Abstract
Introduction
The coronavirus disease 2019 (COVID-19) pandemic created challenges related to disease management of patients with ulcerative colitis (UC).
Methods
The UC Narrative COVID-19 survey was conducted from August to December 2021 among adults with UC from the United States, Canada, Japan, France, and Finland. Patients were questioned on disease management, health care access and experience, and preferences for interactions with their doctor. Data were analyzed descriptively.
Results
In total, 584 patients qualified for and completed the survey. Compared with 2019, 25% experienced more flares during the pandemic (from early 2020). Most patients (88%) taking prescription medication were very/somewhat satisfied with their current treatment plan; 53% were hesitant to make changes during the pandemic. Factors that patients agreed helped control UC symptoms during the pandemic included fewer social outings (37%), working from home (29%), and less busy schedules (28%). Greater anxiety/stress (43%) and hesitancy to visit a hospital/office (34%) made the control of UC symptoms more difficult. Compared with 2019, more patients relied on certain alternative support systems during the pandemic. Patients who used in-person and virtual appointments were equally very satisfied/satisfied with the quality of care (both 81%). In-person appointments were preferred by 68% of patients when meeting a new doctor, 55% when experiencing a flare, and 52% for regular check-ups; 41% preferred virtual appointments for UC prescription refills.
Conclusion
During the pandemic, most patients were satisfied with their current UC treatment plan and access to care; more patients relied on certain alternative UC management support systems, and many were impacted by anxiety/stress.
Graphical Abstract

Plain Language Summary
The coronavirus disease 2019 (COVID-19) pandemic created challenges for patients with ulcerative colitis. These challenges included managing symptoms, lifestyle changes, and access to health care. We asked patients with ulcerative colitis to answer questions about their experience during the pandemic to try to understand how the pandemic was affecting them. A total of 584 patients from the United States, Canada, Japan, France, and Finland took part. Patients were asked questions online. We asked them about their disease activity during the COVID-19 pandemic compared with before the pandemic and how their disease was managed, their access to health care, and their experience during the pandemic. We also asked them about their satisfaction with the types of appointments they had during the pandemic (for example, in-person or virtual meetings), and their interactions and preference for interactions with their doctors. We found that most patients were satisfied with their current treatment plan, their access to health care, and the quality of the care they received. However, many patients experienced greater stress or anxiety, and there was a negative impact on their emotional well-being. During the pandemic, more patients relied on alternative support systems such as online patient portals or virtual appointments, but patients preferred in-person appointments with their doctors in most cases except for refilling prescriptions. This information may help doctors understand the impact of the COVID-19 pandemic on patients with ulcerative colitis, and may help doctors and patients develop treatment plans that include both in-person and virtual appointments.
AbstractSection Graphical Plain Language Summary
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The COVID-19 pandemic has amplified the negative impact of ulcerative colitis (UC) on patients’ quality of life and affected access to health care. |
This global survey aimed to understand how the COVID-19 pandemic impacted patients with UC and assessed overall disease management, health care experience and preferences, and emotional well-being. |
What was learned from the study? |
Most patients were satisfied with their current UC treatment plan, and more used certain alternative support systems, but many were negatively impacted by anxiety/stress. |
The adoption of a hybrid model of patient–doctor interactions that incorporates both virtual and in-person appointments could lead to improvements in how patients manage their disease. |
Lessons from the pandemic can be applied to the post-pandemic era to introduce meaningful improvements to clinical practice. |
Digital Features
This article is published with digital features, including a graphical abstract and graphical plain language summary, to facilitate your understanding of this article. To view this digital feature, go to https://doi.org/10.6084/m9.figshare.24064806.
Introduction
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD), and patients with moderately or severely active disease often require long-term treatment/management with immunosuppressive therapies [1]. Patients with IBD commonly report impaired health-related quality of life that is linked to psychological distress resulting from the physical and mental burden of UC [2]. The coronavirus disease 2019 (COVID-19) global pandemic served to amplify the negative impact of IBD on patients’ quality of life, exacerbating anxieties related to physical health, perceived risks associated with the use of immunomodulating therapies, access to health care, and other uncertainties related to the pandemic [3,4,5]. Additionally, the redeployment of health care resources during the pandemic has led to an increased reliance on telehealth and the emergence of contactless health care tools to monitor and manage patients with chronic diseases such as IBD [5,6,7,8].
Although previous studies have examined the effects of the COVID-19 pandemic on patients with IBD, it is important to understand the impact of changes to the provision of care on patients with UC. The first UC Narrative global survey, the results of which have been previously published, was conducted in 10 countries between 2017 and 2018, and examined patient and doctor experiences with UC, including day-to-day disease impact, disease management, goal-setting, and communication [9, 10]. Here, we report the results of a recent, separate global UC Narrative COVID-19 survey, conducted during the pandemic (August–December 2021), of patients with UC in the United States (US), Canada, Japan, France, and Finland. The aim was to understand how the COVID-19 pandemic impacted patients with UC; it also assessed overall disease management, behaviors around telehealth, health care experience, perceived quality of care, emotional well-being, reliance on alternative support systems, and preferences for virtual and in-person interactions with doctors they see for their UC.
