Abstract
Introduction
The 2018 American Heart Association (AHA)/American College of Cardiology (ACC)/Multisociety blood cholesterol guidelines recommend clinicians consider adding non-statin therapy for patients with very high-risk (VHR) atherosclerotic cardiovascular disease (ASCVD) and low-density lipoprotein cholesterol (LDL-C) ≥ 70 mg/dl while receiving maximally tolerated statins. However, according to a recent study, only 17.1% of patients with established ASCVD received appropriate lipid-lowering therapy (LLT) intensification. Here, we describe the design of a prospective, 12-month study (LOGAN-CV) evaluating a multifaceted site-level intervention to enhance clinicians’ adherence to guidelines to improve LDL-C levels for patients with VHR ASCVD.
Methods
Clinicians from up to ten research sites are eligible if they care for adult patients with ASCVD. Interventions include educational modules, a cloud-based performance platform providing clinicians a tailored summary of their LDL-C management performance, newsletters, periodic peer-to-peer calls, and pre- and post-intervention surveys evaluating knowledge, attitudes, and beliefs around LDL-C management, with additional interventions for clinicians demonstrating a lower readiness to make treatment decisions based on guideline recommendations. Patients with VHR ASCVD, defined as having recent myocardial infarction and LDL-C ≥ 70 mg/dl despite statin treatment, will be included in the study. Patient data will be collected from electronic medical records from baseline (clinician enrollment) through the 12-month intervention. The study started in October 2022, with anticipated completion in March 2024.
Planned Outcomes
The change in proportion of patients with LDL-C < 70 mg/dl achieved at any time during the 12-month intervention (primary); LLT intensification, changes in guideline-aligned LDL-C testing and LLT titration over 12 months, and change in overall clinicians’ knowledge, attitudes, and beliefs are key outcomes of interest. The LOGAN-CV study addresses a critical unmet need in LDL-C control in patients with VHR ASCVD and evaluates the effect of a multifaceted intervention targeting clinicians to improve their adherence to guidelines and consequently improve clinical outcomes for patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Many patients with atherosclerotic cardiovascular disease (ASCVD) receiving lipid-lowering therapy (LLT) do not achieve ≥ 50% reduction in low-density lipoprotein cholesterol (LDL-C) levels and LDL-C remains ≥ 70 mg/dl, despite recommendations made in 2018 by the American Heart Association/American College of Cardiology/Multisociety blood cholesterol guideline. |
The LOGAN-CV (Clinician Engagement in Guideline-based Management of LDL ChOlesterol for Patients at HiGh Risk for a Future Atherosclerotic Cardiovascular Disease [ASCVD] EveNt) study is a prospective, 12-month study that will address a critical unmet need, evaluating the effect of a multifaceted guideline-based intervention on improving clinician behaviors and clinical outcomes in adult patients with a recent myocardial infarction (MI) and LDL-C ≥ 70 mg/dl despite receiving statins. |
The multifaceted intervention includes educational modules, a cloud-based platform providing a summary of LDL-C management performance, newsletters, peer-to-peer calls, and pre- and post-intervention surveys evaluating clinicians’ knowledge, attitudes, and beliefs regarding LDL-C management. |
The primary endpoint is the change in proportion of patients with LDL-C < 70 mg/dl achieved at any time during the 12-month intervention; secondary endpoints will evaluate changes in LDL-C, LLT intensification/titration, LDL-C testing, and change in clinicians’ knowledge, attitudes, and beliefs after the intervention. |
Introduction
In patients with established atherosclerotic cardiovascular disease (ASCVD), the 2018 American Heart Association (AHA)/American College of Cardiology (ACC)/Multisociety blood cholesterol guideline (hereafter referred to as “the guideline”) recommends the use of high-intensity statin therapy to decrease low-density lipoprotein cholesterol (LDL-C) by ≥ 50% to reduce the risk of recurrent cardiovascular events [1, 2]. Furthermore, in patients with ASCVD whose LDL-C level remains ≥ 70 mg/dl, addition of non-statin drugs should be considered [1]. The 2022 ACC Expert Consensus Decision Pathway recently lowered the LDL-C threshold in patients with very high-risk (VHR) ASCVD to ≥ 55 mg/dl and recommended the preferred use of non-statins such as ezetimibe and proprotein convertase subtilisin/kexin type 9 inhibitor (PCSK9i) monoclonal antibodies (mAbs) because of evidence of reduction of future ASCVD events [3].
