Abstract
Introduction
There is limited information regarding multidimensional relationships between asthma control and health-related quality of life (HRQoL), work productivity, and asthma symptom burden in Japan. Furthermore, systematic qualitative investigations about asthma burden have not been performed.
Methods
This cross-sectional, mixed-methods study included Japanese patients (≥ 20 years) with asthma adherent to inhaled corticosteroids/long-acting β2-agonists (ICS/LABA). The primary endpoint was impact of asthma on HRQoL, measured using the Asthma Health Questionnaire-33 (AHQ-33). Secondary endpoints were cough burden (Japanese-adapted Leicester Cough Questionnaire [J-LCQ]) and impact of asthma on work/activities (asthma-specific Work Productivity and Activity Impairment Questionnaire [WPAI:Asthma]). Quantitative data were assessed for the overall population and for well-controlled (WC) and not well-controlled (NWC) asthma subgroups. Qualitative verbal interviews further assessed the impact of NWC asthma on patients’ HRQoL; emergent themes were extracted using thematic analyses.
Results
Of 454 patients, 45.2% (n = 205) had NWC asthma. Patients with NWC asthma had significantly worse asthma- and cough-related HRQoL across all AHQ-33 and J-LCQ domains and significantly greater work and activity impairment versus patients with WC asthma, across all assessed WPAI:Asthma domains. AHQ-33 total score was highly correlated with J-LCQ total and domain scores (r = − 0.8132 to r = − 0.7407). Nine themes emerged from qualitative interviews and confirmed that patients with NWC asthma had considerable HRQoL impairment due to asthma symptoms.
Conclusions
Patients with NWC asthma had higher symptom burden and worse HRQoL than patients with WC asthma, despite ICS/LABA adherence. Cough burden correlated with HRQoL, suggesting cough may be one of the key markers to inform treatment strategy for patients with asthma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
In Japan, approximately 40% of patients with asthma are reported to have symptoms that are not well controlled (NWC), despite adherence to guideline-recommended inhaled corticosteroid/long-acting β2-agonist (ICS/LABA) therapy. |
However, information on the multidimensional relationships between asthma control status and health-related quality of life (HRQoL), work productivity, and symptom burden in Japan is scarce; therefore, it is important to understand the unmet need. |
This mixed-methods study used quantitative and qualitative research components to assess the impact of asthma control on HRQoL and symptom burden in Japanese patients adherent to ICS/LABA. |
What was learned from the study? |
Patients with NWC asthma had worse HRQoL, higher symptom burden, and greater work and activity impairment than patients with well-controlled asthma; cough burden also correlated with asthma-related HRQoL. |
Patients with NWC asthma described how asthma symptoms detrimentally affected their ability to participate in daily and social activities, maintain social relationships, and work, contributing to negative emotional feelings and anxiety about their future; patients also expressed a desire for more effective and better-tolerated treatments. |
These findings indicate considerable unmet need in this patient population despite current ICS/LABA therapy and suggest that cough may be one of the key markers to inform treatment strategies for patients with asthma. |
Introduction
Asthma is a chronic respiratory disease that manifests with variable symptoms, including airflow limitation, shortness of breath, and cough [1], with approximately 262 million people affected worldwide in 2019 [2]. In Japan, approximately 918,000 patients were treated for asthma in 2020 alone [3], and the prevalence of asthma among adult patients is reported to have increased from 3.14% in 1985 to 10.4% in 2017 [4].
Poor asthma control is associated with reduced health-related quality of life (HRQoL), work and activity impairment, greater exacerbation frequency, and increased healthcare resource utilisation (HCRU) and costs [5,6,7,8]. For adult patients with mild to severe asthma, the Japanese Society of Allergology (JSA) and the Japan Asthma Society’s asthma management guidelines primarily recommend combined inhaled corticosteroid/long-acting β2-agonist (ICS/LABA) therapy to control symptoms [9, 10]. However, data from the Japan National Health and Wellness Survey 2018 found that 40.3% of patients with asthma have symptoms that are not well controlled (NWC) despite high adherence to ICS/LABA [11]. A 2019 US study found that 81% of patients with asthma adherent to ICS/LABA continued to experience symptoms and 50% had inadequate asthma control, suggesting that a large burden of disease remains despite following guideline recommendations [6].
Monitoring clinical outcomes and asthma control are essential for asthma management, but evaluating patients’ HRQoL using validated healthcare questionnaires is also important [4, 12]. Increased asthma severity is associated with worse HRQoL when measured using the Asthma Health Questionnaire-33 (AHQ-33) [12], while increased asthma severity and worse asthma control correspond to greater work and activity impairment when measured using the asthma-specific Work Productivity and Activity Impairment Questionnaire (WPAI:Asthma) [13]. A study in adult patients with severe asthma in England using the Leicester Cough Questionnaire (LCQ) found that a substantial proportion of patients had high levels of cough-related morbidity [14]. There was also a moderate correlation between LCQ scores and the Asthma Control Questionnaire and Asthma Quality of Life Questionnaire, suggesting that cough burden may be associated with HRQoL [14]. However, there remains limited information regarding the impact of asthma on the multidimensional HRQoL of patients in Japan.
The aim of this study was to describe and quantify the unmet needs in Japanese patients with asthma who are adherent to ICS/LABA, and whose asthma is either well controlled (WC) or NWC, to better understand the relationship between asthma control status and patients’ HRQoL. We utilised a mixed-methods approach to investigate the impact of asthma on patients’ daily lives and their potential treatment expectations, incorporating multidimensional quantitative and qualitative research components to enhance the range of data collected and to obtain data not readily available from routine clinic visits.
Methods
Study Design and Data Source
This cross-sectional, mixed-methods study sequentially collected self-reported data from quantitative patient surveys and qualitative verbal interviews, conducted independently on an online platform, to explore symptom burden and HRQoL among patients with asthma who were adherent to ICS/LABA, and to assess their treatment expectations (Figure S1). Patient surveys were conducted in May 2022 and all data were anonymised. The patient survey date was defined as the date on which the patient completed the survey.
