Abstract
There is a bidirectional pathophysiological interaction between the heart and the kidneys, and prolonged physiological stress to the heart and/or the kidneys can cause adverse cardiorenal complications, including but not limited to subclinical cardiomyopathy, heart failure and chronic kidney disease. Whilst more common in individuals with Type 2 diabetes, cardiorenal complications also occur in the absence of diabetes. Sodium-glucose cotransporter 2 inhibitors (SGLT2i) were initially approved to reduce hyperglycaemia in patients with Type 2 diabetes. Recently, these agents have been shown to significantly improve cardiovascular and renal outcomes in patients with and without Type 2 diabetes, demonstrating a robust reduction in hospitalisation for heart failure and reduced risk of progression of chronic kidney disease, thus gaining approval for use in treatment of heart failure and chronic kidney disease. Numerous potential mechanisms have been proposed to explain the cardiorenal effects of SGLT2i. This review provides a simplified summary of key potential cardiac and renal mechanisms underlying the cardiorenal benefits of SGT2i and explains these mechanisms in the clinical context. Key mechanisms related to the clinical effects of SGLT2i on the heart and kidneys explained in this publication include their impact on (1) tissue oxygen delivery, hypoxia and resultant ischaemic injury, (2) vascular health and function, (3) substrate utilisation and metabolic health and (4) cardiac remodelling. Knowing the mechanisms responsible for SGLT2i-imparted cardiorenal benefits in the clinical outcomes will help healthcare practitioners to identify more patients that can benefit from the use of SGLT2i.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
There is a bidirectional pathophysiological interaction between the heart and the kidneys, with heart failure and chronic kidney disease often causing or worsening the other |
Sodium-glucose cotransporter 2 inhibitors were initially approved for treatment of Type 2 diabetes but have since demonstrated significant cardiorenal benefits to patients with and without Type 2 diabetes; however, the mechanisms via which these benefits are imparted are largely unknown |
We present three key SGLT2i mechanisms via which this class of therapeutics imparts its cardiorenal benefits; these include improvement in kidney function and tissue oxygen delivery, vascular health and function and metabolic health |
The use of SGLT2i therapy in treating HF and CKD in individuals with and without T2D has a marked impact, reducing the risk associated with worsening of these conditions |
Digital Features
This article is published with digital features, including an infographic to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.23968659.
Introduction
Heart failure (HF) and chronic kidney disease (CKD) are major health problems worldwide. Globally, approximately 64 million people are estimated to have HF, with the disease having a 5-year mortality rate of nearly 50% and predicted to rise significantly by 2030 (24% increase [1, 2]). Similarly, CKD-related mortality and rates of treatment requiring kidney replacement have been rising globally over the last few decades (Fig. 1) [3, 4]. Notably, despite this, a substantial number of patients with HF and CKD remain undiagnosed, especially in the early disease stages [5, 6].
Epidemiology and global burden of CKD and HF. Calculation of disease burden using DALYs: one DALY represents the loss of the equivalent of 1 year of full health. DALYs for a disease or health condition are the sum of the years of life lost to the condition because of premature mortality. CKD chronic kidney disease, DALY, disability-adjusted life year, HF heart failure, IHD ischaemic heart disease. 1. GDB collaboration. Lancet. 2020;395(10225):709–733; 2. National Kidney Foundation. https://www.kidney.org/kidneydisease/global-facts-about-kidney-disease; 3. Lippi et al. AME Med J. 2020;5:15; 4. Roth et al. J Am Coll Cardiol. 2020;76(25)2982–3021
HF and CKD form a vicious circle, in which one disease causes or worsens the other, leading to cardiorenal syndrome [7]. There is an interdependent relationship between the heart and kidneys, wherein the crosstalk is done via various haemodynamic, neurohormonal, inflammatory and metabolic processes [8]. The pathophysiological interaction between these organs is bidirectional, and prolonged physiological stress to either organ can ultimately lead to adverse cardiorenal complications, including but not limited to subclinical cardiomyopathy, advanced HF or CKD (Fig. 2) [9].
Bidirectional pathophysiological interaction between the heart and the kidneys. 1. Sattar N, McGuire DK. Circulation. 2018;138(1):7–9; 2. Verma S, et al. Diabetes Care. 2016;39(12):e212-e3; 3. Kang S, et al. Can J Cardiol. 2020;36(4):543–53; 4. Santos-Gallego CG, et al. J Am Coll Cardiol. 2019;73(15):1931–4; 5. Ronco C, et al. J Am Coll Cardiol. 2008;52(19):1527–39; 6. Rangaswami J, et al. Circulation. 2019;139(16):e840–e78
Sodium-glucose cotransporter 2 inhibitors (SGLT2i) were initially approved for treatment of Type 2 diabetes—and act by selectively inhibiting SGLT2-mediated glucose and sodium reabsorption in the proximal tubule of the kidneys, leading to their increased excretion in the urine (known as glycosuria and natriuresis, respectively) and lowering of blood glucose levels in patients with diabetes. This mechanism of action is insulin independent, thus minimising the risk of hypoglycaemia [10].