Methods
Study Design and Patient Population
The UC Narrative is a collaborative global initiative that is directed by an advisory panel comprising adults living with UC, gastroenterologists, IBD nurses, a psychologist, and representatives of IBD patient advocacy organizations from multiple countries. The goal of the UC Narrative is to improve outcomes for people living with UC internationally by identifying how they are impacted by the disease, as well as common and country-specific barriers to better care, while proposing solutions to overcome these barriers. The methodology for the analysis of survey responses has been described previously [9, 10].
The UC Narrative COVID-19 survey reported here was conducted online by The Harris Poll between August 25 and December 13, 2021, among patients with UC who reside in the US, Canada, Japan, France, and Finland. Patients were asked to recall their experiences pre-pandemic (2019) and during the pandemic (starting early 2020). The survey was conducted among eligible patients who were either members of online panels who had agreed to participate in survey research or through the membership of local patient advocacy groups. All participants provided informed consent. The sampling precision of the survey was measured using a Bayesian credible interval. Eligible patients were aged ≥ 18 years and had a prior diagnosis of UC that was confirmed by colonoscopy or flexible sigmoidoscopy. Patients must not have undergone a colectomy, were required to have seen someone at a gastroenterologist’s or internist’s office in the past 3 years (e.g., nurse, primary care physician, nutritionist, or other health care professional) and must have ever taken any prescription medication for their UC other than only 5-aminosalicylates (5-ASAs).
Patients with UC of any severity were eligible for participation, and the use of prescription medication was used as a proxy for UC severity. Patients with milder UC were defined as those who had ever taken a prescription medication for their UC (excluding those who had only ever taken 5-ASAs, as they were defined as having mild disease), had taken corticosteroids for < 4 of the past 12 months, and had never taken biologic or immunosuppressant therapy. Conversely, patients with moderate to severe UC were defined as those who had ever taken a biologic or immunosuppressant for their UC or had taken corticosteroid treatment for ≥ 4 of the past 12 months.
Ethical Considerations
Patient recruitment was performed from online market research panels consisting of members who agreed to participate in this type of research. Patients provided their consent before completing the questionnaire and received remuneration (on behalf of the investigators by the sponsor) for their participation in the survey. The survey was non-interventional and was not conducted as a clinical study; therefore, all patients agreed to participate but ethics approval was not required.
Survey Outcomes
Survey questions (listed in full in the electronic Supplementary Material) were focused on four main aspects of UC, namely (1) disease activity, (2) disease management, (3) health care access and experience (e.g., ease of scheduling and length of appointment), and (4) patient preference for interactions with their doctor. Disease activity was assessed according to the comparative number of patient-reported flares, defined as a period with a dramatic increase in symptoms compared with those typically experienced. Patients’ disease activity during the pandemic (beginning in early 2020) compared with 2019 (i.e., before the COVID-19 pandemic) was recorded. Additionally, patient-reported remission status was captured and defined as the control of UC with few to no symptoms. Patients’ experience of their disease was also measured in terms of satisfaction with their current treatment plan and any instances of settling behavior, defined as the proportion of patients who agreed with the statement, “If my treatment makes me feel good enough, I don’t see a need to consider other treatment options, even if they might make me feel better than I do now.” Other elements that helped with an understanding of patients’ disease experience included an assessment of overall health, as reported by patients and the proportion who agreed with the statement, “I feel that UC controls my life, rather than me controlling the disease.”
Survey questions on disease management during the pandemic centered around patients’ timing of reliance on other support for UC management (e.g., virtual appointments, patient portals, symptom-tracking applications, and patient support/advocacy groups [defined as alternative support systems]), changes to their UC treatment plan, factors that made the control of UC symptoms easier or more difficult, and feelings of isolation associated with disease management. Access to health care included patient-reported challenges with accessing the health care needed before and during the COVID-19 pandemic (e.g., “difficulty getting an appointment with a specialist for my UC,” “difficulty in getting time off work to go to appointments with my doctor,” and “lack of conveniently located medical care”), satisfaction with their ability to access the health care needed during the pandemic, and the quality of communication with their doctor. Patients were also asked to express their preferences for, and satisfaction with, various aspects of in-person or virtual appointments with their doctor according to the nature of the medical appointment.
Statistical Analysis
The survey responses were analyzed globally. Descriptive statistics were used to assess patient responses, and post-weighting was used for the global, five-country total to adjust for the relative size of each country’s adult population within the total adult population across all countries surveyed [11]. The unweighted sample sizes reflected the total number of patients who completed the survey in each country, while all reported percentages were calculated based on the weighted global total. Proportionate weighting to combine multi-country data into a single total is a common practice because it relies on externally recognized population data to achieve a global total that more accurately represents the real-world patient population relative to the adult populations surveyed. Raw data were not weighted at the individual country level and were therefore only representative of the individuals who completed the survey. As the sample was collected in a non-probability manner, we used a standard uninformed conjugate prior distribution for percentage data of a Beta (1,1) distribution for Bayesian credible intervals [12]. This prior distribution, when combined with the binomial data, produced a posterior distribution with a precision of within ± 6.1% to the true population value for the corresponding credible interval.