Patients were recruited by email from the Rakuten Insight Asthma Panel (Survey Operator), an online market research database that includes patients in Japan who annually self-report asthma [15]. Rakuten Insight implements various measures to improve data quality, including pre-screening of participants, checks for contradictory answers, and 'speeder' checks, where survey responders with quick response times are removed [16]. Patients were asked to complete screening questions to assess their study eligibility and ICS/LABA treatment status; the Asthma Control Test (ACT) questionnaire was used to define asthma control status (WC asthma: ACT score ≥ 20; NWC asthma: ACT score < 20) and the Morisky Medication Adherence Scale (MMAS) questionnaire was used to assess medication adherence [17,18,19,20]. After completing the screening questions, patients were invited to complete the quantitative research survey, which collected patients’ demographic and clinical characteristics data and utilised validated health questionnaires to collect HRQoL (AHQ-33 and Japanese-adapted LCQ [J-LCQ]) and work productivity and activity impairment (WPAI:Asthma) data.
Anonymised survey data were provided by the Survey Operator to the study Investigators, who selected patients with NWC asthma and the greatest HRQoL impairment (based on AHQ-33 total scores) for qualitative interviews from among those who expressed an interest in participating. Selected patients were provided with video conferencing links via email by the Survey Operator. Qualitative interviews were conducted online between July 2022 and August 2022 by an independently contracted Interviewer. Interviews were transcribed and anonymised by the Interviewer, then returned to the survey operator and subsequently to the investigators.
Study Endpoints
The primary endpoint of the quantitative research component was the impact of asthma on patients’ HRQoL, measured by AHQ-33 scores, in the overall population and in WC and NWC asthma subgroups. The AHQ-33 is a widely used health questionnaire developed by the JSA to measure patients’ asthma-related HRQoL; it comprises 33 items (graded 0–4) divided between 6 domains (Asthmatic Symptoms, Factors which Worsened Symptoms, Emotion, Daily Activity, Social Activity, and Economics) and one face scale, where higher scores represent worse HRQoL [21, 22].
The secondary endpoints were the burden of chronic cough symptoms on HRQoL and the impact of asthma on work and activity impairment, measured via the distribution of J-LCQ scores, WPAI:Asthma scores, and patient characteristics, in the overall population and in WC and NWC asthma subgroups. The J-LCQ assesses chronic cough-related HRQoL and is composed of 19 items split across 3 domains: Physical, Psychological, and Social (total score from items in each domain graded 1–7), where lower scores indicate worse chronic cough-related HRQoL [23, 24]. The WPAI:Asthma assesses the impact of asthma on work productivity and activity impairment over the previous 7 days. It consists of 9 items across 3 domains representing work impairment, school impairment, and activity impairment; domain scores are described as percentages of impairment from 0–100%, with higher scores representing greater impairment [13, 25]. Other endpoints were the correlation between AHQ-33 and J-LCQ scores and the correlation between AHQ-33 and WPAI:Asthma scores.
The qualitative research component aimed to further investigate the impact of asthma on the daily lives of patients with NWC asthma despite good adherence to ICS/LABA and to evaluate patients’ potential treatment expectations. Qualitative verbal interviews were reviewed and analysed to explore patients’ perceptions of asthma-related impacts on mental, physical and social activities, daily sleep, work/school, and other aspects of their lives and to investigate patients’ treatment expectations for their current asthma medication.
Study Population
To be eligible for the study, patients were required to be adults (≥ 20 years of age) with self-reported asthma, who had received ICS/LABA combination therapy for ≥ 4 weeks at the survey date. Patients were also required to have good adherence to medication (MMAS score ≥ 6) and demonstrate the ability to answer survey questions by completing an online screening survey. Patients were excluded if they had a diagnosis of chronic obstructive pulmonary disease (COPD), had a smoking history of ≥ 10 years, or were using biologic or long-acting muscarinic antagonist (LAMA) medications. To be included in the qualitative research component, participants had to have completed the quantitative surveys and indicated an intention to participate.
Data Analyses
For the quantitative research component, a target of 200 patients with WC asthma and 200 patients with NWC asthma was set for data collection, based on discussions with the Survey Operator about potentially achievable sample sizes. The 95% confidence intervals (CIs) for the population proportion where the sample size is N = 200 (WC or NWC asthma subgroups) were calculated as shown in Table S1.
Descriptive statistics were used to report patient characteristics data and data collected from the quantitative research component: mean, standard deviation (SD), standard error of the mean (SE), median, interquartile ranges (IQR), and 95% confidence intervals (CIs) were calculated for continuous variables and categorical variables were reported as frequencies and proportions. Wilcoxon rank-sum tests and Fisher exact tests were used to assess differences between WC and NWC asthma subgroups for statistical significance. The effect size was measured using Pearson correlation coefficient. An analysis of covariance was performed to further compare AHQ-33, J-LCQ, and WPAI:Asthma scores between WC and NWC asthma subgroups, adjusted for presence or absence of work with renumeration (AHQ-33 and J-LCQ only), WC and NWC asthma, age, presence of pets, and MMAS score. The correlations between AHQ-33 and J-LCQ or WPAI:Asthma were analysed using Spearman’s rank correlation coefficient. The strength of correlation (positive [negative]) was defined as weak (r = ≥ 0.3 to < 0.5 [r = ≥ − 0.5 to < − 0.3]), moderate (r = ≥ 0.5 to < 0.7 [r = ≥ − 0.7 to < − 0.5]), and high (r = ≥ 0.7 to 1.0 [r = ≥ − 1.0 to − 0.7]) [26].
For the qualitative component, transcribed responses were reviewed and thematic analyses were performed to further investigate patients’ perspectives of the burden of asthma and its impact on their daily lives and patients’ treatment expectations [27]. Lastly, a conceptual saturation analysis was performed to ensure all relevant themes were captured [28,29,30,31].
Compliance with Ethics Guidelines
This study was carried out in accordance with the Declaration of Helsinki, Ethical Guidelines for Medical and Biological Research Involving Human Subjects, and Japanese laws and regulations. Prior to study initiation, documented approval was obtained from the Takahashi Clinic Ethics Committee (LNW00148). To enrol in the study, participants first provided electronic informed consent. Individuals had the option to discontinue their participation at any point, whereupon they were considered as not consenting and were discounted as survey responders. Data collected were anonymised and all data were processed in compliance with the Act on the Protection of Personal Information and related notices applicable to the protection of personal information.
