stress perfusion techniques. Additional information about baseline LV function is obtained in these studies, which is of itself an important prognostic factor governing outcomes. CMR image acquisition offers the advantage over echocardiography of unlimited windows and better coverage of the LV cavity, and thus may be expected to be more sensitive.
Dobutamine stress CMR also offers the possibility of supplementing the study with a stress perfusion component. This would be expected to improve the overall accuracy of the test, but until recently no objective data on this approach were available. Korosoglou et al. [32] have now published a large cohort of 1,493 patients who were followed for 2 years after testing. Fifty-three hard events occurred during the follow-up period. Using multivariable regression analysis, an abnormal result for wall motion or perfusion during stress yielded independent prognostic value (for wall motion: adjusted hazard ratio of 5.9 [95% CI: 2.5–13.6]; and for perfusion: adjusted HR of 5.4 [95% CI: 2.3–12.9]). The presence of inducible WMA was of incremental value for the risk stratification of patients with and without inducible perfusion deficits. Perfusion deficits contributed to poorer outcome only in the absence of diagnosed inducible WMA.
Vessel Wall Imaging and Molecular Markers
CT Angiography and Calcium Scoring
Over the last decade, CT angiography and coronary calcium scanning scoring have emerged as rapid and noninvasive tools for the assessment of coronary arteries. While the detection of coronary atherosclerosis with these techniques is useful for risk stratification [33], and can indicate the need for medical management of CAD, it remains unclear if these techniques can provide enough prognostic power to dictate the need for revascularization on their own. Significantly, diagnostic evidence of atherosclerosis as determined by coronary calcium scanning probably does not confer a markedly increased risk of cardiac events in the absence of ischemia [34]. The converse is not true. In patients without significant epicardial coronary stenosis evident at angiography, a positive stress SPECT is still found to confer an increased risk of cardiac events [35].
Small, single-center studies examining prognosis following CT angiography are beginning to enter the literature. Russo et al. [36] recently reported on a series of 441 patients with suspected CAD who underwent coronary 16-slice multidetector CT angiography and calcium scoring, then were subsequently followed for a mean of 32 months for cardiac death, nonfatal MI, and unstable angina requiring hospitalization. In this cohort (average age 59.7 years, 72% male), an excellent prognosis was noted in patients with normal coronary arteries (annualized event rate of 0.88%). The presence of CAD was diagnosed in 67% of patients and was associated with increased risk for events, which was higher (8.09% person-year) in patients with significant coronary stenoses but was not negligible (3.89%) in subjects with nonobstructive disease. CT angiography provided an additional incremental prognostic value as compared with a baseline clinical risk model plus calcium scoring when considering both nonobstructive versus obstructive CAD. Interestingly, an independent predictor of events was the presence of mixed/noncalcified plaques, regardless of lesion severity.
CMR
CMR is not at present capable of the same degree of spatial resolution as is available with multislice CT angiography. This reality has somewhat slowed the development of MR-based imaging of coronaries in favor of the development of CT-based modalities. Nevertheless, CMR does offer advantages over CT in its superior ability to characterize the content of tissues in the vascular wall. This ability to characterize plaque is of increasing interest, given the realization that mixed plaques identified by CT may have prognostic significance over and above luminal narrowing. The most common approach to vascular wall imaging with CMR uses dual-inversion recovery prepulses to null the signal from the coronary lumen blood pool. With such a noninvasive technique, in vivo human coronary vessel wall imaging has already been successfully performed [37, 38]. Studies to determine the prognostic significance of vascular wall findings by CMR remain to be done. A disadvantage of these techniques is the long scan time required. However, recent advances in phase-sensitive inversion recovery techniques may speed image acquisition time [39].
In addition to the T1 and T2-weighted imaging of vascular wall plaque, it has been proposed that the use of targeted molecular markers in combination with CMR imaging would provide the ultimate manifestation of tissue characterization. A limiting factor in the development of these molecular markers has been the regulatory hurdles required for the adoption of any new bioactive compound that might be used as such a marker.
