Abstract
Introduction
The REVOLUTIONIZE I study aimed to characterize the relationships between medical nutrition therapy (MNT) and hyperkalemia recurrence in patients with stage 3–4 chronic kidney disease (CKD) and hyperkalemia who received MNT in real-world clinical practice.
Methods
This observational cohort study used de-identified electronic health record data from patients aged ≥ 18 years with stage 3–4 CKD who received MNT between January 2019 and October 2022 and had hyperkalemia (serum potassium > 5.0 mmol/L) within 30 days before MNT. Patients were followed for 6 months or until the first censoring event (death, prescription of outpatient potassium binder, or study end). The primary outcome was the percentage of patients with ≥ 1 hyperkalemia recurrence during follow-up. Secondary outcomes included the number of hyperkalemia recurrences per patient, time to each recurrence, and hyperkalemia-related healthcare resource utilization. Exploratory outcomes included all-cause healthcare resource utilization and mortality.
Results
The final cohort comprised 2048 patients; 1503 (73.4%) patients remained uncensored after 6 months. During the 6-month follow-up period, 56.0% of patients had ≥ 1 hyperkalemia recurrence and 37.4% had ≥ 1 recurrence within the first month. Patients with ≥ 1 hyperkalemia recurrence during follow-up had a mean ± standard deviation (SD) of 2.6 ± 2.2 recurrences. The mean ± SD time to first hyperkalemia recurrence was 45 ± 46 days; the time between recurrences decreased with subsequent episodes. Hyperkalemia-related hospitalizations and emergency department visits were recorded for 13.7% and 1.5% of patients, respectively. Sensitivity analyses showed that results were consistent across patient subgroups, including those with comorbid heart failure and patients receiving renin–angiotensin–aldosterone system inhibitor therapy at baseline.
Conclusion
Most patients with stage 3–4 CKD had hyperkalemia recurrence, and MNT alone was inadequate to prevent recurrence. These patients may require additional long-term treatment, such as novel potassium binders, to maintain normokalemia and prevent hyperkalemia recurrence following MNT.
Infographic available for this article.
Infographic

Plain Language Summary
Patients with chronic kidney disease (CKD) typically receive dietary counseling from a registered dietician, referred to as medical nutrition therapy, to help reduce their risk of complications of CKD while addressing their specific nutritional needs. Patients with CKD have an increased risk of elevated blood potassium levels (hyperkalemia), which has potentially life-threatening consequences. Although medical nutrition therapy may help patients with hyperkalemia to manage their dietary potassium intake, its effects in preventing recurrence are unclear. Our aim was to determine whether medical nutrition therapy can help prevent hyperkalemia recurrence after an initial event in patients with non-dialysis-dependent (stage 3–4) CKD in real-world clinical practice. We used data from de-identified electronic health records to study hyperkalemia recurrence over 6 months in patients with stage 3–4 CKD who received medical nutrition therapy within 30 days after experiencing hyperkalemia. Over half of the patients (56.0%) had at least one hyperkalemia recurrence within an average of 45 days during the 6 months after medical nutrition therapy; these patients had an average of 2.6 distinct recurrences in 6 months. In patients with two or more hyperkalemia recurrences, the time between these became shorter than 30 days. Our real-world study results show that hyperkalemia is a chronic, recurring condition in patients with stage 3–4 CKD, and that medical nutrition therapy is not enough to prevent its recurrence. This suggests that these patients may need additional long-term treatment for hyperkalemia, such as novel potassium binder therapy, to prevent hyperkalemia recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Medical nutrition therapy (MNT) is frequently provided to patients with chronic kidney disease (CKD) to address their nutritional needs and reduce the risk of CKD complications. |
CKD is associated with an increased risk of hyperkalemia; although MNT can help patients to manage their dietary intake of potassium, it is not known whether MNT alone is sufficient to prevent hyperkalemia recurrence. |
The aim of this retrospective, observational, cohort study was to evaluate the relationship between MNT and hyperkalemia recurrence in patients with stage 3–4 CKD who received MNT within 30 days after a hyperkalemia event. |
What was learned from the study? |
During the 6-month follow-up period, 56.0% of patients had ≥ 1 hyperkalemia recurrence (mean of 2.6 distinct recurrences); the mean time to first recurrence was 45 days, with the time between recurrences decreasing with subsequent hyperkalemia episodes. |
This study showed that hyperkalemia is a chronic, recurring condition for the majority of patients with stage 3–4 CKD, and that MNT alone was insufficient to prevent its recurrence. |
The results of this study suggest that additional long-term treatment, such as novel potassium binders, may be necessary to prevent hyperkalemia recurrence in patients with stage 3–4 CKD and hyperkalemia. |
Digital Features
This article is published with digital features, including an infographic, to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.25352206.
