Abstract
Exposure to volatile organic compounds (VOCs) during the fetal period may induce negative effects on children’s health (e.g. increased risk of low birth weight and imbalanced development). Whereas VOCs have been analysed extensively in various human biological fluids (i.e. urine, blood, and breath), during pregnancy only urine has been studied and no work has been performed on amniotic fluid (AF), which is in direct contact with the fetus and is essential for its well-balanced development and maturation. This study aimed to detect VOCs in AF and to investigate their links to the lifestyle habits of pregnant women. The VOC composition of the AF collected from 76 healthy pregnant women was analysed using a gas chromatograph coupled to a mass spectrometer. The sources of VOC exposure in pregnant women were assessed using a questionnaire about their home living conditions and their professional exposure. A total of 126 VOCs belonging to 13 chemical families were detected in AF. The majority of these VOCs (92) had an exogenous origin, and their presence was linked to lifestyle habits, especially smoking and fragrance use. Considering the direct contact of these VOCs with multiple fetal organs, this study is an important contribution to the literature exploring the future potential relationships between VOCs and abnormal fetal development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Volatile organic compounds (VOCs) are compounds containing at least one carbon atom and one or more other elements, such as hydrogen, oxygen, or nitrogen. In addition, these compounds are characterized by their high volatility, switching easily from liquid to gaseous states under normal conditions of pressure and temperature. Their negative effects on health have been extensively studied and depend on the nature of the exposure: acute or chronic, and single or combined. Acute exposure to VOCs usually induces irritation of the respiratory tract, skin, and eyes (Takahashi et al. 2007) and damage to the central nervous system (Neubert 2001), which are usually transient. Exposure to low concentrations of VOCs over a long period can affect the body with carcinogenic effects (Yin et al. 1996) and alterations in reproductive functions (Luderer et al. 2004) in fetal development (Hooiveld 2006). In addition, the negative effects of these molecules on health are almost more significant if exposure occurs early in life. Therefore, exposure to VOCs during the fetal period (1) may induce an increased risk of low birth weight (Ghosh et al. 2013; Miller et al. 2020) and preterm birth (Santos and Nascimento 2019; Cassidy-Bushrow et al. 2020; Miller et al. 2020), (2) may adversely affect early postnatal growth (Chang et al. 2017) and neurobehavioural development in the early life stage (Chang et al. 2018; Nakaoka et al. 2021), and (3) may be related to wheezing in early infancy (Franck et al. 2014). Benzene, toluene, and ethylbenzene are the VOCs most frequently linked with adverse birth outcomes, probably because these compounds are the most studied since they are recognized environmental pollutants (Zhou et al. 2023) with well-described toxic properties (mutagenic, carcinogenic, reprotoxic). In addition, they may have negative impacts on maternal health through oxidative stress (Chen et al. 2023), inflammation (Cassidy-Bushrow et al. 2021), and epigenetic change (Yusoff et al. 2023).
Approximately 3000 different VOCs have been detected in expired human air. They have been detected in urine, blood (Miekisch et al. 2001), stool (Frau et al. 2021), and saliva, but it is in breath (Amann et al. 2014) that these compounds have been extensively studied. Most of these samples contained more than 200 VOCs. Their origins may be endogenous or exogenous. VOCs with endogenous origins may result from intestinal bacterial activity (Bone et al. 1976; Cope et al. 2000) or metabolic processes, such as protein oxidation by fecal flora (Miekisch et al. 2004), sulfur amino acid degradation (Scislowski and Pickard 1994; Luo et al. 2011), or sugar catabolism (i.e. the Embden–Meyerhof–Parnas pathway and lactic fermentation) (Miller and Wolin 1979). In addition, studies investigating the chemical composition of exhaled air from patients with various diseases have provided useful insights into the metabolic processes that produce endogenous VOCs. Breath alkane (pentane) output is a good index of lipid peroxidation (Kohlmuller and Kochen 1993; Mendis et al. 1995; Shin et al. 1997; Aghdassi and Allard 2000; Miekisch et al. 2001, 2004); sulfur-containing compounds are considered markers of liver impairment (Scislowski and Pickard 1994); change in isoprene concentration has been related to cholesterol metabolism (Karl et al. 2001); a high level of acetone is a long-recognized and useful marker of uncontrolled diabetes mellitus (Lebovitz 1995); derivates of heptane arise during pulmonary tuberculosis (Phillips et al. 2007); and the use of VOCs as cancer biomarkers, especially for lung cancer, has been extensively studied in the literature (Chen et al. 2007; Bajtarevic et al. 2009; Matsumura et al. 2010). In terms of their exogenous production, various and numerous products in daily use may cause VOC exposure, such as cleaning products, paints, solvents, personal care products, automotive exhaust, or tobacco smoking. They may be absorbed as contaminants through the skin or taken up via inhalation or ingestion.
Although VOCs have been measured in various biological fluids, their characterization in human amniotic fluid (AF) has not been investigated to date. This physiological liquid contained in the amnion cavity constitutes a protective area around the conceptus, allowing its movement and harmonious growth. Aside from its physical protective effects (mechanical and thermal protection), AF also plays a biochemical defensive role and is an essential component of normal fetal development and morphogenic maturation. It is also a dynamically changing nutrient reservoir that includes fetal and maternal proteins, amino acids, carbohydrates, hormones, lipids, and electrolytes. This complex composition results from the diffusion of metabolites and water from maternal plasma, placenta, and developing fetal urinary, respiratory, and alimentary tracts.