Given this limitation, the more recent approach to molecular markers has been to identify paramagnetic markers that are either already approved for diagnostic or therapeutic use, or are closely related to these compounds. Iron compounds represent an important candidate. Iron particles have been shown to be preferentially endocytosed by macrophages in the vascular wall, and the presence of these iron particles can subsequently be identified on CMR [40]. Several studies have addressed the identification of regions of vascular inflammation within the vascular bed as a potential marker of increased cardiac risk. The recruitment of macrophages to atherosclerotic plaque has been hypothesized to be a marker of plaque instability and increased risk of thromboembolic events [41]. Thus, the identification of macrophage-enriched regions of the vasculature using iron particles may prove a useful diagnostic approach.
Conclusions
Cardiac imaging techniques continue to develop at an impressive pace and the evidence will ultimately determine which of these techniques demonstrate utility in clinical medicine and which do not. Today, noninvasive imaging of the coronary vasculature is highly accurate in determining both the presence of coronary disease and in providing useful prognostic information. However, knowledge of the anatomic appearance of the vascular bed cannot on its own provide a rational approach to management of the patient with coronary disease. Additional information regarding parameters such as left ventricular function, ischemic burden, and myocardial viability all provide critical information which helps direct an appropriate treatment plan.
In the future, cardiac imaging will likely provide information not just on the current burden of CAD, but also on the likelihood of progression of disease. Improved imaging of vascular inflammation and a better understanding of the outcomes associated with specific findings on images will contribute to our knowledge. The efficient and appropriate use of these technologies is already improving our management of cardiac ischemia, and this is set to continue.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Emond M, Mock MB, Davis KB, et al. Long-term survival of medically treated patients in the Coronary Artery Surgery Study (CASS) Registry. Circulation, 1994:2645–57.
Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 2003;107:2900–7.
Boden WE, O’Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med, 2007:1503–16.
Shaw LJ, Berman DS, Maron DJ, et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation, 2008:1283–91.
Simoons ML, Windecker S. Controversies in cardiovascular medicine: Chronic stable coronary artery disease: drugs vs. revascularization. European heart journal 2010;31:530–41.
• Tonino P, Fearon W, De Bruyne B, et al. Angiographic Versus Functional Severity of Coronary Artery Stenoses in the FAME Study: Fractional Flow Reserve Versus Angiography in Multivessel Evaluation. Journal of the American College of Cardiology, 2010:2816–2821. This is an important contribution that reinforces the concept of difference between functional ischemia and angiographic appearance of a stenosis.
Shaw L. Prognostic value of gated myocardial perfusion SPECT. Journal of Nuclear Cardiology, 2004:171–185.
Marwick T, Shan K, Patel S, Go RT, Lauer MS. Incremental value of rubidium-82 positron emission tomography for prognostic assessment of known or suspected coronary artery disease. Am J Cardiol 1997;80:6.
• Schwitter J, Wacker C, Van Rossum A, et al. MR-IMPACT: comparison of perfusion-cardiac magnetic resonance with single-photon emission computed tomography for the detection of coronary artery disease in a multicentre, multivendor, randomized trial. European heart journal, 2008:480. This is the first multicenter trial comparing the diagnostic performance of stress perfusion CMR to SPECT.
•• Hamon M, Fau G, Née G, Ehtisham J, Morello R, Hamon M. Meta-analysis of the diagnostic performance of stress perfusion cardiovascular magnetic resonance for detection of coronary artery disease. JCMR 2010;12:10. Meta-analysis providing up-to-date data on the diagnostic performance of CMR as reported over multiple recent trials.
Pilz g, Klos M, Ali E, Hoefling B, Scheck R, Bernhardt P. Angiographic correlations of patients with small vessel disease diagnosed by adenosine stress cardiac magnetic resonance imaging. JCMR 2008; 10:8.
