Abstract
Our previous studies have linked gestational methylmercury exposure, originating from seafood, to changes in maternal thyroid hormones and infant birth size in a Swedish birth cohort. Herein we aimed to determine associations between maternal thyroid hormones and infant birth size and elucidate if maternal hormones could mediate the relationship between methylmercury and lower birth size. In 515 women, without known thyroid disease, we assessed metal exposure by erythrocyte mercury concentrations (mainly methylmercury, reflecting exposure over the past months) in early third trimester measured with inductively coupled plasma-mass spectrometry. Plasma concentrations of total and free thyroxine (tT4 and fT4) and triiodothyronine (tT3 and fT3), and thyroid-stimulating hormone (TSH) were measured at an accredited clinical laboratory. In multivariable-adjusted linear regression models, maternal tT3 (per 1 nmol/L increase) was positively associated with birth weight (B: 125 g; 95% CI 36, 214) and length (B: 0.59 cm; 95% CI 0.21, 0.97). Maternal fT4 was inversely associated with birth weight (B: − 33 g; 95% CI − 57, − 9.5), driven by obese women (n = 76). Causal mediation analyses suggested that a doubling of erythrocyte mercury (> 1 µg/kg; n = 374) was associated with a mean tT3-mediated decrease in birth weight of 11 g (95% CI − 25, − 1.6) and in birth length of 0.1 cm (95% CI − 0.12, − 0.01), both equivalent to about 12% of the total effect. To conclude, tT3 was positively associated with infant birth size. Reduced tT3 levels appeared to mediate a minor part of the inverse association between methylmercury exposure and birth size.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Methylmercury (MeHg) is an organic and highly toxic form of mercury. Exposure occurs via consumption of fish and other seafood (EFSA 2012). Observational studies have found a link between dietary exposure to MeHg during pregnancy and lower birth weight (Dack et al. 2021; Gustin et al. 2020; Karagas et al. 2012), a predictor of both perinatal and later-life morbidity (Gluckman et al. 2008; Katz et al. 2013). Several modes of action have been suggested to underly the metal-related associations with birth weight, including induction of oxidative stress (Fujimura and Usuki 2020), which has been associated with intra-uterine growth restriction (Kamath et al. 2006). Also, experimental studies suggest that MeHg may have endocrine disruptive properties and may interfere with the hypothalamic-pituitary-thyroid axis (Iavicoli et al. 2009), a hormonal system that is essential for fetal growth. Indeed, we have previously found inverse associations between MeHg exposure and plasma triiodothyronine (T3; the active form of thyroid hormone) concentrations in pregnancy in the mother–child cohort NICE (Nutritional impact on the Immunological Maturation during Childhood in relation to the Environment) in northern Sweden (Gustin et al. 2021).
The main product of the thyroid gland is the prohormone thyroxine (T4), produced under the influence of thyroid-stimulating hormone (TSH). In peripheral tissue, most of the T3 is produced by conversion of T4 (about 80%; Robbins 1981). Circulating thyroid hormone levels are regulated via negative feedback mechanisms, where increasing levels of T4 and T3 signal back to reduce the secretion of TSH, in turn leading to reduced hormone production in the thyroid (Ortiga-Carvalho et al. 2016). Both T3 and T4 play important roles in placental (Barber et al. 2005; Kilby et al. 2005) and fetal development (Mullur et al. 2014). The fetus is entirely dependent on the mother’s thyroid hormone production until mid-pregnancy, when the fetus’ own thyroid hormone production starts (Obregon et al. 2007), yet maternal transfer of T4 to the fetus continues throughout gestation (Obregon et al. 2007). Both low and elevated maternal thyroid hormones levels have been associated with impaired fetal development (Korevaar et al. 2016). In pregnant women with no apparent thyroid disease, especially elevated free T4 (fT4) levels have been associated with lower birth weight (Johns et al. 2018; Leon et al. 2015; Medici et al. 2013; Zhang et al. 2019; Zhou et al. 2020).
In the present study, we aimed to assess the potential mediation of maternal thyroid hormones in the previously observed relationship of gestational exposure to MeHg with infant size at birth in the NICE cohort (Gustin et al. 2020). To that end, we first evaluated the impact of maternal thyroid hormone and TSH levels in pregnancy with infant weight and length at birth.
Methods
Study Population
The women and children included in this study are part of the ongoing birth-cohort NICE in northern Sweden. As described in more detail elsewhere (Barman et al. 2018), the primary aim of the NICE cohort is to elucidate how the early-life environment influences allergy development and immune maturation during the first years of life. Secondary outcomes are infant and child anthropometry, growth, dental health, and neurological development. The cohort was established 2015–2018 in the catchment area of Sunderby Hospital in Norrbotten county, in northern Sweden. Expecting parents were given an information leaflet about NICE at their visit to the local maternity clinics in early pregnancy. To be included in the study, the parents had to be residents in the southern or eastern part of Norrbotten county, planning to give birth at Sunderby Hospital, and be able to communicate in written and spoken Swedish. At the routine ultrasound in gestational weeks 18–19, parents wishing to participate were given additional information and an informed consent to sign at home and send back.
A total of 655 pregnancies were registered in the NICE cohort (Englund-Ögge et al. 2022). For the present study, we identified 629 mothers who had singleton live births (Fig. 1). Of these mothers, we excluded those with any notation of thyroid dysfunction in their pregnancy hospital records (n = 43) and one woman with a TSH concentration above 20 mIU/L (Gustin et al. 2021). We also excluded women with missing plasma samples for hormone analyses (n = 5), missing erythrocyte samples for metal analyses (n = 38), and women of infants with missing birth anthropometry data (n = 22). Lastly, women with missing information on education (n = 4) and pre-pregnancy smoking (n = 1) were also excluded, leaving 515 mother–child dyads to be included in the main analyses.
The study was performed in accordance with the Helsinki declaration and approved by the Regional Ethical Review Board, Umeå, Sweden. At enrollment, the mothers provided a written consent about their own participation and at delivery they gave an additional written consent regarding the participation of their child. All participants were informed that they could withdraw from the study at any time point without explanation.
