Abstract
Background
The most reliable quantitative variable on Rubidium-82 (82Rb) cardiac PET/CT for predicting major adverse cardiovascular events (MACE) has not been characterized with low-dose silicon photomultipliers (SiPM) technology, which allows halving injected activity and radiation dose delivering less than 1.0 mSv in a 70-kg individual.
Methods and Results
We prospectively enrolled 234 consecutive participants with suspected myocardial ischemia. Participants underwent 82Rb cardiac SiPM PET/CT (5 MBq/kg) and were followed up for MACE over 652 days (interquartile range 559-751 days). For each participant, global stress myocardial blood flow (stress MBF), global myocardial flow reserve (MFR), and regional severely reduced myocardial flow capacity (MFCsevere) were measured. The Youden index was used to select optimal thresholds.
In multivariate analysis after adjustments for clinical risk factors, reduced global stress MBF < 1.94 ml/min/g, reduced global MFR < 1.98, and regional MFCsevere > 3.2% of left ventricle emerged all as independent predictors of MACE (HR 4.5, 3.1, and 3.67, respectively, p < 0.001). However, only reduced global stress MBF remained an independent prognostic factor for MACE after adjusting for clinical risk factors and the combined use of global stress MBF, global MFR, and regional MFCsevere impairments (HR 2.81, p = 0.027).
Conclusion
Using the latest SiPM PET technology with low-dose 82Rb halving the standard activity to deliver < 1 mSv for a 70-kg patient, impaired global stress MBF, global MFR, and regional MFC were powerful predictors of cardiovascular events, outperforming traditional cardiovascular risk factors. However, only reduced global stress MBF independently predicted MACE, being superior to global MFR and regional MFC impairments.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myocardial perfusion imaging is a powerful non-invasive functional tool for risk stratification, recommended by clinical practice guidelines.1,2,3,4,5 Compared with relative perfusion images, absolute quantification of myocardial blood flow (MBF) by positron emission tomography (PET) could improve risk stratification.6 Global and regional perfusion provide information on different aspects of myocardial perfusion. Impairment in global perfusion may be caused by either multivessel epicardial disease or microcirculatory dysfunction. Regional absolute perfusion measurements may enable the additive detection of small regional defects caused by epicardial coronary artery disease (CAD), which could not be detected with average global perfusion measurements.6
The myocardial flow capacity (MFC) concept is a precise regional approach integrating both MFR and stress MBF through the pathophysiologic severity of CAD to depict regional quantitative flow metrics on a per pixel basis.6,7 MFC may overcome some of the limitations of using stress MBF or MFR alone and represents a promising tool to improve clinical decision-making.7,8,9 However, despite a robust conceptual validation and recently promising clinical data especially after revascularization, further validations of the prognostic potential of MFC in comparison with stress MBF and MFR are still needed.8,9,10
Silicon photomultipliers with digital readout (SiPM) PET represents a major advancement in PET technology. This new system including smaller crystals exhibits a much higher sensitivity and outperforms previous PET scanners using conventional photomultiplier tubes according to essential PET parameters such as spatial and timing resolution or noise-equivalent count-rate.11 Moreover, this novel technology allows for the reduction of the standard dose, with an improved image quality.12 Although research about the diagnostic accuracy of this dedicated SiPM PET system has been performed in a preliminary comparative study with a small sample size,13 no previous study has evaluated the prognostic value of PET myocardial perfusion imaging with SiPM.
The aim of this study was to prospectively compare on a low-dose SiPM PET camera, halving the activity and radiation dose of Rubidium-82 (82Rb), the prognostic value for cardiovascular events of stress MBF, MFR, and MFC.
Methods
Study population
We prospectively enrolled participants with clinical suspicion of myocardial ischemia (at the discretion of the referring clinician) to undergo 82Rb cardiac SiPM PET/computed tomography (CT) between June 2018 and June 2019 at the Lausanne University Hospital. Participants’ cardiovascular risk factors and medication use were ascertained at time of PET imaging. A history of CAD (“known CAD”) was defined as evidence of myocardial infarction (MI), previous percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG), or angiographically significant coronary stenosis (> 50% of the left main coronary artery or > 70% stenosis in any epicardial coronary artery). All procedures performed in this study were in accordance with the 1964 Helsinki declaration and its last amendments or comparable ethical standards. The Local Ethics Committee approved this study protocol (#PB_2017-00,634), and all participants gave written informed consent prior to inclusion.