Jahnke C, Nagel E, Gebker R, et al. Prognostic Value of Cardiac Magnetic Resonance Stress Tests: Adenosine Stress Perfusion and Dobutamine Stress Wall Motion Imaging. Circulation, 2007:1769–1776.
Lerakis S, McLean D, Anadiotis A, et al. Prognostic value of adenosine stress cardiovascular magnetic resonance in patients with low-risk chest pain. Journal of Cardiovascular Magnetic Resonance, 2009:37.
Spuentrup E, Ruhl KM, Botnar RM, et al. Molecular magnetic resonance imaging of myocardial perfusion with EP-3600, a collagen-specific contrast agent: initial feasibility study in a swine model. Circulation, 2009:1768–75.
• Kurita T, Sakuma H, Onishi K, et al. Regional myocardial perfusion reserve determined using myocardial perfusion magnetic resonance imaging showed a direct correlation with coronary flow velocity reserve by Doppler flow wire. European heart journal, 2008. This is an elegant study comparing Doppler flow wire measurements at cardiac catheterization with CMR perfusion.
Watkins S, McGeoch R, Lyne J, et al. Validation of magnetic resonance myocardial perfusion imaging with fractional flow reserve for the detection of significant coronary heart disease. Circulation, 2009:2207–13.
•• Patel A, Antkowiak P, Nandalur K, et al. Assessment of Advanced Coronary Artery Disease: Advantages of Quantitative Cardiac Magnetic Resonance Perfusion Analysis. Journal of the American College of Cardiology, 2010:561. A systematic look at the additional information obtained when performing quantitative perfusion analysis of CMR stress perfusion as compared to subjective evaluation. A persuasive argument in favor of quantitative studies.
Kim R. Viability Assessment by Delayed Enhancement Cardiovascular Magnetic Resonance: Will Low-Dose Dobutamine Dull the Shine? Circulation 2004;109:2476–2479.
Simonetti OP, Kim, R.J., Fieno, D.S., Hillenbrand, H.B., Wu, E., Bundy, J.M., Finn, J.P., Judd, R.M. . An improved MR imaging technique for the visualization of myocardial infarction. Radiology 2001;218:8.
Plein S, Younger J, Sparrow P, Ridgway J, Ball S, Greenwood J. Cardiovascular magnetic resonance of scar and ischemia burden early after acute ST elevation and non-ST elevation myocardial infarction. Journal of Cardiovascular Magnetic Resonance, 2008:47.
• Steel K, Broderick R, Gandla V, et al. Complementary prognostic values of stress myocardial perfusion and late gadolinium enhancement imaging by cardiac magnetic resonance in patients with known or suspected coronary artery disease. Circulation, 2009:1390. This article presents data supporting the combination of stress perfusion with late enhancement analysis. Techniques are shown to provide independent prognostic information.
Heinz-Peer G, Neruda A, Watschinger B, et al. Prevalence of NSF following intravenous gadolinium-contrast media administration in dialysis patients with endstage renal disease. Eur J Radiol;76:129–34.
Thomsen HS, Morcos SK, Dawson P. Is there a causal relation between the administration of gadolinium based contrast media and the development of nephrogenic systemic fibrosis (NSF)? Clin Radiol 2006;61:905–6.
• Wang D, Bi X, Avants B, Meng T. Estimation of perfusion and arterial transit time in myocardium using free-breathing myocardial arterial spin labeling with navigator-echo. Magnetic Resonance in Medicine 2010;64:1289–95. Technical paper advances flow imaging of the coronary arteries.
• Karamitsos T, Leccisotti L, Arnold J, et al. Relationship between regional myocardial oxygenation and perfusion in patients with coronary artery disease: insights from cardiovascular magnetic resonance and positron emission tomography. Circulation: Cardiovascular Imaging, 2009. This well-done study compares PET coronary flow data with BOLD myocardial oxygenation data. It presents evidence suggesting that limitation of myocardial blood supply does not equate to myocardial ischemia.