Despite the guideline recommendations and the ample evidence supporting the use of lipid-lowering therapies (LLTs), the use of LLTs in real-world clinical practice is not aligned with the guideline [4]. For example, in the Getting to an imprOved Understanding of Low-Density Lipoprotein Cholesterol and Dyslipidemia Management (GOULD) study in the US, only 17.1% of patients received LLT intensification after 2 years, with approximately one in three patients achieving LDL-C < 70 mg/dl and one in ten patients achieving LDL-C < 55 mg/dl [5]. In the European DA VINCI study, which was an 18 country, cross-sectional, observational study of patients prescribed LLT, 33% of the patients achieved LDL-C goals as recommended by the 2019 European Society of Cardiology (ESC)/European Atherosclerosis Society (EAS) guideline while receiving stabilized LLT [6]. High-intensity statin monotherapy was used in 20% of VHR primary prevention patients and in 38% of secondary prevention patients, with 2019 ESC/EAS LDL-C goals achieved in 17% and 22%, respectively [6]. The use of ezetimibe and PCSK9i in combination with statins was low (9% and 1%, respectively), with a higher proportion of patients receiving these combination therapies achieving 2019 ESC/EAS LDL-C goals (37% with ezetimibe and 57% with PCSK9i) compared with statin monotherapy. The DA VINCI overall study [6] and the other studies in various countries provide a wealth of evidence that patients on LLTs often do not achieve guideline-recommended LDL-C levels, and LLTs are often not intensified as recommended by current guidelines [7,8,9,10,11,12,13,14,15,16,17]. A key part of implementing guideline-directed lipid lowering is testing for lipid levels in appropriate patients. A recent cross-sectional study conducted in the US revealed that the rates of repeat LDL-C measurement within 1 year were low (27.9%–54.5%), and only approximately one-quarter of patients tested were below the guideline-recommended LDL-C threshold [18].
Reasons for not achieving recommended LDL-C levels may be complex and multifaceted, including insufficient LDL-C monitoring, clinical inertia or lack of provider education, patient non-adherence to treatment, denial by insurance providers for add-on therapies, and the lack of LDL-C quality metrics, which were retired in 2014 [19,20,21]. The Guidelines Oriented Approach to Lipid lowering (GOAL) study indicated the existence of gaps in physicians’ knowledge and actions, resulting in physicians not intensifying LLTs [22]. In another study [23], the LDL-C goal achievement rate was higher among patients whose physicians’ knowledge of LDL-C goals was consistent with guideline recommendations than among those with physicians whose knowledge was inconsistent with guideline recommendations (60.4% vs 31.1%, P < 0.0001). Although several strategies and tools exist to improve adherence to LLTs and attainment of guideline-recommended LDL-C levels, no single strategy has made a substantial impact, and only concurrent use of multiple implementation strategies was associated with a noticeable reduction in LDL-C [20, 24].
To improve current care for patients with ASCVD, the Clinician Engagement in Guideline-based Management of LDL ChOlesterol for Patients at HiGh Risk for a Future Atherosclerotic Cardiovascular Disease EveNt (LOGAN-CV) study was designed to determine whether a multifaceted, guideline-based intervention will affect clinician behaviors and/or clinical outcomes in adult patients with a recent myocardial infarction (MI) and LDL-C ≥ 70 mg/dl despite receiving statins. The rationale and methodology of the study are described in this article.
Methods
Study Design
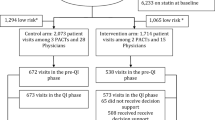
LOGAN-CV is a prospective, 12-month study to evaluate the effect of a multifaceted intervention on clinicians’ understanding of and adherence to current cholesterol guideline through evaluation of several guideline-based metrics (e.g., LDL-C < 70 mg/dl, LLT intensification, and appropriate LDL-C testing). The study started in October 2022 and is expected to be completed in March 2024. Details of study onboarding and interventions are listed in Fig. 1.
Study design of LOGAN-CV. Guideline refers to the 2018 AHA/ACC/Multisociety blood cholesterol guideline. aProportion of patients with an LDL-C testing order within 3 months of a change in LLT (aligned to guideline recommendations for LDL-C test within 4–12 weeks of a change in LLT) and proportion of patients with an LDL-C testing order within 12 months of no change in LLT and prior LDL-C < 70 mg/dl (aligned to guideline recommendations for LDL-C test within 3–12 months of change in LLT). bLLT titration within 3 months and within 12 months if LDL-C ≥ 70 mg/dl (per guidelines, increase in statin intensity or addition of non-statin LLT for each LDL-C ≥ 70 mg/dl). LLT intensification will be defined as any of the following changes: any statin intensification, addition of ezetimibe, addition of PCSK9i mAb, addition of bempedoic acid, addition of inclisiran, one medication change (defined as an increased dose or addition of new medication), two medication changes, or three medication changes. ACC American College of Cardiology, AHA American Heart Association, LDL-C low-density lipoprotein cholesterol, LLT lipid-lowering therapy, LOGAN-CV Clinician Engagement in Guideline-based Management of LDL ChOlesterol for Patients at HiGh Risk for a Future Atherosclerotic Cardiovascular Disease (ASCVD) EveNt, mAb monoclonal antibody, MI myocardial infarction, PCSK9i proprotein convertase subtilisin/kexin type 9 inhibitor
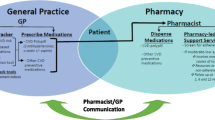
At the start of the study, clinicians will receive access to a web-based platform where they will review the guideline, patient risk factors, and a post-MI case study (Appendix 1). Clinicians are required to complete the modules to retain access to the platform, which will provide a summary of their LDL-C management performance and give access to online resources to support clinicians with desired behavior change and improve engagement with their patients. The data will be refreshed monthly (Fig. 2).