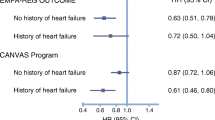
SGLT2i have also been shown to reduce hospitalisations due to HF and death from cardiovascular (CV) causes in patients with and without T2D [11,12,13,14,15,16]. The EMPA-REG Outcome trial was the first SGLT2i study showing that patients with T2D at high risk for CV events receiving empagliflozin had a lower rate of death from CV causes, nonfatal myocardial infarction or nonfatal stroke and death from any cause [13]. Subsequently, DECLARE-TIMI 58 and CANVAS showed that in patients with T2D with a history of atherosclerotic CV disease (CVD) or with high risk for CVD, both dapagliflozin and canagliflozin reduced the rate of CV death or hospitalisation for HF (hHF) [14]. A post hoc analysis of the DECLARE-TIMI 58 study showed that participants achieved cardiorenal benefits with dapagliflozin treatment, irrespective of their baseline HbA1c level [17]. Another large meta-analysis showed SGLT2i to have robust benefits on reducing hHF and progression of kidney disease regardless of existing atherosclerotic CVD or history of HF [18]. DAPA-HF was the first study to demonstrate the CV benefits of SGLT2i in patients with established HF and reduced ejection fraction, regardless of the presence of T2D [11]. The EMPEROR-preserved and -reduced trials and the CHIEF-HF trial replicated these results with empagliflozin and canagliflozin, respectively [16, 19, 20]. Recently, the DELIVER study showed that in patients with HF and a mildly reduced or preserved ejection fraction, dapagliflozin reduced the combined risk of worsening HF or CV death, with lowered symptom burden and without excess adverse events [21]. Results of a patient-level, pooled meta-analysis of the DAPA-HF and DELIVER trials indicated that in patients with HF, dapagliflozin significantly reduced the risk of death from CV causes, any-cause death and major adverse CV events, irrespective of left ventricular ejection fraction; furthermore, there was a larger reduction in total hHF than in death, indicating that most patients with HF, regardless of ejection fraction, are likely to benefit from SGLT2 treatment [22]. Results of another meta-analysis, including five major randomised controlled trials, namely, DELIVER, DAPA-HF, EMPEROR-Preserved, EMPEROR-Reduced and SOLOIST-WHF, were also aligned to the abovementioned studies. Together, these data provide a strong case for the use of SGLT2i for the treatment of HF, irrespective of the presence of left ventricular ejection fraction or the care setting [23].
In addition to demonstrating the CV benefits of canagliflozin, the CANVAS program also showed a possible benefit of canagliflozin in slowing the progression of albuminuria, implying at the possibility of renal benefits of SGLT2i in patients with T2D [12]. Subsequently, the DAPA-CKD study showed that in patients with CKD, regardless of the presence of T2D, dapagliflozin significantly lowered progression of kidney disease and reduced the risk of death from renal or CV causes [24,25,26]. Similar results were seen in the EMPA-REG trial using empagliflozin in patients with and without diabetes and in the CREDENCE trial with canagliflozin in T2D patients [27, 28] (Table 1). Thus, selected SGLT2i have received approval for use in the treatment of HF and CKD in the USA, Europe and many other countries [29,30,31].
Various potential mechanisms have been proposed to explain how SGLT2i impart cardiorenal benefits. This review provides a simplified summary of key potential cardiac and renal mechanisms underlying the cardiorenal benefits of SGLT2i, which can assist in identifying more patients that can benefit from the use of these agents (Fig. 3).
Clinical effects of SGLT2i-mediated cardiorenal protection. CVD cardiovascular disease, eGFR, estimated glomerular filtration rate, ESKD end-stage kidney disease, SGLT2i sodium–glucose cotransporter 2 inhibitor. 1. Sattar N, McGuire DK. Circulation. 2018;138(1):7–9; 2. Verma S, et al. Diabetes Care. 2016;39(12):e212-e3; 3. Kang S, et al. Can J Cardiol. 2020;36(4):543–53; 4. Santos-Gallego CG, et al. J Am Coll Cardiol. 2019;73(15):1931–4; 5. Staels B. Am J Med. 2017;130(6 s):S30-s9; 6. Hallow KM, et al. Diabetes Obes Metab. 2018;20(3):479–87; 7. Solini A, et al. Cardiovasc Diabetol. 2017;16(1):138; 8. Maruyama T, et al. Diabetes Technol Ther. 2019;21(12):713–720; 9. Heerspink HJL, et al. N Engl J Med. 2020;383(15):1436–1446; 10. Heerspink HJL, et al. Lancet Diabetes Endocrinol. 2021;9(11):743–754; 11. Mosenzon O, et al. Diabetes Care. 2021;44(8):1805–15; 12. Hallow KM, et al. Am J Physiol Renal Physiol. 2018;315(5):F1295-F1306; 13. Heerspink HJL, et al. Kidney Int. 2018;94(1):26–39; 14. Packer M. Diabetes Care. 2020;43(3):508–11
Infographic

Improvement in Kidney Function and Tissue Oxygen Delivery
Glomerular filtration and solute reabsorption via the proximal tubules are critical aspects of kidney function. These critical processes appear to be altered in several kidney diseases [32,33,34]. SGLT2i act by selectively inhibiting SGLT2-mediated glucose and sodium reabsorption in the proximal tubule of the kidneys, leading to glycosuria, natriuresis and osmotic diuresis. The metabolic and natriuretic effects of SGLT2i are in themselves potentially beneficial for kidney function. In patients with kidney-related conditions, like diabetes and CKD, decreased sodium delivery to the macula densa in the kidneys causes glomerular vasodilation and hyperfiltration (GFR above normal). SGLT2i reduce sodium reabsorption in the proximal tubule and increase its delivery to the macula densa, thus increasing tubuloglomerular feedback and reducing hyperfiltration. This action of SGLT2i is complementary to angiotensin-converting enzyme inhibitors, which reduce intraglomerular pressure and hyperfiltration by dilating the efferent renal arterioles.