Friedrich MG. Testing for myocardial ischemia: the end of surrogates? JACC Cardiovasc Imaging 2010;3:385–7.
Vohringer M, Flewitt JA, Green JD, et al. Oxygenation-sensitive CMR for assessing vasodilator-induced changes of myocardial oxygenation. J Cardiovasc Magn Reson 2010;12:20.
• McCommis K, Goldstein T, Abendschein D, et al. Quantification of regional myocardial oxygenation by magnetic resonance imaging: validation with positron emission tomography. Circulation: Cardiovascular Imaging, 2009. This proof-of-concept BOLD imaging paper compares PET flow data with BOLD oxygenation imaging in a large animal model.
• Manka R, Paetsch I, Schnackenburg B. BOLD cardiovascular magnetic resonance at 3. 0 tesla in myocardial ischemia. J. Cardiovasc Magn Reson 2010;12:54. BOLD imaging at 3.0 T is shown to be clinically feasible.
•• Jahnke C, Gebker R, Manka R, Schnackenburg B, Fleck E, Paetsch I. Navigator-gated 3D blood oxygen level-dependent CMR at 3.0-T for detection of stress-induced myocardial ischemic reactions. JACC Cardiovasc Imaging 2010;3:375–84. BOLD imaging at 3.0 T is shown to be clinically feasible; compares stress-rest perfusion to BOLD and angiographic results.
Yao SS, Qureshi, E., Sherrid, M.V., Chaudhry, F.A., . Practical applications in stress echocardiography: risk stratification and prognosis in patients with known or suspected ischemic heart disease. J Am Coll Cardiol 2003;42:6.
Korosoglou G, Elhmidi Y, Steen H, et al. Prognostic value of high-dose dobutamine stress magnetic resonance imaging in 1,493 consecutive patients: assessment of myocardial wall motion and perfusion. J Am Coll Cardiol, 2010:1225–34.
Budoff MJ, Diamond GA, Raggi P, et al. Continuous probabilistic prediction of angiographically significant coronary artery disease using electron beam tomography. Circulation 2002;105:1791–6.
Rozanski A, Gransar H, Wong ND, et al. Clinical outcomes after both coronary calcium scanning and exercise myocardial perfusion scintigraphy. J Am Coll Cardiol 2007;49:1352–61.
Adamu U, Knollmann D, Almutairi B, et al. Stress/rest myocardial perfusion scintigraphy in patients without significant coronary artery disease. Journal of Nuclear Cardiology, 2010:38–44.
Russo V, Zavalloni A, Bacchi Reggiani ML, et al. Incremental Prognostic Value of Coronary CT Angiography in Patients With Suspected Coronary Artery Disease. Circulation: Cardiovascular Imaging 2010;3:351–359.
Kim WY. Three-Dimensional Black-Blood Cardiac Magnetic Resonance Coronary Vessel Wall Imaging Detects Positive Arterial Remodeling in Patients With Nonsignificant Coronary Artery Disease. Circulation 2002;106:296–299.
Kim WY, Astrup AS, Stuber M, et al. Subclinical coronary and aortic atherosclerosis detected by magnetic resonance imaging in type 1 diabetes with and without diabetic nephropathy. Circulation 2007;115:228–35.
Abd-Elmoniem KZ, Weiss RG, Stuber M. Phase-sensitive black-blood coronary vessel wall imaging. Magn Reson Med, 2010:1021–30.
Morishige K, Kacher DF, Libby P, et al. High-Resolution Magnetic Resonance Imaging Enhanced With Superparamagnetic Nanoparticles Measures Macrophage Burden in Atherosclerosis. Circulation, 2010:1–10.
Libby P. Inflammation and Atherosclerosis. Circulation, 2002:1135–1143.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Howarth, A.G., Friedrich, M.G. Imaging as an End Point in Ischemia Trials. Curr Cardiovasc Imaging Rep 4, 90–97 (2011). https://doi.org/10.1007/s12410-011-9068-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12410-011-9068-6