Each month, participating clinicians will receive a newsletter or article related to the study and/or management of LDL-C, including a link and reference to a relevant publication. Clinicians showing poor engagement or those who have a lower readiness to change, as demonstrated by their readiness assessments, will receive additional newsletters/articles.
All clinicians will be invited to four peer-to-peer calls during the 12-month study period, which will provide an opportunity to review their performance and engagement reports on the computer platform and identify successful centers or clinicians and prominent gaps in care. A recorded initial peer-to-peer call that provides a tour of the computer platform is available to clinicians on the platform.
Pre- and post-intervention surveys measuring clinicians’ knowledge, attitudes, and beliefs will be conducted at months 0 and 12 (Appendices 2 and 3, respectively). Clinicians will be classified based on the stages of change model [25]. Based on assessment of their readiness to change, clinicians will be provided with customizable engagement plans, including supplemental education and/or support, such as distribution of the 2022 ACC Expert Consensus Decision Pathway on LDL-C management, provision of additional articles, and support from an advisory committee member and/or a research team member.
An advisory committee consisting of national experts met at least quarterly during the study design phase. The advisory committee participated in study design review, protocol finalization, and educational content development and will serve as subject matter experts for peer-to-peer calls. The advisory committee evaluated the face validity of the knowledge, attitudes, and beliefs survey, which was also evaluated by clinician volunteers.
Sample Selection
The team will recruit up to ten healthcare systems to serve as research sites, focusing on large systems with a high MI volume along with those with cardiac rehabilitation programs and/or large cardiovascular centers. The target healthcare systems will have approximately 100 patients per research site (for a total of 1000 patients). Patients will be clustered by clinician. None of the qualified patients will have LDL-C < 70 mg/dl at baseline. The power to determine a difference in proportions was calculated using 100 clinicians, which is a conservative number given the 125 planned enrollments. This will accommodate loss due to clinicians not completing the required education. Details of the sample size calculation and underlying hypotheses and assumptions are provided in Supplementary Material, under Statistical analyses.
Clinicians (physicians of different specialties and advanced practice providers [APPs]) providing care for patients with recent MI will be enrolled in this study. Clinicians will be excluded from the study if they spend < 50% of their time at the research site or do not provide care for patients with recent MI.
Adult patients (aged ≥ 21 years) with an LDL-C level ≥ 70 mg/dl who have had an MI in the past 12 months, are receiving any dose of statin, and have had ≥ 1 outpatient visit in the previous year will be eligible for attribution to their participating clinician. Patients in hospice or end-of-life care and those dwelling in nursing homes will not be included in the study.
Measurements
LDL-C levels and LLT will be assessed at baseline and 3 and 12 months after the initiation of the clinician intervention. Changes or lack of changes in each outcome will be documented. LLT assessment will be based on the most recent medication at the end of each assessment period and reported in the following categories: high-intensity, moderate-intensity, and low-intensity statins; ezetimibe; PCSK9i mAb; bempedoic acid; inclisiran; and intensive/combination LLT (defined as any statin plus a non-statin LLT). The baseline assessment will include only medication changes after MI.
Figure 3 illustrates the performance measures clinicians are able to view on the computer platform. In addition, the platform will contain data on each clinician’s patterns of prescribing LLTs by category. Platform engagement, measured by logins, page views, and time spent on the platform, will also be monitored.
Clinicians’ knowledge, attitudes, and beliefs changes will be determined by comparing baseline and 12-month survey responses. Clinician behavior in response to the intervention will be assessed through a surrogate measure of clinical metrics (optimization of LDL-C control, defined as LDL-C < 70 mg/dl, LLT intensification, and appropriate LDL-C testing follow-up) at the clinician level, site level, and overall study level.
Planned Outcomes
The primary endpoint will be the change in the proportion of patients with an LDL-C level < 70 mg/dl achieved at any time during the 12-month intervention. All secondary and exploratory endpoints are listed in Fig. 1.
