Abstract
Coronary flow reserve (CFR) with positron emission tomography/computed tomography (PET/CT) has an important role in the diagnosis of coronary microvascular disease (CMD), aids risk stratification and may be useful in monitoring therapy. CMD contributes to symptoms and a worse prognosis in patients with coronary artery disease (CAD), nonischemic cardiomyopathies, and heart failure. CFR measurements may improve our understanding of the role of CMD in symptoms and prognosis in CAD and other cardiovascular diseases. The clinical presentation of CAD has changed. The prevalence of nonobstructive CAD has increased to about 50% of patients with angina undergoing angiography. Ischemia with nonobstructive arteries (INOCA) is recognized as an important cause of symptoms and has an adverse prognosis. Patients with INOCA may have ischemia due to CMD, epicardial vasospasm or diffuse nonobstructive CAD. Reduced CFR in patients with INOCA identifies a high-risk group that may benefit from management strategies specific for CMD. Although measurement of CFR by PET/CT has excellent accuracy and repeatability, use is limited by cost and availability. CFR measurement with single-photon emission tomography (SPECT) is feasible, validated, and would increase availability and use of CFR. Patients with CMD can be identified by reduced CFR and selected for specific therapies.





Similar content being viewed by others
Abbreviations
- CAD:
-
Coronary artery disease
- CAC:
-
Coronary artery calcification
- CFR:
-
Coronary flow reserve
- CMD:
-
Coronary microvascular disease
- INOCA:
-
Ischemia with nonobstructive CAD
- LVEF:
-
Left ventricular ejection fraction
- MBF:
-
Myocardial blood flow
- MPI:
-
Myocardial perfusion imaging
- PET/CT:
-
Positron emission tomography/computed tomography
- SPECT:
-
Single-photon emission computed tomography
References
Taqueti VR, Di Carli MF. Coronary microvascular disease pathogenic mechanisms and therapeutic options: JACC state-of-the-art review. J Am Coll Cardiol 2018;72:2625‐41. https://doi.org/10.1016/j.jacc.2018.09.042.
Di Carli MF. Changing epidemiology of CAD: Why should we pay attention? J Nucl Cardiol 2021;28:386‐8. https://doi.org/10.1007/s12350-021-02560-7.
Jespersen L, Hvelplund A, Abildstrøm SZ, Pedersen F, Galatius S, Madsen JK. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J 2012;33:734‐44. https://doi.org/10.1093/eurheartj/ehr331.
Reeh J, Therming CB, Heitmann M, Højberg S, Sørum C, Bech J, et al. Prediction of obstructive coronary artery disease and prognosis in patients with suspected stable angina. Eur Heart J 2019;40:1426‐35. https://doi.org/10.1093/eurheartj/ehy806.
Rozanski A, Gransar H, Hayes SW, Min J, Friedman JD, Thomson LE, et al. Temporal trends in the frequency of inducible myocardial ischemia during cardiac stress testing: 1991 to 2009. J Am Coll Cardiol 2013;61:1054‐65. https://doi.org/10.1016/j.jacc.2012.11.056.
Jouni H, Askew JW, Crusan DJ, Miller TD, Gibbons RJ. Temporal trends of single-photon emission computed tomography myocardial perfusion imaging in patients with coronary artery disease: A 22-year experience from a tertiary academic medical center. Circ Cardiovasc Imaging 2017;10:e005628. https://doi.org/10.1161/CIRCIMAGING.116.005628.
Maddox TM, Stanislawski MA, Grunwald GK, Bradley SM, Ho PM, Tsai TT, et al. Nonobstructive coronary artery disease and risk of myocardial infarction. JAMA 2014;312:1754‐63. https://doi.org/10.1001/jama.2014.14681.
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: A report from the American Heart Association. Circulation 2020;141:e139‐596. https://doi.org/10.1161/CIR.0000000000000757.