Sample Collection
As previously described (Gustin et al. 2021), venous blood samples were collected from the women at the local maternity health clinics in the early third trimester (mean gestational week: 29; min–max: 24–36). Blood was collected in 6 mL trace element-free Na-heparin tubes (Greiner bio-one, Kremsmünster, Austria) for metal analyses, and in 10 mL EDTA tubes (Becton Dickinson, Plymouth, U.K.) for hormone analyses. The samples were stored at 4℃ until they were transported cold to the hospital laboratory, at latest the following workday. At the hospital laboratory, the blood tubes were centrifuged at 2400 rpm for 5 min (Hettich Rotina 420, Hettich Lab Technology, Tuttlingen, Germany) for separation of the erythrocyte and plasma fractions. The plasma fraction was transferred into 1.4 mL polypropylene tubes (Micronic, Nordic Biolabs AB, Sweden). All samples were kept at − 20 or – 80 °C until transported frozen to Karolinska Institutet, Sweden, for trace element analyses, or to the Department of Clinical Chemistry at the University Hospital of Malmö, Sweden, for hormone analyses.
Mercury Analysis
Assessment of maternal methylmercury exposure has been described previously in more detail (Gustin et al. 2021). In short, total mercury was measured in maternal blood (erythrocyte fraction), which is considered to reflect the exposure over the past few months, related to the lifespan of erythrocytes (Shemin and Rittenberg 1946; Zhang et al. 2018). Total mercury in erythrocytes reflects the women’s exposure mainly to MeHg since it, unlike inorganic mercury, accumulates in the erythrocyte fraction (Berglund et al. 2005).
The concentration of mercury in erythrocytes was measured with inductively coupled plasma-mass spectrometry (ICP-MS; Agilent 7700x, Agilent Technologies, Tokyo, Japan), as described in detail previously (Gustin et al. 2020; Lu et al. 2015). The limit of detection (LOD; defined as three times the standard deviation of the blank concentrations) was 0.010 µg/kg, and only two samples had a mercury concentration below the LOD and were replaced by LOD/√2. For quality control of the ICP-MS analyses, two commercial whole blood reference materials were included in each run, and there was good agreement between obtained values and recommended reference values (Gustin et al. 2020, 2021).
Hormone Analyses
Maternal plasma hormone concentrations were measured in an accredited laboratory at the Department of Clinical Chemistry, University Hospital of Malmö, Sweden, as previously described (Gustin et al. 2021). In brief, free and total T4 (fT4, tT4) and free and total T3 (fT3, tT3) were measured with automated electrochemiluminescence immunoassays (ECLIA) by Roche Cobas (Roche Diagnostics, Solna, Sweden), comprising a two-step immunometric-competitive technique followed by chemiluminescent emission measurement. Plasma concentrations of TSH were measured using a one-step sandwich method with ECLIA by Roche Cobas (Roche Diagnostics, Solna, Sweden).
Birth Anthropometry and Covariates
Data on the infants’ birth weight (g) and birth length (cm) were collected from the hospital records, as was information on gestational age at birth (days) and the infants’ sex. Data regarding early-pregnancy body mass index [BMI (kg/m2), based on body weight (kg) and height (cm) measured at registration to the maternity clinic in the first trimester], maternal age (years), maternal education (elementary school, high school, or university), parity (number of previous births), maternal pre-pregnancy alcohol consumption (never, sometimes, or daily), and pre-pregnancy smoking (never, sometimes, or daily) was also collected from the hospital records. Since the thyroid hormone and TSH levels may be influenced by season (Mahwi and Abdulateef 2019; Wang et al. 2018), the collection dates for maternal blood samples were classified into four seasons (spring: March–May; summer: June–August; fall: September–November; winter: December–February). Information on maternal seafood (i.e., fish and shellfish) consumption in pregnancy was obtained from semi-quantitative food frequency questionnaires, administered around gestational week 34 with questions concerning the intake over the past month, as described in detail elsewhere (Gustin et al. 2020; Stråvik et al. 2019). In short, the total seafood intake in grams per day was estimated based on reported portion size and intake frequency.
Statistical Analyses
Statistical analyses were performed using the software Stata/IC 15.0 (StataCorp, TX, U.S.) and R 4.1.2 (R Core Team 2021). P-values below 0.05 were considered statistically significant for all tests. Prior to assessing the associations between maternal hormones (fT4, tT4, fT3, tT3, TSH, and the fT3:fT4 ratio) and the children’s size at birth (birth weight and birth length), covariates were identified by exploring their associations with both the maternal hormone concentrations and the birth outcomes. Spearman rank correlation was used for continuous variables and Kruskal–Wallis or Mann–Whitney U test for categorical variables. Variables that were associated with at least one of the hormones and at least one of the birth size measurements (i.e., parity and maternal education) were considered as covariates and included in a directed acyclic graph (DAG) to identify potential confounders of the hormone-birth size associations (Supplementary Fig S1). Although gestational age at birth and infant sex were not significantly associated with the maternal hormones, they were still included in the DAG, and in the final models, since they were strongly correlated with the outcomes. Since there was a tendency of lower birth weight among the few pre-pregnancy smokers (mean smokers: 3531 g; mean non-smokers: 3631 g), and maternal smoking previously has been associated with both low birth weight (Pereira et al. 2017) and maternal thyroid function (Shields et al. 2009), smoking was also included in the DAG. The minimal adjustment suggested in the DAG included parity, maternal education, and smoking. Therefore, the final models were adjusted for these variables, as well as gestational age at birth and infants’ sex. Maternal BMI was not included in the DAG as the relationship between thyroid function and BMI is complex and likely involves multiple levels of interaction (Garcia-Solis et al. 2018; Korevaar et al. 2017), making it difficult to determine the direction of the BMI-hormone associations. However, previous studies have shown that obesity may influence thyroid hormone homeostasis, possibly through adaptive processes to increase energy expenditure or altered deiodinase activity (Fontenelle et al. 2016), making obesity a potential confounder. Therefore, we also conducted analyses stratifying by obesity (defined as early-pregnancy BMI ≥ 30 kg/m2). Maternal age was correlated with fT4 (rho: − 0.09; p = 0.034) and season of sampling was associated with tT3 (p = 0.043), but neither was associated with the birth outcomes and therefore not included in the DAG or the final models. Pre-pregnancy alcohol consumption was neither associated with the hormones nor the birth size measurements and it was therefore also excluded from further analyses.
