Abstract
Most duodenal diverticula (DD) are asymptomatic and rarely develop perforations. Perforation is the most serious complication of DD and often requires emergency surgery. A 97-year-old woman who had undergone total gastrectomy and Roux-en-Y reconstruction 30 years ago was referred to our department with chief complaints of abdominal pain and fever during her hospitalization after femoral neck fracture surgery in the orthopedic department. Contrast-enhanced computed tomography showed free air and residue in the abdominal cavity and right retroperitoneum, and an emergency laparotomy was performed. The abdominal cavity was mildly contaminated, and a 6-cm DD with a 1-cm perforation in the wall of the diverticulum on the contralateral side of the mesentery of the duodenum was found. Diverticulectomy and duodenal closure were performed and a drainage tube was placed. The patient experienced no complications and was transferred to the orthopedic department on postoperative day 10. Reports of perforation of DD after gastrectomy are very rare. Particular attention should be paid to perforation of DD after Billroth-II and Roux-en-Y reconstructions as they involve the formation of a duodenal stump that differs from the normal anatomy and may be highly invasive surgical procedures, depending on the degree of inflammation and fistula formation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A duodenal diverticulum (DD) is the second most common diverticulum occurring in the gastrointestinal tract after colonic diverticulum, with a prevalence of 1–2% on upper gastrointestinal series and 4–22% at autopsy [1, 2]. The most frequent location is the second portion of the duodenum. Around 95% of the patients are asymptomatic, and complications are reported in 5–10% of patients [3]. Major complications include biliary or pancreatic duct obstruction, hemorrhage, diverticulitis, Lemmel’s syndrome and perforation [4,5,6]. Perforation of a DD is the most serious complication, with diverticulitis being the most common cause, followed by enterolithiasis, iatrogenic origin, ulceration, traumatic injury, and foreign body [7]. Right upper quadrant pain with nausea and vomiting is one of the most frequent symptoms. Because a DD may cause abdominal pain with signs of peritoneal irritation but may only cause perforation to the retroperitoneum and not lead to panperitonitis, the symptoms of DD are frequently nonspecific, often making preoperative diagnosis difficult [8,9,10].
Reports of perforation of DD after gastrectomy are very rare. Particular attention should be paid to DD perforation after Billroth-II and Roux-en-Y (R-Y) reconstructions as they involve the formation of a duodenal stump that differs from the normal anatomy and may be highly invasive surgical procedures, depending on the degree of inflammation and fistula formation.
We report a very rare case of perforation of a DD after R-Y reconstruction in a super-elderly patient who was successfully treated surgically.
Case report
A 97-year-old woman who had undergone orthopedic surgery for a femoral neck fracture with open osteosynthesis and gamma nailing was referred to our department with chief complaints of abdominal pain and fever. Her medical history included a total gastrectomy 30 years ago with unknown details and chronic atrial fibrillation. The patient was taking an anticoagulant, non-steroidal anti-inflammatory drug, and proton pump inhibitor.
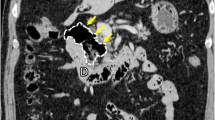
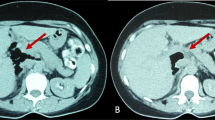
The patient developed sudden abdominal pain 9 days after orthopedic surgery and was referred to our department 3 h after the onset of abdominal pain. At referral to our department, the patient was 139 cm tall, weighed 32.2 kg, body mass index was 16.6 kg/m2, temperature was 38.6 ºC, pulse was 68 bpm, and blood pressure was 120/48 mmHg. Right lower abdominal pain was noted, but there were no signs of perineal irritation. Slightly elevated markers of inflammation and anemia were apparent, with a white blood cell count of 4740/μL, a C-reactive protein value of 2.12 mg/dL and hemoglobin of 9.0 g/dL; liver enzymes and creatinine were within normal limits. Contrast-enhanced computed tomography showed free air and residue in the abdominal cavity and right retroperitoneum (Fig. 1a-c), but it was difficult to identify the site of perforation, and an emergency laparotomy was performed for suspected DD perforation or the lower gastrointestinal tract perforation. At surgery, her abdominal cavity was mildly contaminated, a 6-cm DD located 30 cm from Y-anastomosis, and the DD with a 1-cm perforation in the wall of the diverticulum on the contralateral side of the mesentery of the duodenum were found, with the interior of the DD filled with food residue (Fig. 2a,b). We performed the diverticulectomy and duodenal closure (Fig. 2c) with placement of an infrahepatic drainage tube from the right side of the abdomen. Histopathological findings of the DD showed a true diverticulum with partial wall thinning and rupture (Fig. 3), suggesting perforation of the diverticulum due to increased internal pressure and chronic inflammation caused by food residue for many years. Oral intake was started on postoperative day (POD) 3. The drainage tube was removed on POD 5. The patient experienced no complications and was transferred to the orthopedic department on POD 10.