Data Collection
The primary source of qualified patient data will be the research site’s clinical records systems, including billing systems and electronic medical record (EMR) systems. Files including demographic, billing, and identifiable clinical data will be transferred in a secure manner to the study team that will manage the performance management platform.
Clinicians will be followed-up during the 12-month intervention period. If a clinician moves away or switches practice within 3 months of intervention initiation, the clinician will be considered lost to follow-up and their data will not be included in the final analysis. Clinicians who do not complete the required educational modules within 6 weeks of study initiation will lose access to the platform and will be considered lost to follow-up, and their data will not be included in the final analysis.
Patients’ baseline data up to 1 year before their clinicians’ enrollment into the study will be collected by data extraction from the EMRs from the time their clinicians are enrolled through the end of the 12-month intervention. Clinicians who provided consent will receive access to the platform to complete the required educational modules after completing the pre-intervention survey. They will also participate in periodic peer-to-peer calls and use the platform to monitor their performance before completing the postintervention survey at month 12. If a clinician withdraws from the study, their data up to the withdrawal date will be included; however, no future data for the clinician or their attributed patients will be included.
Clinicians’ knowledge, attitudes, and beliefs related to LDL-C management will be assessed at baseline and 12 months after the start of the intervention. In both pre- and post-intervention surveys, questions will assess guideline knowledge (including questions on two case studies); attitudes and beliefs regarding the guideline, and clinicians’ treatment practices and readiness to change treatment behavior. The pre-intervention survey will also collect demographic and practice information. The postintervention survey will also measure clinicians’ view of the effectiveness of LLT strategies and potential reasons for not achieving the recommended LDL-C level.
Data Analysis
With a nominal alpha of 0.05, this study will have > 99% power to detect an increase in the percentage of patients with LDL-C < 70 mg/dl as small as 10% vs baseline of 0.01% (0% cannot be used in the calculation). We will also test whether the intervention results in a larger improvement in the percentage of patients achieving LDL-C < 70 mg/dl than that observed at 2 years in the non-interventional GOULD study [5]. The current study will have 90% power to detect a difference as small as 13% higher (i.e., postintervention LDL-C < 70 mg/dl of 25%) than the 12% estimated control rate at 1 year in the GOULD study (24%/2 years) and 91% power to detect a difference as small as 16% higher (i.e., postintervention LDL-C < 70 mg/dl of 40%) than the 24% observed control rate at 2 years in the GOULD study [5, 26]. An interim analysis has been planned after 6 months of data collection. After 12 months, the final analysis will include clinical outcomes and qualitative analysis of peer-to-peer calls for trends and themes. Several covariates will be assessed, including site characteristics, clinician characteristics, and patient characteristics. Outliers for underutilization of the platform assessed by access will be evaluated for exclusion from data analysis. A sensitivity analysis of key outcomes will be performed that will include only clinicians with reasonable engagement levels.
Patient demographic and clinical characteristics will be summarized by assessment point (baseline, 3 months, and 12 months after the start of the intervention). Continuous variables will be expressed as mean ± standard deviation or median and interquartile range, and two-group comparisons will be tested using paired t tests or Wilcoxon signed-rank tests, as appropriate. Categorical variables will be expressed as frequency counts and percentages and comparisons between time points will be tested using McNemar’s, chi-square, or Fisher’s exact tests as appropriate.
For missing and incomplete data, the study team will undertake efforts to obtain the data from the research sites. If data are still missing or incomplete, appropriate methods, including data imputation, may be used to handle missing values. Missing data (e.g., no LDL-C measurements within 3 months or within 12 months) will be handled conservatively as non-achievement or non-adherence. Regression analysis, sensitivity analysis, subgroup analysis, and covariate assessment will be performed as necessary (Supplementary Material).
Study Importance
Results from cumulative LDL-C exposure over the lifetime [27, 28] during LLT with statins [29] and non-statins [30,31,32,33] have demonstrated ~ 21%–23% decrease in ASCVD events per each 38.7 mg/dl reduction in LDL-C level, with no lower limit at which the benefit ceases to exist [3, 34]. Moreover, earlier vs later intensive LLT initiation has a positive impact on outcomes [3, 35,36,37].
Based on this evidence, current guidelines across the world support intensive LLT to achieve ≥ 50% LDL-C reduction and LDL-C levels of < 55 mg/dl for patients with VHR ASCVD [1, 3, 38, 39]. Unfortunately, multiple studies have shown lack of adherence to guidelines with resulting poor achievement of LDL-C goals [19, 40,41,42]. In a retrospective US study of 16,344 patients with a history of a major ASCVD event in the MarketScan database, although 94% of patients fulfilled the VHR criteria, 67% had an LDL-C level ≥ 70 mg/dl, therefore remaining at increased risk for recurrent events [43]. In the GOULD observational registry, only 32% of patients with ASCVD achieved an LDL-C level < 70 mg/dl over 2 years, and only 15% achieved an LDL-C level < 55 mg/dl; LLT intensification occurred in only 17% of patients, and 11% did not have a lipid panel performed over the 2 years [5].