Introduction
The burden of chronic kidney disease (CKD) is increasing worldwide, with CKD estimated to affect more than 10% of the global population [1, 2]. In the USA, the estimated prevalence of CKD among people aged 18 years or older is approximately 35.5 million or around 14% of the adult population [3]. CKD is associated with a variety of electrolyte disturbances and is the most common factor associated with elevated levels of potassium [4, 5]. Hyperkalemia, defined as elevated serum potassium levels above the normal range (> 5.0 mmol/L), is a potentially life-threatening electrolyte imbalance that can result in arrhythmias and sudden death [6, 7]. In addition to CKD [7, 8], risk factors for hyperkalemia include diabetes, heart failure (HF), and the use of renin–angiotensin–aldosterone system inhibitors (RAASis) [5, 7, 9,10,11].
The incidence of hyperkalemia has been reported to range between 2% and 35% in patients with CKD [5]. Much of the variation in incidence may be explained by differences in estimated glomerular filtration rate (eGFR), with low eGFR being a key risk factor for increased serum K+ in CKD [5, 12]. Other reasons for this variation include the use of RAASis and potassium-sparing diuretics, and the presence of comorbidities such as diabetes and HF [5, 13]. RAASis are disease-modifying drugs that can slow CKD progression, prevent hospitalization with HF, and reduce mortality in patients with CKD and/or HF [14,15,16]. However, RAASi treatment has often been discontinued or continued at a suboptimal dose in patients who develop hyperkalemia, which compromises its cardiorenal benefits [17]. Consequently, updated guidelines for CKD and HF recommend RAASi discontinuation or dose reduction only if hyperkalemia remains uncontrolled despite medical treatment, including the use of anti-hyperkalemia therapies such as potassium binders or gastrointestinal cation exchangers [14, 15, 18].
Although sodium-glucose cotransporter 2 inhibitors and sacubitril-valsartan appear useful in reducing the risk of hyperkalemia induced by mineralocorticoid receptor antagonists, these agents are not recommended to treat hyperkalemia once it has occurred. Therefore, recommendations for the management of hyperkalemia include monitoring serum potassium levels in patients at risk, reviewing the use of medications associated with increased risk of hyperkalemia, reducing dietary potassium intake (including the use of salt substitutes), treatment of metabolic acidosis, loop diuretic therapy, and treatment with the newer potassium binders, patiromer or sodium zirconium cyclosilicate (SZC) [19, 20]. Potassium binder therapy may allow patients to maintain RAASi treatment, with real-world studies showing that 80% or more patients receiving SZC [21] or patiromer [22] were able to continue RAASi therapy.
An important facet of CKD management is medical nutrition therapy (MNT), also known as dietary counseling, which is mostly provided by registered dietitians [23]. Treatment guidelines recommend MNT for all patients with CKD to avoid complications [24, 25]. MNT involves assessing and addressing individual patients’ nutritional needs; this includes consideration of protein, energy, and fluid intake, treating vitamin deficiencies, and managing sodium, potassium, and phosphorous levels [23, 25, 26]. To reduce the risk of hyperkalemia, patients with CKD may need to lower their dietary potassium intake, particularly if they are receiving RAASi therapy [25, 26]. However, adherence to a low-potassium diet while also meeting nutritional needs can be challenging without the guidance of a registered dietitian [20, 26]. This is because potassium is present in a wide variety of foods, including plant-based foods, which contain high levels of fiber in addition to vitamins and trace elements, as well as other heart-healthy foods [20, 24, 26]. In addition, there are hidden sources of potassium, such as the salt substitutes that are frequently recommended for patients with hypertension [26]. A dietitian can work with patients to identify their individual nutritional needs and their dietary sources of potassium and recommend modifications such as food substitutions or changes to cooking techniques (e.g., boiling or soaking) to reduce the potassium levels in foods [24, 26].
Although MNT has been evaluated in the context of CKD progression [23] and has the potential to reduce hyperkalemia risk by managing dietary potassium intake, the relationship between MNT and hyperkalemia has not been well investigated. Furthermore, although it has been established that hyperkalemia is associated with increased healthcare costs and healthcare resource utilization (HRU) [27,28,29,30], there is a lack of data describing HRU in patients with hyperkalemia who receive MNT. Therefore, the aim of the REVOLUTIONIZE I retrospective cohort study was to better understand the correlations between MNT and hyperkalemia recurrence, hyperkalemia-related hospitalizations, and hyperkalemia-related emergency department (ED) visits in patients with stage 3–4 CKD and hyperkalemia who received MNT in real-world clinical practice.