Considering the potential negative effects of VOC exposure during the fetal period and the anatomical direct (cutaneous or inhalation) contact of the fetus with AF during pregnancy, this study aimed to detect these molecules in AF at the end of normal pregnancy and investigate their links to the lifestyle habits of women during pregnancy.
Materials and Methods
Subject Information
This study was based on a prospective cohort of 76 pregnant women with amniocentesis in the second trimester of pregnancy for cytogenetic-based diagnostics recruited at the Clermont-Ferrand Teaching Hospital between January and September 2019. The inclusion criteria were pregnant women aged 18 years or older, with an agreement for the use of their AF, during a healthy pregnancy leading to a healthy baby with a normal karyotype. Maternal data (age, weight, size, body mass index, gestational age, and ethnic group), mode of delivery (natural delivery or caesarean), and clinical information about the newborn (sex, size, weight, head circumference, and Apgar score at birth) were obtained from obstetrical and neonatal medical records and individual questionnaires filled out at the time of sample collection. Information about the smoking, alcohol consumption, family antecedents, or medicine taking of the pregnant women was collected from this questionnaire. The questionnaire also included questions about home characteristics and living conditions: rural or city housing, type of heating (gas, wood, electric, or fuel oil), and use of air fresheners or cosmetic care products, such as fragrances. The personal or professional use of solvents (e.g. paints, floor varnishes, and glues) was also noted. In order to estimate potential occupational exposure to VOCs, the profession the participants was also required. All the subjects signed an informed consent form, and the protocol was approved by the local ethics committee. The project was authorized by the Ethics Committee CPP Sud-Est VI, with CPP reference no. AU 765 and CODECOH no. DC-2008-558.
Sample Collection Protocol
Immediately after amniocentesis, 5 mL of amniotic liquid was transferred to a 10 mL glass vial sealed with butyl-Teflon septum caps and stored at − 80 °C before analysis (VWR International, France).
VOC Extraction and Analysis
The VOCs were extracted using a multi-purpose sampler (model MPS2, GERSTEL, Baltimore, MD, USA) through the following steps: pre-heating of the sample for 60 min at 70 °C using a stirrer (250 rpm), trapping of the volatile compounds of the headspace for 30 min at 20 °C using a solid phase microextraction fibre (75 µm carboxen-polydimethylsiloxane for Merlin Microseal, 23 gauge needle, auto holder, Supelco, Bellefonte, PA, USA), and thermal desorption of the trapped volatile compounds by introducing the fibre into a gas chromatograph (GC) injector. The splitless injection of volatile components into a GC (GC6890, Agilent) coupled to a mass spectrometer (MS5973, Agilent) was achieved through the thermal desorption of the fibre at 280 °C. The desorbed compounds were then separated through high-resolution gas-phase chromatography (capillary column SPB-5: 60 m length × 0.32 mm i.d. × 1 μm film thickness) (Supelco, Bellefonte, PA, USA). The oven temperature of the GC was maintained at 40 °C for 5 min and increased to 230 °C for 2 min, according to a gradient of 3 °C/min. Helium (99.9999% pure, Messer) was used as a carrier gas at a constant flow rate of 1 mL/min. The temperature of the GC–MS interface was 280 °C. The electron impact energy was set to 70 eV, and data were collected in the range of 20–250 atomic mass units (amu) in the first 10 min and in the range of 33–300 amu from 10 to 70 min. Identification was performed by comparing the experimental spectra with those of the Wiley275 mass spectral database (Hewlett-Packard Co., 1995) and by comparing the retention indices with those of the Bio-Sens internal database (VOCELIA®). For every VOC identified in the samples, abundance was calculated by measuring the peak area. The results were expressed as relative abundance (%) and were calculated by dividing the abundance of each compound by the abundance sum of all the compounds detected. Four external standards were used to correct the instrumental signal drifts: 1-bromo-butane (purity 99.7%), 1-bromo-decane (purity 98%), 1-bromo-heptane (purity 99.0%), and 1, 4-dibromobenzene (purity 98.0%) (Sigma-Aldrich Chimie, St-Quentin-Fallavier, France). The retention indices of these standards were distributed evenly over the sample GC chromatograms. The standards were analysed using the same analytical conditions as in the samples.