Murthy VL, Naya M, Taqueti VR, Foster CR, Gaber M, Hainer J, et al. Effects of sex on coronary microvascular dysfunction and cardiac outcomes. Circulation 2014;129:2518‐27. https://doi.org/10.1161/CIRCULATIONAHA.113.008507.
Sara JD, Widmer RJ, Matsuzawa Y, Lennon RJ, Lerman LO, Lerman A. Prevalence of coronary microvascular dysfunction among patients with chest pain and nonobstructive coronary artery disease. JACC Cardiovasc Interv 2015;8:1445‐53. https://doi.org/10.1016/j.jcin.2015.06.017.
Mygind ND, Michelsen MM, Pena A, Frestad D, Dose N, Aziz A, et al. Coronary microvascular function and cardiovascular risk factors in women with angina pectoris and no obstructive coronary artery disease: The iPOWER Study. J Am Heart Assoc 2016;5:e003064. https://doi.org/10.1161/JAHA.115.003064.
Ong P, Camici PG, Beltrame JF, Crea F, Shimokawa H, Sechtem U, et al. International standardization of diagnostic criteria for microvascular angina. Int J Cardiol 2018;250:16‐20. https://doi.org/10.1016/j.ijcard.2017.08.068.
Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med 2007;356:830‐40. https://doi.org/10.1056/NEJMra061889.
Camici P, Chiriatti G, Lorenzoni R, Bellina RC, Gistri R, Italiani G, et al. Coronary vasodilation is impaired in both hypertrophied and nonhypertrophied myocardium of patients with hypertrophic cardiomyopathy: a study with nitrogen-13 ammonia and positron emission tomography. J Am Coll Cardiol 1991;17:879‐86. https://doi.org/10.1016/0735-1097(91)90869-b.
Cecchi F, Olivotto I, Gistri R, Lorenzoni R, Chiriatti G, Camici PG. Coronary microvascular dysfunction and prognosis in hypertrophic cardiomyopathy. N Engl J Med 2003;349:1027‐35. https://doi.org/10.1056/NEJMoa025050.
Bravo PE, Zimmerman SL, Luo HC, Pozios I, Rajaram M, Pinheiro A, et al. Relationship of delayed enhancement by magnetic resonance to myocardial perfusion by positron emission tomography in hypertrophic cardiomyopathy. Circ Cardiovasc Imaging 2013;6:210‐7. https://doi.org/10.1161/CIRCIMAGING.112.000110.
Castagnoli H, Ferrantini C, Coppini R, Passeri A, Baldini K, Berti V. Role of quantitative myocardial positron emission tomography for risk stratification in patients with hypertrophic cardiomyopathy: A 2016 reappraisal. Eur J Nucl Med Mol Imaging 2016;43:2413‐22. https://doi.org/10.1007/s00259-016-3465-7.
Lu DY, Yalçin H, Yalçin F, Zhao M, Sivalokanathan S, Valenta I, et al. Stress myocardial blood flow heterogeneity is a positron emission tomography biomarker of ventricular arrhythmias in patients with hypertrophic cardiomyopathy. Am J Cardiol 2018;121:1081‐9. https://doi.org/10.1016/j.amjcard.2018.01.022.
Dorbala S, Vangala D, Bruyere J Jr, Quarta C, Kruger J, Padera R, et al. Coronary microvascular dysfunction is related to abnormalities in myocardial structure and function in cardiac amyloidosis. JACC Heart Fail 2014;2:358‐67. https://doi.org/10.1016/j.jchf.2014.03.009.
Omerovic E, Citro R, Bossone E, Redfors B, Backs J, Bruns B, et al. Pathophysiology of Takotsubo syndrome—A joint scientific statement from the Heart Failure Association Takotsubo Syndrome Study Group and Myocardial Function Working Group of the European Society of Cardiology—Part 2: Vascular pathophysiology, gender and sex hormones, genetics, chronic cardiovascular problems and clinical implications. Eur J Heart Fail 2022;24:274‐86. https://doi.org/10.1002/ejhf.2368.