Methods
Study Design and Data Source
REVOLUTIONIZE I was an observational cohort study that utilized de-identified longitudinal electronic health record (EHR) data collected on December 19, 2022, from the TriNetX Dataworks-USA Network database. This network provided access to de-identified inpatient and outpatient EHR data (diagnoses, procedures, medications, laboratory values, genomic information) from approximately 66 million patients at 45 healthcare organizations, including academic medical centers, integrated delivery networks, specialty hospitals, and large specialty physician practices. Healthcare encounters that occurred outside of this network were not captured.
Ethical Considerations
This retrospective, non-interventional study used only patient data that were de-identified in compliance with the standard defined in section §164.514(a) of the Health Insurance Portability and Accountability Act (HIPAA) privacy rule. All data were collected during routine clinical practice prior to access to the final data cut from the TriNetX Dataworks-USA Network database; all data were de-identified and no patient identifiers were available to the study investigators. AstraZeneca did not access or license data from TriNetX for the conduct of this study. This study was not classified as research involving human subjects (under the Code of Federal Regulations title 45 §46.101) and was therefore exempt from institutional review board approval or requirement for informed consent from individual patients. This study was conducted in accordance with the Declaration of Helsinki of 1964 and its later amendments.
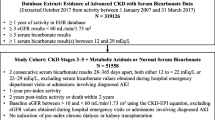
Study Population
Eligible patients were aged 18 years or older, had diagnosed hyperkalemia and stage 3–4 CKD, and received MNT between January 1, 2019, and October 31, 2022 (study period). The MNT date was the date of the first evidence of MNT preceded by a serum potassium level > 5.0 mmol/L (within 30 days before MNT). MNT involved the use of standardized curriculums on dietary counselling with appropriate follow-up monitoring, although the contents of the curriculums used are not visible within the data source. The index date was defined as the MNT date plus 7 days. The baseline period was the 24 months immediately preceding the index date (Fig. 1). To ensure that patients received regular care, within the TriNetX Dataworks-USA Network, all patients were required to have at least one healthcare encounter within 12–24 months prior to the index date. Patients were excluded if they had stage 5 CKD or end-stage kidney disease (eGFR < 15 mL/min/1.73 m2) at any time during the baseline period. Patients were also excluded if they had an outpatient prescription for a potassium binder (sodium polystyrene sulfonate, patiromer, or SZC) within 182 days before the index date to focus on first-line MNT.
Patients included in the study were followed for either 6 months from the index date or until the first censoring event (death or prescription of outpatient potassium binder, or end of study period). All data gathering and analyses were overseen by three pharmacoepidemiologists.
Study Objectives and Outcomes
The primary outcome was the percentage of patients who experienced at least one hyperkalemia recurrence, defined as a serum potassium measurement of > 5.0 mmol/L during follow-up. Hyperkalemia recurrence was classified within six analysis intervals (i.e., 0–1, 0–2, 0–3, 0–4, 0–5, and 0–6 months post index). Secondary outcomes were analyzed for patients who remained uncensored at 6 months post index. These outcomes were described for a single analysis interval (0–6 months) and included (1) hyperkalemia recurrence after the first post-index recurrence, defined as a serum potassium level of >5.0 mmol/L observed more than 7 days after the previous hyperkalemia recurrence; (2) time to each hyperkalemia recurrence for up to six hyperkalemia recurrences during the 6-month follow-up period (calculated as the number of days from the start of the follow-up period [i.e., index date plus 1 day] to the date of the first post-index serum potassium measurement of > 5.0 mmol/L); (3) change in serum potassium level from baseline to the first hyperkalemia recurrence; (4) serum potassium level at each recurrence; (5) hyperkalemia-related hospitalizations, defined as an inpatient encounter in which a hyperkalemia-related diagnosis was recorded in any diagnosis position during admission (classified by Current Procedural Terminology codes for initial and subsequent hospital care, inpatient observations, discharge management, and critical care in the intensive care unit), with the outcome date defined as the date of the first inpatient encounter recorded in the EHR and no analysis of subsequent hospitalizations; (6) hyperkalemia-related ED visits, classified as an ED encounter with a recorded diagnosis of hyperkalemia (in any diagnosis position) on the date of the ED visit, occurring within 6 months post index.