The distributions of the hormone concentrations were close to normal, according to histograms. Linearity of the hormone-birth size associations was explored with generalized additive models (GAMs), with two degrees of freedom and adjusted as described above. These analyses excluded non-linear associations in all of the hormone-birth size associations (p-gain > 0.05; Royston and Ambler 1998), and the associations were then explored in linear regression models, adjusted as described above.
The mediation analyses were performed using the mediation package in R software (Tingley et al. 2014). The model-based causal mediation is conducted in two steps. First, two models are specified: (i) a mediator model modeling the mediator against the exposure and appropriate covariates, and (ii) an outcome model modelling the outcome against the exposure, mediator, and covariates. In the second step, the two models are used to estimate the average causal mediation effect, the average direct effect, and the total effect. Erythrocyte mercury concentrations were skewed and therefore log2-transformed prior to the analyses. Since the associations of maternal erythrocyte mercury with tT3 and birth size outcomes differed below and above the mercury concentration of 1 µg/kg (Gustin et al. 2020, 2021), we let the effect of the exposure be different for positive and negative values of the exposure (since 1 µg/kg equals 0 when log-transformed) also in the underlying models in the mediation analyses (see details in the Supplementary extended method description). Uncertainty in the mediation effect estimates was assessed using a non-parametric bootstrap (boot = TRUE argument) with 1000 replications.
Covariates for the mediator and outcome models were selected as described for the regression analyses above (Supplementary Fig S1). The mediator [maternal tT3 (nmol/L)] was modelled with linear regression against the exposure [maternal erythrocyte mercury (µg/L; log2-transformed)] and covariates [parity (‘0’ and ‘ > 0’), maternal education (‘lower than university’ and ‘university’), maternal pre-pregnancy smoking (‘never’ and ‘sometimes or daily’)]. The outcomes [birth weight (g), or birth length (cm)] were then modelled with linear regression against the exposure, mediator, and covariates [parity, education, pre-pregnancy, gestational length at birth (weeks), and infant’s sex].
MeHg exposure comes almost exclusively from consumption of seafood, including freshwater fish, and seafood also contain micro- and macronutrients (such as iodine, selenium, polyunsaturated fatty acids, and proteins) that may be beneficial for both thyroid function (Obregon et al. 2005) and fetal growth (Leventakou et al. 2014), as well as other environmental pollutants (such as polychlorinated biphenyls and dioxins) that can be harmful to fetal development (Lundqvist et al. 2006). Therefore, we performed sensitivity analyses additionally adjusting the outcome and mediator models for the mothers’ total seafood intake (g/day), which was positively correlated with maternal erythrocyte mercury (rho: 0.49; p < 0.001). Information on consumption of different types of fish and other seafood in pregnancy was available for 493 of the included women only, therefore the model estimates were compared to those of the same mothers without adjustment for seafood intake.
Results
The general characteristics of the 515 women and infants included in the present study are shown in Table 1, together with the corresponding information for the women excluded due to missing data, and the women excluded due to thyroid disease and/or medication with thyroid hormone-interfering drugs. Women excluded due to missing information regarding metal concentrations, hormone levels, birth anthropometry, and/or covariate data, had lower education and slightly lower fT3 than those included in the present analyses, and their children had a lower birth weight and a shorter length of gestation than those in the included group. The women excluded due to thyroid disease or medication with thyroid hormone-interfering drugs had significantly higher fT4 and tT4 levels, and lower fT3 and tT3 levels, and their children were slightly shorter at birth.
Hormone-Birth Size Associations
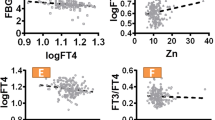
Bivariate associations of the maternal hormones with birth weight and birth length (assessed with Spearman rank correlation; Supplementary Table S1) showed a weak positive correlation between maternal tT3 and birth weight (rho: 0.09, p = 0.036), and an inverse correlation between fT4 and birth weight (rho: − 0.11, p = 0.012). The fT3:fT4 ratio was positively correlated with both birth weight (rho: 0.10, p = 0.020) and birth length (rho: 0.10, p = 0.018). In the multivariable-adjusted linear regression models (Table 2), a 1 pmol/L increase in maternal fT4 was associated with a mean decrease in birth weight of 33 g (95% CI − 57, − 9.5). In contrast, a 1 nmol/L increase in maternal tT3 was associated with a mean increase in birth weight of 125 g (95% CI 36, 214) and in birth length of 0.59 cm (95% CI 0.21, 0.97). Also, a 0.1 increase in the fT3:fT4 ratio was associated with an increase in birth weight of 91 g (95% CI 22, 161) and in birth length of 0.29 cm (95% CI − 0.004, 0.059).
Compared to the leaner women, obese women (BMI ≥ 30 kg/m2; n = 76) had lower fT4 (median: 11.9 and 12.4 pmol/L, for women with BMI above and below 30, respectively; p = 0.031), higher fT3 (4.3 versus 4.0 pmol/L; p < 0.001) and tT3 (2.8 versus 2.5 nmol/L; p < 0.001), and a higher fT3:fT4 ratio (0.36 versus 0.32 pmol/L; p < 0.001). The children of the obese women also differed slightly in birth length from those of leaner women (51 versus 50 cm, for women with BMI ≥ 30 and < 30 km/m2, respectively; p = 0.018). In the stratified analyses, the positive associations of maternal tT3 with birth weight and length persisted in the women with BMI < 30 kg/m2 (Supplementary Table S2), while the inverse association of maternal fT4 with birth weight was diminished and no longer statistically significant. The positive association of the fT3:fT4 ratio with birth weight was also sharply reduced and became statistically non-significant. In women with a BMI ≥ 30 kg/m2, only the inverse association between fT4 and birth weight remained (Supplementary Table S2).