The rate of urinary albumin excretion is a clinical marker highlighting the severity of kidney disease, with albuminuria-improving treatments being associated with a reduction in the progression of CKD [35]. Use of SGLT2i showed a marked reduction in excretion of urinary albumin (as indicated by the improved urinary albumin-to-creatinine ratio [UACR]), an initial decrease in estimated glomerular filtration rate (eGFR) and a longer-term slowing of the rate of eGFR decline [26, 32, 36, 37]. A secondary analysis of the DECLARE-TIMI 58 study showed that dapagliflozin not only reduced the rate of new-onset micro- or macroalbuminuria relatively early during the trial but also showed statistically significant reduction of urinary albumin excretion in patients in all UACR categories (UACR ≤ 15, 15 < UACR < 30, 30 ≤ UACR ≤ 300 and 300 < UACR mg/g) [38]. In patients with vascular disease, changes in albuminuria have been shown to predict mortality and cardiovascular and renal outcomes, independent of baseline albuminuria, implying the presence of an underlying albuminuria-associated mechanism playing a role in the cardiorenal benefits of SGLT2i [39]. It has been postulated that SGLT2i may exert these benefits by favourably affecting glomerular hydrostatic pressure, plasma volume, arterial stiffness and tissue (interstitial) fluid [13, 40,41,42,43,44].
The DIAMOND study was the first investigation evaluating the renal haemodynamic and albuminuria-lowering effects of dapagliflozin treatment in 53 subjects with non-diabetic proteinuric CKD. Results showed that compared with placebo, dapagliflozin did not significantly affect proteinuria while causing an acute but reversible decline in GFR and reduction in bodyweight and blood pressure, though subsequent randomised controlled trials demonstrated that SGLT2i did indeed reduce proteinuria and delay progression of kidney disease in patients with albuminuria [45,46,47]. The DIAMOND study also demonstrated that whilst conferring these benefits, dapagliflozin did not reduce HbA1c or fasting plasma glucose in subjects without diabetes, nor were kidney haemodynamics adversely affected in this population. This implies that dapagliflozin treatment has ubiquitous positive effects on kidney function irrespective of glycaemic status [48]. These positive effects may be mediated via tubuloglomerular feedback in individuals without T2D as they have lower glucose filtration than individuals with diabetes. It is possible that the activation of tubuloglomerular feedback, and/or another autoregulatory system, by SGLT2i, may not affect proteinuria in individuals without diabetes, thus offering renoprotection [48].
Increased Erythropoietin Production
Erythropoietin (EPO) is produced by interstitial fibroblasts in the kidneys in a process involving oxygen sensing. In patients with diabetes, excessive glucose reabsorption overtaxes the proximal tubules, increasing oxygen requirement and causing tubulointerstitial hypoxia. As a consequence, damaged renal tubules undergo transformation, losing their function, thus impairing EPO production. SGLT2 inhibitors reduce the workload of the proximal tubules and improve tubulointerstitial hypoxia, allowing fibroblasts to resume EPO production, thereby leading to an increase in erythropoiesis and an increase in haemoglobin/haematocrit levels. Thus, increased haematocrit could indicate reduced renal stress in diabetic patients [49]. This mechanism has been demonstrated in patients with T2D using dapagliflozin and canagliflozin [50, 51]. Dapagliflozin has also been associated with a modest increase (2–4%) in haematocrit [52]. The resulting increase in haematocrit leads to increased oxygen delivery to tissues, particularly to the heart, which may account for some of the beneficial CV effects of SGLT2i. An exploratory analysis of a phase 3 trial of empagliflozin showed that increases in haemoglobin and haematocrit were the most important mediators of the reduction in risk of CV mortality [53, 54]. This may have implications in individuals with worsening heart conditions or obesity, wherein oxygen delivery by the heart is ineffective due to the increased need for oxygen [55]. However, more research is required to investigate this aspect.
