Abstract
Stomach cancer can occur during chronic inflammation from Helicobacter pylori (HP) infection, and its occurrence can be suppressed by eradication of HP. However, the effects of suppressing stomach cancer by HP eradication are limited, and the cancer is known to recur even after eradication of this infection. Here, we report the case of a 56-year-old male patient with gastric cancer who, although undergoing HP eradication after treatment of early gastric cancer with endoscopy, experienced five metachronous cancer recurrences over a period of 13 years. Whether observation of patients who undergo eradication of HP due to peptic ulcers or chronic gastritis and patients who undergo eradication after endoscopic treatment for early gastric cancer should be performed at the same interval is an issue that must be addressed in the future. The appropriate observation period for each patient must be established while considering the burdens to the patient and from the medical economic perspective.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Eradication of Helicobacter pylori (HP) after endoscopic treatment of early gastric cancer significantly reduces the occurrence of metachronous early gastric cancer [1–3]. In 2010, eradication of HP after endoscopic treatment of early gastric cancer was approved under the Japanese system of health insurance based on results that the onset of metachronous early gastric cancer could be controlled by HP eradication [1]. However, eradication of HP does not completely suppress the occurrence of metachronous gastric cancer, and some cases of recurrence after eradication have been reported [4].
Here, we report the case of a patient experiencing 5 occurrences of metachronous gastric cancer during 13 years of observation after endoscopic treatment of primary early gastric cancer and eradication of HP.
Case report
In 1998, a 56-year-old male was first diagnosed with early stage gastric cancer. In March 1998, his previous doctor removed a Stage IIa early gastric tumor (12 mm) from the lesser curvature of the antrum via endoscopic mucosal resection (EMR). Postoperatively, the patient tested positive for HP infection. Eradication was performed in October 1998 and verified to be successful by HP cultures and microscopy.
The patient underwent periodic check-ups, and no recurrence of gastric cancer or metachronous early gastric cancer was found. Eight years later, in October 2006, a Stage IIa + IIc early gastric tumor (15 mm) was detected at the lesser curvature of the antrum, and a Stage IIa early gastric tumor (10 mm) at the posterior wall of the antrum. They were again removed via EMR by his previous doctor, and were classified as m, tub1, HM0, VM0, ly(−), v(−) according to the histopathology findings.
Since 2007, periodic check-ups have been performed in our hospital, and in October 2009, a Stage IIc early gastric tumor (3 mm) (Fig. 1) was found at the lesser curvature of the antrum. In October 2010, a Stage IIc early gastric tumor (6 mm) (Fig. 2) was found at the posterior wall of the angulus. Both tumors were treated via EMR, and were both classified as m, tub1, HM0, VM0, ly(−), v(−), according to the histopathology findings.
Metachronous early gastric cancer diagnosed in October 2009. a In October 2009, we identified a small red mucosal area near the scar resulting from EMR performed in 2006. b Using NBI, we could observe a minute depressed lesion surrounded by an irregular mucosal pattern that suggested gastric cancer. c We performed EMR for this lesion and extracted a 1-cm specimen on the major axis. d The specimen was diagnosed to be a well-differentiated adenocarcinoma of 3 × 2 mm diameter by pathological examination
Metachronous early gastric cancer diagnosed in October 2010. a In October 2010, we identified a small red mucosa in the posterior wall of the antrum. b NBI examination revealed a minute depressed lesion surrounded by irregular mucosal pattern that suggested minute gastric cancer. c We performed EMR and extracted a 1-cm specimen on the major axis. d The lesion was diagnosed to be a well-differentiated adenocarcinoma of 6 × 5 mm diameter by pathological examination
In March 2011, a Stage IIb early gastric tumor (10 mm) was found at the lesser curvature of the lower gastric body and treated with endoscopic submucosal dissection (ESD) (Fig. 3). Again, the histopathology findings classified the tumor as m, tub1, HM0, VM0, ly(−), v(−), and IM(+), atrophy(+), neutrophil(−), mononuclear cell(+), H. pylori(−) in the background mucosa. The Kimura–Takemoto classification for endoscopic atrophy was O1, and it did not change during the endoscopic follow-up carried out yearly or half-yearly. The endoscopic treatment scars are shown in Fig. 4.
Metachronous early gastric cancer diagnosed in March 2011. a In March 2011, a red mucosa measuring 15 mm in the major axis was detected in the lesser curvature of the lower body and the visible vascular pattern of this area disappeared. b The demarcation line was observed around the lesion and irregular minute vessels on its surface were identified using NBI endoscopy. We diagnosed this lesion as type IIb early gastric cancer. c ESD was performed on this lesion and we identified a 2-cm specimen on the major axis. d Pathological examination revealed the lesion to be a well-differentiated adenocarcinoma measuring 10 × 7 mm
Multiple ulcer scars resulting from endoscopic resections performed between March 1998 and March 2011. a, b The scars after EMR performed for the second and third metachronous cancers in the antrum in 2006 and 2009, respectively. c The scar after EMR performed for the fourth metachronous cancer in the posterior wall of the angulus in 2010. d The scar after ESD performed for the fifth metachronous cancer in the lesser curvature of the middle body in 2011
The urine antibody test performed during follow-up in 2003 and 2006 and the blood antibody and urea breath tests performed in 2011 were negative for HP. Since then, periodic observation with yearly upper endoscopy has been performed, and no new cancerous growths have been found.