Imaging protocol with SiPM 82Rb PET/CT
For each participant, a rest and adenosine or regadenoson stress SiPM PET/CT scan was performed, using a single dedicated camera (Biograph Vision 600, Siemens Medical Solutions, Knoxville, USA). Participants were instructed to fast for 6 h and avoid caffeine-containing food or beverages 24 h prior to the test. At rest, a 15-25 s intravenous (i.v.) infusion of low-dose (5 MBq/kg) 82Rb (Ruby-Fill® generator and 82Rb elution system [v3], Jubilant DraxImage, Kirkland, QC, Canada) was administered with an automatic infusion system and three-dimensional (3D) dynamic PET images were acquired starting at the beginning of the infusion over 6 min 19 s (12 × 8, 5 × 12, 1 × 30, 1 × 60, and 1 × 120 s). A second acquisition was then started following the same protocol with similar activity 2 min after the beginning of an adenosine infusion (140 mg/kg/min over 6 min) or following a regadenoson administration (400 µg over 10 s). A low-dose CT (100 keV, 16 mAs) transmission scan was used for attenuation correction. Images were reconstructed by ordered subsets expectation maximization algorithms (4 iterations, 5 subsets, 4.0 mm Full Width at Half Maximum (FWHM) Gaussian post-filter, 220 × 220-pixel matrix size). Blood pressure, heart rate, and a 12-lead ECG were recorded throughout the procedure. The radiation dose for a 70 kg participant was estimated to be 2 × 0.39 mSv for rest and stress 82Rb, and 1 × 0.17 mSv for the low-dose attenuation correction CT plus CT scout, resulting in a total dose of 0.95 mSv.
Usual quantitative myocardial perfusion analysis
Perfusion was assessed quantitatively measuring MBF in milliliter per minute per gram at rest and stress, using the highly automated FlowQuant v2.7 software (Ottawa, Ontario, Canada), with a 1-tissue compartment model with a flow-dependent extraction correction.14 MFR was calculated as follows: MFR = stress MBF/rest MBF. Rate-pressure product-adjusted rest MBF and MFR were determined to account for high resting heart rate or systolic blood pressure by multiplying rest MBF by 8500 mmHg/min and dividing by rate-pressure product (resting heart rate multiplied by resting systolic blood pressure). To reduce the potential spill-over in image-derived blood activity curves, a dual spill-over correction was systematically applied.15 Global partial-volume recovery correction and motion correction were also systematically applied.16
Myocardial flow capacity
MFC, developed by Johnson and Gould using 82Rb PET imaging, is a metric that integrates per pixel combination of resting MBF, stress MBF, and MFR into pathophysiologic severity categories by an integrated color map.7,8,9 MFC pixels (n = 513 on the polar map) having both MFR ≤ 1.5 and stress MBF ≤ 1.1 mL/min/g were defined as severely reduced MFC (MFCsevere) and were quantified as percent of left ventricle (LV). Because regional MFCsevere was the MFC category previously associated with the higher risk among all MFC category, only regional MFCsevere was included for MFC in this prognostic study.8,9
Clinical follow-up
The endpoint of the study was major adverse cardiovascular event (MACE), defined as cardiac death, MI, delayed revascularization (> 6 months post-PET/CT), hospitalization for congestive heart failure, or de novo stable angina. Early revascularizations observed within the first 6 months post-PET/CT were considered to have been triggered by the myocardial perfusion study and were excluded. Death from cardiac cause was defined as death from MI, congestive heart failure, valvular heart disease, sudden death, death without a witness or of unknown cause, and cardiac interventional/surgical procedure related. Hospitalization for de novo stable angina was defined as angina or chest pain of cardiac origin and requiring further investigations and hospitalization. Outcome information was obtained from medical records available in the hospital information system. If unsuccessful, participant follow-up was obtained by a phone call to cardiologists or general practitioners and/or participants. In participants with multiple MACE, only the first one was considered for survival analysis. Outcome data were collected from January to February 2021.