Galiuto L, De Caterina AR, Porfidia A, Paraggio L, Barchetta S, Locorotondo G, et al. Reversible coronary microvascular dysfunction: a common pathogenetic mechanism in Apical Ballooning or Tako-Tsubo Syndrome. Eur Heart J 2010;31:1319‐27. https://doi.org/10.1093/eurheartj/ehq039.
Anderson JL, Horne BD, Le VT, Bair TL, Min DB, Minder CM, et al. Spectrum of radionuclide perfusion study abnormalities in takotsubo cardiomyopathy. J Nucl Cardiol 2020. https://doi.org/10.1007/s12350-020-02385-w.
Neglia D, Michelassi C, Trivieri MG, Sambuceti G, Giorgetti A, Pratali L, et al. Prognostic role of myocardial blood flow impairment in idiopathic left ventricular dysfunction. Circulation 2002;105:186‐93. https://doi.org/10.1161/hc0202.102119.
Majmudar MD, Murthy VL, Shah RV, Kolli S, Mousavi N, Foster CR, et al. Quantification of coronary flow reserve in patients with ischaemic and non-ischaemic cardiomyopathy and its association with clinical outcomes. Eur Heart J Cardiovasc Imaging 2015;16:900‐9. https://doi.org/10.1093/ehjci/jev012.
Rabkin SW. Considerations in understanding the coronary blood flow—Left ventricular mass relationship in patients with hypertension. Curr Cardiol Rev 2017;13:75‐83. https://doi.org/10.2174/1573397112666160909093642.
Brown JM, Zhou W, Weber B, Divakaran S, Barrett L, Bibbo CF, et al. Low coronary flow relative to myocardial mass predicts heart failure in symptomatic hypertensive patients with no obstructive coronary artery disease. Eur Heart J 2021. https://doi.org/10.1093/eurheartj/ehab610.
Rajappan K, Rimoldi OE, Dutka DP, Ariff B, Pennell DJ, Sheridan DJ, et al. Mechanisms of coronary microcirculatory dysfunction in patients with aortic stenosis and angiographically normal coronary arteries. Circulation 2002;105:470‐6. https://doi.org/10.1161/hc0402.102931.
Rajappan K, Rimoldi OE, Camici PG, Bellenger NG, Pennell DJ, Sheridan DJ. Functional changes in coronary microcirculation after valve replacement in patients with aortic stenosis. Circulation 2003;107:3170‐5. https://doi.org/10.1161/01.CIR.0000074211.28917.31.
Zhou W, Sun YP, Divakaran S, Bajaj NS, Gupta A, Chandra A, et al. Association of myocardial blood flow reserve with adverse left ventricular remodeling in patients with aortic stenosis: The microvascular disease in aortic stenosis (MIDAS) study. JAMA Cardiol 2022;7:93‐9. https://doi.org/10.1001/jamacardio.2021.3396.
Zile MR, Gaasch WH, Patel K, Aban IB, Ahmed A. Adverse left ventricular remodeling in community-dwelling older adults predicts incident heart failure and mortality. JACC Heart Fail 2014;2:512‐22. https://doi.org/10.1016/j.jchf.2014.03.016.
Bairey Merz CN, Pepine CJ, Walsh MN, Fleg JL. Ischemia and no obstructive coronary artery disease (INOCA): Developing evidence-based therapies and research agenda for the next decade. Circulation 2017;135:1075‐92. https://doi.org/10.1161/CIRCULATIONAHA.116.024534.
Pasupathy S, Tavella R, Beltrame JF. Myocardial infarction with nonobstructive coronary arteries (MINOCA): The past, present, and future management. Circulation 2017;135:1490‐3. https://doi.org/10.1161/CIRCULATIONAHA.117.027666.
Taqueti VR, Everett BM, Murthy VL, Gaber M, Foster CR, Hainer J, et al. Interaction of impaired coronary flow reserve and cardiomyocyte injury on adverse cardiovascular outcomes in patients without overt coronary artery disease. Circulation 2015;131:528‐35. https://doi.org/10.1161/CIRCULATIONAHA.114.009716.