Clinicians’ lack of awareness and familiarity with guidelines are important barriers preventing the implementation of and adherence to clinical guidelines [19]. In one study, the most common reason cited by physicians for treating patients with a lower intensity of statin than that recommended by the guideline was LDL-C being stable or “at goal” [27]. This highlights the need for physician education on the importance of maximizing LLT in patients with ASCVD [26] and achieving the lowest LDL-C levels possible [27, 28]. Clinician education, such as the modules developed for the LOGAN-CV study, can help overcome clinical inertia, support clinicians in providing guideline-based LLT, and, ultimately, enable patients to achieve recommended LDL-C levels. Other potentially successful strategies to change clinician behavior involve structured EMR prompts and interventions [44] as well as deployment of LDL-C quality metrics, as recently recommended by the National Lipid Association and the American Society for Preventive Cardiology [21].
Strengths and Limitations
The strengths of this study include use of a multifaceted intervention; availability of clinician-specific, guideline-based metrics for clinicians to view their own patients’ data; and a large sample of clinicians included in the study. LOGAN-CV will enroll a variety of clinicians who manage patients with ASCVD and will use customized engagement plans to facilitate guideline implementation. Use of a performance platform with real-time assessment of outcomes will provide the opportunity for course correction for low-performing clinicians. The study includes assessment of clinician knowledge, attitudes, and beliefs; these pre- and post-intervention surveys were developed, tested, and validated by an expert advisory committee.
This study has several limitations. First, the study design evaluates improvement in clinician performance without a control group. Second, as this study is targeting large healthcare systems, included patient and clinician samples may not represent those at smaller systems or private practices. Additionally, external validity of the study may be restricted to healthcare systems with care team constructs similar to those included in the study. Third, this study will include only clinical data collected from EMR. Lifestyle changes and other factors not reported in the EMR may affect achievement of the LDL-C level and other outcomes. Finally, LDL-C control was based on the 2018 guideline recommendation of < 70 mg/dl for patients with VHR ASCVD, which was recently updated to < 55 mg/dl [3].
Ethics and Dissemination
The study received approval from a central institutional review board (IRB). The IRB waived the requirement for patient consent. If a site is unable to use the central IRB, local IRB approval will be sought. Clinicians will have the right to withdraw from the study at any time and for any reason. The study will be performed in accordance with the principles of the Declaration of Helsinki.
Currently, clinicians are being enrolled in the LOGAN-CV study, and the pre-intervention knowledge, attitudes, and beliefs survey is being administered. Future publications from the LOGAN-CV study will report the baseline data and final results.
Conclusions
The LOGAN-CV study addresses a critical unmet need in LDL-C control in patients with VHR ASCVD, evaluating the effect of a multifaceted clinician intervention on improving clinicians’ adherence to guideline recommendations and on improving clinical outcomes for patients with VHR ASCVD with a recent MI and LDL-C ≥ 70 mg/dl despite statin treatment. The clinician education modules developed for the LOGAN-CV study can help in overcoming clinical inertia, support clinicians in providing guideline-based LLT, and enable patients to achieve recommended LDL-C levels.
References
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1082–143.
Grundy SM, Stone NJ. 2018 American Heart Association/American College of Cardiology/Multisociety Guideline on the Management of Blood Cholesterol-Secondary Prevention. JAMA Cardiol. 2019;4(6):589–91.
Lloyd-Jones DM, Morris PB, Ballantyne CM, Birtcher KK, Covington AM, DePalma SM, Minissian MB, Orringer CE, Smith SC Jr, Waring AA, Wilkins JT. 2022 ACC Expert Consensus Decision Pathway on the Role of Nonstatin Therapies for LDL-Cholesterol Lowering in the Management of Atherosclerotic Cardiovascular Disease Risk: a Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022;80(14):1366–418.
Ferhatbegović L, Mršić D, Kušljugić S, Pojskić B. LDL-C: the only causal risk factor for ASCVD. Why is it still overlooked and underestimated? Curr Atheroscler Rep. 2022;24(8):635–42.
Cannon CP, de Lemos JA, Rosenson RS, Ballantyne CM, Liu Y, Gao Q, Palagashvilli T, Alam S, Mues KE, Bhatt DL, Kosiborod MN. Use of lipid-lowering therapies over 2 years in GOULD, a registry of patients with atherosclerotic cardiovascular disease in the US. JAMA Cardiol. 2021;6(9):1060–8.