Mediation Analyses
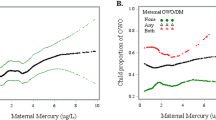
We have previously shown that maternal erythrocyte mercury (log2-transformed) was non-linearly associated with birth size (Gustin et al. 2020) and non-linearly associated with maternal fT3, tT3, and the fT3:fT4 ratio in early third trimester (Gustin et al. 2021). Above the erythrocyte mercury concentration of 1 µg/kg, inverse associations were observed with both birth weight and length, as well as with fT3, tT3, and the fT3:fT4 ratio. Since erythrocyte mercury was not associated with fT4, and fT3 was not significantly associated with birth anthropometry, and the association of the fT3:fT4 ratio with birth weight did not persist after excluding obese women, only tT3 was further explored as a potential mediator in the associations of erythrocyte mercury with both birth weight and length.
In the analyses exploring tT3 as mediator (Table 3), a doubling of erythrocyte mercury concentrations above 1 µg/kg (which 73% of the included women had) was associated with a mean tT3-mediated decrease in birth weight of 11 g (95% CI − 25, − 1.6), corresponding to 12% of the total effect of maternal erythrocyte mercury on birth weight. Similarly, a doubling in erythrocyte mercury (> 1 µg/kg) was associated with a mean tT3-mediated decrease in birth length of 0.05 cm (− 0.12, − 0.01), equivalent to 12% of the total effect.
In sensitivity analyses, we explored the mediation of tT3 in the relationship of maternal erythrocyte mercury with size at birth after additionally adjusting the outcome and mediator models for the mothers’ total seafood intake in pregnancy and compared the estimates to those of the same mothers without adjustment for total seafood intake. The results are shown in Table 4 for erythrocyte mercury concentrations > 1 µg/kg (n = 361). The average causal mediation effect estimates for birth weight and birth length were largely unaffected when adjusted for maternal total seafood intake (− 9.5 g and − 0.05 cm for birth weight and length, respectively) compared to the estimates in models with the same women without adjustment for total seafood intake (− 9.7 g and − 0.05 cm for birth weight and length, respectively). The direct effects of erythrocyte mercury became more pronounced (from − 105 to − 124 g for birth weight and from − 0.48 to 0.56 cm for birth length) after the adjustment for maternal seafood intake, and the total effects became similarly larger. Therefore, the proportion of the mediated effect was slightly reduced for birth weight (7.6% vs. 9.3% when adjusting and not adjusting for seafood intake, respectively) and birth length (8.4% vs. 10% when adjusting and not adjusting for seafood intake, respectively).
Discussion
In this study of pregnant women in the north of Sweden, the third trimester plasma concentrations of tT3 were positively associated with birth weight and length, while the fT4 concentrations were inversely associated with birth weight. The subsequent mediation analysis suggested that 12% of the total effect of maternal erythrocyte mercury concentrations, reflecting MeHg exposure, on birth weight and length was mediated via reduced maternal tT3 levels.
The women included in the present study did not have any known thyroid disease or thyroid-related medication, and essentially all (98%) had TSH concentrations below 4.0 mIU/L, an upper reference limit that may be used when population- and trimester-specific reference ranges are unavailable (Alexander et al. 2017). Still, we found that the rather narrow range of maternal plasma tT3 in early third trimester (5th–95th percentiles: 1.9–3.4 nmol/L) was positively associated with both birth weight and length. There are few previous studies on maternal T3 and birth anthropometry, and measurement of T3 is less common than those of T4 in thyroid monitoring studies. One of the few available observational studies, based on a large Chinese birth cohort (n = 9975), reported positive associations of maternal tT3 in both first and third trimester with birth weight (Zhang et al. 2019). Similarly, in a smaller study in the U.S. (n = 439), early third trimester maternal tT3 levels were positively associated with birth weight z scores (Johns et al. 2018). Neither of these two studies explored associations with birth length. In vitro studies of human trophoblast cells have shown that T3 increases the production of epidermal growth factor which regulates the differentiation and proliferation of trophoblasts (Barber et al. 2005; Kilby et al. 2005), suggesting that T3 may indirectly promote fetal growth through enhanced placental growth and function.
We have previously reported that gestational MeHg exposure, measured by mercury concentrations in erythrocytes, was inversely associated with both fT3 and tT3 in early third trimester in the present cohort (Gustin et al. 2021), as well as with birth weight and length (Gustin et al. 2020). The inverse associations of erythrocyte mercury with birth anthropometry and maternal T3 were consistently observed above erythrocyte mercury concentrations of 1 µg/kg (highest concentration being 11 µg/kg), which would roughly correspond to 0.4–4.3 µg/L in whole blood (Gustin et al. 2020). Similar MeHg exposure levels are observed in most European populations (EFSA 2012), while much higher gestational exposure levels have been reported for island populations, such as Japan (Kobayashi et al. 2019), the Faroese Islands (Needham et al. 2011), and the Seychelles (Xu et al. 2019). In the present study, mediation analyses estimated that around 12% of the total effect of maternal methylmercury exposure (at erythrocyte mercury concentrations above 1 µg/kg) on both birth weight and length were mediated via reduced tT3 levels. Thus, our findings indicate that impairment of maternal tT3 levels may be one of the modes of action by which MeHg exposure impairs fetal growth, although not the major one, which possibly could be through oxidative stress (Fujimura and Usuki 2020).
In sensitivity analyses, we explored the influence of additionally adjusting the mediation models for the women’s total seafood intake (g/day), mostly consisting of marine fish (Gustin et al. 2020; Stråvik et al. 2019). Seafood, the main source of MeHg exposure, may contribute to unmeasured confounding as seafood is also an important source of micronutrients, like iodine and selenium which are essential for thyroid function (Köhrle 2005; Zimmermann 2009), as well as polyunsaturated fatty acids (Strain et al. 2020), which previously have been shown to mask the adverse effects of MeHg exposure in relation to other outcomes (Strain et al. 2008). In the present analyses, however, the small changes observed in the mediated effects when additionally adjusting for maternal seafood intake did not indicate confounding by other pollutants in the consumed fish for the effects mediated via tT3. However, the direct effects of MeHg on birth weight and length became slightly more pronounced (inverse) after adjustment for seafood intake, in line with a positive influence of maternal fish intake on the infants’ birth size (Rogers et al. 2004).
