Abstract
The pathogenesis of liver dysfunction that complicates coronavirus disease 2019 (COVID-19) remains unclear, especially in mild to moderate severity cases. In this case, a novel coronavirus infection was detected by polymerase chain reaction (PCR) in a 76-year-old woman hospitalized after presenting with fever. No other abnormal physical findings were observed, and oxygen administration was not required. Chest computed tomography (CT) showed a ground-glass-like and an infiltrative shadow in the right lung, and moderate COVID-19 was diagnosed. Initially, the fever resolved, and PCR turned negative; however, the fever reappeared on hospitalization day 14, and CT showed pneumonia exacerbation accompanied by new onset of fatty liver. Biochemical testing revealed marked liver dysfunction, accompanied by elevated serum interleukin (IL)-6, IL-10, and tumor necrosis factor-α levels. Physical findings and all laboratory parameters improved after conservative treatment, and she was discharged on day 22. A liver biopsy performed 44 days post-discharge showed T-cell-dominant inflammatory cell infiltration, mainly in the portal region. Some hepatocytes showed fatty degeneration.
We report a case of moderate COVID-19 in which histological hepatitis persisted after a substantial period had passed since the initial infection had cleared and associated transaminase elevations had resolved, with a comparison of serum cytokine dynamics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused a large global outbreak since the first cases of coronavirus disease 2019 (COVID-19) were observed in December 2019 in Wuhan, China [1, 2]. In Japan, the number of infected people has steadily increased since the first infection was confirmed in January 2020, and the cumulative number of cases exceeded 8,900,000 by June 2022 [2, 3].
Liver dysfunction is frequently observed in COVID-19 patients. A systemic immune response to the new coronavirus infection, expressed as a cytokine storm, has been assumed to be involved in the occurrence of liver dysfunction, though many aspects of this mechanism remain unclear [4, 5]. Liver dysfunction observed in COVID-19 patients has been associated with aggravation of clinical symptoms in severe cases; however, the behavior of elevated liver enzymes in non-severe COVID-19 cases has not been investigated thoroughly [6,7,8,9,10,11,12].
Histological liver characteristics in patients who developed liver dysfunction associated with COVID-19 also require clarification, as most previous reports have evaluated liver tissue collected from deceased patients, and histological liver findings in surviving patients have not been fully explored [7, 12,13,14]. Furthermore, there are no reports of a detailed examination of liver histology after clinical improvement of COVID-19 infection with concomitant hepatitis.
Here, we report a case of moderate COVID-19 illness with histological confirmation of hepatitis and steatosis after 6 weeks of viral clearance and normalization of transaminase levels. This case also demonstrated fluctuating serum cytokine levels in accordance with the stage of COVID-19 illness.
Case report
In April 2020, a 76-year-old woman with a history of COVID-19 illness in the family developed a low-grade fever. Two days later, she was hospitalized after her upper respiratory specimens tested positive for SARS-CoV-2 using polymerase chain reaction (PCR). The patient had a 20-year history of hypertension, hyperlipidemia, and hyperthyroidism, and had been receiving antihypertensive, lipid-metabolizing, and antithyroid medications. There was no past history of abnormal liver function or glucose intolerance and no history of smoking or alcohol consumption. In addition, she had no history of COVID-19 vaccination. On the day of admission, no fever, subjective symptoms, or abnormal physical findings were present.
The clinical features of this case are presented in Fig. 1. Computed tomography (CT) of the chest performed on the second day of admission showed ground-glass opacities from the upper lobe to the dorsal side of the lower lobe of the right lung (Fig. 2a, b). Other than CT scan, no imaging studies were performed during her hospitalization. Although imaging showed findings of pneumonia, the patient did not require oxygen administration. Thus, she was diagnosed with COVID-19 with moderate I severity based on the classification of the JAPAN COVID-19 Case Management Guide Review Committee [3]. Because the patient’s clinical symptoms were not severe, blood biochemical tests were not performed at the time of admission. Minocycline (200 mg per day) was initiated on the day of admission, and the following day when she developed a fever of 38 °C, favipiravir was started (3600 mg per day on the first day and 1600 mg per day thereafter). The fever increased to 38.8 °C on the third day of admission and resolved by the 6th day. However, olfactory disturbance appeared on the 7th day and lasted for 2 weeks, and the fever increased again to 38.8 °C on the 14th day.