Statistics
We assessed the distribution of data with the Shapiro-Wilk test. Continuous normally distributed variables were presented as mean ± SD and compared using Student’s t-tests. Continuous non-normally distributed variables were presented as median [interquartile range] and compared using the Mann-Whitney U test. The chi-square test or Fisher exact test was used for analysis of categorical variables.
The Youden index was used to select optimal thresholds based on receiver operating characteristic curves for stress MFR, MFR, and MFCsevere measurements. Kaplan-Meier curves were used to elucidate the survival distributions regarding MACE. Differences in the outcomes of participants were assessed using the log-rank test. A Cox proportional hazard regression with adjustment for potential confounders was performed to determine the predictors of worse outcome. To prevent overfitting of the multivariate Cox proportional hazards models, only cardiovascular risk factors with p values < 0.05 in univariate Cox proportional regression models were considered in the multivariate models.
Collinearity between global stress MBF, global MFR, and regional MFCsevere was assessed by calculating the variance inflation factors in the final model (lower than five for each variable).17
The statistical analysis was performed using R version 4.1.1 (R Foundation for Statistical Computing, Vienna, Austria). All p values used were two-sided, with p < 0.05 considered statistically significant.
Results
Participant’s characteristics
The flowchart of the study is shown in Fig. 1. From June 2018 to June 2019, low-dose 82Rb SiPM PET/CT was performed in 279 participants. Two studies were excluded because of technical issues (delayed imaging after infusion start). Follow-up was successful in 274 of 277 remaining participants (99%). 40 participants were censored due to early revascularization (5 CABG surgery and 35 PCI, < 6 months after PET/CT). Baseline characteristics of the remaining study population of 234 participants are given in Table 1. Participants had a high prevalence of known CAD (54%), with a high burden of cardiovascular risk factors (hypertension: 73%; current or former tobacco use: 45%; dyslipidemia: 68%; diabetes: 36%). Preventive therapies were highly prescribed in the overall population: 58% with aspirin, 62% with beta-blockers, 58% with angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, and 66% with lipid-lowering agents.
Clinical outcomes
Over the 652 days [IQR: 559 to 751 days] of follow-up, a total of 47 participants experienced a MACE event (13 nonfatal MI, 5 cardiac deaths (1 participant had MI and then cardiac death), 10 cases of delayed revascularization, and 19 hospitalizations for congestive heart failure or de novo stable angina).
Comparative analysis
Participants with MACE had significantly worse global stress MBF, global MFR, and regional MFCsevere when compared with participants without (Table 2). In contrast, global rest MBF was similar among both groups. There was a significantly higher prevalence of known CAD or history of MI in participants with MACE as compared to participants without MACE (Table 1).
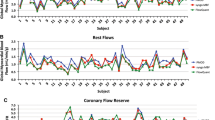
Optimal prognostic thresholds
Using the Youden index, we calculated the maximum potential effectiveness of global stress MBF, global MFR, and regional MFCsevere cutoffs for MACE prediction. For global absolute myocardial perfusion measurements, a threshold of 1.94 mL/min/g for global stress MBF achieved a specificity and sensitivity of 59% and 83%, a threshold of 1.98 for global MFR achieved a specificity and sensitivity of 73% and 64%, and a threshold of 3.2% of LV for regional MFCsevere achieved a specificity and sensitivity of 74% and 64%. Based on these calculated optimal thresholds, global MFR as well as regional MFCsevere was impaired in 78 (33%) participants, whereas global stress MBF was impaired in 113 (48%) participants (Table 2).