Exploratory outcomes included all-cause hospitalizations, all-cause ED visits, and all-cause mortality. Hospitalizations and ED visits were assessed for the 6-month follow-up period; mortality was assessed for an additional month after the follow-up period, because EHR data capture the month after the actual date of death to protect patient privacy.
Sensitivity analyses were conducted to evaluate study outcomes for the following subgroups: stage 3b CKD (eGFR ≥ 30 and < 45 mL/min/1.73 m2); stage 4 CKD (eGFR ≥ 15 and < 30 mL/min/1.73 m2); diagnosis of HF, prescription of RAASi therapy at baseline; stage 3a CKD (eGFR ≥ 45 and < 60 mL/min/1.73 m2); diagnosis of hypertension; diagnosis of type 2 diabetes; diagnosis of HF plus stage 3a/3b CKD; diagnosis of HF plus stage 3a CKD; and moderate-to-severe hyperkalemia (serum potassium ≥5.5 mmol/L for the index hyperkalemia episode). An additional sensitivity analysis was conducted to assess the proportion of patients with hyperkalemia recurrence when recurrence was defined as a serum potassium level of ≥ 5.0 mmol/L; this was done for the overall population and the aforementioned patient subgroups.
Statistical Analyses
A sample size of 263 patients was calculated to provide 90% power to detect a 10% difference in hyperkalemia recurrence, assuming a 50% hyperkalemia recurrence rate under the null hypothesis. Descriptive statistics and 95% confidence intervals (95% CIs; Clopper–Pearson, exact binomial) were used. Hypothesis testing was used for the primary analysis to determine if the observed proportion of patients with a hyperkalemia recurrence was 50%, with a null hypothesis that there was no difference between the observed proportion of patients with a hyperkalemia recurrence and the a priori specified hypothesis of 50% recurrence. For the primary outcome of hyperkalemia recurrence, the analysis set for each interval comprised patients who remained uncensored for the entire duration of that analysis interval. For secondary and exploratory objectives, excluding all-cause mortality, the analysis set comprised all patients with at least 6 months of follow-up; all-cause mortality was analyzed in the cohorts without censoring.
Results
Study Population
The final cohort comprised 2048 patients (Table S1 in the electronic supplementary material), and 1503 (73.4%) remained uncensored at the end of the 6-month follow-up period. Reasons for censoring and the time to the first censoring event are presented in Table S2 in the electronic supplementary material. Baseline demographics, clinical characteristics, treatments, and HRU for the overall study cohort and key patient subgroups are presented in Table 1.
In the overall study cohort, the mean ± standard deviation (SD) age at index was 66.0 ± 14.1 years. The mean ± SD serum potassium level at baseline was 5.5 ± 0.5 mmol/L and the majority (59.0%) of patients had mild hyperkalemia (> 5.0 to < 5.5 mmol/L). Mean ± SD eGFR, based on the last serum creatinine measurement within 12 months of the index date, was 34.6 ± 12.8 mL/min/1.73 m2; 58.1% of patients had stage 3a or 3b CKD and 41.9% had stage 4 CKD at baseline. The most common comorbidities in the overall patient cohort were hypertension (96.1% of patients), type 2 diabetes (65.1%), and HF (57.6%). Notably, during the 6 months before the index date, 71.1% of patients were receiving loop diuretics and 43.6% were receiving RAASi therapy. Baseline data for additional patient subgroups for which sensitivity analyses were conducted are presented in Table S3 in the electronic supplementary material.
Hyperkalemia Recurrence
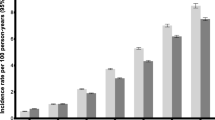
More than half of the overall population experienced hyperkalemia recurrence during the 6 months after MNT (Table 2), with over one-third having a recurrence within the first month. During the 6-month follow-up period, 842 of 1503 patients (56.0%; 95% CI, 53.5–58.6%; p = 0.001 vs the estimated recurrence rate) experienced at least one hyperkalemia recurrence (Fig. 2a). Of the 1790 patients who remained uncensored for the 0–1 month post-index interval, 669 (37.4%; 95% CI, 35.1–39.7%; p < 0.001) experienced hyperkalemia recurrence.
Proportion of patients with hyperkalemia recurrence among the total study cohort (a), patients with stage 3b CKD (b), patients with stage 4 CKD (c), patients with heart failure (d), and patients receiving RAASi therapy at baseline (e). N values represent patients remaining uncensored for the analysis interval. p values are versus the a priori estimated recurrence rate of 50% (vertical red line). *Statistically significant. CI confidence interval, CKD chronic kidney disease, RAASi renin–angiotensin–aldosterone system inhibitor
In patients with at least 6 months of follow-up and at least one hyperkalemia recurrence, the mean ± SD number of recurrences during follow-up was 2.6 ± 2.2 (median 2; range 1–13). In these patients, the mean ± SD time to first hyperkalemia recurrence was 45 ± 46 days and mean ± SD serum potassium at the first recurrence was 5.4 ± 0.4 mmol/L (Table 2). The mean interval between subsequent hyperkalemia recurrences decreased with each recurrence, whereas the mean serum potassium levels remained relatively constant for each recurrence (Table 2).