Improvements in Anaemia
As explained above, treatment with SGLT2i showed increase in levels of haemoglobin, haematocrit and EPO, thus assisting with correcting and/or preventing anaemia [50,51,52,53, 56]. SGLT2i may also alleviate renal hypoxia and prevent resulting kidney injury by improving oxygen supply to the kidneys through improved cardiac function and by reducing renal oxygen requirements in the proximal tubules [32, 36, 57, 58]. Both dapagliflozin and empagliflozin were shown to assist with correcting and/or preventing anaemia in patients with HF irrespective of the presence of diabetes [59, 60]. Increase in haematocrit and haemoglobin could also indicate changes in natriuresis and effective circulating volume contraction. This small increase in haemo-concentration may be linked with improved cardiovascular prognosis in cardiovascular outcome trials involving SGLT2is in individuals with T2D [61].
Improved Cardiovascular Health
Improved Endothelial Function
The endothelium maintains vascular homeostasis through several complex physiological functions, including release of vasoactive factors that regulate vascular tone, blood fluidity and coagulation, while limiting smooth muscle cell proliferation and inflammation. Endothelial dysfunction is a consistent finding in individuals with T2D and can independently predict risk of CV disease [62]. SGLT2i have been shown to improve endothelial function, thus positively affecting vascular function [43]. It has been proposed that this improvement may be related to reduced exposure of the endothelium to sodium and glucose [43, 63, 64]. In vitro observations indicate that SGLT2i may confer cardioprotection partly through their ability to preserve and restore the structural integrity of the endothelial glycocalyx—a protective matrix-like barrier of macromolecules that helps to maintain vascular health by promoting the anti-inflammatory action of the endothelium [65]. Indeed, a preliminary study showed improved systemic endothelial function after 48 h of treatment with dapagliflozin [43]. The randomised, open-label DEFENCE study showed a similar effect, with dapagliflozin improving endothelial function when used in combination with metformin in patients with T2D—an effect that was observed alongside a significant reduction in oxidative stress [66].
Decreased Vascular Stiffness and Inflammation
Increased ventricular mass is associated with an increased risk of CVD. SGLT2i have been shown to improve arterial stiffness and prompt regression towards a normal ventricular mass, thus conferring protection against HF and arrhythmias [67, 68]. A pilot study reported a significant improvement in systemic endothelial function and arterial stiffness 48 h after treatment with dapagliflozin. This was independent of changes in blood pressure and was observed with stable urinary excretion of sodium, suggesting a fast and beneficial effect on the blood vessels, possibly mediated by a reduction in oxidative stress [43]. A recent meta‐analysis of a double‐blind placebo-controlled randomised trial evaluating left ventricular remodelling by cMRI observed that SGLT2i significantly and consistently reduced left ventricular mass in individuals with HF, with and without diabetes, proposing this as a potential mechanism responsible for positive CV effects of SGLT2i [69].
SGLT2i may also be able to confer cardio-protection via a range of anti-inflammatory actions at the tissue and organ levels [70]. For example, hyperuricaemia is common in individuals with heart and kidney diseases, which appears to promote CV pathophysiology by proliferating vascular smooth muscle cells and increasing production of pro-inflammatory, pro-oxidative and vasoconstrictive mediators [71,72,73]. Having demonstrated activity in reducing uric acid levels [74,75,76], it is possible that SGLT2i may be able to ameliorate this pathological pathway. SGLT2i reduce uric acid levels by increasing its excretion in urine. Unabsorbed glucose is thought to compete with uric acid for a glucose transporter in the renal tubules, a major regulator of uric acid homeostasis, explaining why reduction in uric acid levels was greater in individuals without T2D and in those with lower HbA1c in the DAPA-HF study [77].
Another potential mechanism is related to epicardial adipose tissue (EAT), which supplies free fatty acids for energy production by cardiac muscle cells and has been associated with coronary atherosclerosis and insulin resistance [78, 79]. In individuals with T2D and HF, EAT is also known to produce large quantities of activin A, an inflammation-enhancing cytokine [80]. Dapagliflozin and canagliflozin have been shown to decrease EAT in individuals with T2D [81, 82], thus reducing vascular inflammation and fibrosis, possibly by improving the balance between inflammation-promoting and -reducing cytokines secreted by the adipose tissue [42].
Improved Balance of Intra and Extravascular Fluid Volume
SGLT2i reduce volume overload as a result of osmotic diuresis in patients with T2D due to glycosuria resulting in a decrease in intravascular volume [83]. This helps to lessen the strain/stretch on the heart, known as myocardial preload [84]. These actions may also contribute to reduction in ventricular mass. Individuals with HF also suffer from congestion, wherein fluid accumulates both inside and outside the blood vessels. SGLT2i have been shown to reduce the volume of tissue fluid to a greater extent than blood volume, thus increasing fluid clearance and reducing congestion, with minimal impact on circulation, arterial filling, activation of the renin-angiotensin-aldosterone system (RAAS) in response to a drop in blood pressure and blood supply to organs. Consequently, vasoconstriction in response to a fall in blood volume is prevented—an aggravating effect seen with other diuretic treatments [43, 85].