Taqueti VR, Solomon SD, Shah AM, Desai AS, Groarke JD, Osborne MT, et al. Coronary microvascular dysfunction and future risk of heart failure with preserved ejection fraction. Eur Heart J 2018;39:840‐9. https://doi.org/10.1093/eurheartj/ehx721.
Schindler TH, Cardenas J, Prior JO, Facta AD, Kreissl MC, Zhang XL, et al. Relationship between increasing body weight, insulin resistance, inflammation, adipocytokine leptin, and coronary circulatory function. J Am Coll Cardiol 2006;47:1188‐95. https://doi.org/10.1016/j.jacc.2005.10.062.
Bajaj NS, Osborne MT, Gupta A, Tavakkoli A, Bravo PE, Vita T, et al. Coronary microvascular dysfunction and cardiovascular risk in obese patients. J Am Coll Cardiol 2018;72:707‐17. https://doi.org/10.1016/j.jacc.2018.05.049.
Murthy VL, Naya M, Foster CR, Gaber M, Hainer J, Klein J, et al. Association between coronary vascular dysfunction and cardiac mortality in patients with and without diabetes mellitus. Circulation 2012;126:1858‐68. https://doi.org/10.1161/CIRCULATIONAHA.112.120402.
Osborne MT, Bajaj NS, Taqueti VR, Gupta A, Bravo PE, Hainer J, et al. Coronary microvascular dysfunction identifies patients at high risk of adverse events across cardiometabolic diseases. J Am Coll Cardiol 2017;70:2835‐7. https://doi.org/10.1016/j.jacc.2017.09.1104.
Murthy VL, Naya M, Foster CR, Hainer J, Gaber M, Dorbala S, et al. Coronary vascular dysfunction and prognosis in patients with chronic kidney disease. JACC Cardiovasc Imaging 2012;5:1025‐34. https://doi.org/10.1016/j.jcmg.2012.06.007.
Charytan DM, Skali H, Shah NR, Veeranna V, Cheezum MK, Taqueti VR, et al. Coronary flow reserve is predictive of the risk of cardiovascular death regardless of chronic kidney disease stage. Kidney Int 2018;93:501‐9. https://doi.org/10.1016/j.kint.2017.07.025.
Ford TJ, Stanley B, Good R, Rocchiccioli P, McEntegart M, Watkins S, et al. Stratified medical therapy using invasive coronary function testing in angina: The CorMicA trial. J Am Coll Cardiol 2018;72:2841‐55. https://doi.org/10.1016/j.jacc.2018.09.006.
Herzog BA, Husmann L, Valenta I, Gaemperli O, Siegrist PT, Tay FM, et al. Long-term prognostic value of 13N-ammonia myocardial perfusion positron emission tomography added value of coronary flow reserve. J Am Coll Cardiol 2009;54:150‐6. https://doi.org/10.1016/j.jacc.2009.02.069.
Ziadi MC, Dekemp RA, Williams KA, Guo A, Chow BJ, Renaud JM, et al. Impaired myocardial flow reserve on rubidium-82 positron emission tomography imaging predicts adverse outcomes in patients assessed for myocardial ischemia. J Am Coll Cardiol 2011;58:740‐8. https://doi.org/10.1016/j.jacc.2011.01.065.
Murthy VL, Naya M, Foster CR, Hainer J, Gaber M, Di Carli G, et al. Improved cardiac risk assessment with non-invasive measures of coronary flow reserve. Circulation 2011;124:2215‐24. https://doi.org/10.1161/CIRCULATIONAHA.111.050427.
Taqueti VR, Hachamovitch R, Murthy VL, Naya M, Foster CR, Hainer J, et al. Global coronary flow reserve is associated with adverse cardiovascular events independently of luminal angiographic severity and modifies the effect of early revascularization. Circulation 2015;131:19‐27. https://doi.org/10.1161/CIRCULATIONAHA.114.011939.