Results
Study Population
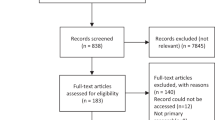
The patient survey was initially distributed to 86,724 patients; 25,405 patients agreed to participate in the survey, of whom 24,058 were excluded and 1347 were identified as potential patients with ICS/LABA use and good medication adherence (Fig. 1). Following screening for completed surveys, 892 patients were excluded. One patient was also excluded from the overall analysis due to deviation from the eligibility criteria. The final study population included 454 patients with asthma; the WC asthma subgroup achieved the target number of patients first (n = 249 [54.8%]) and data collection was terminated, after which, only data for the NWC asthma subgroup were collected until the target number of patients was reached (n = 205 [45.2%]) (Fig. 1).
Patient disposition. aPatients were excluded from the study if they did not complete the survey or if they did not complete the survey honestly (including if they completed the survey in a very short time); bone patient was excluded from the overall analysis population due to deviation from the eligibility criteria; cdata collection for the WC asthma subgroup was completed first, after which, only data for the NWC asthma subgroup continued to be collected. ACT, asthma control test; ICS, inhaled corticosteroid; LABA, long-acting β2-agonist; NWC, not well controlled; WC, well controlled
Most patients in the study population reported a moderate MMAS adherence status (n = 347, 76.4%) (Table 1). The mean (SD) age of the overall population was 48.8 (13.2) years, most patients were female (n = 272, 59.9%), and the majority of patients reported having asthma for ≥ 10 years (n = 276, 60.8%) (Table 1). Patient characteristics were generally comparable between WC and NWC asthma subgroups; however, the mean age of the WC asthma group was significantly higher than the NWC asthma group (p = 0.0326) (Table 1).
Quantitative Research: Patient Questionnaires
AHQ-33
In the overall population, patients had a mean (SD) total AHQ-33 score of 24.1 (23.3) (Fig. 2a, Table S2). Patients with NWC asthma reported significantly higher AHQ-33 mean total scores and mean scores across all AHQ-33 domains compared with the WC asthma group (p < 0.0001) (Fig. 2a, Table S2). Patients in the NWC asthma subgroup had higher symptom burden than patients with WC asthma, with significantly higher domain scores for Asthma symptoms (11.1 [6.3] vs. 3.3 [3.6], p < 0.0001) and Factors that worsened asthma symptoms (9.9 [6.5] vs. 3.1 [4.0], p < 0.0001). In addition, responses to the Asthma symptom domain showed that 49.3–63.9% of patients with NWC asthma experienced symptoms including sputum, wheezing, breathlessness, and cough compared with 8.4–22.1% of patients with WC asthma (Table S3). After completing the covariate-adjusted analysis, significantly higher mean AHQ-33 scores were still observed in the NWC asthma subgroup versus the WC asthma subgroup across all domains (p < 0.0001) (Table S4).
AHQ-33, J-LCQ, and WPAI:Asthma scores, overall and by NWC and WC asthma subgroups. Wilcoxon rank-sum tests were used to compare asthma control subgroups. AHQ-33, 33-item Asthma Health Questionnaire; J-LCQ, Japan Leicester Cough Questionnaire; NWC, not well controlled; SD, standard deviation; WC, well controlled; WPAI, Work Productivity and Activity Impairment
J-LCQ
Overall, the mean (SD) total J-LCQ score was 17.4 (3.4), while mean (SD) scores for Physical, Psychological, and Social domains were 5.6 (1.1), 5.8 (1.2), and 6.0 (1.2), respectively (Fig. 2b, Table S5). Patients with NWC asthma had significantly worse cough-related HRQoL than patients with WC asthma, with a lower mean (SD) total score (15.2 [3.4] vs. 19.1 [2.0], p < 0.0001) and lower Physical (4.9 [1.1] vs. 6.2 [0.7], p < 0.0001), Psychological (5.1 [1.2] vs. 6.4 [0.8], p < 0.0001), and Social (5.3 [1.3] vs. 6.6 [0.7], p < 0.0001) domain scores versus patients with WC asthma (Fig. 2b, Table S5). The covariate-adjusted analysis further confirmed that mean J-LCQ scores were significantly lower in the NWC asthma subgroup versus the WC asthma subgroup across all domains (p < 0.0001) (Table S4).
WPAI:Asthma
The mean (SD) percentages of Absenteeism, Impairment while working, Overall work impairment, and Activity impairment for the overall population were 0.03 (0.13), 0.17 (0.24), 0.18 (0.26), and 0.19 (0.26), respectively (Fig. 2c, Table S5). Significantly greater work and activity impairment was reported by the NWC asthma subgroup compared with the WC asthma subgroup. Patients with NWC asthma had significantly higher mean (SD) percentage of Absenteeism (0.04 [0.15] vs. 0.02 [0.12], p < 0.0001), Impairment while working (0.29 [0.27] vs. 0.06 [0.14], p < 0.0001), Overall work impairment (0.30 [0.29] vs. 0.07 [0.17], p < 0.0001), and Activity impairment (0.33 [0.28] vs. 0.08 [0.17], p < 0.0001) scores compared with patients with WC asthma (Fig. 2c, Table S5). The covariate-adjusted analysis confirmed that WPAI:Asthma scores were significantly higher in the NWC asthma subgroup versus the WC asthma subgroup for Impairment while working, Overall work impairment, and Activity impairment domains (p < 0.0001) and were numerically higher for Absenteeism (p = 0.1926) (Table S4). Data for class impairment domains were not included in the analysis because these questions were relevant for only a few patients (n = 12).
Correlation Between AHQ-33 and J-LCQ
Analyses of the correlation between AHQ-33 and J-LCQ for the overall population revealed that the AHQ-33 total score was highly correlated with J-LCQ total score (r = − 0.8020) and J-LCQ Physical (r = − 0.8132), J-LCQ Psychological (r = − 0.7483), and J-LCQ Social (r = − 0.7407) domain scores (Fig. 3). Further analyses of AHQ-33 domains showed that AHQ-33 Asthmatic symptoms, Factors which worsened symptoms, Emotion, and Social activity scores had a higher correlation with J-LCQ scores (total score and domains) than AHQ-33 Daily activity, Economics, and Face scale scores in the overall population (Table S6). When stratified by asthma control, AHQ-33 scores were generally more highly correlated with J-LCQ scores in the NWC asthma subgroup versus the WC asthma subgroup across all domains, with the exception of AHQ-33 Asthmatic symptoms (Table S6).