Univariate and multivariate analysis
The Kaplan-Meier survival curves indicated that participants with impaired global stress MBF, global MFR, or regional MFCsevere had significantly higher rates of MACE (all p < 0.0001) as compared with those with normal perfusion (Fig. 2). On univariate Cox proportional regression, global stress MBF, global MFR, and regional MFCsevere emerged all as significant predictors of MACE (Table 3). Male sex as well as known history of CAD and history of MI was also found to be significantly predictive of MACE (Table 3).
In multivariate analysis with 3 separate models including each time clinical risk factors and separately global stress MBF, global MFR, and regional MFCsevere, each one of these PET variables emerged as powerful independent predictors of MACE (Table 4). In contrast, clinical variables such as male sex, known CAD, and history of MI did not (Table 4).
Moreover, for the most comprehensive model including clinical parameters and all global MFR, global stress MBF, and regional MFCsevere, only global stress MBF emerged as an independent prognostic factor for MACE (hazard ratio (HR) 2.81, p = 0.027), while global MFR and regional MFCsevere did not (Table 4).
Discussion
Our results support that impaired global stress MBF, global MFR, and regional MFCsevere, as assessed by using low-dose 82Rb with the latest PET SiPM technology, allowing halving of the standard injected activity and radiation dose, are powerful predictors of cardiovascular events, outperforming traditional cardiovascular risk factors such as the presence of known CAD or history of MI. In a comprehensive analysis, we found that only reduced global stress MBF independently predicted MACE.
PET myocardial perfusion imaging is well established for the diagnostic and prognostic evaluation of patients with suspected CAD. Novel PET cameras using SiPM detectors offer a considerable advantage in radiation dose compared with the conventional PET cameras. For a 70-kg patient, the effective radiation dose could be reduced from > 4-mSv with the conventional PET cameras to < 1-mSv.18 However, no previous clinical study has evaluated the prognostic value of PET myocardial perfusion imaging with SiPM.
The independent prognostic value of reduced global stress MBF, being superior to global MFR and regional MFCsevere impairments, was unexpected and is discrepant as compared to previous studies. Regarding the prediction of cardiovascular deaths, Gupta et al. investigated the importance of global stress MBF and MFR.10 In this study, in multivariate analysis, the authors reported that the cardiovascular mortality was independently driven by global MFR, irrespective of whether the global stress MBF was impaired or preserved. Similar findings had been reported in the retrospective study by Fukushima et al.19 with a similar sample size as compared to the current study (n = 224 vs. n = 234 in the current study). However, compared with Fukushima et al.19 study, the current study has a longer follow-up (median, 652 vs. 426 days), and population as well as medication use depicted some difference (male sex, 65% vs. 40%; prior history of MI, 43% vs. 11%; beta-blockers, 62% vs. 18%). Taqueti et al. demonstrated that the prognostic value of MFR for the occurrence of MACE was independent of the extent and severity of coronary lesions as evaluated on coronary angiography, but stress MBF was not included in multivariate analysis.20 In an observational study by Patel et al., a threshold of 1.8 for global MFR has been identified to yield a benefit of coronary revascularization over medical treatment, independently of means of revascularization or the extent of myocardial ischemia on semi-quantitative analysis, but, again, stress MBF was not studied.21
Similar to the current cohort, other studies reported that global stress MBF was independently predictive for events, whereas global MFR was not. Global stress MBF was shown to be superior to global MFR for the prediction of MACE in a 82Rb PET/CT study by Farhad et al.18, and for the prediction of a composite of death and MI in a recent [15O]H2O PET/CT study by Bom et al.22. Since MFR is inherently dependent on resting flow, which is known to be highly sensitive to hemodynamic conditions, impairment of MFR may be less specific for the occurrence of events. However, importantly, both the study by Bom et al. and the current cohort used adjusted MFR for the resting rate-pressure product, accounting at least partially for changes in resting flow caused by differences in hemodynamic conditions. The present finding of a superiority of global stress MBF vs. global MFR impairments is consistent with the lack of association between resting MBF and clinical prognosis.23
