Abstract
Introduction
The cardiovascular disease risk reduction benefits of proprotein convertase subtilisin/kexin type 9 inhibitor monoclonal antibodies (PCSK9i mAb) and ezetimibe are dependent on remaining on treatment and being persistent and adherent. We estimated the percentage of patients on therapy, persistent and adherent at 182 and 365 days among US adults with health insurance who initiated a PCSK9i mAb (n = 16,588) or ezetimibe (n = 83,086) between July 2015 and December 2019.
Methods
Using pharmacy fill claims, being on therapy was defined as having a day of medication supply in the last 60 of 182 and 365 days following treatment initiation, being persistent was defined as not having a gap of 60 days or more between the last day of supply from one prescription fill and the next fill, and being adherent was defined by having medication available to take on ≥ 80% of the 182 and 365 days following treatment initiation. We estimated multivariable-adjusted risk ratios for being persistent and adherent comparing patients initiating PCSK9i mAb versus ezetimibe using Poisson regression.
Results
At 182 days following initiation, 80% and 68% were on therapy and 76% and 64% were persistent among patients who initiated a PCSK9i mAb and ezetimibe, respectively. Among patients who were on therapy and persistent at 182 days following initiation, 88% and 81% of those who initiated a PCSK9i mAb and ezetimibe, respectively, were on therapy at 365 days. Among those on therapy and persistent at 182 days following initiation, being persistent and being adherent at 365 days were each more common among PCSK9i mAb versus ezetimibe initiators (persistent: 82% versus 76%, multivariable-adjusted risk ratio 1.07; 95% confidence interval [CI] 1.06–1.08; adherent: 74% versus 71%, multivariable-adjusted risk ratio 1.02; 95% CI 1.01–1.03).
Conclusions
These data suggest approaches to increase persistence and adherence to PCSK9i mAb and ezetimibe should be implemented prior to or within 182 days following treatment initiation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitor monoclonal antibodies and ezetimibe reduce the risk for atherosclerotic cardiovascular disease events. |
The effectiveness of these medications is related to being on treatment, persistent and adherent. |
This study evaluated being on treatment, persistent and adherent to PCSK9 inhibitor monoclonal antibodies and ezetimibe at 182 and 365 days following initiation. |
What was learned from the study? |
A higher percentage of patients initiating a PCSK9 inhibitor monoclonal antibody versus ezetimibe were on treatment, persistent and adherent. |
Among patients who were persistent for the first 182 days following treatment initiation, a high percentage remained on therapy, persistent and adherent at 365 days following treatment initiation. |
It may be beneficial to apply interventions to increase the percentage of patients that remain on therapy, persistent and adherent prior to or within 182 days following initiating PCSK9 inhibitor monoclonal antibodies and ezetimibe. |
Introduction
In randomized controlled trials, proprotein convertase subtilisin/kexin type 9 inhibitor monoclonal antibodies (PCSK9i mAb) and ezetimibe each lowered low-density lipoprotein cholesterol (LDL-C) and reduced the risk for atherosclerotic cardiovascular disease (ASCVD) events [1,2,3]. In these and other trials, PCSK9i mAb and ezetimibe were well tolerated; the occurrence of side effects was low, with < 7% of participants having discontinued treatment annually [1,2,3,4,5]. The effectiveness of lipid-lowering medications is related to remaining on treatment and being persistent and adherent [6,7,8]. Documenting the percentage of patients who remain on treatment, persistent and adherent following initiation of PCSK9i mAb or ezetimibe can inform the need for interventions to improve access to these medications and medication-taking behaviors.
We compared the percentage of patients on therapy, persistent and adherent at 182 and 365 days following the initiation of a PCSK9i mAb versus ezetimibe. Additionally, to inform when to apply interventions to improve medication-taking behaviors, we estimated the percentage of patients on therapy, persistent and adherent at 365 days following the initiation among those who were persistent at 182 days following initiation. We studied PCSK9i mAb and ezetimibe because the 2018 American Heart Association/American College of Cardiology (AHA/ACC/Multisociety) cholesterol guideline and the 2022 ACC Expert Consensus Decision Pathway recommend these medications as adjunct treatment for patients at very high risk for ASCVD events, taking a statin or with statin associated side effects, and whose LDL-C is ≥ 70 mg/dl and ≥ 55 mg/dl, respectively [9, 10].