We also found an inverse association of maternal fT4 in the early third trimester with birth weight, but not with MeHg exposure (Gustin et al. 2021). Associations of maternal fT4 with smaller fetal growth estimates, such as birth size, have previously been reported in large Chinese (Zhang et al. 2019; Zhou et al. 2020), Dutch (Medici et al. 2013; Vrijkotte et al. 2017), and Spanish (Leon et al. 2015) cohorts, as well as in smaller studies from the U.S. (Johns et al. 2018; Kahr et al. 2016), U.K. (Shields et al. 2011) and China (Sun et al. 2019), despite the fact that the thyroid hormones were assessed at varying time points during pregnancy. Both T4 and TSH vary markedly in the first half of pregnancy (Korevaar et al. 2017), while T3 levels remain stable across the whole pregnancy (Patel et al. 2011). In the present analyses, the inverse association between fT4 and birth weight was only observed in women with an early-pregnancy BMI of 30 kg/m2 or higher, but not among leaner women. Similarly, the positive association observed between the fT3:fT4 ratio and birth weight markedly decreased when excluding obese mothers. The fT3:fT4 ratio is a potential marker of deiodinase type I activity (Panicker et al. 2008), the enzyme responsible for converting T4 into the active T3 and providing T3 for circulation (Larsen and Zavacki 2012). Thus, the inverse association of fT4 with birth weight may be, at least partly, driven by increased deiodinase type I activity, related to obesity (Ortega et al. 2012). Indeed, Kahr et al. (2016) reported reduced maternal fT4 levels in mothers with a BMI over 35 kg/m2 and an increased fT3:fT4 ratio in women with a BMI above 25 kg/m2. Also, a recent large observational study of pregnant women in Denmark found that maternal adiposity was positively associated with the T3:T4 ratio in early pregnancy (Andersen et al. 2021).
The main strengths of this study include the individual assessments of MeHg exposure using a highly sensitive ICP-MS method. We measured mercury in erythrocytes, which reflects the gestational MeHg exposure in the studied women, but since we did not speciate mercury in erythrocytes, we cannot completely rule out a potential minor influence of inorganic mercury, which is more evenly distributed between plasma and erythrocytes (Berglund et al. 2005). However, as previously discussed, the exposure to inorganic mercury in young Swedish women is most likely very low (Gustin et al. 2021). A limitation in the mediation analyses is that the exposure (erythrocyte mercury) and the mediator (plasma tT3) were measured in samples collected at the same timepoint. To facilitate causal inference, the exposure should be measured prior to the mediator. However, since erythrocyte mercury reflects the exposure over the past 3–4 months (as discussed in Section "Mercury analysis") and T3 in plasma has a half-life of less than two days (Gharib 1974), the measured exposure can still be considered to have occurred prior to changes in the mediator. Another limitation is that approximately only 10% of all women giving birth at Sunderby hospital during the recruitment period participated in the study (Englund-Ögge et al. 2022). However, although self-selection bias has been shown for some lifestyle factors in the NICE cohort, it does not seem to skew pregnancy outcomes, or influence the impact of certain well-known lifestyle parameters on pregnancy outcomes (Englund-Ögge et al. 2022). Further, the mercury concentrations among the included women were similar to those previously reported among pregnant women in central Sweden (Vahter et al. 2000). Another limitation is that free thyroid hormone concentrations were measured in plasma by immunoassays which may be sensitive to the pregnancy-related increase in thyroxine binding globulin, yet, calculating the fT4 or fT3 index (Villanger et al. 2017) was not feasible. Also, we did not obtain any measurements of autoimmune thyroid disease, such as thyroid peroxidase antibody (TPOAb) tests. However, the implications of TPOAb positivity for birth weight are unclear (Medici et al. 2013). Still, women with a notation regarding TPOAb positivity in their hospital records were excluded from the present analyses. Regarding the sensitivity analyses, where we further adjusted the mediation models for the women’s seafood consumption, it should be noted that the semi-quantitative questionnaire data on total seafood intake during the past month is a somewhat crude estimate of the women’s true intake. It is possible that the women’s erythrocyte mercury concentrations better reflect their actual total seafood intake, why residual confounding from fish intake may still be present in the analyses, resulting in an underestimation of the effects of methylmercury exposure (Budtz-Jorgensen et al. 2021). Lastly, we assumed no other unmeasured confounding in the mediation analyses. Nevertheless, this is an observational study and unmeasured confounding cannot be entirely ruled out.
Conclusion
Our study indicates that maternal tT3 in pregnancy is positively associated with birth weight and birth length and that this may, to a limited extent, mediate the adverse effect of maternal MeHg exposure on infant size at birth. Further studies in other populations of pregnant women are warranted to confirm these findings, and to identify other modes of action of MeHg. The present exposure levels were quite low, and similar or higher exposure is likely experienced by millions of mothers around the world.
Data Availability
Data and Material are available from the corresponding author on reasonable request.