Results
Patient Demographics and Disease Characteristics
In total, 584 patients completed the survey: 100 (US), 100 (Canada), 100 (Japan), 100 (France), and 184 (Finland). Overall, 47% of the patients were female, and the mean age of the respondents was 46.7 years [standard deviation (SD) 14.4 years], with the majority (65%) aged under 50 years. Nearly half (46%) of the patients had ever received tumor necrosis factor inhibitor (TNFi) therapy for their UC, and 81% of patients had moderate to severe disease (Table 1). Patients had been diagnosed with UC for a mean of 10.8 years (SD 11.3 years).
Disease Activity and Patient Profile During the COVID-19 Pandemic
Globally, 25% of patients reported they experienced more flares since the beginning of the COVID-19 pandemic in early 2020, compared with 2019, while 18% of patients experienced fewer flares over the same period (based on recall of their experience). The proportions of patients reporting more flares, stratified by subgroups of interest (gender, age, urbanicity, and experience of challenges accessing health care), are shown in Fig. S1a in the electronic Supplementary Material. Patients more likely to report more flares were aged 18–49 years versus ≥ 50 years and those who had ever experienced challenges accessing the health care needed versus those who had not. In total, 61% of patients had ever experienced challenges accessing the health care needed.
During the pandemic, over half of patients (57%) reported excellent or good overall health (Fig. 1a), and 64% considered their UC to be in remission (Fig. 1b). Overall, 88% of respondents taking prescription medication were very satisfied or somewhat satisfied with their current UC treatment plan (36% were very satisfied; 53% were somewhat satisfied) (Fig. 1c). However, overall, 60% of all patients said they would not see a need to consider other treatment options and would settle for treatment that made them feel good enough, even if other treatment options might make them feel better than they did at the time (Fig. 1d).
Patient-reported a overall healtha and b remission status and duration of remission or years since remission,b and the proportion of patients reporting c satisfaction with their current treatment plan (among those currently taking prescription medication),c d settling behavior,d and e agreement that UC controls their lifee. Percentages may not sum to 100% due to weighting and/or computer rounding. UC ulcerative colitis. aQuestion: “How would you describe your current overall health?” bQuestions: “Do you currently consider your UC to be in remission (when we say remission, we mean that your disease is controlled with few to no symptoms)?” “How long has your UC been in remission?” “How long has it been since your UC was last in remission?” cQuestion: “You indicated you are currently taking prescription medication for your UC. How satisfied are you with your current UC treatment plan?” dAgreement with the statement, “If my treatment makes me feel good enough, I don’t see a need to consider other treatment options, even if they might make me feel better than I do now.” eAgreement with the statement, “I feel that my UC controls my life, rather than me controlling the disease”
In total, 56% of respondents agreed with the statement, “I feel that UC controls my life rather than me controlling the disease,” with 20% strongly agreeing (Fig. 1e). Patients aged 18–49 years were more likely to agree with this statement than patients aged ≥ 50 years, as were patients who had previously experienced challenges accessing the health care needed versus those who had not and those patients who reported more flares during the pandemic than in 2019 versus those who reported the same or less number of flares (see Fig. S1b in the electronic Supplementary Material).
Aspects of Disease Management During the COVID-19 Pandemic
The aspects of UC management that were most negatively impacted by the COVID-19 pandemic were emotional well-being and the ability to perform daily activities. Aspects of UC related to the use of prescription medications appeared to be the least affected by the pandemic (Table 2).
Globally, patients reported that having fewer social outings (37%), working from home (29%), having less busy schedules (28%), and having more time to focus on their overall health (26%) made it easier to control their symptoms during the pandemic (Fig. 2a). However, 30% of the survey respondents reported that nothing made it easier to control their UC symptoms during the pandemic (Fig. 2a). Conversely, respondents reported that anxiety/stress (43%), hesitancy to go into a hospital or office to receive care or treatment (34%), and not being able to get an appointment (23%) made it more difficult to control their UC symptoms during the pandemic (Fig. 2b). In total, 26% of patients felt that nothing made it more difficult to control symptoms during the pandemic (Fig. 2b).
Factors that made the control of UC symptoms a easier and b more difficult during the COVID-19 pandemica. COVID-19 coronavirus disease 2019, UC ulcerative colitis. aQuestion: “Do you think any of the following have made it easier/more difficult to control your symptoms during the COVID-19 pandemic? Please select all that apply”
Just under half of patients globally (47%) agreed that they felt more isolated and alone in managing their UC during the COVID-19 pandemic, with 17% strongly agreeing and 30% somewhat agreeing. Patients more likely to agree with this statement were aged 18–49 years versus ≥ 50 years, residing in inner city, urban, or suburban areas versus small town/rural areas, those who had ever experienced challenges accessing the health care needed versus those who had not, and those patients who reported more flares during the pandemic than in 2019 versus those who reported the same or less number of flares (see Fig. S2a in the electronic Supplementary Material). In total, 51% of patients worried about their ability to control their symptoms once life returned to normal post the pandemic.