Correlationa between AHQ-33 total score and J-LCQ total and domain scores in the overall population. aCorrelation was measured using Spearman's rank correlation coefficient. AHQ-33, 33-item Asthma Health Questionnaire; J-LCQ, Japan Leicester Cough Questionnaire; r, Spearman's rank correlation coefficient
Correlation Between AHQ-33 and WPAI:Asthma
For the overall population, AHQ-33 total score was moderately correlated with WPAI:Asthma Percent impairment while working (r = 0.6982), Percent overall work impairment (r = 0.6928), and Percent activity impairment (r = 0.7155) but was weakly correlated with Percent work time missed (r = 0.3091) (Fig. 4). When stratified by asthma control subgroups, AHQ-33 scores were more highly correlated with WPAI:Asthma scores in patients with NWC asthma versus patients with WC asthma across all AHQ-33 and WPAI:Asthma domains (Table S7).
Correlationa between AHQ-33 total score and WPAI:Asthma total and domain scores in the overall population. aCorrelation was measured using Spearman's rank correlation coefficient. AHQ-33, 33-item Asthma Health Questionnaire; r, Spearman's rank correlation coefficient; WPAI, Work Productivity and Activity Impairment
Qualitative Research
A total of 98 patients with NWC asthma indicated an intention to participate in qualitative verbal interviews, of whom 38 confirmed that they were able to use online video conferencing software. From these 38 potential participants, the final 20 patients selected were those with the highest AHQ-33 total scores. Patient characteristics and AHQ-33, J-LCQ, and WPAI:Asthma scores for patients in the qualitative component are described in Tables S8 and S9.
Nine themes were extracted from the thematic analysis of patient interviews: (1) patients’ expectations for asthma treatments; (2) emotional burden in relation to asthma symptoms; (3) impacts of asthma on patients’ social and daily activities; (4) patients’ perceptions about communication with physicians; (5) patients’ remorse when symptoms manifest around people; (6) difficulties related to peer understanding; (7) impacts of asthma on work; (8) misunderstandings and psychological burdens during the COVID-19 pandemic; (9) sleep deprivation caused by asthma symptoms (Table S10). Descriptive summaries of emergent themes based on patients’ responses are presented below; patients’ quotes categorised according to themes are detailed in Table S11.
Theme 1: Patients’ Expectations for Asthma Treatments
All patients discussed their expectations for asthma medications. Over half of patients highlighted the need for effective and safe medication, including treatments that acted quickly and controlled asthma symptoms such as cough; patients also discussed their concerns about the side effects associated with medication use, especially long term.
Patients expected treatments to be easy to use and expressed a desire for medication requiring less frequent administration, more compact devices, and devices that were easier to operate. Costs of medication were described as high by three patients and as an economic burden by four patients. Three patients also expressed a need for preventative medications that could be taken before the onset of symptoms.
Theme 2: Emotional Burden in Relation to Asthma Symptoms
All patients experienced emotional burden caused by asthma. Two key sub-themes were identified: current emotional burden and emotional anxiety about the future. Many patients reported that asthma symptoms, including breathlessness and cough, caused negative feelings such as irritation and distress. Over half of patients discussed concerns about worsening asthma in the future, including that asthma symptoms would become uncontrolled with current medication and that asthma may lead to complications or comorbidities, while one patient reported anxiety that medication costs may become prohibitive after retirement.
Theme 3: Impacts of Asthma on Patients’ Social and Daily Activities
Almost all patients discussed asthma-related burdens on their social and daily activities.
Most patients said that asthma impacted their social activities, such as limiting their enjoyment of hobbies or preventing socialising with friends and family because of concerns about worsening symptoms or causing inconvenience from coughing, leading to feelings of dissatisfaction and frustration. Patients also described asthma affecting their daily activities and preferred lifestyle, for example, restricting their ability to drive, have pets, cook, and exercise.
Theme 4: Patients’ Perceptions About Communication with Physicians
Almost all patients described difficulties communicating with their physician about additional burdens related to their asthma and improving their prescriptions. Patients discussed withholding details of these burdens to their physician, with reasons including that they did not expect their physician to understand their psychological and daily burdens or desire for better medication, they did not think that their physician was responsible for treating these burdens, consultation times were too short, or because of previous negative experiences with physicians.
Theme 5: Patients’ Remorse When Symptoms Manifest Around People
Most patients reported feeling guilt about their asthma following symptom onset in front of family, friends, and co-workers or when they perceived that friends and family could not smoke, have pets, sleep, or spend time with them because of their symptoms. Patients also discussed not wanting to worry about their asthma in front of people and that they did not want attention from others because of their asthma.
Theme 6: Difficulties Related to Peer Understanding
Most patients perceived that their peers did not understand their disease, and several patients described how they did not tell others about their asthma or hid their asthma because it was unnecessary or too bothersome to explain, or because they had an inferiority complex about their asthma.
Theme 7: Impacts of Asthma on Work
The majority of patients reported that asthma impacted on their work. Patients felt that they lost job opportunities by highlighting their asthma in applications, and one patient was concerned about losing their job if they reported their asthma to their employer. Patients discussed needing time off work due to symptoms and described concerns about future absenteeism because of their asthma. Patients also described issues with work performance, including needing to stop tasks due to symptoms, an inability to focus due to sleep deprivation, and issues with work relationships, where co-workers lacked empathy or harassed patients because of their asthma.
Theme 8: Misunderstandings and Psychological Burdens During the COVID-19 Pandemic
Many patients reported that the onset of asthma-related cough symptoms in public led to misperceptions that they were infected with COVID-19, with patients having to explain that they had asthma, leading to negative feelings of irritation and sadness. Patients were also concerned about the worsening of their asthma due to COVID-19 and vice versa.