Taqueti VR, Shaw LJ, Cook NR, Murthy VL, Shah NR, Foster CR, et al. Excess cardiovascular risk in women relative to men referred for coronary angiography is associated with severely impaired coronary flow reserve. Not Obstr Dis Circ 2017;135:566‐77. https://doi.org/10.1161/CIRCULATIONAHA.116.023266.
Gupta A, Taqueti VR, van de Hoef TP, Bajaj NS, Bravo PE, Murthy VL, et al. Integrated noninvasive physiological assessment of coronary circulatory function and impact on cardiovascular mortality in patients with stable coronary artery disease. Circulation 2017;136:2325‐36. https://doi.org/10.1161/CIRCULATIONAHA.117.029992.
Murthy VL, Bateman TM, Beanlands RS, Berman DS, Borges-Neto S, Chareonthaitawee P, et al. Clinical quantification of myocardial blood flow using PET: Joint position paper of the SNMMI cardiovascular council and the ASNC. J Nucl Cardiol 2018;25:269‐97. https://doi.org/10.1007/s12350-017-1110-x.
Feher A, Sinusas AJ. Quantitative assessment of coronary microvascular function: Dynamic single-photon emission computed tomography, positron emission tomography, ultrasound, computed tomography, and magnetic resonance imaging. Circ Cardiovasc Imaging 2017;10:e006427. https://doi.org/10.1161/CIRCIMAGING.117.006427.
Slomka PJ, Miller RJH, Hu LH, Germano G, Berman DS. Solid-state detector SPECT myocardial perfusion imaging. J Nucl Med 2019;60:1194‐204. https://doi.org/10.2967/jnumed.118.220657.
Wells RG, Timmins R, Klein R, Lockwood J, Marvin B, deKemp RA, et al. Dynamic SPECT measurement of absolute myocardial blood flow in a porcine model. J Nucl Med 2014;55:1685‐91. https://doi.org/10.2967/jnumed.114.139782.
Nkoulou R, Fuchs TA, Pazhenkottil AP, Kuest SM, Ghadri JR, Stehli J, et al. Absolute myocardial blood flow and flow reserve assessed by gated SPECT with Cadmium-Zinc-telluride detectors using 99mTc-tetrofosmin: Head-to-head comparison with 13N-Ammonia PET. J Nucl Med 2016;57:1887‐92. https://doi.org/10.2967/jnumed.115.165498.
Wells RG, Marvin B, Poirier M, Renaud J, deKemp RA, Ruddy TD. Optimization of SPECT measurement of myocardial blood flow with corrections for attenuation, motion, and blood binding compared with PET. J Nucl Med 2017;58:2013‐9. https://doi.org/10.2967/jnumed.117.191049.
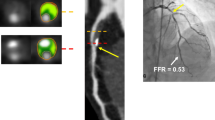
Agostini D, Roule V, Nganoa C, Roth N, Baavour R, Barienti JJ, et al. First validation of myocardial blood flow reserve assessed by dynamic (99m) Tc-sesamibi CZT-SPECT camera: Head to head comparison with (15)0-water PET and fractional flow reserve in patients with suspected coronary artery disease. The WATERDAY study. Eur J Nucl Med Mol Imaging 2018;45:1079‐90.
Giubbini R, Bertoli M, Durmo R, Bonacina M, Peli A, Faggiano I, et al. Comparison between N13NH3-PET and 99mTc-tetrofosmin-CZT-SPECT in the evaluation of absolute myocardial blood flow and flow reserve. J Nucl Cardiol 2019. https://doi.org/10.1007/s12350-019-01939-x.
Acampa W, Zampella E, Assante R, Genova A, De Simini G, Mannarino T, et al. Quantification of myocardial perfusion reserve by CZT-SPECT: A head to head comparison with 82Rubidium PET imaging. J Nucl Cardiol 2021;28:2827‐39. https://doi.org/10.1007/s12350-020-02129-w.
Wells RG, Radonjic I, Clackdoyle D, Do J, Marvin B, Carey C, et al. Test-retest precision of myocardial blood flow measurements with 99mtc-tetrofosmin and solid-state detector single photon emission computed tomography. Circ Cardiovasc Imaging 2020;13:e009769. https://doi.org/10.1161/CIRCIMAGING.119.009769.