Beneficial effects of SGLT2i on blood volume have also been demonstrated in individuals without T2D [86, 87]. Empagliflozin decreases 24‐h systolic blood pressure by 5 mmHg with significant renal tubular effects in individuals with normal blood pressure; mechanisms involved in this decrease were independent of weight control but may be related to volume contraction [86]. Empagliflozin has also been shown to reduce pulmonary pressure in patients with HF, possibly via modulation of sympathetic activity [87, 88]. Furthermore, in individuals without T2D, it has been hypothesized that SGLT2i-induced osmotic diuresis results in greater electrolyte-free water clearance and thus in greater fluid clearance from the interstitial fluid (IF) space than from the circulation. This alleviates cardiac congestion with minimal impact on blood volume, arterial filling and organ perfusion. Using a mathematical model, this hypothesis was tested using data from a study in healthy subjects receiving dapagliflozin or bumetanide; the model predicted that dapagliflozin produces a twofold greater reduction in IF volume compared to blood volume, while the reduction in IF volume with bumetanide is only 78% of the reduction in blood volume. Excess fluid accumulation in the vascular compartment and IF space is a typical characteristic of HF. Thus, by causing a greater reduction in IF volume compared with that in blood volume, SGLT2i may provide better cardiorenal protection in individuals without T2D [85, 89].
Regulation of sodium ion channels in the heart and kidneys may also be a way in which SGLT2i produce their cardiorenal benefits. For example, evidence suggests that dapagliflozin may help to reduce blood pressure by improving the sodium balance [90]. The sodium-hydrogen exchanger-3 (NHE3) in kidneys mediates sodium reabsorption following renal glomerular filtration [91,92,93]. Reduced NHE3 activity in the proximal tubule following treatment with SGLT2i leads to decreased sodium reabsorption followed by lowering of glomerular pressure, and reduction of blood and tissue fluid volume. Sodium-hydrogen exchanger-1 (NHE1) is also thought to play an important role in the pathogenesis of HF [91]. NHE1 activity is raised in HF, and its inhibition decreases susceptibility to severe ventricular arrhythmia, reduces contractile dysfunction and limits tissue death/damage both when blood supply to the heart muscle is insufficient (ischaemia), and when it subsequently returns (reperfuses) [94]. Benefits of SGLT2i on HF have been suggested to be mediated by inhibition of sodium-hydrogen exchange in the heart via NHE1, thus resulting in reduced sodium concentration [14, 42, 95,96,97]. It is possible that SGLT2i may favourably induce cardiac remodelling by these mechanisms, thus reducing the risk of arrhythmias and sudden death [42, 97]. However, a recent study found that empagliflozin and other SGLT2i had no effect on cardiac NHE1 activity over a range of concentrations, including the therapeutic dose, warranting further research on this hypothesis [98].
Suppressed Collagen Synthesis/Fibrosis
Cardiac fibrosis is widely regarded as a pathway leading to HF [42]. The fibrosis results from remodelling of the heart, making the ventricles less compliant to expansion and thus accelerating development of HF. In individuals with diabetes, remodelling of the extracellular matrix leads to accumulation of collagen, subsequent cross-linking of the collagen and activation of signalling pathways promoting fibrosis [99]. These structural changes contribute to the cardiac stiffness and diastolic dysfunction seen in individuals with diabetes, which ultimately produce stress on the heart wall, chamber enlargement and contractile dysfunction [100]. Dapagliflozin and empagliflozin have been shown to prevent cardiac fibrosis in studies with murine myocytes [101, 102]. Similarly, preliminary data using human myofibroblasts have shown that empagliflozin may have a direct effect on restructuring of the extracellular matrix via attenuation of myofibroblast activity and cell-mediated collagen remodelling. This may be a potential mechanism for SGLT2i-mediated CV benefits in individuals without T2D [103].
Improved metabolic health
Shift in Substrate Utilisation
The constant high-energy demand of the heart is primarily met by the oxidation of lipid-derived long-chain fatty acids [104]. However, it can also derive energy from several other substrates, including glucose, pyruvate and lactate; a proportional amount of ketones may also be used to generate energy. Under conditions of a mild persistent elevation of ketones in the blood (hyperketonaemia), as is seen in T2D and HF, larger-than-usual amounts of the ketone, beta-hydroxybutyrate, are taken up by the heart for energy utilisation instead of fatty acids [67, 105]. It is proposed that this improves transduction of oxygen consumption into work efficiency at the mitochondrial level. Furthermore, SGLT2i-induced haemoconcentration enhances oxygen release. Thus, aligned with other SGLT2i benefits, such a metabolic substrate shift is capable of conferring cardioprotection in diabetic and non-diabetic patients.