Methods
Administrative data from the Truven Health MarketScan Research Database and Medicare were analyzed in the current study. The MarketScan Research Database contains information for people in the US with commercial and Medicare supplementary health insurance. Medicare is a government program that provides health insurance for US adults ≥ 65 years of age and younger adults with end-stage kidney disease or who are disabled. For the current analysis, we used data from the Marketscan database, a 5% random sample of all Medicare beneficiaries (i.e., 5% Medicare sample) and all Medicare beneficiaries ≥ 65 years of age hospitalized for myocardial infarction (MI) with pharmacy benefits (i.e., 100% Medicare MI sample). Approval for this analysis was obtained from the Institutional Review Board at the University of Alabama at Birmingham. All data used in this analysis were collected as part of routine medical care. The requirement to obtain informed consent for this analysis of de-identified data was waived by the Institutional Review Board at the University of Alabama at Birmingham. Marketscan data were licensed from International Business Machines Corporation (Armonk, NY), and Medicare data were licensed from the US Centers for Medicare and Medicaid Services (CMS) Chronic Conditions Warehouse.
We identified adults in the Marketscan database and all Medicare beneficiaries ≥ 65 years of age hospitalized for MI who had a pharmacy claim for a PCSK9i mAb fill or ezetimibe between July 1, 2015, and December 31, 2019. From the 5% Medicare sample, we identified adults who had a pharmacy claim for a PCSK9i mAb or ezetimibe between July 1, 2015, and December 31, 2018. The date of each participant’s first PCSK9i mAb or ezetimibe fill was used as their index date.
We restricted the Marketscan sample to patients 21–64 years of age on their index date and the Medicare samples to those who were ≥ 65 years of age 365 days prior to their index date. These age restrictions were applied because almost all Medicare beneficiaries are ≥ 65 years of age, and this would allow us to avoid including the same patient from both the Marketscan and Medicare databases. Also, patients in the 5% Medicare sample with a history of MI before their index date were excluded as they were included in the 100% Medicare MI sample. Patients in the 100% Medicare MI sample without an MI before their index date were excluded because they may be included in the 5% Medicare sample. To provide adequate time prior to the first PCSK9i mAb and ezetimibe fill to identify patient characteristics, we restricted the analyses to patients who lived in the US and had continuous fee-for-service inpatient, outpatient and pharmacy coverage for the 365 days prior to their index date. To evaluate the outcomes of being on therapy, persistent and adherent, we required patients to have pharmacy insurance coverage for the 365 days following their index date.
Outcomes
We assessed three outcomes for PCSK9i mAb and ezetimibe separately, including the percentage of patients on therapy, persistent and adherent (Fig. 1). These outcomes were evaluated at two times: 182 and 365 days following treatment initiation. The percentage on therapy was defined as having at least 1 day of supply in the last 60 days of the follow-up period (i.e., from day 123 to 182 and from day 306 to 365). Being persistent was defined as not having a gap of ≥ 60 days between the last day of supply for a medication and the next pharmacy fill of that medication [11,12,13]. Adherence was estimated using the proportion of days covered (PDC), which was calculated as the percentage of days for which the patient had a day of supply for a PCSK9i mAb and ezetimibe, separately. Being adherent was defined as having medication available to take on ≥ 80% of days during the follow-up period (i.e., PDC ≥ 80%) [14].
Patient Characteristics
Demographic factors obtained from administrative Marketscan and Medicare computer files included age, sex and region of residence. Information on race and ethnicity was not available in Marketscan. Therefore, we did not include race and ethnicity as variables in the analyses. Additional factors identified using administrative claims included calendar period that PCSK9i mAb and ezetimibe were initiated, smoking, diabetes, chronic kidney disease, heart failure, history of ASCVD, having a myocardial infarction or ischemic stroke in the past year, history of peripheral artery disease, history of coronary heart disease, depression, statin use, non-statin lipid-lowering medication use, polypharmacy and a prior visit to a cardiologist. Among patients taking a statin, we assessed being adherent in the past year and statin intolerance. The definitions for these variables are provided in Supplementary Materials Table S1. Very high ASCVD risk was defined by a history of two or more major ASCVD events or a history of one major ASCVD event with the presence of two or more high-risk conditions [10, 15].