Theme 9: Sleep Deprivation Caused by Asthma Symptoms
Sleep deprivation caused by asthma symptoms including breathlessness, cough, and exacerbation was reported by many patients. Sleep deprivation led to both physical and psychological burdens, such as reduced concentration, daytime sleepiness, fatigue, irritation, and distress; these burdens resulted in problems at work and in patients’ daily lives, including impacting on presenteeism, work productivity, and childcare.
Conceptual Saturation Analysis
Patients were categorised into four groups based on when they participated in qualitative interviews; Groups 1 and 2 completed their interviews first, followed by Groups 3 and 4.
All themes emerged in Groups 1 and 2, while no new themes emerged in Groups 3 and 4, indicating that conceptual saturation was achieved (Table S12).
Discussion
Japanese asthma management guidelines primarily recommend combined ICS/LABA therapy for patients with mild to severe asthma [4, 9, 10]; however, many patients remain NWC despite high adherence to ICS/LABA [11]. The results of this quantitative analysis of 454 patients with asthma in Japan with good adherence to ICS/LABA showed that patients with NWC asthma had significantly greater HRQoL impairment, work productivity and activity impairment, and cough burden compared with patients with WC asthma. Results from a qualitative analysis supported these findings, with most patients stating that their asthma symptoms led to physical and emotional burdens that impacted their daily lives.
The results of the AHQ-33 and WPAI:Asthma questionnaires revealed that patients with NWC asthma (defined as an ACT score < 20) had significantly worse HRQoL across all domains compared with patients with WC asthma, including increased symptom burden, worse emotional state, work and activity impairment, and greater financial burden. This is consistent with findings from a systematic literature review of the impact of asthma on patients in Australia, Europe, Japan, the US, and the UK [32]. This review showed that patients with uncontrolled moderate/severe asthma have impaired HRQoL and clinical outcomes, including lung function and exacerbation burden [32]. Other studies have also found that low ACT scores are associated with higher HCRU and costs, increased work, activity and HRQoL impairment, as well as a greater chance of treatment step-up and exacerbations than high ACT scores [7, 33]. In the present study, patients were asked as part of the AHQ-33 Asthmatic symptoms domain if they “have asthma attacks”. The mean score for this domain was significantly higher in the NWC asthma subgroup versus the WC asthma subgroup, suggesting that an increased risk of asthma attacks and worse symptom burden was associated with poor asthma control. This may indicate an insufficient benefit from ICS/LABA treatment for these patients and that periodic monitoring of asthma control could help clinicians identify and mitigate against future exacerbation risk by optimising early treatment. However, ACT scores and symptoms were not followed over time in this study, and no statistical methodology was applied to test the difference; therefore, further research is needed to explore this relationship and its link to HRQoL.
Uncontrolled moderate/severe asthma is also associated with considerable healthcare costs, including direct costs due to increased HCRU and medication use and indirect costs from reduced work productivity and activity impairment [8, 32, 34, 35]. These findings are reflected in the qualitative analysis presented in this study. Patients with NWC asthma described how asthma symptoms detrimentally affected their ability to participate in daily and social activities, maintain social relationships, and work, contributing to negative emotional feelings and anxiety about their future. Collectively, these findings highlight both the personal and economic impact of NWC asthma on patients’ lives [8, 32, 34, 35].
This study showed that cough symptoms had a considerable impact on patients’ HRQoL. Patients with NWC asthma reported significantly higher total, physical, psychological, and social cough-related burden compared with patients with WC asthma, as measured by the J-LCQ. Similarly, a recent interview-based study among patients with refractory cough in Japan showed that patients reported high levels of physical, psychological, and social burden due to cough, measured via the LCQ, while qualitative assessments revealed that patients were particularly affected by emotional and psychological burdens [36]. A separate study also showed that patients with chronic cough in Japan had increased WPAI and HCRU compared with matched non-cough patients [37]. In the present study, patients described not being able to enjoy social activities because of anxiety about cough symptoms manifesting in public places. Furthermore, many patients experienced misunderstandings from members of the public because of their asthma-related cough symptoms during the COVID-19 pandemic, leading to negative feelings of irritation and sadness. These results highlight how cough can affect all aspects of patient life, ranging from social burden to physical and emotional impairment. Public health initiatives that aim to increase societal awareness of asthma in Japan may help to alleviate this burden by reducing the stigma attached to asthma and cough.
In the present study, J-LCQ scores were negatively correlated with AHQ-33 scores, indicating that when J-LCQ scores decrease (greater cough-specific HRQoL impairment), AHQ-33 scores increase (greater asthma-related HRQoL impairment). This suggests that when patients with asthma have cough, asthma-related HRQoL is also impaired. These findings suggest that more efficient and personalised treatments could be utilised to guide treatment decisions, such as the treatable traits approach [38, 39]. This approach is changing the strategy for the treatment of severe asthma, with recent studies showing that high baseline blood eosinophil counts are a predictor of treatment response to biologics [40, 41], while increasing the dose of ICS improves lung function and reduces exacerbations in patients with high baseline levels of type 2 inflammation biomarkers [42]. Identifying traits and implementing specific treatment interventions early in the treatment pathway may lead to an improved treatment response and enhanced asthma control. For patients with substantial cough burden, this may involve considering interventions aimed specifically at improving patients' cough-related HRQoL.
The Japan Asthma Society’s Practical Guidelines for Asthma Management recommend ICS/LAMA/LABA triple therapy if cough symptoms, sputum, or dyspnoea remain after ICS/LABA treatment and as initial maintenance therapy if cough, sputum, or dyspnoea are strong [9], while Japanese Respiratory Society (JRS) guidelines also recommend add-on LAMA for moderate-severe cough-variant asthma [43]. While data supporting the use of LAMA to treat cough are limited, a 2018 study showed that the use of add-on LAMA (tiotropium) significantly improved cough-related HRQoL and asthma control, as measured by cough visual analogue scale, J-LCQ, and ACT, in patients with asthmatic cough resistant to ICS/LABA [44]. As such, cough presents a treatable trait that may benefit from the use of add-on LAMA. However, the cause of cough is variable, and identifying the treatable traits underlying a patient’s cough is important. It has been suggested that ICS-refractory cough can have a different pathophysiology depending on daytime or nighttime occurrence, with a lower capsaicin cough threshold found to be associated with residual daytime cough and methacholine hyperreactivity and lower immunoglobulin E levels reported to be predictors of residual nighttime cough [45]. These findings further emphasise the need for a personalised approach to patients’ treatment.