Clinical course of the patient. PCR polymerase chain reaction, DLST drug-induced lymphocyte stimulation test, CT computed tomography, AST aspartate aminotransferase, ALT alanine aminotransferase, LDH lactate dehydrogenase, ALP alkaline phosphatase, CRP C-reactive protein, Alb albumin, WBC white blood cells, IL-6 interleukin-6, IL-10 interleukin-10, TNF-α tumor necrosis factor-alpha, TSH thyroid stimulating hormone, FT3 free triiodothyronine, FT4 free thyroxine, CA19-9 carbohydrate antigen 19–9
a Chest computed tomography (CT) taken on the second day of admission shows frosted and infiltrated shadows from the upper lobe of the right lung (arrowheads) to b the dorsal side of the lower lobe (arrowheads). c CT scan taken on the 16th day shows that the infiltrative image in the upper and lower lobes of the right lung, which had been noted on the second day, has improved, but there is the appearance of new frosted glassy shadows in the upper lobes (arrows). d New appearance of a partially frosted glassy shadow is also noted in the upper lobe of the left lung (arrow)
A second CT scan was performed on the 16th day, which showed that the infiltrative lesion in the upper and lower lobes of the right lung that had been noted at the time of admission had improved, but a frosted glassy shadow had appeared in the upper lobe. A new partially frosted glassy shadow was also noted in the upper lobe of the left lung (Fig. 2c, d). The hepatic CT attenuation values and the liver-to-spleen attenuation (L/S) ratio decreased from 52.8 to 34.4 and 1.05 to 0.77, respectively (Fig. 3a, b, c, d). This was considered to reflect the appearance of fatty change in the patient’s liver [15]. Consecutive SARS-CoV-2 PCR assays were conducted three times (on days 14, 15, and 17) and were all negative. Hence, re-infection or re-growth of SARS-CoV-2 was ruled out.
a Abdominal computed tomography (CT) taken the second day of admission shows that the attenuation value of the liver parenchyma is higher than those of the inferior vena cava and hepatic veins (arrowheads). b On the second day, hepatic CT attenuation value (HU: Hounsfield units) and liver-to-spleen attenuation (L/S) ratio was 52.8 and 1.05, respectively. c CT scan taken on the 16th day shows that the attenuation value of the liver parenchyma is reduced to the same level as that of the major intrahepatic vessels. d On the 16th day, the hepatic CT attenuation value (HU) and L/S ratio were 34.4 and 0.77, respectively
In order to examine the aetiology of fever recurrence, blood tests were performed alongside a second CT scan, which revealed an elevated white blood cell count with a predominance of neutrophils, accompanied by elevated C-reactive protein (CRP) levels. Elevated hepatobiliary enzymes were also observed as follows: aspartate aminotransferase, 431 U/L; alanine aminotransferase, 445 U/L; and alkaline phosphatase, 554 U/L. Increased serum lactate dehydrogenase (LDH) and decreased albumin (Alb) levels were also observed; however, there was no increase in serum bilirubin levels. There were no findings suggestive of viral hepatitis, and tumor markers indicated a minor abnormality in carbohydrate antigen 19–9 (CA 19–9). Although thyroid-stimulating hormone (TSH) levels slightly decreased, free triiodothyronine and free thyroxine levels were within normal limits. Serum interleukin (IL)-6 and tumor necrosis factor (TNF)-α levels were elevated to 26.4 and 31.0 pg/mL, respectively, on day 16. IL-10 levels were elevated to 8.0 pg/mL on day 18 (Table 1).
Although the patient had recurrent fever and olfactory disturbance, her general condition was good and no other abnormal findings, such as hypoxemia or skin rash, were observed. Favipiravir and minocycline were discontinued on days 15 and 16, respectively, and conservative treatment was continued. The patient’s fever resolved on the 19th day, and her blood test findings improved. She was discharged on the 22nd day. Along with clinical symptoms and elevated hepatobiliary enzyme levels, white blood cell count and serum IL-6, IL-10, TNF-α, CA 19–9, and TSH levels also improved (Fig. 1).