Statistical Analysis
Summary statistics for patient characteristics among those initiating PCSK9i mAb and ezetimibe, separately, were estimated as percentages for the overall population and for patients in the Medicare and Marketscan databases, separately. The percentage on therapy and persistent, on therapy but not persistent and not on therapy was estimated at 182 days and 365 days following treatment initiation. We estimated the mean PDC at 182 and 365 days following initiation of a PCSK9i mAb and ezetimibe. The percentages that were on therapy, persistent and adherent were estimated at 182 and 365 days following initiation of a PCSK9i mAb or ezetimibe with the statistical significance of differences between those initiating PCSK9i mAb and ezetimibe determined using chi-square tests. We used multivariable-adjusted Poisson regression models with robust variance estimates to calculate the risk ratios for remaining on therapy and being persistent and adherent between those who initiated a PCSK9i mAb versus ezetimibe at 182 days and 365 days following treatment initiation. Initial models included adjustment for calendar period of initiation, age and sex (Model 1). A second level of adjustment included calendar period of treatment initiation, age, sex, region of residence, smoking, diabetes, chronic kidney disease, heart failure, having a history of ASCVD, depression, statin use, statin adherence among those taking a statin, statin intolerance, non-statin lipid-lowering medication use, polypharmacy and having a prior visit to a cardiologist (Model 2). All analyses that assessed outcomes at 365 days following treatment initiation were conducted for the overall population and among those who were persistent at 182 days and 365 days following treatment initiation. In a sensitivity analysis, the percentages of patients that were on therapy, persistent and adherent and risk ratios were estimated after excluding patients who initiated ezetimibe and then a PCSK9i mAb (n = 2944), a PCSK9i mAb and then ezetimibe (n = 477) or ezetimibe and a PCSK9i mAb on the same day (n = 4).
Guidelines and consensus statements recommend initiation of a PCSK9i mAb or ezetimibe for patients with a very high risk of recurrent events and whose LDL-C is ≥ 70 mg/dl and ≥ 55 mg/dl while taking a maximally tolerated statin [9, 10]. Therefore, we estimated the percentage of patients and risk ratios for being on therapy, persistent and adherent associated with initiating a PCSK9i mAb versus ezetimibe among those at very high ASCVD risk and not at very high risk, separately. Risk ratios were calculated with the second level of adjustment described above with differences in the risk ratios for those with and without very high ASCVD risk, in the Marketscan and Medicare databases, and for women and men, separately, assessed using multiplicative interaction terms. LDL-C levels were not available in the Marketscan or Medicare databases. Analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC).
Results
Overall, 16,588 patients initiated a PCSK9i mAb and 83,086 patients initiated ezetimibe and met the inclusion criteria (Supplementary Materials Fig. S1). Patients who initiated both a PCSK9i mAb and ezetimibe (n = 3125) were included in both groups. Compared to patients who initiated ezetimibe, those who initiated a PCSK9i mAb were older; more likely to have a history of ASCVD, a history of coronary heart disease (CHD) and very high ASCVD risk; to not be taking a statin; to be taking a non-statin lipid-lowering medication; to be on polypharmacy and to have a cardiologist visit in the year before treatment initiation (Table 1). Among patients who were taking a statin in the year prior to treatment initiation, those initiating a PCSK9i mAb were less likely to be adherent to this medication compared with their counterparts initiating ezetimibe. Characteristics of patients who initiated a PCSK9i mAb and ezetimibe for Medicare beneficiaries and those in the Marketscan database, separately, are shown in Supplementary Materials Table S2.
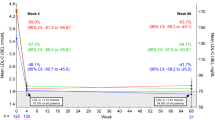
At 182 days following initiation of a PCSK9i mAb and ezetimibe, 76% and 64% of patients, respectively, were on therapy and persistent (Fig. 2). At 365 days following initiation of PCSK9i mAb and ezetimibe, 62% and 48% of patients, respectively, were on therapy and persistent. Among patients who were persistent to their treatment at 182 days following initiation, 82% and 75% of those who initiated a PCSK9i mAb and ezetimibe, respectively, were on therapy at 365 days. At 182 and 365 days following treatment initiation, 4% and 10% of those initiating a PCSK9i mAb, respectively, and 4% and 11% of those initiating ezetimibe, respectively, were on treatment but not persistent (i.e., had a gap of ≥ 60 days without medication available to take but with medication available in the last 60 days of the follow-up period). Among patients who were persistent at 182 days, 82%, 5% and 12% of those who initiated PCSK9i mAb and 75%, 6% and 19% of those who initiated ezetimibe were on therapy and persistent, on therapy but not persistent and not on therapy at 365 days, respectively.