Ray KK, Molemans B, Schoonen WM, Giovas P, Bray S, Kiru G, Murphy J, Banach M, De Servi S, Gaita D, et al. EU-wide cross-sectional observational study of lipid-modifying therapy use in secondary and primary care: the DA VINCI study. Eur J Prev Cardiol. 2021;28(11):1279–89.
Talic S, Marquina C, Zomer E, Ofori-Asenso R, Petrova M, Vargas-Torres S, Abushanab D, Wolfe R, Lybrand S, Thomson D, et al. Attainment of low-density lipoprotein cholesterol goals in statin treated patients: real-world evidence from Australia. Curr Probl Cardiol. 2022;47(7):101068.
Schwarz A, Demuth I, Landmesser U, Haghikia A, König M, Steinhagen-Thiessen E. Low-density lipoprotein cholesterol goal attainment in patients with clinical evidence of familial hypercholesterolemia and elevated Lp(a). Lipids Health Dis. 2022;21(1):114.
Meier R, Rachamin Y, Rosemann T, Markun S. The impact of the 2019 European guideline for cardiovascular risk management: a cross-sectional study in general practice. J Clin Med. 2020;9(7):2140.
Makhmudova U, Wolf M, Willfeld K, Beier L, Weingärtner O. Different perspectives of patients and physicians on LDL-C target achievement in the treatment of hypercholesterolemia: results on secondary prevention from the German PROCYON survey. Adv Ther. 2023;40(2):460–73.
Fox KM, Tai MH, Kostev K, Hatz M, Qian Y, Laufs U. Treatment patterns and low-density lipoprotein cholesterol (LDL-C) goal attainment among patients receiving high- or moderate-intensity statins. Clin Res Cardiol. 2018;107(5):380–8.
Offiah G, O’Connor C, Kennedy C, Gallagher J, O’Connor P, McAdam B, Ray KK, Schoonen M, Maher V. The DA VINCI study: is Ireland achieving ESC/EAS guideline-directed LDL-C goals? Ir J Med Sci. 2023;192(3):1077–84.
van de Borne P, Peeters A, Janssens L, Leone A, Lemmens R, Verhaegen A, De Meulemeester M, Balthazar Y, Heijmans S, Calozet Y, et al. Lipid-lowering therapy and risk-based LDL-C goal attainment in Belgium: DA VINCI observational study. Acta Cardiol. 2022. https://doi.org/10.1080/00015385.2022.2030568.
Siostrzonek P, Brath H, Zweiker R, Drexel H, Hoelzl R, Hemetsberger M, Ray KK. Lipid lowering therapy in primary and secondary prevention in Austria: are LDL-C goals achieved?: results from the DA VINCI study. Wien Klin Wochenschr. 2022;134(7–8):294–301.
Vrablik M, Seifert B, Parkhomenko A, Banach M, Jóźwiak JJ, Kiss RG, Gaita D, Rašlová K, Zachlederova M, Bray S, Ray KK. Lipid-lowering therapy use in primary and secondary care in Central and Eastern Europe: DA VINCI observational study. Atherosclerosis. 2021;334:66–75.
De Backer G, Jankowski P, Kotseva K, Mirrakhimov E, Reiner Ž, Rydén L, Tokgözoğlu L, Wood D, De Bacquer D. Management of dyslipidaemia in patients with coronary heart disease: results from the ESC-EORP EUROASPIRE V survey in 27 countries. Atherosclerosis. 2019;285:135–46.
Gouni-Berthold I, Schaper F, Schatz U, Tabbert-Zitzler A, Fraass U, Sauer S, Ray KK. Low-density lipoprotein cholesterol goal attainment in Germany: results from the DA VINCI study. Atheroscler Plus. 2022;50:10–6.
Gold ME, Nanna MG, Doerfler SM, Schibler T, Wojdyla D, Peterson ED, Navar AM. Prevalence, treatment, and control of severe hyperlipidemia. Am J Prev Cardiol. 2020;3: 100079.
Underberg J, Toth PP, Rodriguez F. LDL-C target attainment in secondary prevention of ASCVD in the United States: barriers, consequences of nonachievement, and strategies to reach goals. Postgrad Med. 2022;134(8):752–62.
Desai NR, Farbaniec M, Karalis DG. Nonadherence to lipid-lowering therapy and strategies to improve adherence in patients with atherosclerotic cardiovascular disease. Clin Cardiol. 2023;46(1):13–21.