Based on studies involving dapagliflozin and empagliflozin, it has been hypothesised that SGLT2i shift metabolism towards the oxidation of free fatty acids and stimulate ketone production (ketogenesis) [106, 107]. This shift results in increased levels of beta hydroxybutyrate in circulation, which offers significant cardioprotection to individuals with diabetes [67, 108, 109]. The shift in substrate utilisation can also be explained as follows. In individuals with prolonged diabetes, there is altered insulin sensitivity and a decrease in insulin-stimulated glucose disposal. Dapagliflozin treatment induces glucosuria, lowers plasma glucose and increases insulin-stimulated glucose disposal. This increase in glucose uptake is mainly reflected in an increase in non-oxidative glucose disposal (glycogen synthesis), while glucose oxidation is decreased. To meet the energy demand of the cell, there is a switch from glucose to fat oxidation for energy production [106], accompanied by increased ketone production. These changes in fuel utilisation may lead to improvements in the function and efficiency of the heart [107, 110]. Stimulation of ketogenesis also imparts benefits such as reductions in inflammatory responses and blood pressure [111, 112].
Improved Mitochondrial Function
Autophagy is a cellular degradation and recycling process [113]. The process involves the recycling of unwanted cellular components, degrading the glycogen and lipids present in the components to generate adenosine triphosphate (ATP), the most basic form of cellular fuel. Autophagy also serves to remove damaged mitochondria and other organelles from the cytosol, thereby reducing oxidative stress and inflammation [114]. On detection of low energy levels by the mitochondria, the enzymes sirtuin 1 (SIRT1) and 5’ adenosine monophosphate-activated protein kinase (AMPK) function stimulate autophagy [115]. Suppression of SIRT1-AMPK signalling pathway results in impaired autophagy, which may play a role in the pathogenesis of heart and kidney diseases in individuals with T2D [115]. Impaired autophagy has also been linked to dysfunction of cardiac muscle cells, increased inflammation and appearance of renal lesions in diabetic nephropathy [115]. By assessing changes in circulating protein levels in patients with HF, Zannad et al. explored the effect of empagliflozin on the circulating levels of intracellular proteins by using large-scale proteomics in 1134 patients with HF from the EMPEROR-Reduced and EMPEROR-Preserved studies. They showed that empagliflozin altered heart proteins, promoting autophagic flux. Other treatment effects of empagliflozin, including reduced oxidative stress, inhibition of inflammation and fibrosis, enhanced energy stores and increased regenerative capacity of the heart, also contributed in imparting positive cardiac changes. Changes in circulating protein levels in patients with HF seen in this study are consistent with the findings of other experimental studies showing that the effects of SGLT2i are likely related to actions on the heart and kidney to promote autophagic flux, nutrient deprivation signalling and transmembrane sodium transport [116].
Hyperglycaemia may increase mitochondrial oxygen consumption, causing cellular hypoxia [117, 118]. Thus, by reducing blood glucose levels, anti-hyperglycaemic drugs may be capable of promoting autophagy by inducing activation of various low-energy sensors, such as SIRT1 and AMPK. Indeed anti-hyperglycaemic drugs, such as incretins and thiazolidinediones, have been shown to induce autophagy [119,120,121]. However, the magnitude of this effect may be offset by other actions. It has been proposed that SGLT2i activate SIRT1-AMPK signalling, thus promoting autophagy [115]. It is possible that the magnitude of autophagy induced by SGLT2i is more prominent compared to other anti-hyperglycaemic drugs because of several other SGLT2i-associated mechanisms involved in the manifestation of the cardiorenal benefits shown by this drug class. Increased autophagy leads to reduced oxidative stress, normalised mitochondrial structure and function, suppressed inflammation, reduced injury to coronary vessels, enhanced cardiac performance and lowered risk of cardiomyopathy [115]. Kidney cells, including podocytes and proximal tubular cells, strongly express AMPK, and metabolic-related renal diseases—like obesity-related and diabetic chronic kidney disease—are associated with dysregulated AMPK in the kidneys. Conversely, activating AMPK ameliorates the pathological and phenotypical features in such renal diseases [122]. Mimicking the cellular response to starvation by indirectly activating low-energy sensor AMPK, SGLT2i hinder the development of nephropathy [115].
Figure 3 details the various mechanisms that may be involved in cardiorenal protection by SGLT2i.
Other: Cardiac Remodelling
In addition to improved cardio-energetics (see ‘Shift in substrate utilisation’) and positive effects on ventricular mass (see ‘Decreased vascular stiffness and inflammation’), SGLT2i have also been indicated to play a decisive role in cardiac remodelling. Individuals with T2D may have decreased ability to revascularise ischaemic tissues due to low levels of circulating perivascular progenitor cells. Recent data suggest SGLT2i stimulate vascular repair via increased trafficking of bone marrow—derived haematopoietic stem/progenitor cells (HSPCs)—known to be essential for regeneration of cardiac vessels in individuals without T2D [123, 124]. Dapagliflozin improved endothelial repair through enhanced HSPCs at the site of vessel injury for repair, thus facilitating cardiac regenerative and remodelling processes [125]. Restoration of vascular regenerative cell production, by reducing glucotoxicity and systemic inflammation post bariatric surgery or by modulating HSPC functions, may provide unique approaches for treating ischaemic disease using SGLT2i [126]. Dapagliflozin has also demonstrated enhanced healing of carotid artery wounds, wherein the vascular repair was stimulated, in part, through distinct alterations in systemic metabolism, including improved glucose control and induction of ketogenesis [125, 127]. Preventing adverse cardiac remodelling and/or preventing ischaemia/reperfusion injury is another way in which SGLT2i are associated with cardiac remodelling. Empagliflozin has been shown to prevent adverse left ventricular remodelling in nondiabetic pigs with HF, possibly by enhancing myocardial energetics [128]. A preliminary study in humans showed that empagliflozin improves ‘cardiac energy-deficient’ and hinders unwanted myocardial cellular remodelling, thus improving cardiac function and offering therapeutic opportunities to prevent or modulate HF in individuals with T2D [128].