Statistics
Statistical analysis was performed using R software (http://www.R-project.org). The continuous data were presented according to a statistical distribution using the mean ± standard deviation. The assumption of normality was checked using normal probability plots and the Shapiro–Wilk test. To (i) analyse the relationships between the VOCs and the living conditions of the population, such as smoking, type of heating, usage of air fresheners and fragrance, and exposure to solvents, and to (ii) identify the groups of patients with similar VOCs, factorial analyses were performed rather than the more conventional statistical inferential approaches. The significance of the association was tested using the chi-square or Fisher’s exact test, which did not provide information on the significant individual associations between row–column pairs. Factorial analyses show how the variables are related, not just whether a relationship exists, and can handle a large amount of data to unfold hidden patterns. A two-step statistical plan analysis was proposed. In the first step, multiple correspondence analysis (MCA)—which is an extension of correspondence analysis or a generalization of principal component analysis (PCA) for categorical variables rather than quantitative variables—was applied to study the associations between VOCs and living conditions. MCA is an exploratory method that performs cross-tabulations, and it can be considered a useful tool for uncovering the relationships between categorical variables (Sourial et al. 2010). Whereas PCA is preferred for continuous parameters, MCA is applied to contingency tables, with the aim of transforming a table of numerical information into a graphical display in which each row and each column are illustrated as a point. All variables in a data set can be related to each other without differentiation between the explanatory and descriptive variables. The result is a representation of the two first discriminant plane projections of the discriminant scores of the patients and VOCs. Because the objective of the MCA was to determine profiles, it was impossible to consider VOCs that were not discriminating (always present or still absent) for this analysis. Thus, we used only VOCs present in 10–90% of the pregnant women. In the second step, hierarchical clustering (HC) was used to confirm groups of patients sufficiently close according to the relationships between the VOCs and living conditions as defined by MCA. HC does not require pre-specifying the number of clusters to be generated. To determine which clusters should be combined, a measure of dissimilarity between the sets of observations and a linkage criterion (Ward’s minimum variance method), which specifies the dissimilarity of sets as a function of the pairwise distances of observations in the sets, were defined. To apply this method, in the initial step, all clusters are singletons. Then, in each step, the pair of clusters that leads to a minimum increase in the total within-cluster variance after merging is determined. This increase is a weighted squared distance between the cluster centres. To apply a recursive algorithm under this objective function, the initial distance between the individual objects must be proportional to the squared Euclidean distance. The result is a tree-based representation of the observations called a dendrogram, which uses a pairwise distance matrix between patients as a clustering criterion.
Results
Description of the Population
The AF samples were collected from 76 pregnant women aged 20–43 years who underwent amniocentesis in the second trimester of pregnancy (gestational age 17.9 ± 1.6 weeks) for cytogenetic-based diagnostics. The maternal data are summarized in Table 1. Delivery was spontaneous in 88.2% of the women and occurred through natural birth in 77.6%. The rate of caesarean delivery was 22.4%, of which 41.2% were planned. Concerning the newborn sex ratio, 52.6% were female, and 47.4% were male. The average size of the newborns was 49.8 ± 2.1 cm. The Apgar scores were 8.7 ± 1.3, 9.5 ± 1.0, and 9.8 ± 0.5 at 1, 5, and 10 min after birth, respectively. As in previous parameters, the mean birth weight (3252 ± 503 g) and head circumference (34.6 ± 2.1 cm) were also in the usual range. The outcome was normal for all newborns included.
Home Characteristics, Living Conditions, and Professional Situation
Overall, 51.7% of the pregnant women lived in rural areas and 48.3% in cities (Table 1). Gas was the most-used type of heating (46.1%) (Table 1). The majority of the women used cosmetic care products, such as fragrances, whereas few of them used air fresheners (Table 1). A total of 28% of subjects worked in the medical field, in hairdressing, in hotels, or did household or agricultural work and were considered to be occupationally exposed, whereas the others, without a profession or with an administrative job, were considered not professionally exposed (Table 1). The percentage of pregnant women potentially occupationally exposed (28%) was comparable with the percentage of pregnant women who auto-declared the use of solvents (personal or professional) (22.4%).
Volatile Organic Compounds
A total of 126 different VOCs were detected in human AF. Table 2 shows the chemical classification, frequency, relative abundance, and origins of the VOCs. The identified VOCs belonged to 13 chemical families. They were present in 2.6–100% of the AF samples, and their relative abundance was 0.002–63.300. With a higher relative abundance (63.300), acetone was quantitatively the most important VOC detected and was present in all 76 AF samples tested. Among the 126 VOCs detected, 29 others, aside from acetone, were present in all the AF samples, and 8 of them had a relative abundance higher than 1: benzaldehyde, p-cymene, diphenyl ether, propan-2-ol, propan-1-ol, 4-Methylpentan-1-ol, butan-2-one, and pentan-2one. Benzaldehyde is known to be implicated in the metabolic pathway of phenylalanine, and p-cymene is present in essential oils (cosmetic and alimentary products). Most of the VOCs identified (92/126) were from exogenous origins and belonged to chemical families, such as alkanes, Maillard compounds, benzenes, halogens, terpenes, and ethers. The endogenous or exogenous origin of these compounds was determined by performing bibliographic research in pubchem with the CAS number. According to the CMR codification (a European harmonized classification of carcinogenic (C), mutagenic (M), and toxicity for reproduction (R) substances), among the 126 VOCs detected, 3 of them were known to be carcinogenic (dichloromethane, trichloromethane, benzene), 1 (benzene) to be mutagenic, and 4 (styrene, toluene, carbon disulfide, trichloromethane) to be reprotoxic.