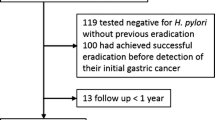
Figure 5 shows the occurrences of cancer during the 13-year follow-up period, and Fig. 6 shows the locations of all the lesions.
Relevant occurrences during the 13-year follow-up period. The red arrow shows the time of eradication of H. pylori. The white arrows show the detection times of each instance of early gastric cancer. The black arrows show the times and methods of examination of H. pylori infection during the follow-up period
The patient was a moderate drinker, but stopped drinking after he suffered from a head injury in a traffic accident in 2003. He is a non-smoker, does not take medicines regularly, and avoids salty foods. Except for his mother who had early gastric cancer, he had no family history of malignant disease.
Discussion
In 1984, Marshall and Warren were able to isolate a culture of HP from a patient with chronic gastritis [5], and confirmed that HP infection is indeed the cause of various gastric illnesses, which are now understood to be infections. As a result, eradication of HP became the first choice of treatment for several many gastric illnesses. At first, eradication of HP was performed mainly for patients with peptic ulcers to prevent a relapse of the ulcers [6]. Uemura et al. indicated that gastric cancer rarely occurs in the stomach in the absence of HP infection, and that an infected stomach has a higher occurrence of gastric cancer during the course of observation [7]. Since then, eradication of HP has been extensively examined for the prevention of metachronous gastric cancer in patients who have undergone endoscopic treatment for early gastric cancer.
In 2008, Fukase et al. conducted a multi-institutional joint research to examine the effects of HP eradication on metachronous gastric cancer for patients who had undergone endoscopic treatment for early gastric cancer. They found a significant difference in the occurrence of metachronous gastric cancer between the eradicated and uneradicated groups, and showed that the risk of metachronous gastric cancer was reduced by up to one-third by HP eradication [1].
Based on these reports, eradication of HP has been recommended since 2009 for the diagnosis and treatment of HP-positive patients who have undergone endoscopic treatment of early gastric cancer; eradication of HP is now performed more actively from this perspective. However, even when eradication of HP is successful, the occurrence of metachronous gastric cancer cannot be completely prevented [2, 3].
Metachronous gastric cancer first occurred in our patient after a relatively long period, i.e., 8 years after the initial eradication, and the patient subsequently developed additional metachronous gastric tumors at 11, 12, and 13 years after eradication. These metachronous gastric cancers were found at very early stages; the tumors found at 11 and 12 years post-HP eradication were minute, i.e., barely detectable by magnifying endoscopy combined with narrow band imaging (NBI). Therefore, it is unlikely that these metachronous gastric tumors developed simultaneously with the first gastric cancer or immediately after the eradication of HP, and we speculate instead that they developed on the gastric mucosa from where the HP infection was removed at a later time point.
Some reports mention that the occurrence rate of metachronous gastric cancer does not decrease after HP eradication [8, 9], whereas the results of other studies indicate that the rate of occurrence is indeed decreased, with the decrease ranging from 1.5 % [10] to 14.6 % [11]. Thus, the types of cases that develop gastric cancer after eradication of HP and their differences from those that do not, are topics that need further investigation.
Take et al. [4] divided patients with peptic ulcers into 3 groups according to the levels of gastric mucosal atrophy and compared the rate of gastric cancer recurrence after eradication of HP in each group. Interestingly, they found that stronger levels of atrophy correlated with a more frequent occurrence of gastric cancer. For the examination of HP eradication after endoscopic treatment of early gastric cancer, Chon et al. [12] compared patients who developed metachronous atypical epithelium and those who did not. They found a significant difference in the degree of intestinal metaplasia on the gastric mucosa between the groups, and hence suspected that the degree of intestinal metaplasia, i.e., the level of gastric mucosal atrophy, affected the development of metachronous gastric cancer after HP eradication. Maehata et al. [13] also examined potential factors related to the development of metachronous gastric cancer after eradication of HP using multivariate analysis and indicated that an observation period of >5 years and a high level of mucosal atrophy were independent factors for metachronous gastric cancer occurrence.
Based on these studies, we believe that the development of gastric cancer after eradication of HP appears to be influenced largely by the presence and degree of gastric mucosal atrophy at the time of HP eradication, and regular observation after eradication should therefore be considered. Even though in this case the degree of intestinal metaplasia of the resected specimen by ESD was not remarkable, endoscopic atrophy already existed in the area of the fundic gland when the first lesion was found and the degree of atrophy did not change during the observation period. Thus, mucosal atrophy was identified as an important marker for metachronous gastric cancer. However, whether observation of patients who undergo HP eradication for peptic ulcers or chronic gastritis and patients who undergo eradication after endoscopic treatment for early gastric cancer should be performed at the same interval is an issue that must be addressed in the future. The appropriate observation period for each patient must be established while considering the burdens to the patient and from the medical economic perspective.