Sensitivity analyses of patient subgroups with stage 3b CKD, stage 4 CKD, HF, and baseline RAASi use also showed that over half of all patients in each subgroup experienced hyperkalemia recurrence during the follow-up period. As in the total study cohort, the time to recurrence among patients with at least 6 months of follow-up and at least one hyperkalemia recurrence decreased with subsequent recurrences, but the mean serum potassium levels were consistent (Table 2).
Patients with Stage 3b CKD
Among patients with stage 3b CKD (n = 657), 256 of 472 patients with at least 6 months’ follow-up (54.2%; 95% CI, 49.7–58.7%; p = 0.066) experienced at least one hyperkalemia recurrence (Fig. 2b). In this subgroup, 222 of 571 patients (38.9%; 95% CI, 34.9–42.9%; p < 0.001) who remained uncensored for the 0–1 month post-index interval experienced hyperkalemia recurrence during the first month post index.
Patients with Stage 4 CKD
In the subgroup with stage 4 CKD (n = 859), 614 patients had at least 6 months’ follow-up available; 365 of these patients (59.4%; 95% CI, 55.6–63.3%; p < 0.001) experienced at least one hyperkalemia recurrence (Fig. 2c). During the first month post index, 287 of 734 patients (39.1%; 95% CI, 35.6–42.6%; p < 0.001) had hyperkalemia recurrence.
Patients with HF
In the subgroup with HF (n = 1179), 861 patients had at least 6 months of follow-up. Of these patients, 485 (56.3%; 95% CI, 53.0–59.6%; p < 0.001) experienced at least one hyperkalemia recurrence (Fig. 2d). Hyperkalemia recurrence was recorded for 395 of 1036 patients (38.1%; 95% CI, 35.2–41.1%; p < 0.001) during the 0–1 month post-index interval.
Patients Receiving RAASi Therapy
Among patients receiving RAASi therapy at baseline (n = 892), 681 patients had at least 6 months’ follow-up available, of whom 367 (53.9%; 95% CI 50.1–57.6%; p = 0.042) experienced at least one hyperkalemia recurrence (Fig. 2e). During the 0–1 month post-index interval, 283 of 794 patients (35.6%; 95% CI 32.3–39.0%; p < 0.001) experienced hyperkalemia recurrence.
Other Patient Subgroups
Sensitivity analyses for the subgroups of patients with hypertension, patients with stage 3a CKD, patients with type 2 diabetes, patients with HF and stage 3a/3b CKD, patients with HF and stage 3a CKD, and patients with moderate-to-severe hyperkalemia also showed that more than half (52.5–57.2%) of each subgroup had at least one hyperkalemia recurrence during the 6-month follow-up period (Table S4 in the electronic supplementary material). Within these subgroups, time to recurrence also decreased with subsequent recurrences, while mean serum potassium levels remained consistent for each recurrence (Table S4 in the electronic supplementary material).
Hyperkalemia Recurrence with Serum Potassium ≥ 5.5 mmol/L
The sensitivity analysis with recurrence defined as serum potassium of ≥ 5.5 mmol/L showed that hyperkalemia recurrence occurred in approximately one-third of patients within 6 months after MNT (Table S5 in the electronic supplementary material).
HRU and All-Cause Mortality
Among the 1503 patients in the total study cohort with at least 6 months of follow-up, hyperkalemia-related hospitalizations were recorded for 206 patients (13.7%), and hyperkalemia-related ED visits were recorded for 22 patients (1.5%) (Table 2). In addition, all-cause hospitalizations were recorded for 955 patients (63.5%), and all-cause ED visits for 339 patients (22.6%). Sensitivity analyses revealed similar HRU in patient subgroups, with the proportions of patients with hyperkalemia-related hospitalization ranging from 10.8% to 15.6%, and the proportions with hyperkalemia-related ED visits ranging from 0.4% to 1.8% (shown in Table 2 and in Table S4 in the electronic supplementary material).
In the overall study cohort (N = 2048), all-cause mortality was recorded for 325 patients (15.9%) (Table 2). All-cause mortality rates in patient subgroups ranged from 12.6% among patients with stage 3a CKD to 19.0% among patients with HF (shown in Table 2 and in Table S4 in the electronic supplementary material).