More patients relied on certain alternative support systems to manage UC during the pandemic, compared with pre-pandemic (Table 3). Overall, the largest increases in reliance, compared with pre-pandemic conditions, were reported for “having had virtual appointments with their doctor” (13% vs. 55% pre-pandemic and during the pandemic, respectively), “used an online patient portal to contact their doctor’s office or see laboratory results” (31% vs. 47%), and “used social media to connect with other patients or learn about UC” (24% vs. 39%).
In total, 25% of patients reported they had never set goals for managing their UC with their doctor and did not plan to do so (Table 3). The proportions of patients who had ever set goals declined from 48% before the pandemic to 46% during it, and 40% planned to do so after the pandemic. Over half of patients globally had never relied on and did not plan to rely on a patient support group (59%) or advocacy group for information (54%; Table 3). Nearly two-thirds of patients (62%) agreed that they had become better at tracking their symptoms during the pandemic, and this was directionally consistent with the reported use of symptom tracking or disease management applications, which increased from 23% pre-pandemic to 31% during the pandemic (Table 3).
Overall, the survey respondents showed a reluctance to make changes to their treatment plan; 53% of patients agreed with the statement, “I was hesitant to make changes to my UC treatment plan during the COVID-19 pandemic.” Certain patients were more likely to agree with this statement, including those aged 18–49 years versus ≥ 50 years, those who had ever experienced challenges accessing the health care needed versus those who had not, and those who reported more flares during the pandemic than in 2019 versus those who reported the same or less number of flares (see Fig. S2b in the electronic Supplementary Material).
During the COVID-19 pandemic, 36% of respondents taking prescription medications discussed and made changes to their treatment plan (specifically in terms of the prescription medication for their UC) with their doctor, and a similar proportion (35%) discussed but did not make changes to their plan. Changes to treatment plans were more common in patients aged 18–49 years versus ≥ 50 years, those who had ever experienced challenges accessing the health care needed versus those who had, and those who reported more flares during the pandemic than in 2019 versus those who reported the same or less number of flares (see Fig. S2c in the electronic Supplementary Material).
Health Care Access During the COVID-19 Pandemic
Overall, patients’ satisfaction with their ability to access the health care needed during the COVID-19 pandemic was high, with 79% reporting that they were very/somewhat satisfied (Fig. 3a). During the pandemic, 55% of patients attended virtual appointments with their doctor (e.g., via telephone or video chat). The mean (SD) numbers of in-person, virtual-telephone, and virtual-video appointments with a doctor for UC during the pandemic were 3.8 (5.7), 1.6 (3.1), and 2.0 (3.3), respectively. Globally, 26% of patients reported that they had ever experienced difficulties getting an appointment with their UC specialist and, of these, 74% reported that this challenge grew worse during the pandemic (see Fig. S3 in the electronic Supplementary Material). Other challenges associated with access to health care that worsened during the COVID-19 pandemic among those who had ever experienced each challenge included difficulty getting time off work to go to medical appointments (47% said this challenge grew worse), lack of conveniently located medical care (51% said this challenge grew worse), and financial difficulties in paying for care (71% of patients said this challenge grew worse; see Fig. S3 in the electronic Supplementary Material, which demonstrates the challenges encountered). Those patients who had ever experienced challenges accessing the health care needed reported having more virtual appointments since the start of the pandemic, compared with patients who had never had access challenges, either by video (mean number of appointments 2.7 vs. 0.9, respectively) or by telephone (mean number of appointments 2.2 vs. 0.8, respectively).
Proportion of patients reporting satisfaction with a ability to access the health care needed during the COVID-19 pandemica, b aspects of in-person and virtual appointments during the COVID-19 pandemicb, and c the technology platform used to access virtual appointments during the COVID-19 pandemicb. Percentages may not sum to 100% due to weighting and/or computer rounding. COVID-19 coronavirus disease 2019, UC ulcerative colitis. aQuestion: “How satisfied have you been with your ability to access the health care you need during the COVID-19 pandemic?” bQuestion: “Thinking about your last in-person/virtual appointment during the COVID-19 pandemic with the doctor that you see for your UC, how satisfied were you with each of the following?” (By virtual appointments, we mean the process of providing health care from a distance [as opposed to in-person] through technology [e.g., telephone or video chat])
Health Care Experience of Patients During the COVID-19 Pandemic
Patients were equally satisfied with the overall quality of care they received, regardless of whether the appointment was in-person or virtual (81% of patients being very satisfied/satisfied with both in-person or virtual appointments; Fig. 3b). Additionally, both in-person and virtual appointments were associated with high levels of patient satisfaction (> 75% of patients being very satisfied/satisfied in terms of ability to be open with their doctor about their experiences, discussion of disease management goals, discussion of symptoms and flares, and quality of communication; Fig. 3b). Patients reported lower levels of satisfaction with in-person versus virtual appointments in terms of the length of the appointment (73% vs. 80% were very satisfied/satisfied, respectively) and ease of scheduling the appointment (69% vs. 76% were very satisfied/satisfied, respectively; Fig. 3b). Patients reported higher satisfaction with in-person versus virtual appointments for their doctor’s ability to physically assess their symptoms (78% vs. 66% for in-person vs. virtual appointments, respectively). In addition, most patients (83%) were very satisfied/satisfied with the technology platform they used to access their virtual appointments (Fig. 3c).