The mean PDC for patients initiating a PCSK9i mAb and ezetimibe was 0.77 and 0.72 at 182 days, respectively, and 0.71 and 0.63 at 365 days, respectively. At 182 and 365 days following treatment initiation, higher percentages of patients initiating a PCSK9i mAb versus ezetimibe were on therapy, persistent and adherent (Table 2). Among patients who were persistent at 182 days following treatment initiation, those who initiated a PCSK9i mAb were more likely to be on therapy, persistent and adherent at 365 days following treatment initiation. After multivariable adjustment, the risk ratio for being on therapy, persistent and adherent comparing patients initiating a PCSK9i mAb versus ezetimibe was 1.15 (95% CI 1.14, 1.16), 1.15 (95% CI 1.14, 1.17) and 1.07 (95% CI 1.05, 1.08) at 182 days, respectively, and 1.20 (95% CI 1.18, 1.21), 1.22 (95% CI 1.20, 1.24) and 1.16 (95% CI 1.14, 1.18) at 365 days, respectively (Table 3). Among patients who were persistent for 182 days following treatment initiation, those who had initiated a PCSK9i mAb were more likely to be on therapy (risk ratio 1.07; 95% CI 1.06–1.08), persistent (risk ratio 1.07; 95% CI 1.06–1.08) and adherent (risk ratio 1.02; 95% CI 1.01–1.03) at 365 days following treatment initiation. Among patients who were persistent for 365 days following treatment initiation, those who had initiated a PCSK9i mAb were less likely than those who initiated ezetimibe to be adherent at 365 days following treatment initiation (risk ratio 0.96; 95% CI 0.95–0.97). Results after excluding patients who initiated both a PCSK9i mAb and ezetimibe are provided in Supplementary Materials Tables S3 and S4. The percentage of patients who initiated a PCSK9i mAb and ezetimibe, separately, that were on treatment, persistent and adherent are provided for those with and without very high ASCVD risk in Supplementary Materials Table S5, in the Marketscan and Medicare databases in Supplementary Materials Table S6 and for women and men in Supplementary Materials Table S7 with multivariable adjusted risk ratios provided in Supplementary Materials Tables S8, S9 and S10 by very high ASCVD risk, database and sex, respectively.
Being on a PCSK9i mAb at 182 and 365 days following treatment initiation was more common among men versus women, patients taking a low or moderate statin versus no statin, with high statin adherence, taking non-statin lipid-lowering therapy prior to PCSK9i mAb initiation and with a prior cardiologist visit and was less common for patients who were 65–74 and ≥ 75 versus 18 to 54 years of age (Supplementary Materials Table S11). Being on ezetimibe at 182 and 365 days following treatment initiation was more common for those who initiated treatment after versus before June 2016, among men, for those with depression, taking a high-intensity statin, with high statin adherence and taking non-statin lipid-lowering therapy prior to ezetimibe initiation while it was less common among those with statin intolerance. Factors associated with being persistent and adherent with PCSK9i mAb and ezetimibe are shown in Supplementary Materials Tables S12 and S13.
Discussion
In the current study, a high percentage of patients initiating PCSK9i mAb or ezetimibe were on therapy at 182 and 365 days following treatment initiation. Additionally, almost all patients who were on therapy were persistent to their treatment. A high percentage of patients who were persistent to a PCSK9i mAb or ezetimibe for the initial 182 days following initiation were on therapy, persistent and adherent at 365 days following treatment initiation. Furthermore, being on therapy, persistent or adherent was each more common at 365 days for patients initiating a PCSK9i mAb compared with ezetimibe.
Extensive data support the LDL-C lowering benefit of PCSK9i mAb and ezetimibe. In a network meta-analysis including 48 randomized trials, PCSK9i mAb lowered LDL-C an average of 57–62% and ezetimibe lowered LDL-C by 25% [16]. Additionally, a meta-analysis of 12 randomized trials reported a reduction in major adverse cardiovascular events with PCSK9i mAb (risk ratio 0.83, 95% CI 0.79–0.87) and a number needed to treat of 36 [17]. A Cochrane review of 26 randomized trials found ezetimibe reduced the risk for major adverse cardiovascular events by 6% (risk ratio 0.94; 95% CI 0.90–0.98) [4]. Taken together, these data strongly support the benefit for PCSK9i mAb and ezetimibe for LDL-C lowering and ASCVD risk reduction.
Both PCSK9i mAb and ezetimibe are well tolerated with few side effects [18]. However, persistence to these medications was lower in the current study of real-world data compared to prior randomized trials [1, 2, 5]. Several modifiable factors were associated with being on therapy, persistent and adherent to both PCSK9i mAb and ezetimibe. Being adherent to one drug has predicted being persistent and adherent to subsequently prescribed medications in prior studies [19, 20]. Similarly, in this study, being adherent to a statin prior to initiating a PCSK9i mAb or ezetimibe was associated with both being persistent and adherent to PCSK9i mAb and ezetimibe, respectively. Additionally, taking statins and other non-statin lipid-lowering medications was associated with being persistent and adherent to PCSK9i mAb and ezetimibe. Therefore, patients who are naïve or not adherent to other lipid-lowering therapy may benefit from guidance to increase their likelihood of being adherent to PCSK9i mAb and ezetimibe. Patients who had a visit to a cardiologist prior to initiating a PCSK9i mAb or ezetimibe were more likely to be on therapy and persistent and adherent at 182 days and 365 days. This finding is consistent with prior studies showing cardiology visits being associated with better adherence to statins [21, 22].