A strength of this study is that it prospectively collected data among patients with asthma in Japan using multiple validated health questionnaires, which are typically challenging to obtain in the real-world setting, and comprehensively captured different dimensions of patient outcomes, thus providing valuable insight into patients’ disease burden and unmet needs. Furthermore, given there are limited qualitative data available to describe the unmet need of patients with asthma in Japan, the inclusion of a qualitative component in this mixed-methods study enriched the findings from the quantitative component and helped to contextualise the considerable disease burden experienced by patients. For example, in the J-LCQ, patients with NWC asthma reported greater sleep impairment from cough symptoms than patients with WC asthma. Patients with NWC asthma also reported significantly higher work and activity impairment than patients with WC asthma. In the qualitative analysis, most patients said that they experienced sleep deprivation because of asthma symptoms such as breathlessness and cough, leading to physical and emotional burdens; these burdens in turn negatively impacted on work and daily activities, further highlighting the relationship between asthma symptoms such as cough and patients’ HRQoL.
Notably, most patients participating in qualitative interviews highlighted perceived challenges in communicating with their physician about different prescriptions or seeking additional treatments for psychological and daily burdens stemming from their asthma. By improving the patient-physician experience and using a collaborative approach to treatment and shared decision making, patients may be able to access treatments better suited to their individual needs and to better understand and manage their disease [46, 47]. In addition, most patients in the qualitative analysis expressed an expectation for more effective medicines despite being adherent to current ICS/LABA therapy. While adherence to medication is essential for effective asthma management [1, 48, 49], physicians’ perceptions of the importance of treatment adherence may potentially delay the switch to more appropriate treatments; in patients with COPD, delayed initiation of treatment is associated with increased rates of exacerbations, greater HCRU and costs compared with prompt treatment initiation [50,51,52]. This further supports the value of shared decision making in seeking individualised treatments.
There are several limitations to this study, which include its generalisability to the broader asthma population. Survey participants had to have an internet connection, which may have excluded specific patient demographics with lower computer literacy or reduced access to the internet, such as the elderly or those with a low level of education or reduced income [53], thereby limiting the generalisability of the asthma control-related outcomes reported here. In addition, patients with greater concern about their asthma control may have been more inclined to participate in the study than those with less concern, which in turn may have influenced the high level of HRQoL impairment reported in the NWC asthma subgroup. All patients who participated in the qualitative component had NWC asthma and were selected based on the highest AHQ-33 total scores from those who expressed an intention to participate. Consequently, qualitative data showing the impact of asthma on patients’ daily lives and treatment expectations reflect those patients with the greatest burden of disease and cannot be directly compared with patients with WC asthma. We chose to limit the number of questions in the patient survey to focus on HRQoL, rather than on factors affecting patients achieving asthma control, and to reduce the burden of completing the survey in favour of increasing the response rate [54]. However, a limitation to this approach was the resulting absence of specific demographic data, such as insurance status, education status, and body mass index, which have been associated with asthma severity and level of asthma control [55,56,57]. Furthermore, as patient data were self-reported, this may allow for false reports to be recorded, potentially affecting the validity of results. Patients in the survey also self-determined if they met the study’s selection criteria during the screening test. Therefore, the study population may include patients who do not actually meet selection criteria or who may have misreported their disease status, asthma control status, or adherence status. Lastly, there are limitations associated with the exclusion criteria in this study. Patients were excluded if receiving biologic or LAMA medications alongside ICS/LABA; however, the use of other concomitant medications was not accounted for and may have influenced the results. In addition, we did not consider lung tissue resection due to lung diseases as an exclusion criterion to keep the study population as generalised to a real-world population as possible. As a result, patients' HRQoL results may have been impacted by the presence of comorbid lung diseases or previous lung tissue resection, although the number of patients affected by this is expected to be small.
Conclusion
In summary, patients with NWC asthma in Japan had greater symptom burden and impaired HRQoL and work productivity compared with patients with WC asthma, despite good adherence to ICS/LABA. Cough symptoms presented a considerable burden and were also correlated with asthma-related HRQoL impairment, suggesting that cough may be one of the key markers to inform personalised treatment strategies for patients with asthma.
Data Availability
The datasets generated during and/or analysed during the current study are available on request by submitting an enquiry to: https://www.gsk-studyregister.com/en/.
Change history
01 December 2023
A Correction to this paper has been published: https://doi.org/10.1007/s12325-023-02723-7
References
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention 2023. https://ginasthma.org/2023-gina-main-report/. Accessed 30 June 2023.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020; 396:1204–22.
Ministry of Health, Labour and Welfare. Overview of patient survey in 2020. https://www.mhlw.go.jp/toukei/saikin/hw/kanja/20/dl/suikeikanjya.pdf. Accessed 5 Jan 2023.
Nakamura Y, Tamaoki J, Nagase H, et al. Japanese guidelines for adult asthma 2020. Allergol Int. 2020;69:519–48.
Adachi M, Hozawa S, Nishikawa M, Yoshida A, Jinnai T, Tamura G. Asthma control and quality of life in a real-life setting: a cross-sectional study of adult asthma patients in Japan (ACQUIRE-2). J Asthma. 2019;56:1016–25.
Davis J, Trudo F, Siddall J, Small M. Burden of asthma among patients adherent to ICS/LABA: a real-world study. J Asthma. 2019;56:332–40.
Lee LK, Ramakrishnan K, Safioti G, Ariely R, Schatz M. Asthma control is associated with economic outcomes, work productivity and health-related quality of life in patients with asthma. BMJ Open Respir Res. 2020;7.
Nagase H, Adachi M, Matsunaga K, et al. Prevalence, disease burden, and treatment reality of patients with severe, uncontrolled asthma in Japan. Allergol Int. 2020;69:53–60.
Japan Asthma Society. Practical guidelines for asthma management 2022. https://jasweb.or.jp/guideline.html. Accessed 26 Jan 2023.