Patient Preferences for Provision of Health Care During the COVID-19 Pandemic
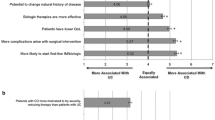
Overall, patients reported that they strongly or slightly preferred in-person versus virtual appointments for most interactions with their doctor, including when meeting a new doctor for the first time (68% vs. 17%, respectively), during a disease flare (55% vs. 25%, respectively), and for regular check-ups with the doctor managing their UC (52% vs. 29%, respectively; Fig. 4). In contrast, 41% of respondents agreed that they strongly or slightly preferred virtual appointments when they needed to refill their prescriptions, compared with 21% who reported that they strongly or slightly preferred in-person appointments. Patient subgroups more likely to state a preference for virtual appointments for every appointment type were patients aged 18–49 years versus ≥ 50 years, those residing in inner city, urban, or suburban areas versus those residing in small town/rural areas, and those who had ever experienced challenges accessing the health care needed versus those who have never had access issues (see Fig. S4 in the electronic Supplementary Material).
Patient preferences for appointment types (in-person vs. virtual) during the COVID-19 pandemic. Percentages may not sum to 100% due to weighting and/or computer rounding. COVID-19 coronavirus disease 2019, UC ulcerative colitis. Question: “Which type of appointment with the doctor you see for your UC would you prefer for each of the following circumstances?”
Discussion
This large-scale global survey was one of the first to specifically evaluate trends around disease management, access to medical care, patient experience, and emotional well-being among patients with UC during the global COVID-19 pandemic. Previous studies have examined the impact of the COVID-19 pandemic on patients with IBD; however, to date, these have generally focused on data from individual countries [13,14,15]. In addition, while the patients with IBD in these previous studies (which included those with Crohn’s disease) share many priorities regarding their medical care, with some symptoms overlapping, the disease characteristics are not the same; therefore, overall management, burden of disease, and even patient expectations can differ. Accordingly, it is important to be able to report data specifically for patients with UC.
In the current survey, which included 584 patients from 5 countries, over half of patients (57%) experienced similar levels of self-reported UC flares during the COVID-19 pandemic, compared with 2019 (i.e., pre-pandemic). During the pandemic, compared to 2019, patients aged 18–49 years had an increased tendency to report worsening of disease activity in terms of the number of flares reported, compared with patients aged ≥ 50 years (33% vs. 11%, respectively). This is consistent with the findings of a previous survey of patients with UC or Crohn’s disease in Japan [16], which attributed reporting differences to the negative impact of lockdown being more pronounced in younger people and the impact of age at IBD onset on rates of disease progression (although this trend was noted only in patients with Crohn’s disease). Similarly, a study assessing the impact of the COVID-19 pandemic on disease symptoms, management, and emotional well-being on patients in the US with IBD found that older patients demonstrated better emotional well-being than younger patients [17]. Previous surveys have reported nonadherence to medication due to a perceived increase in the risk of medications for COVID-19 susceptibility [3], which could impact disease activity. However, in this analysis, most patients (88%) taking prescription medication were satisfied with their current treatment plan, and only a minority of patients (13%) felt the pandemic had a negative impact on how safe they felt taking their medication.
Patients in the present study reported high rates of satisfaction with their ability to access the health care needed during the pandemic. Overall, patient reliance on certain alternative sources of information or support for UC management increased during the pandemic, particularly with respect to online patient portals, virtual appointments, and the use of social media, and this may account, in part, for the high rates of patient satisfaction. The ability of the doctor or health care provider to pivot to telehealth and remote health care strategies during the pandemic was apparently well received by their patients. It will be interesting to observe if any of these changes are retained as we transition into a post-pandemic era of UC management.
Telemedicine was a pivotal component of disease management during periods of lockdown, and patients were reportedly broadly satisfied with the transition [14, 18,19,20]. During the COVID-19 pandemic, surveys carried out among patients with IBD reported that access to remote health care delivery systems can help to reduce disease-related concerns and suggest that telemedicine could remain a viable approach to disease management in the post-pandemic era [21, 22]. The data reported here suggest that many patients plan to keep using alternative methods of support, particularly online patient portals, virtual appointments, and symptom tracking and disease management applications, after the pandemic. Approximately half of the patients (51%) surveyed were worried about their ability to control their symptoms once life returned to normal after the pandemic, which suggests that many patients considered aspects of pandemic life, such as the increased convenience of telehealth and pandemic-mandated lifestyle restrictions, to be beneficial in helping them control their disease. Although patients were generally equally satisfied with the quality of care during in-person and virtual appointments, we observed a broad preference for in-person appointments, the exception being a preference for virtual appointments for the purposes of prescription refills. However, patient data collected during the pandemic suggest that most face-to-face consultations, for either routine or urgent consultations, could be converted to telephone consultations without negatively impacting patient satisfaction [21]. Emerging evidence suggests that transitioning to telemedicine would help to reduce work absenteeism and could potentially improve work productivity among patients with IBD [23]. However, it is important to consider that not all patients will be able to benefit from the telemedicine model. In India, for example, nearly 30% of patients with IBD were unable to contact their health care provider by any means during the pandemic [18].