Consistent with a prior study, patients with Medicare health insurance were less likely to be persistent to PCSK9i mAb compared with their counterparts with commercial health insurance at 182 and 365 days following treatment initiation [23]. However, among those persistent at 182 days following treatment initiation, a similar percentage of patients with Medicare insurance and commercial insurance in the Marketscan database were on therapy, persistent and adherent at 365 days following initiation. Non-clinical factors including pharmacy type and pharmacy benefit managers may contribute to PCSK9i mAb persistence and adherence among Medicare beneficiaries initiating treatment.
A few prior studies have reported adherence to PCSK9i mAb and ezetimibe in real-world settings. In a study of 13,151 US adults with health insurance initiating a PCSK9i mAb in January to June 2016, 57.4% and 48.9% were persistent and adherent in the 182 days following treatment initiation [23]. In contrast, a study from Canada reported 92% of patients (n = 131) were persistent 12 months after initiating a PCSK9i mAb [24]. The high percentage of patients who were persistent may be related to pharmacy benefits; only 5% of patients noted reimbursement as a reason for discontinuation. Being persistent and adherent is important for ASCVD risk reduction. Not being adherent can lead to higher intra-individual fluctuations in LDL-C, which has been associated with increased ASCVD risk [25].
Prior studies of prevalent users of PCSK9i mAb and ezetimibe have found a high percentage remain on treatment, persistent and adherent. For example, over 90% of patients in the GOULD and HEYMANS studies were persistent to their PCSK9i mAb over ≥ 2 year follow-up [26, 27]. These data suggest the initial 182 days of PCSK9i mAb and ezetimibe treatment may be an important period to implement interventions to increase long-term persistence and adherence. In a clinic that used a pharmacist and a physician assistant, a specialty pharmacy and follow-up visits with a physician assistant, 92.7% of patients initiating a PCSK9i mAb successfully continued treatment for 1 year [28]. This may be an efficient approach to increase persistence and adherence to PCSK9i mAb and ezetimibe.
Being on treatment, persistent and adherent at 182 and 365 days following treatment initiation was more common among patients initiating PCSK9i mAb versus ezetimibe. Reasons for these differences may include the less frequent dosing schedule of PCSK9i mAb versus ezetimibe. A systematic review of real-world data on adults with osteoporosis taking bisphosphonates indicate that weekly versus daily dosing is associated with a higher likelihood of being persistent [29]. Additionally, the LDL-C and ASCVD risk reduction with PCSK9i mAb is substantially larger than for ezetimibe [30, 31]. Informing patients of the large benefit of PCSK9i mAb may contribute to increased persistence and adherence [32, 33]. This is particularly relevant for patients with very high ASCVD risk, a population that had modestly lower persistence and adherence in the current study and that should achieve a large absolute risk reduction with intensive lipid-lowering therapy [15].
A major strength of the current study is the inclusion of a large sample of US adults who initiated a PCSK9i mAb or ezetimibe. Additional strengths include the availability of data for individuals with commercial and government health insurance and longitudinal data that allowed for the definition of patient characteristics prior to the initiation of PCSK9i mAb or ezetimibe and for follow-up to assess on therapy, persistence and adherence. Despite these strengths, the results of the current study should be interpreted in the context of its potential and known limitations. Being on therapy, persistent and adherent was determined only by filled prescriptions. We were unable to confirm whether patients took their medication or if medication was prescribed but not filled. Prior studies have documented challenges that patients have in receiving approval from their insurance company to fill a PCSK9i mAb and high co-payments. We do not know if these challenges were present in the current study and, if present, whether they contributed to the lack of persistence or adherence in some patients. LDL-C levels and physician notes were not available. Some patients may have stopped their PCSK9i mAb or ezetimibe treatment based on their LDL-C level and physician’s advice. We do not know if patients were counseled on the importance of medication persistence and adherence, which could be used to facilitate persistence and adherence. Data were not available for US adults without health insurance or for populations outside of the US. Finally, being on therapy, persistent and adherent was only available for 1 year following treatment initiation. While there was only a small decline from 182 to 365 days following treatment initiation, being on therapy, persistent and adherent was not assessed over a longer time horizon.
Conclusions
The majority of patients initiating PCSK9i mAb were on therapy at 182 and 365 days following treatment initiation with only a small decline in the percentage of patients taking PCSK9i mAb from 182 to 365 days following treatment initiation. Additionally, a higher percentage of patients initiating PCSK9i mAb versus ezetimibe were on therapy, persistent and adherent at 182 and 365 days following treatment initiation. These data suggest approaches to increase persistence and adherence to PCSK9i mAb and ezetimibe should be implemented prior to or within 182 days following treatment initiation. Interventions may include informing patients of the ASCVD risk reduction benefits of PCSK9i mAb and team-based care including a physician assistant, nurse practitioner or pharmacist conducting follow-up visits to promote being on therapy, persistent and adherent.