To examine whether there were any residual effects of COVID-19-associated liver damage even after the patient’s general condition recovered, an echo-guided percutaneous liver biopsy was performed 44 days after her discharge from the hospital, on day 66 of admission. Hematoxylin and eosin staining showed mononuclear cell-dominant inflammatory cell infiltration mainly in the portal area and partially in the dilated sinusoidal lumens. There was no evidence of thrombus formation in the sinusoids or other vessels. Fatty degeneration of some hepatocytes was also observed (Fig. 4a, b). There were no obvious abnormalities in the bile ducts. Masson’s trichrome staining showed inconspicuous fibrous enlargement of the portal area, and silver staining showed little evidence of destruction of the marginal plate, indicating the absence of preexisting liver fibrosis (Fig. 4c, d). Tissue immunostaining revealed that the infiltrating mononuclear cells were predominantly cluster of differentiation (CD) 3-positive mature T lymphocytes, with a similar proportion of CD4 and CD8 positive cells (Fig. 5a, b, c). Only a few CD20, forkhead box P3, and CD68 positive cells were found. Therefore, B cells, regulatory T cells, and macrophages were considered rare (Fig. 5d, e, f). These findings indicate that the histological liver dysfunction associated with COVID-19 may persist for a substantial amount of time even after the patient’s general condition has improved. Additionally, angiotensin-converting enzyme 2 (ACE2) expression, which plays a role in the intracellular invasion of SARS-CoV-2 [4, 5], was not found in the tissues (Fig. 5g). Sixty-three days after discharge (the 85th day), a drug-induced lymphocyte stimulation test (DLST) for favipiravir and minocycline was performed, and both were found to be negative.
a Pathological manifestations of the liver biopsy specimen obtained on the 66th day. Hematoxylin and eosin (H&E) staining shows mononuclear cell-dominant inflammatory cell infiltration mainly in the portal area (arrows). Fatty degeneration of some hepatocytes is also observed (arrowheads). b Inflammatory cell infiltration is also mainly observed in the dilated sinusoidal lumens (arrowheads). There is no evidence of thrombus formation in the sinusoids or other vessels. c Masson’s trichrome staining shows an inconspicuous fibrous enlargement of the portal area (arrows), (d) and silver staining shows little evidence of destruction of the marginal plate (arrows). (a H&E staining, × 100, b H&E staining, × 200, c Masson’s trichrome staining, × 100, d Silver staining, × 100)
a Tissue immunostaining reveals that the infiltrating mononuclear cells are predominantly cluster of differentiation (CD) 3-positive mature T lymphocytes, b with a similar proportion of CD4 and c CD8 positive cells. d Only a few CD20, e forkhead box P3 (FOXP3), and f CD68 positive cells are found. g Angiotensin-converting enzyme 2 (ACE2) expression, which functions in the intracellular invasion of SARS-CoV-2, is not found in the tissues. h Abundant ACE2 staining is seen in the epithelium of normal small intestinal specimens obtained from a 64 year-old woman (shown as a positive control). For immunostainings of ACE2, goat antihuman/mouse/rat/hamster ACE‑2 antigen affinity-purified polyclonal antibody (R&D Systems, Catalog # AF933) was used as primary antibody and rabbit antigoat biotinylated IgG (Vector Laboratories, Catalog # BA-5000) as secondary antibody. (a CD3 staining, × 200, b CD4 staining, × 200, c CD8 staining, × 200, d CD20 staining, × 200, e FOXP3 staining, × 200, f CD68 staining, × 200, g & h ACE2 staining, × 200)
Discussion
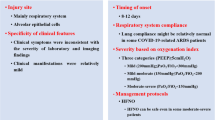
This report described a case of moderate COVID-19 illness with liver dysfunction where histological findings and cytokine dynamics were evaluated. Abnormal hepatological results have been reported in 14–76.3% of COVID-19 cases and have been recognized as a risk factor for worsening COVID-19 symptoms, especially in severe cases [6,7,8,9,10,11,12]. However, the significance of elevated hepatobiliary enzymes in mild and moderate cases of COVID-19 has not been fully investigated [4]. Because literature is scarce, we investigated the prevalence and clinical features of all non-severe COVID-19 cases with liver dysfunction at our institution. Among 39 cases of mild or moderate COVID-19 illness, 16 (41.0%) had developed liver dysfunction in the form of elevated hepatobiliary enzymes and/or jaundice (Table 2). Interestingly, 14 of them, including the present case, showed the presence of one or more of the following: hypoalbuminemia, increased serum CRP and LDH levels, or other reported markers of COVID-19 severity [4, 16]. In six cases, oxygen saturation fell below 93%, requiring oxygen supplementation [3]. These results suggest that non-severe cases of COVID-19 with abnormal liver function may also exhibit systemic features similar to severe cases. Among the 16 cases with liver dysfunction, liver biopsy and serum cytokine measurements were performed only for this case.