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Adverse Effects of SGLT2i-Associated Mechanisms Imparting Cardiorenal Benefits
Under specific circumstances, some of the above-listed mechanisms activated by SGLT2i can produce undesirable effects. One such undesirable effect is normoglycaemic ketosis (blood glucose < 250 mg/dl; arterial pH < 7.3, serum bicarbonate < 18 mEq/l [severe metabolic acidosis] and presence of ketone bodies) [129]. This can have serious clinical consequences and may need professional intervention for resolution, which may require reducing SGLT2i dose or stopping SGLT2i treatment [130,131,132]. However, since these are known adverse events related to SGLT2i treatment; evidence and guidance are available for the clinical management of these conditions when patients are on SGLT2i therapy [132,133,134,135,136,137].
Conclusion
There is a bidirectional pathophysiological interaction between the heart and the kidneys. SGLT2i produce cardiorenal benefits that are not solely dependent on their effects to improve glycaemia and are not limited to individuals with T2D. In addition to the effects of SGLT2i on the heart and kidneys, other mechanisms involving alteration and regulation of metabolism, energy sources, sodium ion channels, haematocrit and EPO levels and anti-inflammatory effects may underlie their ability to confer cardiorenal protection to individuals with and without diabetes. The use of SGLT2i therapy in treating HF and CKD in individuals with and without T2D has a marked impact, reducing the risk associated with worsening of these conditions and decreasing complications in T2D. Notably, the use of SGLT2i therapy may be beneficial in managing multiple comorbidities and protecting the heart and the kidney from developing cardiorenal disease.
Data Availability
This publication is a review article based on information available in the public sector. As such we beleive that the data availibility statement does not apply to it.
References
GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1211–59.
Lippi G, Sanchis-Gomar F. Global epidemiology and future trends of heart failure. AME Med J 2020;5.
Jager KJ, Fraser SDS. The ascending rank of chronic kidney disease in the global burden of disease study. Nephrol Dial Transplant. 2017;32:ii121–ii28.
Liyanage T, Ninomiya T, Jha V, et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. 2015;385:1975–82.
Packer M. Do most patients with obesity or Type 2 diabetes, and atrial fibrillation, also have undiagnosed heart failure? A critical conceptual framework for understanding mechanisms and improving diagnosis and treatment. Eur J Heart Fail. 2020;22:214–27.
Tuttle KR, Alicic RZ, Duru OK, et al. Clinical characteristics of and risk factors for chronic kidney disease among adults and children: an analysis of the CURE-CKD Registry. JAMA Netw Open. 2019;2: e1918169.
Ronco C, Haapio M, House AA, Anavekar N, Bellomo R. Cardiorenal syndrome. J Am Coll Cardiol. 2008;52:1527–39.
Rangaswami J, Bhalla V, Blair JEA, et al. Cardiorenal syndrome: classification, pathophysiology, diagnosis, and treatment strategies: a scientific statement From the American Heart Association. Circulation. 2019;139:e840–78.
Sattar N, McGuire DK. Pathways to cardiorenal complications in Type 2 diabetes mellitus: A need to rethink. Circulation. 2018;138:7–9.
Vasilakou D, Karagiannis T, Athanasiadou E, et al. Sodium-glucose cotransporter 2 inhibitors for Type 2 diabetes: a systematic review and meta-analysis. Ann Intern Med. 2013;159:262–74.
McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381:1995–2008.
Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in Type 2 diabetes. N Engl J Med. 2017;377:644–57.
Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in Type 2 diabetes. N Engl J Med. 2015;373:2117–28.
Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in Type 2 diabetes. N Engl J Med. 2019;380:347–57.
Verma S, Jüni P, Mazer CD. Pump, pipes, and filter: do SGLT2 inhibitors cover it all? Lancet. 2019;393:3–5.
Anker SD, Butler J, Filippatos G, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385:1451–61.
Cahn A, Wiviott SD, Mosenzon O, et al. Association of baseline HbA1c with cardiovascular and renal outcomes: analyses from DECLARE-TIMI 58. Diabetes Care. 2022;45:938–46.
Zelniker TA, Wiviott SD, Raz I, et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet. 2019;393:31–9.