Data Availability
The datasets analyzed during the current study are not publicly available as they were licensed from ResDAC (Medicare) and Truven Health (Marketscan). Individuals interested in accessing Medicare and Marketscan data can contact ResDAC (https://resdac.org/) or Merative, which acquired Truven Health (https://www.merative.com/).
References
Cannon CP, Blazing MA, Giugliano RP, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372(25):2387–97. https://doi.org/10.1056/NEJMoa1410489.
Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376(18):1713–22. https://doi.org/10.1056/NEJMoa1615664.
Schwartz GG, Steg PG, Szarek M, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018;379(22):2097–107. https://doi.org/10.1056/NEJMoa1801174.
Zhan S, Tang M, Liu F, et al. Ezetimibe for the prevention of cardiovascular disease and all-cause mortality events. Cochrane Database Syst Rev. 2018;11(11):CD012502. https://doi.org/10.1002/14651858.CD012502.pub2.
Sabatine MS. PCSK9 inhibitors: clinical evidence and implementation. Nat Rev Cardiol. 2019;16(3):155–65. https://doi.org/10.1038/s41569-018-0107-8.
Vupputuri S, Joski PJ, Kilpatrick R, et al. LDL cholesterol response and statin adherence among high-risk patients initiating treatment. Am J Manag Care. 2016;22(3):e106–15.
Vodonos A, Ostapenko I, Toledano R, et al. Statin adherence and LDL cholesterol levels. Should we assess adherence prior to statin upgrade? Eur J Intern Med. 2015;26(4):268–72. https://doi.org/10.1016/j.ejim.2015.02.014.
Rodriguez F, Maron DJ, Knowles JW, et al. Association of Statin adherence with mortality in patients with atherosclerotic cardiovascular disease. JAMA Cardiol. 2019;4(3):206–13. https://doi.org/10.1001/jamacardio.2018.4936.
Writing Committee, Lloyd-Jones DM, Morris PB, et al. 2022 ACC expert consensus decision pathway on the role of nonstatin therapies for LDL-cholesterol lowering in the management of atherosclerotic cardiovascular disease risk: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022;80(14):1366–418. https://doi.org/10.1016/j.jacc.2022.07.006.
Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73(24):3168–209. https://doi.org/10.1016/j.jacc.2018.11.002.
Cramer JA, Roy A, Burrell A, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11(1):44–7. https://doi.org/10.1111/j.1524-4733.2007.00213.x.
Booth JN 3rd, Colantonio LD, Chen L, et al. Statin discontinuation, reinitiation, and persistence patterns among medicare beneficiaries after myocardial infarction: a cohort study. Circ Cardiovasc Qual Outcomes. 2017;10(10): e003626. https://doi.org/10.1161/CIRCOUTCOMES.117.003626.
Booth JN 3rd, Colantonio LD, Rosenson RS, et al. Healthcare utilization and statin re-initiation among medicare beneficiaries with a history of myocardial infarction. J Am Heart Assoc. 2018;7(10): e008462. https://doi.org/10.1161/JAHA.117.008462.
Raebel MA, Schmittdiel J, Karter AJ, Konieczny JL, Steiner JF. Standardizing terminology and definitions of medication adherence and persistence in research employing electronic databases. Med Care. 2013;51(8 Suppl 3):S11-21. https://doi.org/10.1097/MLR.0b013e31829b1d2a.
Colantonio LD, Shannon ED, Orroth KK, et al. Ischemic event rates in very-high-risk adults. J Am Coll Cardiol. 2019;74(20):2496–507. https://doi.org/10.1016/j.jacc.2019.09.025.
Toth PP, Bray S, Villa G, et al. Network meta-analysis of randomized trials evaluating the comparative efficacy of lipid-lowering therapies added to maximally tolerated statins for the reduction of low-density lipoprotein cholesterol. J Am Heart Assoc. 2022;11(18): e025551. https://doi.org/10.1161/JAHA.122.025551.
Wang HF, Mao YC, Xu XY, et al. Effect of alirocumab and evolocumab on all-cause mortality and major cardiovascular events: a meta-analysis focusing on the number needed to treat. Front Cardiovasc Med. 2022;9:1016802. https://doi.org/10.3389/fcvm.2022.1016802.