Studies evaluating the prognostic value of MFC in comparison with stress MBF and MFR are scarce. Gould et al. showed in two recent observational studies with large cohorts over long-term follow-up that the extent of severe regional impairment of MFC, expressed as percent of LV as in the current cohort, provides optimal risk stratification and is associated with a survival benefit gain after revascularization.8,9 This risk stratification after revascularization was better assessed by severe regional MFC alteration rather than global MBF alteration.9 Recent studies using modified MFC with average MFR and stress MBF per coronary territory have shown an association with cardiovascular death and MACE.24,25
Considering other regional quantitative measures, our results are consistent with Bom et al. who found in a [15O]H2O PET/CT study that both global and regional stress MBF have prognostic value in predicting cardiac events, while the combination of global and regional stress MBF did not improve the prognostic performance compared to either alone.22 Harjulahti et al. found similar results using also [15O]H2O PET/CT.4 In contrast, Von Felten et al. recently demonstrated using 13 N-ammonia, an independent prognostic value of regional MFR < 2, being superior to global stress MBF and MFR.26 In the current study, the first using the latest SiPM technology, whose characteristics might offer potential benefits for precise analysis, we found that severe regional per pixel MFC impairment is a powerful predictor of cardiovascular events, independent from traditional cardiovascular risk factors, but not from global perfusion parameters. Although the current study has inherent limitations which could limit the scope of the results, these data support a close relationship between global and regional perfusion.22
Limitations
This study must be interpreted in the context of its single-center design, with an average sample size despite a high completeness of follow-up, which still limits extensive subgroup analysis. The follow-up period was middle range, with a low incidence of hard cardiac events such as cardiac death. The present thresholds for the MFCsevere category (pixel having both MFR ≤ 1.5 and stress MBF ≤ 1.1 mL/min/g) were slightly different as compared to the thresholds used by Johnson and Gould (pixel having both MFR ≤ 1.27 and stress MBF ≤ 0.83 mL/min/g). However, significant contributions of these slight differences to the present results seem unlikely. Furthermore, currently available SiPM cameras differ significantly in design, and it cannot be excluded that different SiPM cameras have different prognostic ability. The current study emphasized on myocardial blood flow measurements, and LV ejection fraction, LV volumes, regional wall motion, coronary artery calcium score, and semi-quantitative evaluation of relative perfusion defects were not assessed in this study based on myocardial blood flow quantification, despite representing important information that could be part of routine PET/CT imaging. Finally, the current prognostic study did not assess diagnostic accuracy, which could be a strength of the quantification of regional perfusion with MFC.
New Knowledge Gained
This study shows the prognostic value of impaired stress MBF, MFR, and MFC for cardiovascular event using low-dose 82Rb SiPM PET/CT technology with halved injected activity delivering < 1.0-mSv radiation dose for a 70-kg patient.
Conclusion
In conclusion, this study using the latest SiPM PET technology with low-dose 82Rb, halving the standard activity, demonstrates that impaired global stress MBF, global MFR, and regional MFC are powerful predictors of cardiovascular events, outperforming traditional cardiovascular risk factors. However, we found that only reduced global stress MBF independently predicted MACE, being superior to global MFR and regional MFC impairments.
Abbreviations
- MBF:
-
Myocardial blood flow
- MFR:
-
Myocardial flow reserve
- PET:
-
Positron emission tomography
- CAD:
-
Coronary artery disease
- MFC:
-
Myocardial flow capacity
- SiPM:
-
Silicon photomultipliers with digital readout
- 82Rb:
-
Rubidium-82
- LV:
-
Left ventricle
- MACE:
-
Major adverse cardiovascular event
- MI:
-
Myocardial infarction
References
Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 2020;41:407‐77.
Juarez-Orozco LE, Tio RA, Alexanderson E, Dweck M, Vliegenthart R, El Moumni M, et al. Quantitative myocardial perfusion evaluation with positron emission tomography and the risk of cardiovascular events in patients with coronary artery disease: a systematic review of prognostic studies. Eur Heart J Cardiovasc Imaging 2018;19:1179‐87.
Zampella E, Acampa W, Assante R, Gaudieri V, Nappi C, Mannarino T, et al. Combined evaluation of regional coronary artery calcium and myocardial perfusion by (82)Rb PET/CT in predicting lesion-related outcome. Eur J Nucl Med Mol Imaging 2020;47:1698‐704.