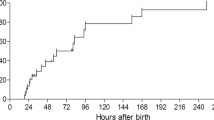
Statistical Links Between VOCs and Maternal Characteristics
Statistical analysis differentiated six clusters of patients characterized by specific VOC profiles and/or maternal characteristics in terms of living conditions (Fig. 1). Groups 1–6 were composed of 19, 11, 7, 12, 8, and 19 pregnant women, respectively. Each of the six VOC profiles was defined statistically by the presence of specific VOCs and the absence of others in the majority of patients from the cluster considered. Group 1 (Fig. 1a) was characterized by electric heating and a profile of 18 VOCs composed of MetCldiF, which was present in 100% of 19 pregnant women, and PaneN, 159cym, Oane, Bol3CH3, Oal, 2Hone4CH3, BoneCH3, Hone6CH3, ClBol, Fur25CH3, Fur3CH3, TetHfur, S2CH3, D3Car, Linalyl, Terpol, and 2PolMet, which were absent in the majority of the women in this cluster. BuTal and Ethol, which were also present in 100% of the women in this cluster, were not statistically identified as a characteristic of Group 1 because they were equally present in the majority of the women in the five other groups. Similarly, allyl, which was absent in 19 women in the group, was not specified for this cluster because it was also absent in almost all patients in the other 5 groups. The patients in Group 2 (Fig. 1b) were specified as non-solvent users, and their VOC profile was poor, as in Group 1. Group 2 was statistically characterized by the presence of Oal, x4ditert, and S2CH3 (in more than 75% of the women in this group) and by the almost total absence of nine compounds: tertBut, 2PoneDib, 2PolMet, Terpol, D3Car, Thii, Cymde, Bol3CH3, and 2Bol2CH3. The VOC profiles of Groups 1 and 2 can be clearly classified as poor because they were characterized by the absence of VOCs rather than by their presence. Group 3 (Fig. 1c) included seven patients who were characterized by smoking and a VOC profile constituting six compounds: AcCH3, which was absent in more than 75% of the women in this group, and PaneN, Benz, Sty, Fur25CH3, and Fur3CH3, which were present in all seven patients. Among these five compounds, four belonged to two chemical families (benzenes and Maillard compounds) and were all identified in the literature on tobacco or tobacco smoke. Groups 4 (Fig. 1d) and 5 (Fig. 1e) were characterized only by specific VOC profiles and not by lifestyle habits. Group 6 (Fig. 1f) was defined by the use of fragrance, smoking, and a rich VOC profile with 21 compounds (Oane, Tane, B2ol2CH3, Bol3CH3, Oal, 2Pone4CH3, Hone6CH3, Benzal, Fur24CH3, Fur3CH3, S02, D3Car, Euyptol, IsoMone, Linalool, Linalyl, Men3one, Terpol, AcCH3, AcPro2CH3, and Buteth) present in almost all 19 patients in this cluster, along with the absence of benzF. The 21 VOCs mostly had exogenous origins, with 11 identified in the literature on tobacco or tobacco smoke and 17 known to be present in fragrances. Most of the Group 6 specific compounds (7/22) were terpenes.
Volatile organic compound (VOC) profiles. Volatile organic compound (VOC) profiles and lifestyle habits of the six clusters of pregnant women. Statistical analyses were performed only on the VOCs (n = 58) present in 10–90% of the pregnant women. Six clusters (Groups 1 (a), 2 (b), 3 (c), 4 (d), 5 (e), 6 (f)) of patients were identified using specific VOC profiles and/or lifestyle habits. *VOC and lifestyle habit characteristics of the cluster considered. For these specific compounds, we determined whether they were known to be present in fragrance (P), tobacco, or smoke (C) and whether they had endogenous (En) or exogenous (Ex) origins. The figures are interpreted in relation to the others. The correspondence between the abbreviated and complete names of the chemical compounds is described in Table 2
Discussion
Considering the potential negative effects of VOCs on fetal health, their significant emissions in atmospheric air due to pollution, and their presence in various and numerous products of daily use, VOC exposure during pregnancy is interesting to investigate to evaluate their effects on the fetus. Works studying the fetal exposure of VOC and the adverse outcome in health have adopted a traditional approach by predicting air pollution with mathematical models (Williams et al. 2019; Nakhjirgan et al. 2019) or with questionnaires (Nakaoka et al. 2021). Other studies have measured VOC concentrations in indoor/outdoor air (Ghosh et al. 2013; Helen et al. 2015; Chang et al. 2017, 2018; Caron-Beaudoin et al. 2022; Ghassabian et al. 2023), or measured the metabolites of these compounds in the body fluid (urine) (Boyle et al. 2016; Caron-Beaudoin et al. 2018; Weinstein et al. 2020; Ronde et al. 2022; Li et al. 2023) of pregnant women. With advances in analytical techniques, human biomonitoring involving measurement of biomarkers in body fluids, such as blood, urine, or exhaled air, is recognized as a more appropriate method for assessing health risk than environmental monitoring, since it evaluates the internal dose, achieving an estimate of the biologically active burden of the chemicals. The strength and the originality of our work lies in the fact that (1) it evaluated fetal exposure to VOCs by measuring the concentrations of these compounds not in the pregnant women’s fluids (blood or urine) but directly in a fetal fluid (AF) and (2) it did not focus on quantitative determination of specific VOCs but performed a broad screening of these compounds. A limitation of the study is that the screening method is semi-quantitative, so the level of VOCs obtained (Table 2) is expressed in relative abundance and cannot be compared with the majority of the results from other studies. Only one previous study examined these compounds in a fetal biological fluid—the blood cord—but on a limited panel of compounds (Dowty et al. 1976). The VOCs present in AF reflect maternal–foetal passage, and the fetus is bathed in AF; hence, it is in direct (cutaneous or inhalation) contact with these compounds, so measuring them in this fluid provides the best estimate of fetal exposure, whereas measurement of these compounds in maternal fluids or ambient air only provides an indirect and incomplete estimate of exposure.
In the literature, there are no data on the concentration of VOCs in the blood of pregnant women, since works which have used human biomonitoring to assess VOC exposure during pregnancy measured these chemical compounds only in urine, probably because of the ease with which it can be collected (no invasiveness of sampling and no need for the presence of professional operators). VOC metabolites in urine are considered reliable biomarkers for assessing exposure to VOCs owing to their specificity and their longer half-lives in the human body compared to the parent compounds (Alwis et al. 2012). After entering the body, VOCs are mainly metabolized by the hepatic cytochrome P450 pathway and excreted through urine (Alwis et al. 2012; Ghosh et al. 2013). Our study showed the presence of VOCs (parent compounds) in AF, which may indicate direct passage of these compounds through placental transfer and a lack of metabolism by the immature fetal liver.