Evaluation of associated hepatic histological findings in COVID-19 patients with liver dysfunction, may aid in understanding the pathogenesis of novel coronavirus infection. In previous reports, morphological changes in the intrahepatic portal veins and sinusoids, inflammatory cell infiltration, and fatty degeneration of hepatocytes has been demonstrated [7, 12,13,14]. However, those were mainly derived from autopsies of cases with a serious clinical course including acute respiratory distress syndrome, respiratory failure, and hemorrhagic shock. Interestingly, similar characteristics were observed in this case of moderate COVID-19 illness with complete recovery. In addition, histological evidence of hepatitis persisted for a long time after virus elimination and normalization of liver enzymes. Hepatic steatosis has been suggested as a risk factor for severe COVID-19, but the mechanism is still unknown [9, 15]. In this case with non-severe COVID-19, CT showed new-onset fatty changes in the liver along with worsening pneumonia. These indicate that inflammatory cell infiltration of the portal region and hepatic fatty degeneration persist in the recovery phase of non-severe COVID-19 cases without a serious clinical course. Therefore, liver dysfunction with concomitant histological changes in the liver may contribute to disease severity to some extent, but progression to severe COVID-19 illness may be dependent on other factors.
Massive cytokine production is considered to be one of the causes of COVID-19-associated liver injury [4, 5]. As previously reported, systemic symptoms associated with cytokine (IL-6, IL-10, and TNF-α) surge may develop even after the viral load in the host has plummeted, showing a bimodal course of the illness [17, 18]. Despite testing negative for SARS-CoV-2 later on and showing an improvement in symptoms, the present case developed a recurrent fever. A repeat chest CT scan revealed progressing pneumonia accompanied by fluctuating serum IL-6, IL-10, and TNF-α levels (26.4, 8.0, and 31.0 pg/mL, respectively), which are possibly linked to serum hepatobiliary enzyme elevations. Thus, cytokine release after viral elimination could have resulted in liver injury.
Several previous studies had measured serum IL-6, IL-10, and TNF-α concentrations at the onset of acute viral hepatitis. Average serum IL-6, IL-10, and TNF-α levels ranged from 9.0 to 43.0, 7.8 pg/mL, and 10.3 to 44.6 pg/mL in acute hepatitis B, respectively. The analysis of acute hepatitis A, C, and E cases showed that the mean values of IL-6 in the acute phase were 61.6, 26.3, and 15.5 pg/mL, respectively, and those of TNF-α were 52.3, 22.8, and 61.6 pg/mL, respectively. Interestingly, in all the studies, the serum cytokine concentrations were significantly higher in patients with acute hepatitis than in normal participants [19,20,21]. In addition, two reports of Japanese patients with severe acute Epstein–Barr virus or cytomegalovirus infection accompanied by extreme liver dysfunction, described elevated serum IL-6 levels of 7.0 and 10.3 pg/mL, respectively, at the time of admission [22, 23]. These facts indicate that acute hepatic dysfunction associated with viral infection is mediated by the host immune response. Therefore, the cytokines dynamics may also correlate with the development of COVID-19-associated liver injury and affect the severity of SARS-CoV-2 illness [24, 25].
Invasion of novel coronavirus into the liver via the ACE2 receptors expressed in cholangiocytes has also been assumed to cause liver dysfunction in COVID-19 [4, 5]. However, direct viral toxicity is less likely to have contributed to liver dysfunction in this case for two reasons. First, SARS-CoV-2 PCR tests conducted thrice were found to be negative. Second, ACE2 receptors were not expressed in the immunohistochemical study of liver biopsy tissue.
In this patient, both minocycline and favipiravir were initiated on admission, so drug-induced hepatitis is an important differential diagnosis. In general, hepatic and pulmonary damage caused by minocycline is associated with skin rashes and hypereosinophilia [26, 27], but neither was present in this case. Furthermore, concurrent drug-induced hepatic dysfunction, fever, and worsening respiratory symptoms are considered to be extremely rare based on the results of a Japanese multicenter study of COVID-19 patients receiving fabipiravir [28]. Murai et al. reported a case of favipiravir-associated drug-induced liver injury with fever where DLST was positive, unlike in the present case [29]. Thus, in this case of recurrent fever and progressive pneumonia, the likelihood of drug-induced hepatitis due to minocycline and favipiravir is low.