Abbreviations
- ACME:
-
Average causal mediation effect
- ADE:
-
Average direct effect
- BMI:
-
Body mass index
- DAG:
-
Directed acyclic graph
- ECLIA:
-
Electrochemiluminescence immunoassay
- fT3:
-
Free triiodothyronine
- fT4:
-
Free thyroxine
- GAM:
-
Generalized additive model
- ICP-MS:
-
Inductively coupled plasma-mass spectrometry
- IQR:
-
Interquartile range
- LOD:
-
Limit of detection
- NICE:
-
Nutritional impact on the immunological maturation during childhood in relation to the environment
- MeHg:
-
Methylmecury
- TPOAb:
-
Thyroid peroxidase antibody
- TSH:
-
Thyroid-stimulating hormone
- tT3:
-
Total triiodothyronine
- tT4:
-
Total thyroxin
References
Alexander EK, Pearce EN, Brent GA, Brown RS, Chen H, Dosiou C et al (2017) 2017 guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid 27:315–389. https://doi.org/10.1089/thy.2016.0457
Andersen SL, Knosgaard L, Handberg A, Vestergaard P, Andersen S (2021) Maternal adiposity, smoking, and thyroid function in early pregnancy. Endocr Connect 10:1125–1133. https://doi.org/10.1530/EC-21-0376
Barber KJ, Franklyn JA, McCabe CJ, Khanim FL, Bulmer JN, Whitley GS et al (2005) The in vitro effects of triiodothyronine on epidermal growth factor-induced trophoblast function. J Clin Endocrinol Metab 90:1655–1661. https://doi.org/10.1210/jc.2004-0785
Barman M, Murray F, Bernardi AI, Broberg K, Bolte S, Hesselmar B, et al (2018) Nutritional impact on immunological maturation during childhood in relation to the environment (NICE): a prospective birth cohort in northern Sweden. BMJ Open 8:e022013. https://doi.org/10.1136/bmjopen-2018-022013
Berglund M, Lind B, Bjornberg KA, Palm B, Einarsson O, Vahter M (2005) Inter-individual variations of human mercury exposure biomarkers: a cross-sectional assessment. Environ Health 4:20. https://doi.org/10.1186/1476-069X-4-20
Budtz-Jorgensen E, Grandjean P, Weihe P (2021) Separation of risks and benefits of seafood intake. Environ Health Perspect 115:323–327
Dack K, Fell M, Taylor CM, Havdahl A, Lewis SJ (2021) Mercury and prenatal growth: a systematic review. Int J Environ Res Public Health 18:7140. https://doi.org/10.3390/ijerph18137140
EFSA (2012) Scientific opinion on the risk for public health related to the presence of mercury and methylmercury in food. EFSA panel on contaminants in the food chain (CONTAM). EFSA J. 2012 10:2985.
Englund-Ögge L, Murray F, Modzelewska D, Lundqvist R, Nilsson S, Carre H, et al (2022) Maternal characteristics and pregnancy outcomes in the NICE birth cohort: an assessment of self-selection bias. J Matern Fetal Neonatal Med 1–9. https://doi.org/10.1080/14767058.2021.2011854
Fontenelle LC, Feitosa MM, Severo JS, Freitas TE, Morais JB, Torres-Leal FL et al (2016) Thyroid function in human obesity: underlying mechanisms. Horm Metab Res 48:787–794. https://doi.org/10.1055/s-0042-121421
Fujimura M, Usuki F (2020) Methylmercury-mediated oxidative stress and activation of the cellular protective system. Antioxidants (basel) 9:1004. https://doi.org/10.3390/antiox9101004
Garcia-Solis P, Garcia OP, Hernandez-Puga G, Sanchez-Tusie AA, Saenz-Luna CE, Hernandez-Montiel HL et al (2018) Thyroid hormones and obesity: a known but poorly understood relationship. Endokrynol Pol 69:292–303. https://doi.org/10.5603/EP.2018.0032
Gharib H (1974) Triiodothyronine: physiological and clinical significance. JAMA 227:302–304. https://doi.org/10.1001/jama.1974.03230160030007
Gluckman PD, Hanson MA, Cooper C, Thornburg KL (2008) Effect of in utero and early-life conditions on adult health and disease. New Engl J Med 359:61–73. https://doi.org/10.1056/NEJMra0708473
Gustin K, Barman M, Stråvik M, Levi M, Englund-Ögge L, Murray F et al (2020) Low-level maternal exposure to cadmium, lead, and mercury and birth outcomes in a Swedish prospective birth-cohort. Environ Pollut 265:114986. https://doi.org/10.1016/j.envpol.2020.114986
Gustin K, Barman M, Skroder H, Jacobsson B, Sandin A, Sandberg AS et al (2021) Thyroid hormones in relation to toxic metal exposure in pregnancy, and potential interactions with iodine and selenium. Environ Int 157:106869. https://doi.org/10.1016/j.envint.2021.106869
Iavicoli I, Fontana L, Bergamaschi A (2009) The effects of metals as endocrine disruptors. J Toxicol Env Health-Pt b-Crit Rev 12:206–223. https://doi.org/10.1080/10937400902902062
Johns LE, Ferguson KK, Cantonwine DE, Mukherjee B, Meeker JD, McElrath TF (2018) Subclinical changes in maternal thyroid function parameters in pregnancy and fetal growth. J Clin Endocr Metab 103:1349–1358. https://doi.org/10.1210/jc.2017-01698
Kahr MK, Antony KM, DelBeccaro M, Hu M, Aagaard KM, Suter MA (2016) Increasing maternal obesity is associated with alterations in both maternal and neonatal thyroid hormone levels. Clin Endocrinol (oxf) 84:551–557. https://doi.org/10.1111/cen.12974
Kamath U, Rao G, Kamath SU, Rai L (2006) Maternal and fetal indicators of oxidative stress during intrauterine growth retardation (IUGR). Indian J Clin Biochem 21:111–115. https://doi.org/10.1007/BF02913077
Karagas MR, Choi AL, Oken E, Horvat M, Schoeny R, Kamai E et al (2012) Evidence on the human health effects of low-level methylmercury exposure. Environ Health Persp 120:799–806. https://doi.org/10.1289/ehp.1104494
Katz J, Lee AC, Kozuki N, Lawn JE, Cousens S, Blencowe H et al (2013) Mortality risk in preterm and small-for-gestational-age infants in low-income and middle-income countries: a pooled country analysis. Lancet 382:417–425. https://doi.org/10.1016/S0140-6736(13)60993-9
Kilby MD, Barber K, Hobbs E, Franklyn JA (2005) Thyroid hormone action in the placenta. Placenta 26:105–113. https://doi.org/10.1016/j.placenta.2004.08.004