It is important to note that 6 in 10 patients admitted a hesitancy to consider other treatment options if their treatment made them feel good enough, even if other treatment options might make them feel better than they did at the time. Reasons for settling may relate directly to pandemic-related changes in disease management. However, a similar incidence of settling behavior (60%) was reported in a pre-pandemic sample of patients from 10 countries in 2018 (data on file), which suggests that the pandemic did not contribute significantly to patients’ propensity to explore alternative treatment options if their current treatment made them feel “good enough.”
Lifestyle restrictions during the pandemic, such as fewer outings, working from home, and less busy schedules, helped some patients better control their UC symptoms. Patients aged 18–49 years and those living in inner city, urban, and suburban areas were more likely to feel isolated and alone in managing their UC during the COVID-19 pandemic compared with those aged ≥ 50 years and those residing in small town and rural areas. The availability of virtual consultations during the pandemic may have helped to resolve prior difficulties accessing health care for some patients and may have translated into better symptom control and patient satisfaction. In this analysis, patients who had ever experienced challenges accessing the health care needed were more likely to utilize virtual management options than patients who had never had challenges with health care access.
Conversely, higher rates of anxiety or stress and a reluctance to attend in-person medical appointments during the pandemic may have had a negative effect on UC symptom control. Another survey of patients with IBD conducted during the COVID-19 pandemic reported an increase in illness-associated anxiety that was linked with a higher likelihood of symptom worsening [24]. A previous study by El-Dallal et al. found that women and participants with self-reported anxiety and depression were more likely to have worse symptoms, poorer psychological well-being, and worse daily functioning [17].
Noted limitations of the current analysis include a reliance on accurate recall by patients and an adequate understanding of the survey questions; the survey was conducted in late 2021, with patients asked to recall their experiences pre-pandemic (2019) and during the pandemic (starting early 2020). It is possible that the anxiety caused by the COVID-19 pandemic impacted patients’ opinions on their disease during the pandemic. Survey recruitment was based on patient-reported diagnosis of UC with no clinical disease activity assessment, and patient participation was limited to those with internet access. Therefore, it is possible that patient-reported increases in symptoms during the pandemic may have been due to comorbid conditions that can be impacted upon by stress, such as irritable bowel syndrome, and not necessarily due to worsening of UC. It is important to acknowledge that the findings may not be applicable to all countries owing to regional differences in health care systems, access to UC treatments, barriers to health care, cultural differences, and disparities in health care provision between different communities that may have been magnified during the COVID-19 pandemic. The impact of country-specific variations in COVID-19 public health regulations/directives (e.g., enforced societal lockdowns and reprioritization of access to medical care) on patient satisfaction and perceptions of disease control during the COVID-19 pandemic may have impacted patient responses. In countries that enforced lockdowns, health care providers placed increased emphasis on reassuring patients, increased and unsolicited doctor–patient communication, and the role of patient associations and scientific societies [19, 25]. Moreover, 64% of patients had been living with UC for 5 years or more, compared with 1% who had been diagnosed for less than a year; therefore, these results may not be applicable to patients with shorter-term disease who may have had a different experience/perception of their disease management, health care experience, and preferences for interactions with doctors. Patients whose disease negatively impacts their lives may be more likely to take part in surveys. In this survey, 81% of patients had moderate to severe UC, therefore these data may not be representative of the general UC population. In addition, while the sampling precision of the online poll was accurate to within 6.1%, as measured using a Bayesian credible interval, this interval may be wider among subsets of the surveyed population of interest. Finally, the impact of the patients’ COVID-19 vaccination status, and that of their COVID-19 infection status on survey responses, was unknown, and the COVID-19 infection rates in the individual countries included in this analysis varied during the field period, which may have influenced the results.
Conclusion
During the COVID-19 global pandemic, most patients with UC were satisfied with their current treatment plan and ability to access the health care needed, but many reported a negative impact on their emotional well-being. Patients showed a greater reliance on certain alternative means of support for UC management, and, generally, were equally satisfied with the quality of care received during in-person and virtual appointments. Overall, patients preferred in-person appointments for most appointment types, except for refilling prescriptions. Moving forward, it is important to apply what has been learned from the pandemic concerning patient preferences regarding the provision of health care to the post-pandemic era, in particular from the subgroups of patients who were most negatively impacted by the pandemic in order to introduce meaningful improvements to clinical practice. The adoption of a hybrid model of patient–doctor interactions that incorporates both virtual and in-person appointments could ultimately lead to improvements in how patients manage their disease.
Data Availability
The datasets generated and analyzed during the current study are not publicly available in order to ensure the protection of patient privacy in compliance with the EU General Data Protection Regulation (GDPR) but are available from the corresponding author on reasonable request.
References
Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel JF. Ulcerative colitis. Lancet. 2017;389:1756–70.
Jones JL, Nguyen GC, Benchimol EI, et al. The impact of inflammatory bowel disease in Canada 2018: quality of life. J Can Assoc Gastroenterol. 2019;2:S42–8.
Goodsall TM, Han S, Bryant RV. Understanding attitudes, concerns, and health behaviors of patients with inflammatory bowel disease during the coronavirus disease 2019 pandemic. J Gastroenterol Hepatol. 2021;36:1550–5.