Apart from elevated liver enzymes, other risk factors for COVID-19 severity, such as older age and elevated CRP and LDH, were observed in this case [4, 6, 16]. The patient, however, had moderate disease, which was self-limiting. In addition to the absence of preexisting liver disease, which is reported to correlate with the severity of COVID-19 [30], it is worthwhile to discuss other predictive histological and immunological factors preventing this case from becoming severe.
In addition to systemic inflammation, microvascular thrombosis is hypothesized to induce liver dysfunction in patients with COVID-19 [30,31,32]. Recently, the frequency of circulating platelet aggregates and longitudinal variation of the frequency were reported to be strongly correlated with severity and mortality in patients with COVID-19 [33]. In this case, liver biopsy specimens were obtained after her general condition and liver dysfunction had improved; it showed remnant findings of hepatitis but no evidence of microthrombi. Therefore, microthrombi might not be formed even during the peak of liver dysfunction; or if they did form, they disappeared. This may provide another hint in her not developing severe COVID-19. However, more insight could have been gained by comparing the liver biopsy findings obtained during the extreme phases of the patient`s liver dysfunction and systemic inflammatory response with those of the recovery phase.
Elevated serum cytokines levels and ACE2 expression in the liver should also be mentioned in this case. Using serum samples collected from patients with COVID-19, Del Valle et al. reported that high IL-6 (above cut-offs of 70 pg/mL) and TNF-α (in like manner, 35 pg/mL) levels at the time of hospitalization were independent and significant predictors of disease severity and death [25]. Recently, Li et al. described that IL-6 could be the key cytokine in patients with COVID-19 developing severe liver injury. They also suggested that downregulation of ACE2 from host cells due to endocytosis of SARS-CoV-2 may be the starting point for amplification of serum IL-6 levels, leading to a systemic “cytokine storm” [30]. Hence, the scarce ACE2 expression in the liver and the insufficient cytokine elevation, including IL-6, may have prevented this case from becoming severe.
In this report, we demonstrated histological findings and cytokine levels in a case of non-severe COVID-19 complicated by liver injury. Herein, distinct histologic changes were present despite disease improvement and reduction in cytokine levels with recovery. In patients infected with SARS-CoV-2, a cytokine surge may predict COVID-19-related liver disease.
References
Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–33.
COVID-19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). https://coronavirus.jhu.edu/map.html. Accessed 7 June 2022.
Japan COVID-19 Case Management Guide Review Committee. Clinical management of patients with COVID-19: A guide for front-line healthcare workers. version 7.2; 2022. https://www.mhlw.go.jp/content/000936623.pdf (in Japanese). Accessed 7 June 2022.
Alqahtani SA, Schattenberg JM. Liver injury in COVID-19: the current evidence. Unit Europ Gastroenterol J. 2020;8:509–19.
Jothimani D, Venugopal R, Abedin MF, et al. COVID-19 and the liver. J Hepatol. 2020;73:1231–40.
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–62.
Wang Y, Liu S, Liu H, et al. SARS-CoV-2 infection of the liver directly contributes to hepatic impairment in patients with COVID-19. J Hepatol. 2020;73:807–16.
Wang Q, Zhao H, Liu LG, et al. Pattern of liver injury in adult patients with COVID-19: a retrospective analysis of 105 patients. Mil Med Res. 2020;7:28.
Uchida Y, Uemura H, Yamaba S, et al. Significance of liver dysfunction associated with decreased hepatic CT attenuation values in Japanese patients with severe COVID-19. J Gastroenterol. 2020;55:1098–106.
Mao R, Qiu Y, He JS, et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5:667–78.
Fix OK, Hameed B, Fontana RJ, et al. Clinical best practice advice for hepatology and liver transplant providers during the COVID-19 pandemic: AASLD expert panel consensus statement. Hepatology. 2020;72:287–304.
Cai Q, Huang D, Yu H, et al. COVID-19: abnormal liver function tests. J Hepatol. 2020;73:566–74.
Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–2.
Sonzogni A, Previtali G, Seghezzi M, et al. Liver histopathology in severe COVID 19 respiratory failure is suggestive of vascular alterations. Liver Int. 2020;40:2110–6.