To identify the sources of VOC exposure, we used a questionnaire—an indirect approach whose accuracy is dependent on the participants’ honesty. We established that many VOCs (n = 126) were present in the AF, with the majority resulting from environmental (exogenous) sources. We identified more VOCs (126) in the AF samples of pregnant women than in Dowty et al.’s study in 1976 (Dowty et al. 1976). In this previous work, only 12 VOCs were identified in blood cord. This difference is probably due to the better sensitivity of our analytical methodology and the smaller sample size of pregnant women recruited in this previous work (n = 11). However, this observation could suggest that exposure to environmental sources of VOCs is actually more frequent now than in the past. Home living conditions, smoking, use of fragrances, and non-use of solvents were associated with a specific VOC profile. Thus, the six groups of pregnant women were identified according to their living conditions and VOC profiles. Group 3 was particularly interesting because it was characterized by smoking and the presence of VOCs (4/5) that belong to the chemical families of benzene and Maillard compounds, known to be present in smoking or tobacco components. Among these VOCs, 2,5-dimethylfuran is a highly selective breath biomarker of active smoking and a robust marker of smoking contamination in indoor environments (Gordon et al. 2002; Alonso et al. 2010). We confirmed a direct association between smoking and the finding of tobacco metabolite constituents in AF, as previously described by Boyle et al. (2016) in pregnant women. However, in their study, VOCs were not measured in AF but in urine. Considering the carcinogenic and mutagenic properties of these compounds, their presence in AF supports the hypothesis of the negative effects of maternal (active or passive) smoking on newborns’ health. Smoking and fragrance use also characterized Group 6. Its VOC profile was consistent with these lifestyle habits. In included components identified in cigarettes and those that belong to the chemical family of terpene compounds known to be present in fragrances. Potential occupational exposure was not associated with a VOC profile. However, this result should be analysed with caution because occupational exposure was not assessed by measuring VOC levels in the professional environment of the participants but was estimated from their jobs.
Among the 126 VOCs identified, acetone had the highest relative abundance (63.3%) and was present in 100% of the AF samples. Under physiological conditions, acetone is produced by hepatocytes through the decarboxylation of acetoacetate, which is derived from lipolysis or lipid peroxidation. Ketone bodies in the blood, including acetoacetate and β-hydroxybutyrate, increase in all physiological situations (e.g. fasting, starving, or during a high-fat diet) in which the body uses fat instead of glucose for energy production (Laffel 1999). In terms of the origin of acetone in AF, it cannot be produced by the fetus because ketogenesis is not active but is of maternal origin. Maternal plasma ketone body levels increase as a consequence of physiologically enhanced adipose tissue lipolysis during pregnancy (free fatty acid oxidation and ketone body synthesis) (Bonvallot et al. 2013). The presence of acetone in AF is also explained by the fact that this compound can easily pass through the placenta (Herrera and Amusquivar 2000). Therefore, the fetus benefits from this product of maternal fatty acid metabolism. The activity of ketone body-metabolizing enzymes is present in fetal tissues (brain, liver, and kidney) and can be increased by conditions of maternal ketonemia, such as starvation during late pregnancy or high-fat feeding. These changes may represent an important adaptation to guarantee fetal brain development through the condition of limited availability of other substrates and a special preservation of this organ (Herrera 2002).
In this study, numerous (126) VOCS were identified in AF, and although some of them, such as dichloromethane, trichloromethane, benzene, styrene, toluene, and carbon disulfide, are well-known to be especially toxic, this was not correlated with adverse outcomes for newborns. This result is comparable to those of Nakhjirgan et al. (2019), who also observed no association between low body weight and VOC exposure, but is different from various studies that show a link between VOC exposure and adverse outcome at birth. These works are generally epidemiological retrospective studies which estimate VOC exposure by calculation. Hence, they are limited by their reliance on estimated exposure and thus are subject to bias due to potential exposure misclassification. In addition, these studies have often been performed in highly polluted areas, which may mean that the doses of pollutants involved were higher than those measured in this work, where pregnant women were recruited from the Auvergne, a French region with a medium level of industrialization and a low urban density. We may hypothesize that concentrations of VOCs were too low to induce toxic effects, and since this is a semi-quantitative study, comparison with safety criteria is not possible. The number of pregnant women is probably too low to observe an effect on birth outcome, contrary to epidemiological studies, which include a great number of participants. Finally, if prenatal exposure to toxicants is not associated with short-term adverse outcomes in this work, we cannot exclude the possibility that adverse long-term effects on the children’s health may develop. To study this point, it would be interesting to conduct a follow-up of the newborns during childhood with human fluid biomonitoring, as performed by Drago et al. (2020). In this birth cohort, named “Neonatal Environment and Health Outcomes” (NEHO), the authors have a project to measure VOCs in the placenta. Compared to this fetal matrix, the strength of AF is its simple composition (98% water plus electrolytes, proteins, peptides, carbohydrates, lipids, and hormones). Indeed, AF is classically studied to detect biomarkers, either of the normal development of the fetus or of the onset and evolution of disorders affecting the fetus’s or mother’s health (e.g. Down syndrome or intra-amniotic infection) (Smith and Blandford 1995).