Choi HD, Kim JH. An updated meta-analysis for safety evaluation of alirocumab and evolocumab as PCSK9 inhibitors. Cardiovasc Ther. 2023;2023:7362551. https://doi.org/10.1155/2023/7362551.
Muntner P, Yun H, Sharma P, et al. Ability of low antihypertensive medication adherence to predict statin discontinuation and low statin adherence in patients initiating treatment after a coronary event. Am J Cardiol. 2014;114(6):826–31. https://doi.org/10.1016/j.amjcard.2014.06.009.
Muntner P, Mann DM, Woodward M, et al. Predictors of low clopidogrel adherence following percutaneous coronary intervention. Am J Cardiol. 2011;108(6):822–7. https://doi.org/10.1016/j.amjcard.2011.04.034.
Colantonio LD, Huang L, Monda KL, et al. Adherence to high-intensity statins following a myocardial infarction hospitalization among medicare beneficiaries. JAMA Cardiol. 2017;2(8):890–5. https://doi.org/10.1001/jamacardio.2017.0911.
Rehman H, Ahmed ST, Akeroyd J, et al. Relation between cardiology follow-up visits, evidence-based statin prescribing, and statin adherence (from the Veterans Affairs Health Care System). Am J Cardiol. 2019;124(8):1165–70. https://doi.org/10.1016/j.amjcard.2019.07.022.
Hines DM, Rane P, Patel J, Harrison DJ, Wade RL. Treatment patterns and patient characteristics among early initiators of PCSK9 inhibitors. Vasc Health Risk Manag. 2018;14:409–18. https://doi.org/10.2147/VHRM.S180496.
Gupta M, Mancini GBJ, Wani RJ, et al. Real-world insights into evolocumab use in patients with hyperlipidemia: Canadian analysis from the ZERBINI Study. CJC Open. 2022;4(6):558–67. https://doi.org/10.1016/j.cjco.2022.03.003.
Simpson WG. Biomarker variability and cardiovascular disease residual risk. Curr Opin Cardiol. 2019;34(4):413–7. https://doi.org/10.1097/HCO.0000000000000627.
Cannon CP, de Lemos JA, Rosenson RS, et al. Use of lipid-lowering therapies over 2 years in GOULD, a registry of patients with atherosclerotic cardiovascular disease in the US. JAMA Cardiol. 2021;6(9):1–9. https://doi.org/10.1001/jamacardio.2021.1810.
Ray KK, Bruckert E, Peronne-Filardi P, et al. Long-term persistence with evolocumab treatment and sustained reductions in LDL-cholesterol levels over 30 months: final results from the European observational HEYMANS study. Atherosclerosis. 2023;366:14–21. https://doi.org/10.1016/j.atherosclerosis.2023.01.002.
Kaufman TM, Warden BA, Minnier J, et al. Application of PCSK9 inhibitors in practice. Circ Res. 2019;124(1):32–7. https://doi.org/10.1161/CIRCRESAHA.118.314191.
Kothawala P, Badamgarav E, Ryu S, Miller RM, Halbert RJ. Systematic review and meta-analysis of real-world adherence to drug therapy for osteoporosis. Mayo Clin Proc. 2007;82(12):1493–501. https://doi.org/10.1016/S0025-6196(11)61093-8.
Toth PP, Worthy G, Gandra SR, et al. Systematic review and network meta-analysis on the efficacy of evolocumab and other therapies for the management of lipid levels in hyperlipidemia. J Am Heart Assoc. 2017;6(10): e005367. https://doi.org/10.1161/JAHA.116.005367.
Nissen SE, Stroes E, Dent-Acosta RE, et al. Efficacy and tolerability of evolocumab vs ezetimibe in patients with muscle-related statin intolerance: the GAUSS-3 randomized clinical trial. JAMA. 2016;315(15):1580–90. https://doi.org/10.1001/jama.2016.3608.
Atreja A, Bellam N, Levy SR. Strategies to enhance patient adherence: making it simple. MedGenMed. 2005;7(1):4.
Baryakova TH, Pogostin BH, Langer R, McHugh KJ. Overcoming barriers to patient adherence: the case for developing innovative drug delivery systems. Nat Rev Drug Discov. 2023;22(5):387–409. https://doi.org/10.1038/s41573-023-00670-0.
Funding
This research is sponsored by Amgen Inc, Thousand Oaks, CA. Amgen Inc. funded the journal’s Rapid Service and Open Access Fees.