Discussion
Among patients with stage 3–4 CKD who received MNT after experiencing hyperkalemia, more than one-third of patients (37.4%) had a hyperkalemia recurrence within 1 month after MNT. By 6 months, more than half (56.0%) had experienced at least one recurrence, with an average of 45 days until the first recurrence, which exceeded the prespecified recurrence rate of 50.0% (p < 0.001). The time between subsequent hyperkalemia recurrences tended to decrease to less than 30 days by the third recurrence, indicating the recurrent nature of hyperkalemia. In addition, serum potassium levels were relatively constant and unchanged between each recurrence. Results of sensitivity analyses were consistent with those for the overall study cohort and did not reveal clinically relevant differences between the patient subgroups investigated.
HRU in patients with CKD who experienced hyperkalemia after MNT was substantial, with approximately 14% of patients having hyperkalemia-related inpatient hospitalizations. Although MNT is an important component of CKD management, there is a lack of evidence regarding its utility in the treatment of hyperkalemia and the prevention of recurrent hyperkalemia. Our results suggest that MNT is insufficient to treat hyperkalemia and prevent recurrence of hyperkalemia in patients with CKD, and that augmentation of MNT with well-tolerated and efficacious treatments to reduce potassium levels in a sustained manner, such as novel potassium binder therapies, may be necessary. Furthermore, the results of this study indicate that hyperkalemia is a chronic risk for most patients with stage 3–4 CKD, for which long-term treatment will be required to prevent subsequent recurrences. Notably, the hyperkalemia recurrence was high despite the majority (71.1%) of patients receiving loop diuretics during the 6 months before the index date. This suggests that further research is needed to determine whether loop diuretic therapy is sufficient to prevent hyperkalemia recurrence.
A strength of our study was that patients who received outpatient oral potassium binder therapy within 6 months before MNT were excluded, allowing a focus on patients who received first-line MNT. Moreover, to mitigate the potential for selection bias, the study cohort systematically included all patients with stage 3–4 CKD and hyperkalemia who received MNT during the study period. Importantly, the patient population included in the TriNetX Dataworks-USA Network has been shown to be broadly representative of patients who receive medical care in the USA, because the database captures de-identified EHR data from large healthcare systems with multiple affiliated sites across a large geographic region. The requirement for patients to have received regular care within the network reduces the potential for missing data and increases the probability that patients included in the study received follow-up treatment at centers within the network.
However, the results of this EHR study should be interpreted in the context of its inherent limitations, including misclassification bias. To mitigate the potential for misclassification, patients were required to have diagnosed hyperkalemia with a clinically accepted serum potassium threshold (> 5.0 mmol/L), and MNT was required to be initiated within 30 days of the index hyperkalemia episode. In addition, the contents of the standardized curriculums used during the MNT visits and patients’ adherence to dietary counseling were unknown, as these were not captured in the data source. It is also important to note that, as a retrospective observational study, causality cannot be inferred from the study results.
Conclusion
Our real-world study results showed that hyperkalemia is a chronic and recurrent condition for most patients with stage 3–4 CKD and that MNT alone was inadequate to prevent its recurrence. Furthermore, all-cause and hyperkalemia-related HRU were high even after patients received MNT. Patients with stage 3–4 CKD may require additional long-term treatment, such as novel potassium binders, to maintain normokalemia and prevent hyperkalemia recurrence following MNT.
Data Availability
The datasets analyzed during the current study are not publicly available and only employees and subcontractors of TriNetX had access to the database for this study. However, the TriNetX Federated Data Network offers a subscription-based clinical data platform comprising worldwide de-identified electronic medical records that are accessible for querying. Detailed insights regarding the TriNetX Network are available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6816049/. For data requests, interested researchers may contact join@trinetx.com, and access the network via https://live.trinetx.com/.
References
Feng X, Hou N, Chen Z, et al. Secular trends of epidemiologic patterns of chronic kidney disease over three decades: an updated analysis of the Global Burden of Disease Study 2019. BMJ Open. 2023;13(3):e064540.
Jager KJ, Kovesdy C, Langham R, Rosenberg M, Jha V, Zoccali C. A single number for advocacy and communication—worldwide more than 850 million individuals have kidney diseases. Nephrol Dial Transplant. 2019;34(11):1803–5.
Centers for Disease Control and Prevention. Chronic kidney disease in the United States, 2023. 2023. https://www.cdc.gov/kidneydisease/publications-resources/ckd-national-facts.html. Accessed 6 July 2023.