Japanese Society of Allergology. Asthma prevention and management guidelines 2021. https://www.jsaweb.jp/modules/journal/index.php?content_id=4. Accessed 26 Jan 2023.
Gon Y, Ohyanagi N, Kobayashi A. The association between control level and self-reported treatment adherence across different treatment types in Japanese asthma patients. Respir Investig. 2021;59:454–63.
Muraki M, Ichihashi H, Haraguchi R, Iwanaga T, Kubo H, Tohda Y. Comparison of the Asthma Health Questionnaire-33-Japan and the short-form 36-item health survey for measuring quality of life in Japanese patients with asthma. Allergol Int. 2008;57:339–46.
Chen H, Blanc PD, Hayden ML, et al. Assessing productivity loss and activity impairment in severe or difficult-to-treat asthma. Value Health. 2008;11:231–9.
Natarajan S, Free RC, Bradding P, McGarvey L, Siddiqui S. The relationship between the Leicester cough questionnaire, eosinophilic airway inflammation and asthma patient related outcomes in severe adult asthma. Respir Res. 2017;18:44.
Rakuten Insight. Rakuten Insight Asthma Panel. https://insight.rakuten.com/. Accessed 2 Nov 2022.
Rakuten Insight. Rakuten insight panel quality control procedures. https://insight.rakuten.com/wordpress/wp-content/uploads/RI-PanelQualityControlProcedures.pdf. Accessed 18 July 2023.
Berlowitz DR, Foy CG, Kazis LE, et al. Effect of intensive blood-pressure treatment on patient-reported outcomes. N Engl J Med. 2017;377:733–44.
Bress AP, Bellows BK, King JB, et al. Cost-effectiveness of intensive versus standard blood-pressure control. N Engl J Med. 2017;377:745–55.
Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich). 2008;10:348–54.
Nathan RA, Sorkness CA, Kosinski M, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004;113:59–65.
Arioka H. Bronchial asthma and QOL. Nippon Naika Gakkai Zasshi. 2006;95:1507–13.
Arioka H, Kobayashi K, Kudo K, Kabe J. Validation Study of a Disease-specific Module, the Asthma Health Questionnaire (AHQ) Using Japanese Adult Asthmatic Patients. Allergol Int. 2005;54:473–82.
Birring SS, Prudon B, Carr AJ, Singh SJ, Morgan MD, Pavord ID. Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ). Thorax. 2003;58:339–43.
Kanemitsu Y, Niimi A, Matsumoto H, et al. Gastroesophageal dysmotility is associated with the impairment of cough-specific quality of life in patients with cough variant asthma. Allergol Int. 2016;65:320–6.
Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4:353–65.
Mukaka MM. Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24:69–71.
Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15:398–405.
Guest G, Namey E, Chen M. A simple method to assess and report thematic saturation in qualitative research. PLoS ONE. 2020;15: e0232076.
Hennink M, Kaiser BN. Sample sizes for saturation in qualitative research: a systematic review of empirical tests. Soc Sci Med. 2022;292: 114523.
Lamoureux RE, Shields A, Stokes J, Yaworsky A, Galipeau N. How many subjects are enough for symptom-focused concept elicitation studies? A retrospective analysis of saturation across twenty-six studies. Value Health. 2015;18:PRM132.
Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52:1893–907.
Czira A, Turner M, Martin A, et al. A systematic literature review of burden of illness in adults with uncontrolled moderate/severe asthma. Respir Med. 2022;191: 106670.
Ko FW, Hui DS, Leung TF, et al. Evaluation of the asthma control test: a reliable determinant of disease stability and a predictor of future exacerbations. Respirology. 2012;17:370–8.
Inoue H, Kozawa M, Milligan KL, Funakubo M, Igarashi A, Loefroth E. A retrospective cohort study evaluating healthcare resource utilization in patients with asthma in Japan. NPJ Prim Care Respir Med. 2019;29:13.
To Y, Taguchi Y, Shimazaki T, et al. Real-world treatment and health care resource use among severe asthma patients in Japan. Respir Investig. 2021;59:464–77.
Ueda N, Yakushiji A, Schelfhout J, Tokita S, Kubo T. Impact of refractory and unexplained chronic cough on disease burden: a qualitative study. BMC Pulm Med. 2022;22:372.
Kubo T, Tobe K, Okuyama K, et al. Disease burden and quality of life of patients with chronic cough in Japan: a population-based cross-sectional survey. BMJ Open Respir Res. 2021;8.
Cazzola M, Ora J, Cavalli F, Rogliani P, Matera MG. Treatable mechanisms in asthma. Mol Diagn Ther. 2021;25:111–21.
Pavord ID, Beasley R, Agusti A, et al. After asthma: redefining airways diseases. Lancet. 2018;391:350–400.
Castro M, Corren J, Pavord ID, et al. Dupilumab efficacy and safety in moderate-to-severe uncontrolled asthma. N Engl J Med. 2018;378:2486–96.
Ortega HG, Yancey SW, Mayer B, et al. Severe eosinophilic asthma treated with mepolizumab stratified by baseline eosinophil thresholds: a secondary analysis of the DREAM and MENSA studies. Lancet Respir Med. 2016;4:549–56.
Lee LA, Bailes Z, Barnes N, et al. Efficacy and safety of once-daily single-inhaler triple therapy (FF/UMEC/VI) versus FF/VI in patients with inadequately controlled asthma (CAPTAIN): a double-blind, randomised, phase 3A trial. Lancet Respir Med. 2021;9:69–84.
Mukae H, Kaneko T, Obase Y, et al. The Japanese respiratory society guidelines for the management of cough and sputum (digest edition). Respir Investig. 2021;59:270–90.
Fukumitsu K, Kanemitsu Y, Asano T, et al. Tiotropium attenuates refractory cough and capsaicin cough reflex sensitivity in patients with asthma. J Allergy Clin Immunol Pract. 2018;6(1613–20): e2.
Kanemitsu Y, Matsumoto H, Oguma T, et al. Independent factors contributing to daytime and nighttime asthmatic cough refractory to inhaled corticosteroids. J Investig Allergol Clin Immunol. 2019;29:30–9.