Graff LA, Fowler S, Jones JL, et al. Crohn’s and colitis Canada’s 2021 impact of COVID-19 and inflammatory bowel disease in Canada: mental health and quality of life. J Can Assoc Gastroenterol. 2021;4:S46–53.
Jones JL, Benchimol EI, Bernstein CN, et al. Crohn’s and colitis Canada’s 2021 impact of COVID-19 and inflammatory bowel disease in Canada: health care delivery during the pandemic and the future model of inflammatory bowel disease care. J Can Assoc Gastroenterol. 2021;4:S61–7.
El Ouali S, Rubin DT, Cohen BL, Regueiro MD, Rieder F. Optimal inflammatory bowel disease management during the global coronavirus disease 2019 pandemic. Curr Opin Gastroenterol. 2021;37:313–9.
Schreiber S, Ben-Horin S, Alten R, et al. Perspectives on subcutaneous infliximab for rheumatic diseases and inflammatory bowel disease: before, during, and after the COVID-19 era. Adv Ther. 2022;39:2342–64.
Vigano C, Mulinacci G, Palermo A, et al. Impact of COVID-19 on inflammatory bowel disease practice and perspectives for the future. World J Gastroenterol. 2021;27:5520–35.
Dubinsky MC, Watanabe K, Molander P, et al. Ulcerative Colitis Narrative global survey findings: the impact of living with ulcerative colitis – a patients’ and physicians’ view. Inflamm Bowel Dis. 2021;27:1747–55.
Rubin DT, Hart A, Panaccione R, et al. Ulcerative Colitis Narrative global survey findings: communication gaps and agreements between patients and physicians. Inflamm Bowel Dis. 2021;27:1096–106.
Kish L. Survey sampling. New York: Wiley; 1965.
Gelman A, Carlin JB, Stern HS, Dunson DB, Vehtari A, Rubin DB. Bayesian Data Analysis. 3rd ed. New York: Chapman and Hall/CRC; 2013.
Saibeni S, Scucchi L, Dragoni G, et al. Activities related to inflammatory bowel disease management during and after the coronavirus disease 2019 lockdown in Italy: how to maintain standards of care. United European Gastroenterol J. 2020;8:1228–35.
Martin Arranz E, Suarez Ferrer C, García Ramírez L, et al. Management of COVID-19 pandemic in Spanish inflammatory bowel disease units: results from a national survey. Inflamm Bowel Dis. 2020;26:1149–54.
Allocca M, Fiorino G, Furfaro F, et al. Maintaining the quality standards of care for inflammatory bowel disease patients during the COVID-19 pandemic. Clin Gastroenterol Hepatol. 2020;18:1882–3.
Nishida Y, Hosomi S, Fujimoto K, et al. Impact of the lockdown due to the COVID-19 pandemic on patients with inflammatory bowel disease. Front Med (Lausanne). 2021;8: 649759.
El-Dallal M, Saroufim A, Systrom H, et al. Assessing the repercussions of COVID-19 pandemic on symptoms, disease management, and emotional well-being in patients with inflammatory bowel disease: a multi-site survey study. Scand J Gastroenterol. 2022;57:406–14.
Kale A, Shinde L, Sundaram S, et al. COVID-19 pandemic and inflammatory bowel disease from patients’ perspective: a survey from COVID epicenter in India. JGH Open. 2022;6:126–31.
Kornbluth A, Kissous-Hunt M, George J, Legnani P. Management of inflammatory bowel disease and COVID-19 in New York City 2020: the epicenter of IBD in the first epicenter of the global pandemic. Inflamm Bowel Dis. 2020;26:1779–85.
Tian WN, Huang YH, Dai C. The effect of the COVID-19 pandemic on the medical mode of patients with inflammatory bowel disease in China. Inflamm Bowel Dis. 2020;26:e116–7.
Taxonera C, Alba C, Olivares D, Martin M, Ventero A, Canas M. Innovation in IBD care during the COVID-19 pandemic: results of a cross-sectional survey on patient-reported experience measures. Inflamm Bowel Dis. 2021;27:864–9.
Harris RJ, Downey L, Smith TR, Cummings JRF, Felwick R, Gwiggner M. Life in lockdown: experiences of patients with IBD during COVID-19. BMJ Open Gastroenterol. 2020;7: e000541.
Shah R, Wright E, Tambakis G, et al. Telehealth model of care for outpatient inflammatory bowel disease care in the setting of the COVID-19 pandemic. Intern Med J. 2021;51:1038–42.
Stone ML, Feng M, Forster EM. COVID-19 pandemic increased anxiety among patients with inflammatory bowel disease: a patient survey in a tertiary referral center. Dig Dis Sci. 2021;67:2876–81.
Fiorino G, Allocca M, Furfaro F, et al. Inflammatory bowel disease care in the COVID-19 pandemic era: the Humanitas, Milan, experience. J Crohns Colitis. 2020;14:1330–3.
DeTora LM, Toroser D, Sykes A, et al. Good Publication Practice (GPP) guidelines for company-sponsored biomedical research: 2022 update. Ann Intern Med. 2022;175:1298–304.