Harjulahti E, Maaniitty T, Nammas W, Stenstrom I, Biancari F, Bax JJ, et al. Global and segmental absolute stress myocardial blood flow in prediction of cardiac events: [(15)O] water positron emission tomography study. Eur J Nucl Med Mol Imaging 2021;48:1434‐44.
Weber BN, Stevens E, Perez-Chada LM, Brown JM, Divakaran S, Bay C, et al. Impaired Coronary Vasodilator Reserve and Adverse Prognosis in Patients With Systemic Inflammatory Disorders. JACC Cardiovasc Imaging 2021;14:2212‐20.
Gould KL, Johnson NP, Bateman TM, Beanlands RS, Bengel FM, Bober R et al. Anatomic versus physiologic assessment of coronary artery disease. Role of coronary flow reserve, fractional flow reserve, and positron emission tomography imaging in revascularization decision-making. J Am Coll Cardiol 2013;62:1639-53.
Johnson NP, Gould KL. Integrating noninvasive absolute flow, coronary flow reserve, and ischemic thresholds into a comprehensive map of physiological severity. JACC Cardiovasc Imaging 2012;5:430‐40.
Gould KL, Johnson NP, Roby AE, Nguyen T, Kirkeeide R, Haynie M, et al. Regional, Artery-Specific Thresholds of Quantitative Myocardial Perfusion by PET Associated with Reduced Myocardial Infarction and Death After Revascularization in Stable Coronary Artery Disease. J Nucl Med 2019;60:410‐7.
Gould KL, Kitkungvan D, Johnson NP, Nguyen T, Kirkeeide R, Bui L, et al. Mortality Prediction by Quantitative PET Perfusion Expressed as Coronary Flow Capacity With and Without Revascularization. JACC Cardiovasc Imaging 2021;14:1020‐34.
Gupta A, Taqueti VR, van de Hoef TP, Bajaj NS, Bravo PE, Murthy VL, et al. Integrated Noninvasive Physiological Assessment of Coronary Circulatory Function and Impact on Cardiovascular Mortality in Patients With Stable Coronary Artery Disease. Circulation 2017;136:2325‐36.
van Sluis J, de Jong J, Schaar J, Noordzij W, van Snick P, Dierckx R, et al. Performance Characteristics of the Digital Biograph Vision PET/CT System. J Nucl Med 2019;60:1031‐6.
Wagatsuma K, Miwa K, Sakata M, Oda K, Ono H, Kameyama M, et al. Comparison between new-generation SiPM-based and conventional PMT-based TOF-PET/CT. Phys Med 2017;42:203‐10.
Koenders SS, van Dalen JA, Jager PL, Knollema S, Timmer JR, Mouden M, et al. Value of SiPM PET in myocardial perfusion imaging using Rubidium-82. J Nucl Cardiol 2022;29:204‐12.
Dekemp RA, Declerck J, Klein R, Pan XB, Nakazato R, Tonge C, et al. Multisoftware reproducibility study of stress and rest myocardial blood flow assessed with 3D dynamic PET/CT and a 1-tissue-compartment model of 82Rb kinetics. J Nucl Med 2013;54:571‐7.
Efseaff M, Klein R, Ziadi MC, Beanlands RS, deKemp RA. Short-term repeatability of resting myocardial blood flow measurements using rubidium-82 PET imaging. J Nucl Cardiol 2012;19:997‐1006.
Hunter CR, Klein R, Beanlands RS, deKemp RA. Patient motion effects on the quantification of regional myocardial blood flow with dynamic PET imaging. Med Phys 2016;43:1829.
Sheather SJ. A Modern Approach to Regression with R. New York: Springer; 2009.
Farhad H, Dunet V, Bachelard K, Allenbach G, Kaufmann PA, Prior JO. Added prognostic value of myocardial blood flow quantitation in rubidium-82 positron emission tomography imaging. Eur Heart J Cardiovasc Imaging 2013;14:1203‐10.