Belmar Vega L, Galabia ER, Bada da Silva J, et al. Epidemiology of hyperkalemia in chronic kidney disease. Nefrologia (Engl Ed). 2019;39(3):277–86.
Watanabe R. Hyperkalemia in chronic kidney disease. Rev Assoc Med Bras (1992). 2020;66(Suppl 1):S31–6.
Dunn JD, Benton WW, Orozco-Torrentera E, Adamson RT. The burden of hyperkalemia in patients with cardiovascular and renal disease. Am J Manag Care. 2015;21(15 Suppl):S307–15.
Einhorn LM, Zhan M, Hsu VD, et al. The frequency of hyperkalemia and its significance in chronic kidney disease. Arch Intern Med. 2009;169(12):1156–62.
Sarafidis PA, Blacklock R, Wood E, et al. Prevalence and factors associated with hyperkalemia in predialysis patients followed in a low-clearance clinic. Clin J Am Soc Nephrol. 2012;7(8):1234–41.
Hunter RW, Bailey MA. Hyperkalemia: pathophysiology, risk factors and consequences. Nephrol Dial Transplant. 2019;34(Suppl 3):iii2–11.
Thomsen RW, Nicolaisen SK, Hasvold P, et al. Elevated potassium levels in patients with congestive heart failure: occurrence, risk factors, and clinical outcomes. J Am Heart Assoc. 2018;7(11): e008912.
Bandak G, Sang Y, Gasparini A, et al. Hyperkalemia after initiating renin-angiotensin system blockade: the Stockholm Creatinine Measurements (SCREAM) Project. J Am Heart Assoc. 2017. https://doi.org/10.1161/JAHA.116.005428.
Kovesdy CP, Matsushita K, Sang Y, et al. Serum potassium and adverse outcomes across the range of kidney function: a CKD Prognosis Consortium meta-analysis. Eur Heart J. 2018;39(17):1535–42.
Bianchi S, Aucella F, De Nicola L, Genovesi S, Paoletti E, Regolisti G. Management of hyperkalemia in patients with kidney disease: a position paper endorsed by the Italian Society of Nephrology. J Nephrol. 2019;32(4):499–516.
Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int. 2021;99(3 Suppl):S1–87.
Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(18):e895–e1032.
Xie X, Liu Y, Perkovic V, et al. Renin-angiotensin system inhibitors and kidney and cardiovascular outcomes in patients with CKD: a Bayesian network meta-analysis of randomized clinical trials. Am J Kidney Dis. 2016;67(5):728–41.
Rosano GMC, Tamargo J, Kjeldsen KP, et al. Expert consensus document on the management of hyperkalaemia in patients with cardiovascular disease treated with renin angiotensin aldosterone system inhibitors: coordinated by the Working Group on Cardiovascular Pharmacotherapy of the European Society of Cardiology. Eur Heart J Cardiovasc Pharmacother. 2018;4(3):180–8.
Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group. KDIGO 2022 clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int. 2022;102(5 Suppl):S1–127.
Alfonzo D, Harrison A, Baines R, Chu A, Mann S. Clinical practice guidelines: treatment of acute hyperkalaemia in adults. 2020. https://ukkidney.org/sites/renal.org/files/RENAL%20ASSOCIATION%20HYPERKALAEMIA%20GUIDELINE%20-%20JULY%202022%20V2_0.pdf. Accessed 15 June 2023.
Palmer BF, Carrero JJ, Clegg DJ, et al. Clinical management of hyperkalemia. Mayo Clin Proc. 2021;96(3):744–62.
Agiro A, Amin AN, Cook EE, et al. Real-world modifications of renin-angiotensin-aldosterone system inhibitors in patients with hyperkalemia initiating sodium zirconium cyclosilicate therapy: the OPTIMIZE I study. Adv Ther. 2023;40(6):2886–901.
Kovesdy CP, Gosmanova EO, Woods SD, et al. Real-world management of hyperkalemia with patiromer among United States Veterans. Postgrad Med. 2020;132(2):176–83.
de Waal D, Heaslip E, Callas P. Medical nutrition therapy for chronic kidney disease improves biomarkers and slows time to dialysis. J Ren Nutr. 2016;26(1):1–9.
Ikizler TA, Burrowes JD, Byham-Gray LD, et al. KDOQI clinical practice guideline for nutrition in CKD: 2020 update. Am J Kidney Dis. 2020;76(3 Suppl 1):S1–107.