Surgical illustrations and intraoperative findings. a Illustration of the DD after the previous total gastrectomy and Roux-en-Y reconstruction. b A 6 cm duodenal diverticulum (DD) (arrowheads) and 1 cm perforation in the wall of the diverticulum on the contralateral side of the mesentery of the duodenum (arrow) were found. c After the diverticulectomy and simple duodenal closure. Sutures were on the contralateral side of the mesentery of the duodenum
Discussion
Reconstruction procedures for gastric cancer include the Billroth-I, Billroth-II, and R-Y reconstruction, with Billroth-II and R-Y reconstruction having an afferent loop and duodenal stump. Postoperative complications of R-Y reconstruction include Roux stasis syndrome, Petersen’s hernia, and duodenal stump leakage [11], with the latter considered to be caused by increased pressure at the edge of the stump due to intestinal peristalsis [12, 13]. To our knowledge, there have been only two reports of perforation of DD after gastric cancer surgery, one case with Billroth-II reconstruction [14] and two cases with R-Y reconstruction [15], both of which were considered to be caused by increased pressure in the afferent loop of the duodenum. Our patient was receiving postoperative care following repair of a femoral neck fracture, and there was food residue in the DD. In addition to weakening of the diverticular wall due to chronic inflammation caused by food residue remaining in the DD for many years, the temporary decrease in intestinal peristalsis caused by the physical stress of femoral bone surgery, especially the decrease in duodenal peristalsis, was considered to have increased pressure in the duodenum and caused the perforation of the DD.
Treatment options for perforation of DD can be conservative or surgical. Conservative treatment may be chosen for patients with micro-perforation, localized inflammation or abscess, and stable general condition with few symptoms [3, 16], but surgical treatment should be chosen for patients with panperitonitis or sepsis or those with significant leakage of intestinal contents due to perforation who are not expected to improve with conservative treatment. The first surgical treatment for perforation of DD is diverticulectomy and two-tiered duodenal closure [17,18,19]. However, in cases of severe inflammation of the duodenum and insecure closure or weakness of the duodenal wall, a duodenojejunostomy may be needed to reduce the risk of duodenal leakage or fistula. Although variations from R-Y duodenojejunostomy with gastro-jejunal exclusion to truncal vagotomy/antrectomy with Billroth II gastrojejunostomy or even pancreaticoduodenectomy have been reported [15, 20,21,22], an increase in surgical complications due to the high invasiveness of the procedure is a concern. Intra-abdominal drainage and feeding jejunostomy have also been reported to improve symptoms [23], and surgery such as surgical drainage or tube-duodenostomy is an option for older patients who are not expected to improve with conservative treatment and cannot tolerate highly invasive surgery or whose general condition is unstable. Fortunately, although our patient was 97 years old, she was still able to tolerate the surgery, which was completed with only a diverticulectomy and two-tiered duodenal closure. Because she had previously undergone total gastrectomy and R-Y reconstruction, gastrojejunostomy was not feasible. In addition, due to her age, it was difficult to perform highly invasive surgery such as pancreatoduodenectomy. If simple closure is not feasible because of excessive inflammation and a large DD fistula, palliative surgery such as surgical drainage or duodenojejunostomy, or biliary drainage through the biliary duct with cholecystectomy, may be considered.
In conclusion, in patients with total gastrectomy and R-Y reconstruction who develop a DD, the possibility of perforation due to increased intraduodenal pressure should be considered.
Abbreviations
- DD:
-
Duodenal diverticulum
- R-Y:
-
Roux-en-Y
- POD:
-
Postoperative day
References
Reed MF, Mathisen DJ. Tracheoesophageal fistula. Chest Surg Clin N Am. 2003;13:271–89.
Sakthivel S, Kannaiyan K, Thiagarajan S. Prevalence of duodenal diverticulum in South Indians: a cadaveric study. ISRN Anat. 2013. https://doi.org/10.5402/2013/767403.