Virani SS, Aspry K, Dixon DL, Ferdinand KC, Heidenreich PA, Jackson EJ, Jacobson TA, McAlister JL, Neff DR, Gulati M, Ballantyne CM. The importance of low-density lipoprotein cholesterol measurement and control as performance measures: a joint clinical perspective from the National Lipid Association and the American Society for Preventive Cardiology. Am J Prev Cardiol. 2023;13:100472.
Langer A, Tan M, Goodman SG, Grégoire J, Lin PJ, Mancini GBJ, Stone JA, Wills C, Spindler C, Leiter LA. GOAL Canada: physician education and support can improve patient management. CJC Open. 2020;2(2):49–54.
Ding R, Ye P, Zhao S, Zhao D, Yan X, Dong Y, Li J, Ran Y, Hu D. Effect of physician characteristics and knowledge on the quality of dyslipidemia management and LDL-C target goal achievement in China: subgroup analysis of the Dyslipidemia International Study. J Glob Health. 2017;7(2): 020702.
Jones LK, Tilberry S, Gregor C, Yaeger LH, Hu Y, Sturm AC, Seaton TL, Waltz TJ, Rahm AK, Goldberg A, et al. Implementation strategies to improve statin utilization in individuals with hypercholesterolemia: a systematic review and meta-analysis. Implement Sci. 2021;16(1):40.
DiClemente CC, Prochaska JO. Toward a comprehensive, transtheoretical model of change: stages of change and addictive behaviors. New York: Plenum Press; 1998.
Cannon CP, de Lemos JA, Rosenson RS, Ballantyne CM, Liu Y, Yazdi D, Elliott-Davey M, Mues KE, Bhatt DL, Kosiborod MN. Getting to an Improved Understanding of Low-Density Lipoprotein-Cholesterol and Dyslipidemia Management (GOULD): methods and baseline data of a registry of high cardiovascular risk patients in the United States. Am Heart J. 2020;219:70–7.
Toth PP. Low-density lipoprotein cholesterol treatment rates in high risk patients: more disappointment despite ever more refined evidence-based guidelines. Am J Prev Cardiol. 2021;6:100186.
Shapiro MD, Bhatt DL. “Cholesterol-years” for ASCVD risk prediction and treatment. J Am Coll Cardiol. 2020;76(13):1517–20.
Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, Peto R, Barnes EH, Keech A, Simes J, Collins R. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670–81.
Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, Kuder JF, Wang H, Liu T, Wasserman SM, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376(18):1713–22.
Schwartz GG, Steg PG, Szarek M, Bhatt DL, Bittner VA, Diaz R, Edelberg JM, Goodman SG, Hanotin C, Harrington RA, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018;379(22):2097–107.
Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, Darius H, Lewis BS, Ophuis TO, Jukema JW, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372(25):2387–97.
Nissen SE, Lincoff AM, Brennan D, Ray KK, Mason D, Kastelein JJP, Thompson PD, Libby P, Cho L, Plutzky J, et al. Bempedoic acid and cardiovascular outcomes in statin-intolerant patients. N Engl J Med. 2023;388(15):1353–64.
Sabatine MS, Wiviott SD, Im K, Murphy SA, Giugliano RP. Efficacy and safety of further lowering of low-density lipoprotein cholesterol in patients starting with very low levels: a meta-analysis. JAMA Cardiol. 2018;3(9):823–8.
O’Donoghue ML, Giugliano RP, Wiviott SD, Atar D, Keech A, Kuder JF, Im K, Murphy SA, Flores-Arredondo JH, López JAG, et al. Long-term evolocumab in patients with established atherosclerotic cardiovascular disease. Circulation. 2022;146(15):1109–19.
Martinez L, Multani JK, Sun K, Kalich BA, Miglins M.L., Sidelnikov E, Baber U: Timing of PCSK9i initiation and its relationship with clinical outcomes in US patients with prior cardiovascular events: a claims database analysis. In National Lipid Association Scientific Sessions; June 1–4, 2023; Atlanta, GA2023: s.
Lewek J, Niedziela J, Desperak P, Dyrbuś K, Osadnik T, Jankowski P, Witkowski A, Bielecka-Dąbrowa A, Dudek D, Gierlotka M, et al. Intensive statin therapy versus upfront combination therapy of statin and ezetimibe in patients with acute coronary syndrome: a propensity score matching analysis based on the PL-ACS data. J Am Heart Assoc. 2023;12(18): e030414.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, Chapman MJ, De Backer GG, Delgado V, Ference BA, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–88.
Samson SL, Vellanki P, Blonde L, Christofides EA, Galindo RJ, Hirsch IB, Isaacs SD, Izuora KE, Low Wang CC, Twining CL, et al. American Association of Clinical Endocrinology Consensus Statement: comprehensive type 2 diabetes management algorithm—2023 update. Endocr Pract. 2023;29(5):305–40.