Kobayashi S, Kishi R, Saijo Y, Ito Y, Oba K, Araki A et al (2019) Association of blood mercury levels during pregnancy with infant birth size by blood selenium levels in the Japan Environment and Children’s Study: a prospective birth cohort. Environ Int 125:418–429. https://doi.org/10.1016/j.envint.2019.01.051
Köhrle J (2005) Selenium and the control of thyroid hormone metabolism. Thyroid 15:841–853. https://doi.org/10.1089/thy.2005.15.841
Korevaar TI, Muetzel R, Medici M, Chaker L, Jaddoe VW, de Rijke YB et al (2016) Association of maternal thyroid function during early pregnancy with offspring IQ and brain morphology in childhood: a population-based prospective cohort study. Lancet Diabetes Endocrinol 4:35–43. https://doi.org/10.1016/S2213-8587(15)00327-7
Korevaar TIM, Medici M, Visser TJ, Peeters RP (2017) Thyroid disease in pregnancy: new insights in diagnosis and clinical management. Nat Rev Endocrinol 13:610–622. https://doi.org/10.1038/nrendo.2017.93
Larsen PR, Zavacki AM (2012) The role of the iodothyronine deiodinases in the physiology and pathophysiology of thyroid hormone action. Eur Thyroid J 1:232–242. https://doi.org/10.1159/000343922
Leon G, Murcia M, Rebagliato M, Alvarez-Pedrerol M, Castilla AM, Basterrechea M et al (2015) Maternal thyroid dysfunction during gestation, preterm delivery, and birthweight. The Infancia y Medio Ambiente Cohort. Spain Paediatr Perinat Ep 29:113–122. https://doi.org/10.1111/ppe.12172
Leventakou V, Roumeliotaki T, Martinez D, Barros H, Brantsaeter AL, Casas M et al (2014) Fish intake during pregnancy, fetal growth, and gestational length in 19 European birth cohort studies. Am J Clin Nutr 99:506–516. https://doi.org/10.3945/ajcn.113.067421
Lu Y, Kippler M, Harari F, Grander M, Palm B, Nordqvist H et al (2015) Alkali dilution of blood samples for high throughput ICP-MS analysis-comparison with acid digestion. Clin Biochem 48:140–147. https://doi.org/10.1016/j.clinbiochem.2014.12.003
Lundqvist C, Zuurbier M, Leijs M, Johansson C, Ceccatelli S, Saunders M et al (2006) The effects of PCBs and dioxins on child health. Acta Paediatr Suppl 95:55–64. https://doi.org/10.1080/08035320600886257
Mahwi TO, Abdulateef DS (2019) Relation of different components of climate with human pituitary-thyroid axis and ft3/ft4 ratio: a study on euthyroid and sch subjects in two different seasons. Int J Endocrinol 2019:2762978. https://doi.org/10.1155/2019/2762978
Medici M, Timmermans S, Visser W, Keizer-Schrama SMPFD, Jaddoe VWW, Hofman A et al (2013) Maternal thyroid hormone parameters during early pregnancy and birth weight: the Generation R study. J Clin Endocr Metab 98:59–66. https://doi.org/10.1210/jc.2012-2420
Mullur R, Liu YY, Brent GA (2014) Thyroid hormone regulation of metabolism. Physiol Rev 94:355–382. https://doi.org/10.1152/physrev.00030.2013
Needham LL, Grandjean P, Heinzow B, Jorgensen PJ, Nielsen F, Patterson DG Jr et al (2011) Partition of environmental chemicals between maternal and fetal blood and tissues. Environ Sci Technol 45:1121–1126. https://doi.org/10.1021/es1019614
Obregon MJ, Escobar del Rey F, Morreale de Escobar G (2005) The effects of iodine deficiency on thyroid hormone deiodination. Thyroid 15:917–929. https://doi.org/10.1089/thy.2005.15.917
Obregon MJ, Calvo RM, Escobar Del Rey F, Morreale de Escobar G (2007) Ontogenesis of thyroid function and interactions with maternal function. Endocr Dev 10:86–98. https://doi.org/10.1159/000106821
Ortega FJ, Jilkova ZM, Moreno-Navarrete JM, Pavelka S, Rodriguez-Hermosa JI, Kopeck Ygrave J et al (2012) Type I iodothyronine 5’-deiodinase mRNA and activity is increased in adipose tissue of obese subjects. Int J Obes (lond) 36:320–324. https://doi.org/10.1038/ijo.2011.101
Ortiga-Carvalho TM, Chiamolera MI, Pazos-Moura CC, Wondisford FE (2016) Hypothalamus-pituitary-thyroid axis. Compr Physiol 6:1387–1428. https://doi.org/10.1002/cphy.c150027
Panicker V, Cluett C, Shields B, Murray A, Parnell KS, Perry JR et al (2008) A common variation in deiodinase 1 gene DIO1 is associated with the relative levels of free thyroxine and triiodothyronine. J Clin Endocrinol Metab 93:3075–3081. https://doi.org/10.1210/jc.2008-0397
Patel J, Landers K, Li H, Mortimer RH, Richard K (2011) Thyroid hormones and fetal neurological development. J Endocrinol 209:1–8. https://doi.org/10.1530/JOE-10-0444
Pereira PP, Da Mata FA, Figueiredo AC, de Andrade KR, Pereira MG (2017) Maternal active smoking during pregnancy and low birth weight in the Americas: a systematic review and meta-analysis. Nicotine Tob Res 19:497–505. https://doi.org/10.1093/ntr/ntw228
R Core Team (2021) R: a language and environment for statistical computing. R foundation for statistical computing, Vienna, Austria. https://www.R-project.org/. Accessed 29 December 2021
Robbins J (1981) Factors altering thyroid hormone metabolism. Environ Health Perspect 38:65–70. https://doi.org/10.1289/ehp.813865
Rogers I, Emmett P, Ness A, Golding J (2004) Maternal fish intake in late pregnancy and the frequency of low birth weight and intrauterine growth retardation in a cohort of British infants. J Epidemiol Community Health 58:486–492. https://doi.org/10.1136/jech.2003.013565
Royston P, Ambler G (1998) Generalized additive models. Stata Tech Bull 7:38–43
Shemin D, Rittenberg D (1946) The life span of the human red blood cell. J Biol Chem 166:627–636. https://doi.org/10.1016/S0021-9258(17)35201-8
Shields B, Hill A, Bilous M, Knight B, Hattersley AT, Bilous RW et al (2009) Cigarette smoking during pregnancy is associated with alterations in maternal and fetal thyroid function. J Clin Endocrinol Metab 94:570–574. https://doi.org/10.1210/jc.2008-0380
Shields BM, Knight BA, Hill A, Hattersley AT, Vaidya B (2011) Fetal thyroid hormone level at birth is associated with fetal growth. J Clin Endocrinol Metab 96:E934-938. https://doi.org/10.1210/jc.2010-2814