Duarte B, Nagy KK, Cintron J. Perforated duodenal diverticulum. Br J Surg. 1992;79:877–81.
Chitambar IA, Springs C. Duodenal diverticula. Surgery. 1953;33:68–791.
Vassilakis JS, Tzovaras G, Chrysos E, et al. Roux-Y choledochojejunostomy and duodenojejunostomy for the complicated duodenal diverticulum. Am J Surg. 1997;174:45–8.
Bakula B, Romic I, Sever M, et al. Duodenal diverticulum causing obstructive jaundice—Lemmel’s syndrome. Rev Esp Enferm Dig. 2021;113:375–7.
Thorson CM, Paz Ruiz PS, Roeder RA, et al. The perforated duodenal diverticulum. Arch Surg. 2012;147:81–8.
Rossetti A, Christian BN, Pascal B, et al. Perforated duodenal diverticulum, a rare complication of a common pathology: a seven-patient case series. World J Gastrointest Surg. 2013;5:47–50.
Costa Simões V, Santos B, Magalhães S, et al. Perforated duodenal diverticulum: surgical treatment and literature review. Int J Surg Case Rep. 2014;5:547–50.
Kansoun A, El-Helou E, Amiry AR, et al. Surgical approach for duodenal diverticulum perforation: a case report. Int J Surg Case Rep. 2020;76:217–20.
Aurello P, Sirimarco D, Magistri P, et al. Management of duodenal stump fistula after gastrectomy for gastric cancer: Systematic review. World J Gastroenterol. 2015;21:7571–6.
Cozzaglio L, Coladonato M, Biffi R, et al. Duodenal fistula after elective gastrectomy for malignant disease : an Italian retrospective multicenter study. J Gastrointest Surg. 2010;14:805–11.
Ali BI, Park CH, Song KY. Outcomes of non-operative treatment for duodenal stump leakage after gastrectomy in patients with gastric cancer. J Gastric Cancer. 2016;16:28–33.
Tsukamoto T, Ohta Y, Hamba H, et al. Perforated duodenal diverticulum: report of two cases. Hepatogastroenterology. 1999;46:1755–8.
Yagi S, Ida S, Ohashi M, et al. Two cases of a perforated duodenal diverticulum after gastrectomy with Roux-en-Y reconstruction. Surg Case Rep. 2019;5:169.
Kim KH, Park SH. Conservative treatment of duodenal diverticulitis perforation: a case report and literature review. Open Access Emerg Med. 2018;10:101–4.
Juler GL, List JW, Stemmer EA, et al. Perforating duodenal diverticulitis. Arch Surg. 1969;99:572–8.
Stebbings WS, Thomson JP. Perforated duodenal diverticulum: a report of two cases. Postgrad Med J. 1985;61:839–40.
Oukachbi N, Brouzes S. Management of complicated duodenal diverticula. J Visc Surg. 2013;150:173–9.
Fujisaki S, Takashina M, Sakurai K, et al. Simple diversion by duodenojejunostomy for a retroperitoneal perforation of the second portion of the duodenal diverticulum. Int Surg. 2014;99:628–31.
Philip J, Cocieru A. Pancreatoduodenectomy in patient with perforated duodenal diverticulum and peritonitis: case report. Int J Surg Case Rep. 2019;58:48–9.
Kalogiannis E, Gussago S, Chappalley D, et al. Perforated duodenal diverticulitis: a case report of a rare surgical entity treated by Roux-en-Y deriving intestinal patch. Cureus. 2022;14: e23167.
Chen CF, Wu DC, Chen CW, et al. Successful management of perforated duodenal diverticulitis with intra-abdominal drainage and feeding jejunostomy: a case report and literature review. Kaohsiung J Med Sci. 2008;24:425–9.
Acknowledgements
We would like to thank Rise-Japan LLC (http://rise-japan.rulez.jp/) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights
All procedures performed in the study were in accordance with the ethical standards of the institutional review board and with the 1964 Helsinki Declaration and its later amendments.
Informed consent
This report was approved by the institutional review board of Takayama Red Cross Hospital (approval no.: R05-18), and informed consent was obtained from the patient presented in this report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ohno, S., Shinoda, T., Kawahara, T. et al. A perforation of a duodenal diverticulum in a 97-year-old patient after total gastrectomy and Roux-en-Y reconstruction: a case report. Clin J Gastroenterol (2024). https://doi.org/10.1007/s12328-024-01965-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12328-024-01965-4