Author information
Authors and Affiliations
Contributions
Paul Muntner contributed to the study conception and design, interpretation of the results, preparation of the first manuscript draft and revisions to the manuscript based on co-author and peer reviewer comments. Lama Ghazi contributed to the study design and interpretation of results and provided comments on draft versions of the manuscript. Jenna Jones contributed to the study design and interpretation of results and provided comments on draft versions of the manuscript. Nafeesa Dhalwani contributed to the study conception and design and interpretation of results and provided comments on draft version of the manuscript. Bharat Poudel contributed to the study design and interpretation of results, provided supervision to the statisticians conducting the analyses and provided comments on draft versions of the manuscript. Ying Wen contributed to the study design, conducted data management and statistical analyses and provided comments on draft versions of the manuscript. Ligong Chen contributed to the study design, provided supervision to the statisticians conducting the data management and analyses and provided comments on draft versions of the manuscript. Zhixin Wang contributed to the study design and conducted data management and statistical analyses and provided comments on draft versions of the manuscript. Vera Bittner contributed to the study conception and design and interpretation of results and provided comments on draft versions of the manuscript. Bethany Kalich contributed to the study conception and design and interpretation of results and provided comments on draft versions of the manuscript. Michael E. Farkouh contributed to the study conception and design and interpretation of results and provided comments on draft versions of the manuscript. Mark Woodward contributed to the study conception and design and interpretation of results and provided comments on draft versions of the manuscript. Lisandro D. Colantonio contributed to the study design and interpretation of results, provided supervision to the statisticians conducting data management and analyses and provided comments on draft versions of the manuscript. Robert S. Rosenson contributed to the study conception and design and interpretation of results and provided comments on draft versions of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Paul Muntner is an employee of the US Centers for Disease Control and Prevention. This work was conducted while he was at the University of Alabama at Birmingham, and the findings and conclusions in this report are those of the authors and do not necessarily reflect the Centers for Disease Control and Prevention. Lama Ghazi and Lisandro D. Colantonio receive research support from Amgen Inc. Jenna Jones, Nafeesa Dhalwani and Bethany Kalich are employee and stockholders of Amgen Inc. Vera Bittner receives research grants to her institution from Sanofi and Regeneron (ODYSSEY OUTCOMES trial, Steering Committee member), Esperion (CLEAR OUTCOMES trial, National Coordinator), Dalcor (DalGene trial, National Coordinator), Astra Zeneca (STRENGTH trial, National Coordinator), Novartis (ORION trial, Site PI) and Amgen (Industry Collaboration between the UAB School of Public Health and Amgen, co-Investigator). Vera Bittner also receives or received payments as Senior Guest Editor for Circulation (American Heart Association, ongoing), Editor in Chief of the American College of Cardiology Self-Assessment Program (ACCSAP, American College of Cardiology, ongoing), Advisory Board member (Pfizer, concluded at the end of 2021) and Data Safety Monitoring Board member (Verve Therapeutics, ongoing). Mark Woodward was recently a consultant to Amgen and Freeline. Robert S. Rosenson receives research grants to his institution from Amgen, Arrowhead, Eli Lilly, NIH, Novartis and Regeneron; consulting fees from Amgen, CRISPER Therapeutics Eli Lilly, Lipigon, Novartis, Precision Biosciences, Regeneron, UltraGenyx and Verve; non-promotional honoraria from Kowa; royalties from Wolters Kluwer (UpToDate); stock holding in MediMergent, LLC; and patent applications on: Methods and systems for biocellular marker detection and diagnosis using a microfluidic profiling device (EFS ID: 32278349, Application No. PCT/US2019/026364, provisional); Compositions and methods relating to the identification and treatment of immunothrombotic conditions (New International Application No. PCT/US2021/63104926), and Quantification of Lp(a) vs. non-Lp(a) apoB concentration: development of a novel validated equation. (Application No. PCT/US2021/63248837). Bharat Poudel, Michael E. Farkouh, Zhixin Wang, Ligong Chen and Ying Wen report no disclosures.
Ethical Approval
Approval for this analysis was obtained from the Institutional Review Board at the University of Alabama at Birmingham. All data used in this analysis were collected as part of routine medical care. The requirement to obtain informed consent for this analysis of de-identified data was waived by the Institutional Review Board at the University of Alabama at Birmingham. Marketscan data were licensed from International Business Machines Corporation (Armonk, NY), and Medicare data were licensed from the US Centers for Medicare and Medicaid Services (CMS) Chronic Conditions Warehouse.
Additional information
Prior presentation: This work was presented as a poster on November 13, 2023 at the 2023 American Heart Association Scientific Sessions in Philadelphia, Pennsylvania.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Muntner, P., Ghazi, L., Jones, J. et al. Persistence and Adherence to PCSK9 Inhibitor Monoclonal Antibodies Versus Ezetimibe in Real-World Settings. Adv Ther (2024). https://doi.org/10.1007/s12325-024-02868-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12325-024-02868-z