Fukushima K, Javadi MS, Higuchi T, Lautamaki R, Merrill J, Nekolla SG, et al. Prediction of short-term cardiovascular events using quantification of global myocardial flow reserve in patients referred for clinical 82Rb PET perfusion imaging. J Nucl Med 2011;52:726‐32.
Taqueti VR, Hachamovitch R, Murthy VL, Naya M, Foster CR, Hainer J, et al. Global coronary flow reserve is associated with adverse cardiovascular events independently of luminal angiographic severity and modifies the effect of early revascularization. Circulation 2015;131:19‐27.
Patel KK, Spertus JA, Chan PS, Sperry BW, Al Badarin F, Kennedy KF, et al. Myocardial blood flow reserve assessed by positron emission tomography myocardial perfusion imaging identifies patients with a survival benefit from early revascularization. Eur Heart J 2020;41:759‐68.
Bom MJ, van Diemen PA, Driessen RS, Everaars H, Schumacher SP, Wijmenga JT, et al. Prognostic value of [15O]H2O positron emission tomography-derived global and regional myocardial perfusion. Eur Heart J Cardiovasc Imaging 2020;21:777‐86.
Johnson NP, Gould KL, De Bruyne B. Autoregulation of Coronary Blood Supply in Response to Demand: JACC Review Topic of the Week. J Am Coll Cardiol 2021;77:2335‐45.
Miura S, Naya M, Kumamaru H, Ando A, Miyazaki C, Yamashita T. Prognostic value of modified coronary flow capacity by (13)N-ammonia myocardial perfusion positron emission tomography in patients without obstructive coronary arteries. J Cardiol 2022;79:247‐56.
de Winter RW, Jukema RA, van Diemen PA, Schumacher SP, Driessen RS, Stuijfzand WJ, et al. The impact of coronary revascularization on vessel-specific coronary flow capacity and long-term outcomes: a serial [15O]H2O positron emission tomography perfusion imaging study. Eur Heart J Cardiovasc Imaging 2022;23:743‐52.
von Felten E, Benz DC, Benetos G, Baehler J, Patriki D, Rampidis GP, et al. Prognostic value of regional myocardial flow reserve derived from (13)N-ammonia positron emission tomography in patients with suspected coronary artery disease. Eur J Nucl Med Mol Imaging 2021;49:311‐20.
Acknowledgements
The authors would like to thank Mr. Pierre Louis Dietz (MSc, Squarepoint Capital, Paris, France) for his scientific help in this study and Ms. Christine Geldhof (Lausanne University Hospital, Lausanne, Switzerland) for her help with the Ethics Committee.
Funding
Open access funding provided by University of Lausanne. Dr. Matthieu Dietz was supported by Research Fellowship Awards from the Société Française de Radiologie, Paris, France, and from the Agence Régionale de Santé Auvergne-Rhone-Alpes, Lyon, France.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Dietz has nothing to disclose. Dr. Kamani has nothing to disclose. Dr. Allenbach has nothing to disclose. Dr. Rubimbura has nothing to disclose. Dr. Fournier has nothing to disclose. Dr. Dunet has nothing to disclose. Dr. Treglia has nothing to disclose. Dr. Nicod Lalonde has nothing to disclose. Dr. Schaefer has nothing to disclose. Dr. Eeckhout has nothing to disclose. Dr. Muller has nothing to disclose. Dr. Prior has nothing to disclose. The authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
The authors have also provided an audio summary of the article, which is available to download as ESM, or to listen to via the JNC/ASNC Podcast.
All editorial decisions for this article, including selection of reviewers and the final decision, were made by guest editor Jeroen J Bax, MD.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dietz, M., Kamani, C.H., Allenbach, G. et al. Comparison of the prognostic value of impaired stress myocardial blood flow, myocardial flow reserve, and myocardial flow capacity on low-dose Rubidium-82 SiPM PET/CT. J. Nucl. Cardiol. 30, 1385–1395 (2023). https://doi.org/10.1007/s12350-022-03155-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-022-03155-6