Conclusion
Whereas the negative effects of VOCs on fetal or children’s health have been extensively studied by experimental or epidemiologic approaches, our study is the first to perform a broad screening of VOCs directly in a fetal fluid, AF, and to investigate their potential relationship with the lifestyle habits of women during normal pregnancy. This dynamic biological liquid is interesting to study because it allows for the monitoring of both the mother’s and the foetus’s health. In the AF samples collected from healthy pregnant women, 126 VOCs belonging to 13 chemical families were identified. The most abundant compound detected was the endogen metabolite acetone, which resulted from the mother’s fatty acid metabolism. Nevertheless, the majority of VOCs identified had exogenous origins (92/126) and were linked to lifestyle habits, especially smoking and fragrance use.
This study is the first to demonstrate the presence of and identify numerous VOCs in AF. Although some of them are known to be toxic, no adverse outcome for the newborns was observed, which may be explained by low VOC concentrations or small sample size. Future studies are now required to perform a quantitative determination of these components in order to compare levels with safety criteria and to evaluate the long-term issues of this early exposure to VOCs.
Data Availability
The data presented in this study are available upon request from the corresponding author.
References
Aghdassi E, Allard JP (2000) Breath alkanes as a marker of oxidative stress in different clinical conditions. Free Radic Biol Med 28:880–886. https://doi.org/10.1016/S0891-5849(00)00189-1
Alonso M, Godayol A, Anticó E, Sanchez JM (2010) Assessment of environmental tobacco smoke contamination in public premises: significance of 2,5-dimethylfuran as an effective marker. Environ Sci Technol 44:8289–8294. https://doi.org/10.1021/es1016075
Alwis KU, Blount BC, Britt AS et al (2012) Simultaneous analysis of 28 urinary VOC metabolites using ultra high performance liquid chromatography coupled with electrospray ionization tandem mass spectrometry (UPLC-ESI/MSMS). Anal Chim Acta 750:152–160. https://doi.org/10.1016/j.aca.2012.04.009
Amann A, de Costello BL, Miekisch W et al (2014) The human volatilome: volatile organic compounds (VOCs) in exhaled breath, skin emanations, urine, feces and saliva. J Breath Res 8:034001. https://doi.org/10.1088/1752-7155/8/3/034001
Bajtarevic A, Ager C, Pienz M et al (2009) Noninvasive detection of lung cancer by analysis of exhaled breath. BMC Cancer 9:348. https://doi.org/10.1186/1471-2407-9-348
Bone E, Tamm A, Hill M (1976) The production of urinary phenols by gut bacteria and their possible role in the causation of large bowel cancer. Am J Clin Nutr 29:1448–1454. https://doi.org/10.1093/ajcn/29.12.1448
Bonvallot N, Tremblay-Franco M, Chevrier C et al (2013) Metabolomics tools for describing complex pesticide exposure in pregnant women in Brittany (France). PLoS ONE 8:e64433. https://doi.org/10.1371/journal.pone.0064433
Boyle E, Viet S, Wright D et al (2016) Assessment of exposure to VOCs among pregnant women in the national children’s study. Int J Environ Res Public Health 13:376. https://doi.org/10.3390/ijerph13040376
Caron-Beaudoin É, Valter N, Chevrier J et al (2018) Gestational exposure to volatile organic compounds (VOCs) in northeastern British Columbia, Canada: a pilot study. Environ Int 110:131–138. https://doi.org/10.1016/j.envint.2017.10.022
Caron-Beaudoin É, Whyte KP, Bouchard MF et al (2022) Volatile organic compounds (VOCs) in indoor air and tap water samples in residences of pregnant women living in an area of unconventional natural gas operations: Findings from the EXPERIVA study. Sci Total Environ 805:150242. https://doi.org/10.1016/j.scitotenv.2021.150242
Cassidy-Bushrow AE, Burmeister C, Lamerato L et al (2020) Prenatal airshed pollutants and preterm birth in an observational birth cohort study in Detroit, Michigan, USA. Environ Res 189:109845. https://doi.org/10.1016/j.envres.2020.109845
Cassidy-Bushrow AE, Burmeister C, Birbeck J et al (2021) Ambient BTEX exposure and mid-pregnancy inflammatory biomarkers in pregnant African American women. J Reprod Immunol 145:103305. https://doi.org/10.1016/j.jri.2021.103305
Chang M, Park H, Ha M et al (2017) The effect of prenatal TVOC exposure on birth and infantile weight: the mothers and children’s environmental health study. Pediatr Res 82:423–428. https://doi.org/10.1038/pr.2017.55
Chang M, Lee D, Park H et al (2018) Prenatal TVOCs exposure negatively influences postnatal neurobehavioral development. Sci Total Environ 618:977–981. https://doi.org/10.1016/j.scitotenv.2017.09.046
Chen X, Xu F, Wang Y et al (2007) A study of the volatile organic compounds exhaled by lung cancer cells in vitro for breath diagnosis. Cancer 110:835–844. https://doi.org/10.1002/cncr.22844
Chen S, Wan Y, Qian X et al (2023) Urinary metabolites of multiple volatile organic compounds, oxidative stress biomarkers, and gestational diabetes mellitus: association analyses. Sci Total Environ 875:162370. https://doi.org/10.1016/j.scitotenv.2023.162370