Kitkungvan D, Johnson NP, Roby AE, Patel MB, Kirkeeide R, Gould KL. Routine clinical quantitative rest stress myocardial perfusion for managing coronary artery disease: clinical relevance of test-retest variability. JACC Cardiovasc Imaging 2017;10:565‐77. https://doi.org/10.1016/j.jcmg.2016.09.019.
Ben Bouallègue F, Roubille F, Lattuca B, Cung TT, Macia JC, Gervasoni R, et al. SPECT myocardial perfusion reserve in patients with multivessel coronary artery disease: Correlation with angiographic findings and invasive fractional flow reserve measurements. J Nucl Med 2015;56:1712‐7.
Shiraishi S, Sakamoto F, Tsuda N, Yoshida M, Tomiguchi S, Utsunomiya D, et al. Prediction of left main or 3-vessel disease using myocardial perfusion reserve on dynamic thallium-201 single-photon emission computed tomography with a semiconductor gamma camera. Circ J 2015;79:623‐31.
Miyagawa M, Nishiyama Y, Uetani T, Ogimoto A, Ikeda S, Ishimura H, et al. Estimation of myocardial flow reserve utilizing an ultrafast cardiac SPECT: Comparison with coronary angiography, fractional flow reserve, and the SYNTAX score. Int J Cardiol 2017;244:347‐53.
Han S, Kim YH, Ahn JM, Kang SJ, Oh JS, Shin E, et al. Feasibility of dynamic stress 201 Tl/rest 99m Tc-tetrofosmin single photon emission computed tomography for quantification of myocardial perfusion reserve in patients with stable coronary artery disease. Eur J Nucl Med Mol Imaging 2018;4:2173‐80.
Zavadovsky KV, Mochula AV, Boshchenko AA, Vrublevsky AV, Baev AE, Krylov AL, et al. Absolute myocardial blood flows derived by dynamic CZT scan vs invasive fractional flow reserve: Correlation and accuracy. J Nucl Cardiol 2019. https://doi.org/10.1007/s12350-019-01678-z.
Li C, Xu R, Yao K, Zhang J, Chen S, Pang L, et al. Functional significance of intermediate coronary stenosis in patients with single-vessel coronary artery disease: A comparison of dynamic SPECT coronary flow reserve with intracoronary pressure-derived fractional flow reserve (FFR). J Nucl Cardiol 2022;29:622‐9. https://doi.org/10.1007/s12350-020-02293-z.
Shiraishi S, Tsuda N, Sakamoto F, Ogasawara K, Tomiguchi S, Tsujita K, et al. Clinical usefulness of quantification of myocardial blood flow and flow reserve using CZT-SPECT for detecting coronary artery disease in patients with normal stress perfusion imaging. J Cardiol 2020;75:400‐9.
Panjer M, Dobrolinska M, Wagenaar NRL, Slart RHJA. Diagnostic accuracy of dynamic CZT-SPECT in coronary artery disease. A systematic review and meta-analysis. J Nucl Cardiol 2021. https://doi.org/10.1007/s12350-021-02721-8.
Liga R, Neglia D, Kusch A, Favilli B, Giorgetti A, Gimelli A. Prognostic role of dynamic CZT imaging in CAD patients: Interaction between absolute flow and CAD burden. JACC Cardiovasc Imaging 2022;15:540‐2. https://doi.org/10.1016/j.jcmg.2021.09.030.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Terrence Ruddy: GE Healthcare. Anahita Tavoosi: None. Viviany Taqueti: NIH K23HL135438.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarizes the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ruddy, T.D., Tavoosi, A. & Taqueti, V.R. Role of nuclear cardiology in diagnosis and risk stratification of coronary microvascular disease. J. Nucl. Cardiol. 30, 1327–1340 (2023). https://doi.org/10.1007/s12350-022-03051-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-022-03051-z