Tahtabasi M, Hosbul T, Karaman E, et al. Frequency of hepatic steatosis and its association with the pneumonia severity score on chest computed tomography in adult COVID-19 patients. World J Crit Care Med. 2021;10:47–57.
Malik P, Patel U, Mehta D, et al. Biomarkers and outcomes of COVID-19 hospitalisations: systematic review and meta-analysis. BMJ EBM. 2021;26:107–8.
Siddiqi HK, Mehra MR. COVID-19 illness in native and immunosuppressed states: a clinical-therapeutic staging proposal. J Heart Lung Trans. 2020;39:405–7.
Cevik M, Kuppalli K, Kindrachuk J, et al. Virology, transmission, and pathogenesis of SARS-CoV-2. BMJ. 2020;371:m3862.
Torre D, Zeroli C, Giola M, et al. Serum levels of interleukin-1 alpha, interleukin-1 beta, interleukin-6, and tumor necrosis factor in patients with acute viral hepatitis. Clin Infect Dis. 1994;18:194–8.
Arya RP, Arankalle VA. Phenotypic analysis of monocytes and CD4(+) T cells in hepatitis E patients with or without pregnancy. Hum Immunol. 2019;80(10):855–62.
Ribeiro CRA, Beghini DG, Lemos AS, et al. Cytokines profile in patients with acute and chronic hepatitis B infection. Microbiol Immunol. 2022;66:31–9.
Sato S, Kawashima H, Oshiro H, et al. Virological and immunological characteristics of a 19 year-old Japanese female with fatal outcome with Epstein-Barr virus-associated hemophagocytic syndrome. J Clin Virol. 2004;31:235–8.
Tetsuka S, Suzuki T, Ogawa T, et al. Encephalopathy associated with severe cytomegalovirus infection in an immunocompetent young woman. Case Rep Infect Dis. 2021;2021:5589739.
Laing AG, Lorenc A, Molino Del Barrio Del I, et al. A dynamic COVID-19 immune signature includes associations with poor prognosis. Nat Med. 2020;26:1623–35.
Del Valle DM, Kim-Schulze S, Huang HH, et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat Med. 2020;26:1636–43.
Dykhuizen RS, Zaidi AM, Godden DJ, et al. Minocycline and pulmonary eosinophilia. BMJ. 1995;310:1520–1.
Grim SA, Romanelli F, Jennings PR, et al. Late-onset drug fever associated with minocycline: case report and review of the literature. Pharmacotherapy. 2003;23:1659–62.
Favipiravir observational study group, Fujita Health University. Favipiravir observational study interim report 4 (as of July 1, 2021); 2021. https://www.kansensho.or.jp/uploads/files/topics/2019ncov/covid19_favip_210701_eng.pdf. Accessed 7 June 2022.
Murai Y, Kawasuji H, Takegoshi Y, et al. A case of COVID-19 diagnosed with favipiravir-induced drug fever based on a positive drug-induced lymphocyte stimulation test. Int J Infect Dis. 2021;106:33–5.
Li D, Ding X, Xie M, et al. COVID-19-associated liver injury: from bedside to bench. J Gastroenterol. 2021;56:218–30.
Tsutsumi T, Saito M, Nagai H, et al. Association of coagulopathy with liver dysfunction in patients with COVID-19. Hepatol Res. 2021;51:227–32.
Kondo R, Kawaguchi N, McConnell MJ, et al. Pathological characteristics of liver sinusoidal thrombosis in COVID-19 patients: a series of 43 cases. Hepatol Res. 2021;51:1000–6.
Nishikawa M, Kanno H, Zhou Y, et al. Massive image-based single-cell profiling reveals high levels of circulating platelet aggregates in patients with COVID-19. Nat Commun. 2021;12:7135.
Acknowledgements
This research was partially supported by AMED under Grant Numbers JP21fk0210077, JP21fk0210047, and JP21fk0210058, JSPS KAKENHI Grant Number 20K16954, and Research Promotion Project 2020 for Novel Coronavirus Infections in Fukui Prefecture. We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human/animal rights
All procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and its later amendments.
Informed consent
Informed consent was obtained from the patient included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Matsuda, H., Nosaka, T., Hiramatsu, K. et al. Histology and cytokine levels in hepatic injury accompanying a case of non-severe COVID-19. Clin J Gastroenterol 16, 270–278 (2023). https://doi.org/10.1007/s12328-023-01755-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-023-01755-4