Cope K, Risby T, Diehl AM (2000) Increased gastrointestinal ethanol production in obese mice: implications for fatty liver disease pathogenesis. Gastroenterology 119:1340–1347. https://doi.org/10.1053/gast.2000.19267
dos Santos DAA, Nascimento LFC (2019) Maternal exposure to benzene and toluene and preterm birth. A longitudinal study. Sao Paulo Med J 137:486–490. https://doi.org/10.1590/1516-3180.2019.0224170919
Dowty BJ, Laseter JL, Storer J (1976) The transplacental migration and accumulation in blood of volatile organic constituents. Pediatr Res 10:696–701. https://doi.org/10.1203/00006450-197607000-00013
Drago G, Ruggieri S, Bianchi F et al (2020) Birth cohorts in highly contaminated sites: a tool for monitoring the relationships between environmental pollutants and children’s health. Front Public Health 8:125. https://doi.org/10.3389/fpubh.2020.00125
Franck U, Weller A, Röder SW et al (2014) Prenatal VOC exposure and redecoration are related to wheezing in early infancy. Environ Int 73:393–401. https://doi.org/10.1016/j.envint.2014.08.013
Frau A, Lett L, Slater R et al (2021) The stool volatile metabolome of pre-term babies. Molecules 26:3341. https://doi.org/10.3390/molecules26113341
Ghassabian A, Afanasyeva Y, Yu K et al (2023) Characterisation of personalised air pollution exposure in pregnant women participating in a birth cohort study. Paediatric Perinatal Epidemiol 37:436–444. https://doi.org/10.1111/ppe.12960
Ghosh JKC, Wilhelm M, Ritz B (2013) Effects of residential indoor air quality and household ventilation on preterm birth and term low birth weight in Los Angeles County, California. Am J Public Health 103:686–694. https://doi.org/10.2105/AJPH.2012.300987
Gordon SM, Wallace LA, Brinkman MC et al (2002) Volatile organic compounds as breath biomarkers for active and passive smoking. Environ Health Perspect 110:689–698. https://doi.org/10.1289/ehp.02110689
Helen GST, Aguilar-Villalobos M, Adetona O et al (2015) Exposure of pregnant women to cookstove-related household air pollution in urban and periurban Trujillo, Peru. Arch Environ Occup Health 70:10–18. https://doi.org/10.1080/19338244.2013.807761
Herrera E (2002) Lipid metabolism in pregnancy and its consequences in the fetus and newborn. Endocrine 19:43–56. https://doi.org/10.1385/ENDO:19:1:43
Herrera E, Amusquivar E (2000) Lipid metabolism in the fetus and the newborn. Diabetes Metab Res 16:202–210. https://doi.org/10.1002/1520-7560(200005/06)16:3%3c202::AID-DMRR116%3e3.0.CO;2-#
Hooiveld M (2006) Adverse reproductive outcomes among male painters with occupational exposure to organic solvents. Occup Environ Med 63:538–544. https://doi.org/10.1136/oem.2005.026013
Karl T, Prazeller P, Mayr D et al (2001) Human breath isoprene and its relation to blood cholesterol levels: new measurements and modeling. J Appl Physiol 91:762–770. https://doi.org/10.1152/jappl.2001.91.2.762
Kohlmuller D, Kochen W (1993) Is n-pentane really an index of lipid peroxidation in humans and animals? A methodological reevaluation. Anal Biochem 210:268–276. https://doi.org/10.1006/abio.1993.1195
Laffel L (1999) Ketone bodies: a review of physiology, pathophysiology and application of monitoring to diabetes. Diabetes Metab Res Rev 15:412–426. https://doi.org/10.1002/(SICI)1520-7560(199911/12)15:6%3c412::AID-DMRR72%3e3.0.CO;2-8
Lebovitz HE (1995) Diabetic ketoacidosis. Lancet 345:767–772. https://doi.org/10.1016/S0140-6736(95)90645-2
Li M, Wan Y, Qian X et al (2023) Urinary metabolites of multiple volatile organic compounds among pregnant women across pregnancy: Variability, exposure characteristics, and associations with selected oxidative stress biomarkers. Environ Int 173:107816. https://doi.org/10.1016/j.envint.2023.107816
Luderer U, Bushley A, Stover BD et al (2004) Effects of occupational solvent exposure on reproductive hormone concentrations and fecundability in men. Am J Ind Med 46:614–626. https://doi.org/10.1002/ajim.20100
Luo L, Chen S, Jin H et al (2011) Endogenous generation of sulfur dioxide in rat tissues. Biochem Biophys Res Commun 415:61–67. https://doi.org/10.1016/j.bbrc.2011.10.012
Matsumura K, Opiekun M, Oka H et al (2010) Urinary volatile compounds as biomarkers for lung cancer: a proof of principle study using odor signatures in mouse models of lung cancer. PLoS ONE 5:e8819. https://doi.org/10.1371/journal.pone.0008819
Mendis S, Sobotka PA, Leia FL, Euler DE (1995) Breath pentane and plasma lipid peroxides in ischemic heart disease. Free Radic Biol Med 19:679–684. https://doi.org/10.1016/0891-5849(95)00053-Z
Miekisch W, Schubert JK, Vagts DA, Geiger K (2001) Analysis of volatile disease markers in blood. Clin Chem 47:1053–1060. https://doi.org/10.1093/clinchem/47.6.1053
Miekisch W, Schubert JK, Noeldge-Schomburg GFE (2004) Diagnostic potential of breath analysis—focus on volatile organic compounds. Clin Chim Acta 347:25–39. https://doi.org/10.1016/j.cccn.2004.04.023