National Institute of Diabetes and Digestive and Kidney Diseases. Diet & nutrition for adults with advanced chronic kidney disease. https://www.niddk.nih.gov/health-information/kidney-disease/chronic-kidney-disease-ckd/eating-nutrition/nutrition-advanced-chronic-kidney-disease-adults#potassium. Accessed 12 July 2023.
Cupisti A, Kovesdy CP, D’Alessandro C, Kalantar-Zadeh K. Dietary approach to recurrent or chronic hyperkalaemia in patients with decreased kidney function. Nutrients. 2018;10(3):261.
Mu F, Betts KA, Woolley JM, et al. Prevalence and economic burden of hyperkalemia in the United States Medicare population. Curr Med Res Opin. 2020;36(8):1333–41.
Betts KA, Woolley JM, Mu F, et al. Postdischarge health care costs and readmission in patients with hyperkalemia-related hospitalizations. Kidney Int Rep. 2020;5(8):1280–90.
Betts KA, Woolley JM, Mu F, McDonald E, Tang W, Wu EQ. The prevalence of hyperkalemia in the United States. Curr Med Res Opin. 2018;34(6):971–8.
Fitch K, Woolley JM, Engel T, Blumen H. The clinical and economic burden of hyperkalemia on Medicare and commercial payers. Am Health Drug Benefits. 2017;10(4):202–10.
Medical Writing, Editorial, and Other Assistance.
Raewyn M. Poole of inScience Communications, Springer Healthcare and Marie Cheeseman, on behalf of inScience Communications, Springer Healthcare, provided medical writing support in accordance with Good Publication Practice, funded by AstraZeneca. Thomas Peer provided quality control support for TriNetX, LLC.
Authorship.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding
The REVOLUTIONIZE I study and development of this manuscript and infographic, including medical writing support, Rapid Service Fee, and Open Access Article Processing Charge, were supported by AstraZeneca.
Author information
Authors and Affiliations
Contributions
Christopher G. Rowan: methodology, formal analysis, visualization, and writing – reviewing and editing. Abiy Agiro: conceptualization, methodology, visualization, writing – reviewing and editing, and supervision. K. Arnold Chan: methodology, investigation, visualization, and writing – reviewing and editing. Ellen Colman: methodology, visualization, and writing – reviewing and editing. Katie White: investigation, data curation, and writing – reviewing and editing. Pooja Desai: conceptualization, methodology, visualization, and writing – reviewing and editing. Jamie P. Dwyer: methodology, visualization, and writing – reviewing and editing.
Corresponding author
Ethics declarations
Conflict of Interest
Christopher G. Rowan was paid by TriNetX, LLC as an observational scientist to design and execute this study and is a paid consultant for Harvard Pilgrim Health Care Institute and Puma Biotech. Abiy Agiro, Ellen Colman, and Pooja Desai are employees and stockholders of AstraZeneca. K. Arnold Chan and Katie White are employees of TriNetX, LLC. The study described in this manuscript was conducted as part of their employment responsibilities at TriNetX, LLC. The authors were compensated by TriNetX, LLC for their contributions to the design, data collection, analysis, and interpretation of the study findings presented herein. The funding for this study was provided by AstraZeneca. Jamie P. Dwyer has acted as a scientific consultant for AstraZeneca and received fees from AstraZeneca for the conduct of this study; has received fees from Sanofi and CSL Behring as part of a steering committee; has received fees from Novo Nordisk for outcome adjudication for a clinical trial; has received fees from Boehringer Ingelheim and Lilly for study design; and has received personal fees from Bayer, CinCor, Caladrius Biosciences, Inversago, GlaxoSmithKline LLC, and ProKidney.
Ethical Approval
This study used only patient data that were de-identified in compliance with the standard defined in section §164.514(a) of the Health Insurance Portability and Accountability Act (HIPAA) privacy rule. All data were collected during routine clinical practice prior to access to the final data cut from the TriNetX Dataworks-USA Network database; all study data were de-identified and no patient identifiers were available to the study investigators. AstraZeneca did not access or license data from TriNetX for the conduct of this study. The study was not classified as research involving human subjects (under the Code of Federal Regulations title 45 §46.101) and was therefore exempt from institutional review board approval or requirement for informed consent from individual patients. This study was conducted in accordance with the Declaration of Helsinki of 1964 and its later amendments.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Rowan, C.G., Agiro, A., Chan, K.A. et al. Hyperkalemia Recurrence Following Medical Nutrition Therapy in Patients with Stage 3–4 Chronic Kidney Disease: The REVOLUTIONIZE I Real-World Study. Adv Ther 41, 2381–2398 (2024). https://doi.org/10.1007/s12325-024-02835-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-024-02835-8