Strain JJ, Davidson PW, Bonham MP, Duffy EM, Stokes-Riner A, Thurston SW et al (2008) Associations of maternal long-chain polyunsaturated fatty acids, methyl mercury, and infant development in the Seychelles Child dDevelopment Nutrition Study. Neurotoxicology 29:776–782. https://doi.org/10.1016/j.neuro.2008.06.002
Strain JJ, Bonham MP, Duffy EM, Wallace JMW, Robson PJ, Clarkson TW et al (2020) Nutrition and neurodevelopment: the search for candidate nutrients in the Seychelles Child Development Nutrition Study. Neurotoxicology 81:300–306. https://doi.org/10.1016/j.neuro.2020.09.021
Stråvik M, Jonsson K, Hartvigsson O, Sandin A, Wold AE, Sandberg AS et al (2019) Food and nutrient intake during pregnancy in relation to maternal characteristics: results from the NICE birth cohort in northern Sweden. Nutrients 11:1680. https://doi.org/10.3390/nu11071680
Sun XJ, Liu WY, Zhang B, Shen XT, Hu C, Chen XM et al (2019) Maternal heavy metal exposure, thyroid hormones, and birth outcomes: a prospective cohort study. J Clin Endocr Metab 104:5043–5052. https://doi.org/10.1210/jc.2018-02492
Tingley D, Yamamoto T, Hirose K, Keele L, Imai K (2014) Mediation: R package for causal mediation analysis. J Stat Softw 59:1–38
Vahter M, Akesson A, Lind B, Bjors U, Schutz A, Berglund M (2000) Longitudinal study of methylmercury and inorganic mercury in blood and urine of pregnant and lactating women, as well as in umbilical cord blood. Environ Res 84:186–194. https://doi.org/10.1006/enrs.2000.4098
Villanger GD, Learner E, Longnecker MP, Ask H, Aase H, Zoeller RT et al (2017) Effects of sample handling and analytical procedures on thyroid hormone concentrations in pregnant women’s plasma. Epidemiology 28:365–369. https://doi.org/10.1097/EDE.0000000000000606
Vrijkotte TG, Hrudey EJ, Twickler MB (2017) Early maternal thyroid function during gestation is associated with fetal growth, particularly in male newborns. J Clin Endocrinol Metab 102:1059–1066. https://doi.org/10.1210/jc.2016-3452
Wang D, Cheng X, Yu S, Qiu L, Lian X, Guo X et al (2018) Data mining: seasonal and temperature fluctuations in thyroid-stimulating hormone. Clin Biochem 60:59–63. https://doi.org/10.1016/j.clinbiochem.2018.08.008
Xu Y, Wahlberg K, Love TM, Watson GE, Yeates AJ, Mulhern MS et al (2019) Associations of blood mercury and fatty acid concentrations with blood mitochondrial DNA copy number in the seychelles child development nutrition study. Environ Int 124:278–283. https://doi.org/10.1016/j.envint.2019.01.019
Zhang HD, Ma YJ, Liu QF, Ye TZ, Meng FY, Zhou YW, et al (2018) Human erythrocyte lifespan measured by Levitt's CO breath test with newly developed automatic instrument. J Breath Res 12:036003. https://doi.org/10.1088/1752-7163/aaacf1
Zhang C, Yang X, Zhang Y, Guo F, Yang S, Peeters RP et al (2019) Association between maternal thyroid hormones and birth weight at early and late pregnancy. J Clin Endocrinol Metab 104:5853–5863. https://doi.org/10.1210/jc.2019-00390
Zhou B, Chen Y, Cai WQ, Liu L, Hu XJ (2020) Effect of gestational weight gain on associations between maternal thyroid hormones and birth outcomes. Front Endocrinol (lausanne) 11:610. https://doi.org/10.3389/fendo.2020.00610
Zimmermann MB (2009) Iodine deficiency in pregnancy and the effects of maternal iodine supplementation on the offspring: a review. Am J Clin Nutr 89:668S-672S. https://doi.org/10.3945/ajcn.2008.26811C
Acknowledgements
We give our warmest thanks to all the families who participated in this study, without whom the NICE cohort would not exist.
Funding
Open access funding provided by Karolinska Institute. This project was funded by the Swedish Research Council Formas (Project No. 2018-02275, MK, and 2019-01007, MV), the Swedish Research Council (VR; Project No 2019-01317, A-SS), Swedish Research Council for Health, Working Life and Welfare (FORTE; Project No 2018-00485, AEW), and Karolinska Institutet. The funding sources for this study were not involved in the study design, the collection, analysis or interpretation of data, or in the writing of the article, or the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
KG: Methodology, formal analysis, investigation, data curation, writing—original draft, visualization. KOE: Methodology, formal analysis writing—review and editing. MB: Data curation, writing—review and editing, project administration. BJ: Writing—review and editing. AS: Resources, project administration, writing—review and editing. ASS: Project administration, funding acquisition, writing—review and editing. AEW: Project administration, funding acquisition, writing—review and editing. MV: Conceptualization, project administration, funding acquisition, writing—review and editing. MK: Conceptualization, writing—review and editing, supervision, project administration, funding acquisition.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no known competing financial interests or personal relationships that could have influenced the work reported in this paper.
Ethical Approval
The study was performed in accordance with the principles of the Declaration of Helsinki and approved by the Regional Ethical Review Board, Umeå, Sweden (Ethical Permits: 2013/18-31M and 2018-256-32M).
Consent to Participate
Participation of this study was voluntary, and the mothers provided a written consent about their own participation at enrollment and about the participation of their child at delivery. All participants were informed that they could withdraw from the study at any time point without explanation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gustin, K., Ekvall, K.O., Barman, M. et al. Mediation by Thyroid Hormone in the Relationships Between Gestational Exposure to Methylmercury and Birth Size. Expo Health 16, 357–368 (2024). https://doi.org/10.1007/s12403-023-00556-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12403-023-00556-x