Miller TL, Wolin MJ (1979) Fermentations by saccharolytic intestinal bacteria. Am J Clin Nutr 32:164–172. https://doi.org/10.1093/ajcn/32.1.164
Miller CJ, Runge-Morris M, Cassidy-Bushrow AE et al (2020) A review of volatile organic compound contamination in post-industrial urban centers: reproductive health implications using a Detroit lens. Int J Environ Res Public Health 17:8755. https://doi.org/10.3390/ijerph17238755
Nakaoka H, Hisada A, Matsuzawa D et al (2021) Associations between prenatal exposure to volatile organic compounds and neurodevelopment in 12-month-old children: the Japan Environment and Children’s Study (JECS). Sci Total Environ 794:148643. https://doi.org/10.1016/j.scitotenv.2021.148643
Nakhjirgan P, Kashani H, Naddafi K et al (2019) Maternal exposure to air pollutants and birth weight in Tehran. Iran J Environ Health Sci Eng 17:711–717. https://doi.org/10.1007/s40201-019-00386-7
Neubert D (2001) Multicenter field trial on possible health effects of toluene. II. Cross-sectional evaluation of acute low-level exposure. Toxicology 168:159–183. https://doi.org/10.1016/S0300-483X(01)00407-3
Phillips M, Cataneo RN, Condos R et al (2007) Volatile biomarkers of pulmonary tuberculosis in the breath. Tuberculosis 87:44–52. https://doi.org/10.1016/j.tube.2006.03.004
Ronde E, Frerichs NM, Brantenaar S et al (2022) Detection of spontaneous preterm birth by maternal urinary volatile organic compound analysis: a prospective cohort study. Front Pediatr 10:1063248. https://doi.org/10.3389/fped.2022.1063248
Scislowski PWD, Pickard K (1994) The regulation of transaminative flux of methionine in rat liver mitochondria. Arch Biochem Biophys 314:412–416. https://doi.org/10.1006/abbi.1994.1461
Shin YK, Collea JV, Kim YD, Kim SY (1997) Breath pentane concentrations during labor and the effect of epidural analgesia on the pentane concentration. Int J Obstet Anesth 6:82–86. https://doi.org/10.1016/S0959-289X(97)80002-7
Smith ICP, Blandford DE (1995) Nuclear magnetic resonance spectroscopy. Anal Chem 67:509–518. https://doi.org/10.1021/ac00108a037
Sourial N, Wolfson C, Zhu B et al (2010) Correspondence analysis is a useful tool to uncover the relationships among categorical variables. J Clin Epidemiol 63:638–646. https://doi.org/10.1016/j.jclinepi.2009.08.008
Takahashi S, Tsuji K, Fujii K et al (2007) Prospective study of clinical symptoms and skin test reactions in medical students exposed to formaldehyde gas: formaldehyde-induced symptoms and patch test results. J Dermatol 34:283–289. https://doi.org/10.1111/j.1346-8138.2007.00274.x
Weinstein JR, Diaz-Artiga A, Benowitz N, Thompson LM (2020) Reductions in urinary metabolites of exposure to household air pollution in pregnant, rural Guatemalan women provided liquefied petroleum gas stoves. J Expo Sci Environ Epidemiol 30:362–373. https://doi.org/10.1038/s41370-019-0163-0
Williams AD, Grantz KL, Zhang C et al (2019) Ambient volatile organic compounds and racial/ethnic disparities in gestational diabetes mellitus: Are Asian/Pacific Islander women at greater risk? Am J Epidemiol 188:389–397. https://doi.org/10.1093/aje/kwy256
Yin SN, Hayes RB, Linet MS et al (1996) An expanded cohort study of cancer among benzene-exposed workers in China. Benzene study group. Environ Health Perspect 104:1339–1341. https://doi.org/10.1289/ehp.961041339
Yusoff NA, Abd Hamid Z, Budin SB, Taib IS (2023) Linking benzene, in utero carcinogenicity and fetal hematopoietic stem cell niches: a mechanistic review. Int J Mol Sci 24:6335. https://doi.org/10.3390/ijms24076335
Zhou X, Zhou X, Wang C, Zhou H (2023) Environmental and human health impacts of volatile organic compounds: a perspective review. Chemosphere 313:137489. https://doi.org/10.1016/j.chemosphere.2022.137489
Acknowledgements
The authors thank Dr Moreau Stephane for his advice on chemical classification.
Funding
This study was supported by the French government’s IDEX-ISITE initiative 16-IDEX-0001 (CAP20-25).
Author information
Authors and Affiliations
Contributions
Conceptualization: RM-Q, LB, and VS; Methodology: RM-Q, NG-M, and DG; Software and formal analysis: BP, CL, and RM-Q; Investigation: DG; Resources: VS; Writing—original draft preparation: RM-Q; Writing—review & editing: RM-Q, DB, MB, and VS; Project administration and funding acquisition: VS. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no financial and non-financial conflicts of interest.
Ethical Approval
The study was conducted according to the guidelines of the Declaration of Helsinki and authorized by the Ethics Committee CPP Sud-Est VI, with CPP reference no. AU 765 and CODECOH no. DC-2008-558.
Consent to Participate and to Publish
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Minet-Quinard, R., Goncalves-Mendes, N., Gallot, D. et al. Volatile Organic Compounds Detected in Amniotic Fluid of Women During Normal Pregnancy. Expo Health (2023). https://doi.org/10.1007/s12403-023-00617-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12403-023-00617-1