Barrios V, Soronen J, Carter AM, Anastassopoulou A. Lipid management across Europe in the real-world setting: a rapid evidence review. Curr Med Res Opin. 2021;37(12):2049–59.
Bruckert E, Parhofer KG, Gonzalez-Juanatey JR, Nordestgaard B, Arca M, Giovas P, Ray K. Proportion of high-risk/very high-risk patients in europe with low-density lipoprotein cholesterol at target according to European guidelines: a systematic review. Adv Ther. 2020;37(5):1724–36.
Navar AM, Wang TY, Li S, Robinson JG, Goldberg AC, Virani S, Roger VL, Wilson PWF, Elassal J, Lee LV, Peterson ED. Lipid management in contemporary community practice: results from the Provider Assessment of Lipid Management (PALM) Registry. Am Heart J. 2017;193:84–92.
Muntner P, Orroth KK, Mues KE, Exter J, Shannon ED, Zaha R, Rosenson RS, Jackson EA. Evaluating a simple approach to identify adults meeting the 2018 AHA/ACC cholesterol guideline definition of very high risk for atherosclerotic cardiovascular disease. Cardiovasc Drugs Ther. 2022;36(3):475–81.
Shah NN, Ghazi L, Yamamoto Y, Martin M, Simonov M, Riello RJ, Faridi KF, Ahmad T, Wilson FP, Desai NR. Rationale and design of a pragmatic trial aimed at improving treatment of hyperlipidemia in outpatients with very high risk atherosclerotic cardiovascular disease: a pragmatic trial of messaging to providers about treatment of hyperlipidemia (PROMPT-LIPID). Am Heart J. 2022;253:76–85.
Medical Writing, Editorial, and Other Assistance.
Medical writing assistance was provided by Sarayu Pai, PhD, CMPP, of Cactus Life Sciences (part of Cactus Communications), Ellen Stoltzfus, PhD, of Amgen Inc., and Martha Mutomba, PhD, on behalf of Amgen Inc. and was funded by Amgen according to Good Publication Practice guidelines.
Funding
This research is sponsored by Amgen Inc., Thousand Oaks, CA. Rapid Service Fee and Open Access Fee for this article were paid by Amgen Inc.
Author information
Authors and Affiliations
Contributions
Conceptualization: J. Nikki McKoy, Bethany A. Kalich, Laura Greene, Rachel H. Mackey, Ning A. Rosenthal, Yosef Khan, Jenna Jones, and Leslie A. Carabuena; Data curation: Rachel H. Mackey, Ning A. Rosenthal, and Leslie A. Carabuena; Formal analysis: Rachel H. Mackey, Ning A. Rosenthal, and Leslie A. Carabuena; Investigation: J. Nikki McKoy, Laura Greene, and Yosef Khan; Methodology: J. Nikki McKoy, Bethany A. Kalich, Laura Greene, Rachel H. Mackey, Ning A. Rosenthal, Yosef Khan, and Leslie A. Carabuena; Project administration: J. Nikki McKoy, Laura Greene, and Yosef Khan; Resources: J. Nikki McKoy, Laura Greene, Ning A. Rosenthal and Yosef Khan; Supervision: J. Nikki McKoy, Laura Greene, and Yosef Khan; Validation: Rachel H. Mackey, Ning A. Rosenthal, and Leslie A. Carabuena; Writing, review, interpretation, and editing: J. Nikki McKoy, Bethany A. Kalich, Laura Greene, Rachel H. Mackey, Ning A. Rosenthal, Yosef Khan, Cezary Wójcik, Jenna Jones, and Leslie A. Carabuena.
Corresponding author
Ethics declarations
Conflict of Interest
J. Nikki McKoy, Laura Greene, Rachel H. Mackey, Ning A. Rosenthal, Yosef Khan, and Leslie A. Carabuena are full-time employees of Premier, Inc., which received payment from Amgen to conduct the study, but have no competing interests with respect to the study. Bethany A. Kalich, Cezary Wójcik, and Jenna Jones are employees of Amgen Inc. and may be Amgen stockholders at the time of publication.
Ethical Approval
The study received approval from a central institutional review board (IRB). The IRB waived the requirement for patient consent. If a site is unable to use the central IRB, local IRB approval will be sought. Clinicians will have the right to withdraw from the study at any time and for any reason. The study will be performed in accordance with the principles of the Declaration of Helsinki.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
McKoy, J.N., Kalich, B.A., Greene, L. et al. LOGAN-CV: A Prospective Study of a Multifaceted Intervention Targeting United States Clinicians to Improve Guideline-Based Management of Lipid-Lowering Therapy. Adv Ther 41, 451–463 (2024). https://doi.org/10.1007/s12325-023-02716-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02716-6