Bukstein DA, Guerra DG Jr, Huwe T, Davis RA. A review of shared decision-making: a call to arms for health care professionals. Ann Allergy Asthma Immunol. 2020;125:273–9.
Wilson SR, Strub P, Buist AS, et al. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med. 2010;181:566–77.
Engelkes M, Janssens HM, de Jongste JC, Sturkenboom MC, Verhamme KM. Medication adherence and the risk of severe asthma exacerbations: a systematic review. Eur Respir J. 2015;45:396–407.
Murphy AC, Proeschal A, Brightling CE, et al. The relationship between clinical outcomes and medication adherence in difficult-to-control asthma. Thorax. 2012;67:751–3.
Bogart M, Glassberg MB, Reinsch T, Stanford RH. Impact of prompt versus delayed initiation of triple therapy post COPD exacerbation in a US-managed care setting. Respir Med. 2018;145:138–44.
Mannino D, Bogart M, Germain G, et al. Benefit of prompt versus delayed use of single-inhaler fluticasone furoate/umeclidinium/vilanterol (FF/UMEC/VI) following a COPD exacerbation. Int J Chron Obstruct Pulmon Dis. 2022;17:491–504.
Sicras Mainar A, Huerta A, Navarro Artieda R, Monso E, Landis SH, Ismaila AS. Economic impact of delaying initiation with multiple-inhaler maintenance triple therapy in Spanish patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2019;14:2121–9.
Arcury TA, Sandberg JC, Melius KP, et al. Older adult internet use and ehealth literacy. J Appl Gerontol. 2020;39:141–50.
Aiyegbusi OL, Roydhouse J, Rivera SC, et al. Key considerations to reduce or address respondent burden in patient-reported outcome (PRO) data collection. Nat Commun. 2022;13:6026.
To M, Hitani A, Kono Y, et al. Obesity-associated severe asthma in an adult Japanese population. Respir Investig. 2018;56:440–7.
Ilmarinen P, Stridsman C, Bashir M, et al. Level of education and asthma control in adult-onset asthma. J Asthma. 2022;59:840–9.
Hasegawa K, Stoll SJ, Ahn J, Kysia RF, Sullivan AF, Camargo CA Jr. Association of insurance status with severity and management in ED patients with asthma exacerbation. West J Emerg Med. 2016; 17:22–7.
Acknowledgements
Permission for use of the scale and its coding is required. A license agreement is available from MMAR, LLC., Donald E. Morisky, ScD, ScM, MSPH, 294 Lindura Ct., USA; donald.morisky@moriskyscale.com. Permission for use of the J-LCQ is required for commercial studies supported by the pharmaceutical industry; studies meeting these criteria should email Professor Akio Niimi for permission: a.niimi@med.nagoya-cu.ac.jp. Permission to use the AHQ-33, J-LCQ and MMAS was acquired, and we thank the respective rights holders. Permission to use the ACT and WPAI was not required.
Medical Writing, Editorial, and Other Assistance
GSK was involved in the study design, data analysis and interpretation, and preparation of the report. Data collection and analysis was performed by Mebix, Inc., and was funded by GSK. The MMAS-8 Scale, content, name, and trademarks are protected by US copyright and trademark laws. Editorial support, in the form of preparation of the first draft based on input from all authors, and collation and incorporation of author feedback to develop subsequent drafts, was provided by Ben Usher, PhD, of Fishawack Indicia Ltd, UK, part of Avalere Health, and was funded by GSK.
Funding
This study was funded by GSK (GSK Study 214955). Funding for Advances in Therapy’s Rapid Service and Open Access fees was also provided by GSK.
Author information
Authors and Affiliations
Contributions
The authors meet criteria for authorship as recommended by the International Committee of Medical Journal Editors, take responsibility for the integrity of the work as a whole, contributed to the writing and reviewing of the manuscript, and have given final approval for the version to be published. Hiroyuki Nagase, Takeo Ishii, and Risako Ito contributed to the conception and design of the study, and data analysis and interpretation. Moe Ishii and Hideki Shibata contributed to the conception and design of the study, acquisition of data, and data analysis and interpretation. Shintaro Suo and Liza Yuanita contributed to the data analysis and interpretation. Isao Mukai, Shiyuan Zhang, Kieran J. Rothnie, and Claire Trennery contributed to the conception and design of the study.
Corresponding authors
Ethics declarations
Conflict of Interest
Hiroyuki Nagase has received speaker and consultation fees from GSK, and speaker fees from AstraZeneca, Boehringer Ingelheim, Kyorin Pharmaceutical, Novartis and Sanofi. Risako Ito, Shiyuan Zhang, Kieran J. Rothnie and Liza Yuanita are employees of GSK and own stocks/shares in GSK. Isao Mukai is an employee of GSK. Claire Trennery and Takeo Ishii were employees of GSK at the time of the study and own stocks/shares in GSK. Hideki Shibata and Shintaro Suo are employees of Mebix, Inc., an agency that received funding from GSK to undertake this study; Moe Ishii was an employee of Mebix, Inc. at the time of the study.
Ethical Approval
This study was carried out in accordance with the Declaration of Helsinki, Ethical Guidelines for Medical and Biological Research Involving Human Subjects, and Japanese laws and regulations. Prior to study initiation, documented approval was obtained from the Takahashi Clinic Ethics Committee (LNW00148). To enrol in the study, participants first provided electronic informed consent. Individuals had the option to discontinue their participation at any point, whereupon they were considered as not consenting and were discounted as survey responders. Data collected were anonymised and all data were processed in compliance with the Act on the Protection of Personal Information and related notices applicable to the protection of personal information.
Additional information
Moe Ishii, Claire Trennery, Takeo Ishii: affiliation at the time of study.
Prior presentation: Part of the data included in this manuscript have been presented as a poster presentation at the 63rd annual meeting of the Japanese Respiratory Society 2023, 28–30 April 2023, Tokyo, Japan: Nagase H, et al. Japanese Respiratory Society 2023: Poster PP570.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Nagase, H., Ito, R., Ishii, M. et al. Relationship Between Asthma Control Status and Health-Related Quality of Life in Japan: A Cross-Sectional Mixed-Methods Study. Adv Ther 40, 4857–4876 (2023). https://doi.org/10.1007/s12325-023-02660-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02660-5