Acknowledgements
The authors would like to thank the patients and doctors who were involved in the UC Narrative COVID-19 survey. The authors also acknowledge the contributions of Edward P. Johnson, Elizabeth Priore, and Kathy Steinberg from The Harris Poll.
Medical Writing/Editorial Assistance.
Medical writing support, under the direction of the authors, was provided by Anthony G. McCluskey, PhD, CMC Connect, a division of IPG Health Medical Communications, and Eleanor Finn, PhD, on behalf of CMC Connect, and was funded by Pfizer, New York, NY, USA, in accordance with Good Publication Practice (GPP 2022) guidelines [26].
Funding
The UC Narrative surveys were sponsored by Pfizer, and The Harris Poll was commissioned by Pfizer to conduct the research. Pfizer also funded the journal’s rapid service fee.
Author information
Authors and Affiliations
Contributions
All authors have made a significant contribution to the research described in this manuscript. Laurent Peyrin-Biroulet: data review, analysis, and interpretation; manuscript development and critical review/revision. Karoliina Ylänne: study design; data interpretation; manuscript development and critical review/revision. Allyson Sipes: data review, analysis, and interpretation; manuscript development and critical review/revision. Michelle Segovia: data review, analysis, and interpretation; manuscript development and critical review/revision. Sean Gardiner: study design; data interpretation; manuscript development and critical review/revision. Joseph C. Cappelleri: study design; data interpretation; manuscript development and critical review/revision. Amy Mulvey: study design; statistical analysis; data interpretation; manuscript development and critical review/revision. Remo Panaccione: data review, analysis, and interpretation; manuscript development and critical review/revision. All authors approved the final version of the article, including the authorship list.
Corresponding author
Ethics declarations
Disclosures
Michelle Segovia is an employee of The Medical Affairs Company and a former Postdoctoral Fellow of Rutgers University, which was a paid contractor to Pfizer in connection with the development of this manuscript. Amy Mulvey is an employee of The Harris Poll, which was a paid contractor to Pfizer for related statistical analysis.
Conflict of Interest
Laurent Peyrin-Biroulet has received consulting fees from AbbVie, Abivax, Adacyte, Alimentiv, Alma Bio Therapeutics, Amgen, Applied Molecular Transport, Arena, Biogen, BMS, Celltrion, CONNECT Biopharm, Cytoki Pharma, Enthera, Ferring, Fresenius Kabi, Galapagos, Genentech, Gilead, Gossamer Bio, GSK, HAC-Pharma, IAG Image Analysis, Index Pharmaceuticals, Inotrem, Janssen, Lilly, Medac, Mopac, Morphic, MSD, Nordic Pharma, Norgine, Novartis, OM Pharma, ONO Pharma, OSE Immunotherapeutics, Pandion Therapeutics, Par’Immune, Pfizer Inc, Prometheus, Protagonist, Roche, Roivant, Samsung, Sandoz, Sanofi, Takeda, Theravance, Thermo Fisher, Tigenix, Tillotts, Vectivbio, Ventyx, Viatris, Vifor, and Ysopia. Karoliina Ylänne was an employee of Sidekick Health, Kopavogur, Iceland, at the time of the analysis and is currently an employee and shareholder of Pfizer Inc; has received lecture fees from IBD ja muut suolistosairaudet Ry (patient association), Pfizer Inc, Takeda, and Tillotts Pharma, and consultancy fees from Pfizer Inc, Sandoz, Sidekick Health, and Takeda. Allyson Sipes has received consultancy fees from Pfizer Inc for work unrelated to this analysis. Amy Mulvey is an employee of The Harris Poll, which was a paid contractor to Pfizer for related statistical analysis. Sean Gardiner and Joseph C. Cappelleri are employees and stockholders of Pfizer Inc. Michelle Segovia is an employee of The Medical Affairs Company and a former Postdoctoral Fellow of Rutgers University, which was a paid contractor to Pfizer in connection with the development of this manuscript. Remo Panaccione has received advisory and/or consulting fees from AbbVie, Abbot, Alimentiv (formerly Robarts), Amgen, Arena Pharmaceuticals, AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Celltrion, Cosmos Pharmaceuticals, Eisai, Elan, Eli Lilly, Ferring, Galapagos, Genentech, Gilead, GlaxoSmithKline, Janssen, Merck, Mylan, Oppilan Pandion, Pandion Pharma, Pfizer Inc, Progenity, Protagonist Therapeutics, Roche, Sandoz, Satisfai Health, Schering-Plough, Shire, Sublimity Therapeutics, Takeda Pharmaceuticals, Theravance Biopharma, and UCB.
Ethical Approval
Patient recruitment was performed from online market research panels consisting of members who agreed to participate in this type of research. Patients provided their consent before completing the questionnaire and received remuneration (on behalf of the investigators by the sponsor) for their participation in the survey. The survey was non-interventional and was not conducted as a clinical study; therefore, all patients agreed to participate but ethics approval was not required.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Peyrin-Biroulet, L., Ylänne, K., Sipes, A. et al. The Impact of the COVID-19 Pandemic on Patients with Ulcerative Colitis: Results from a Global Ulcerative Colitis Narrative Patient Survey. Adv Ther 41, 598–617 (2024). https://doi.org/10.1007/s12325-023-02673-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02673-0