Watari et al. [14] indicated that patients with gastric cancer who developed metachronous gastric cancer after eradication of HP showed higher rates of microsatellite instability and a colonic phenotype (Das-1 protein expression), which are biomarkers for intestinal metaplasia. Hence, they pointed out that cases with intestinal metaplasia after eradication of HP may have a higher risk of developing metachronous gastric cancer.
In Japan, the treatment to eradicate HP for HP-related chronic gastritis, which affects a high proportion of the population, has been covered by health insurance since February 2013. Therefore, we suspect that the number of reported cases undergoing HP eradication has increased drastically since this time. In the future, it will be necessary to investigate whether patients undergoing HP eradication due to peptic ulcers or chronic gastritis and after the treatment of early gastric cancer, should be observed at the same intervals and to determine the appropriate length of long-term observation. Thereafter, it will be necessary to develop a useful clinical index to set up an appropriate observation interval for each case.
References
Fukase K, Kato M, Kikuchi S, Japan Gast Study Group, et al. Effect of eradication of Helicobacter pylori on incidence of metachronous gastric carcinoma after endoscopic resection of early gastric cancer: an open-label, randomised controlled trial. Lancet. 2008;372:392–7.
Seo JY, Lee DH, Cho Y, et al. Eradication of Helicobacter pylori reduces metachronous gastric cancer after endoscopic resection of early gastric cancer. Hepatogastroenterology. 2013;60:776–80.
Kwon YH, Heo J, Lee HS, et al. Failure of Helicobacter eradication and age are independent risk factors for recurrent neoplasia after endoscopic resection of early gastric cancer in 283 patients. Aliment Pharmacol Ther. 2014;39:609–18.
Take S, Mizuno M, Ishiki K, et al. The long-term risk of gastric cancer after the successful eradication of Helicobacter pylori. J Gastroenterol. 2011;46:318–24.
Marshall BJ, Warren JR. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet. 1984;1:1311–5.
Miyamoto M, Haruma K. Gastric ulcer and duodenal ulcer. Nihon Rinsho. 2013;71:1418–23.
Uemura N, Okamoto S, Yamamoto S, et al. Helicobacter pylori infection and the development of gastric cancer. N Engl J Med. 2001;345:784–9.
Choi J, Kim SG, Yoon H, et al. Eradication of Helicobacter pylori after endoscopic resection of gastric tumors does not reduce incidence of metachronous gastric carcinoma. Clin Gastroenterol Hepatol. 2014;12:793–800.
Kato M, Nishida T, Yamamoto K, et al. Scheduled endoscopic surveillance controls secondary cancer after curative endoscopic resection for early gastric cancer: a multicentre retrospective cohort study by Osaka University ESD study group. Gut. 2013;62:1425–32.
Bae SE, Jung HY, Kang J, et al. Effect of Helicobacter pylori eradication on metachronous recurrence after endoscopic resection of gastric neoplasm. Am J Gastroenterol. 2014;109:60–7.
Hanaoka N, Ueda N, Shiotani A, et al. Autofluorescence imaging for predicting development of metachronous gastric cancer after Helicobacter pylori eradication. J Gastroenterol Hepatol. 2010;25:1844–9.
Chon I, Choi C, Shin CM, et al. Effect of Helicobacter pylori eradication on subsequent dysplasia development after endoscopic resection of gastric dysplasia. Korean J Gastroenterol. 2013;61:307–12.
Maehata Y, Nakamura S, Fujisawa K, et al. Long-term effect of Helicobacter pylori eradication on the development of metachronous gastric cancer after endoscopic resection of early gastric cancer. Gastrointest Endosc. 2012;75:39–46.
Watari J, Moriichi K, Tanabe H, et al. Biomarkers predicting development of metachronous gastric cancer after endoscopic resection: an analysis of molecular pathology of Helicobacter pylori eradication. Int J Cancer. 2012;130:2349–58.
Disclosures
Conflict of Interest
Atsushi Mitsunaga, Tomoko Tagata, Tetsuya Hamano, Honami Teramoto, Motoyasu Kan, Yutaka Mitsunaga, Maki Tobari, Izumi Shirato, Miho Shirato, Shuhei Yoshida, Masahiko Shimada, and Takayoshi Nishino declare that they have no conflict of interest.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008(5).
Informed Consent
Informed consent was obtained from the patient for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Mitsunaga, A., Tagata, T., Hamano, T. et al. Metachronous early gastric cancer over a period of 13 years after eradication of Helicobacter pylori . Clin J Gastroenterol 7, 490–495 (2014). https://doi.org/10.1007/s12328-014-0536-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-014-0536-9