Bhatt D. Canagliflozin impact on health status, quality of life, and functional status in heart failure - CHIEF-HF. Presented at ACC 2021.
Packer M, Anker SD, Butler J, et al. Empagliflozin in patients with heart failure, reduced ejection fraction, and volume overload: EMPEROR-Reduced Trial. J Am Coll Cardiol. 2021;77:1381–92.
Solomon SD, McMurray JJV, Claggett B, et al. Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N Engl J Med. 2022;387:1089–98.
Jhund PS, Kondo T, Butt JH, et al. Dapagliflozin across the range of ejection fraction in patients with heart failure: a patient-level, pooled meta-analysis of DAPA-HF and deliver. Nat Med. 2022;28:1956–64.
Vaduganathan M, Docherty KF, Claggett BL, et al. SGLT-2 inhibitors in patients with heart failure: a comprehensive meta-analysis of five randomised controlled trials. Lancet. 2022;400:757–67.
Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383:1436–46.
Jongs N, Greene T, Chertow GM, et al. Effect of dapagliflozin on urinary albumin excretion in patients with chronic kidney disease with and without type 2 diabetes: a prespecified analysis from the DAPA-CKD trial. Lancet Diabetes Endocrinol. 2021;9:755–66;9:755–56.
Heerspink HJL, Jongs N, Chertow GM, et al. Effect of dapagliflozin on the rate of decline in kidney function in patients with chronic kidney disease with and without Type 2 diabetes: a prespecified analysis from the DAPA-CKD trial. Lancet Diabetes Endocrinol. 2021;9:743–54.
Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and renal outcomes in Type 2 diabetes and nephropathy. N Engl J Med. 2019;380:2295–306.
Herrington WG, Staplin N, Wanner C, et al. Empagliflozin in patients with chronic kidney disease. N Engl J Med. 2022;388:117–27.
US Food and Drug Administration. FDA approves treatment for chronic kidney disease. Press Release. https://www.fda.gov/news-events/press-announcements/fda-approves-treatment-chronic-kidney-disease [press release]. 2021.
AstraZeneca. Forxiga Summary of Product Characteristics 2017 [Available from: https://www.ema.europa.eu/en/documents/product-information/forxiga-epar-product-information_en.pdf.
US Food and Drug Administration. FDA approves new treatment for a type of heart failure [Available from: https://www.fda.gov/news-events/press-announcements/fda-approves-new-treatment-type-heart-failure.
Heerspink HJL, Kosiborod M, Inzucchi SE, Cherney DZI. Renoprotective effects of sodium-glucose cotransporter-2 inhibitors. Kidney Int. 2018;94:26–39.
Duni A, Liakopoulos V, Roumeliotis S, Peschos D, Dounousi E. Oxidative stress in the pathogenesis and evolution of chronic kidney disease: untangling Ariadne’s thread. Int J Mol Sci. 2019;20:3711.
Tonneijck L, Muskiet MH, Smits MM, et al. Glomerular hyperfiltration in diabetes: nechanisms, clinical significance, and treatment. J Am Soc Nephrol. 2017;28:1023–39.
Heerspink HJL, Greene T, Tighiouart H, et al. Change in albuminuria as a surrogate endpoint for progression of kidney disease: a meta-analysis of treatment effects in randomised clinical trials. Lancet Diabetes Endocrinol. 2019;7:128–39.
Heerspink HJ, Perkins BA, Fitchett DH, Husain M, Cherney DZ. Sodium glucose cotransporter 2 inhibitors in the treatment of diabetes mellitus: cardiovascular and kidney effects, potential mechanisms, and clinical applications. Circulation. 2016;134:752–72.
Jongs N, Greene T, Chertow GM, et al. Effect of dapagliflozin on urinary albumin excretion in patients with chronic kidney disease with and without Type 2 diabetes: a prespecified analysis from the DAPA-CKD trial. Lancet Diabetes Endocrinol. 2021;9:755–66.
Mosenzon O, Wiviott SD, Heerspink HJL, et al. The effect of dapagliflozin on albuminuria in DECLARE-TIMI 58. Diabetes Care. 2021;44:1805–15.
Schmieder RE, Mann JF, Schumacher H, et al. Changes in albuminuria predict mortality and morbidity in patients with vascular disease. J Am Soc Nephrol. 2011;22:1353–64.
Rieg T, Masuda T, Gerasimova M, et al. Increase in SGLT1-mediated transport explains renal glucose reabsorption during genetic and pharmacological SGLT2 inhibition in euglycemia. Am J Physiol Renal Physiol. 2014;306:F188–93.
Staels B. Cardiovascular protection by sodium glucose cotransporter 2 inhibitors: potential mechanisms. Am J Med. 2017;130:S30–9.
Verma S, McMurray JJV. SGLT2 inhibitors and mechanisms of cardiovascular benefit: a state-of-the-art review. Diabetologia. 2018;61:2108–17.
Solini A, Giannini L, Seghieri M, et al. Dapagliflozin acutely improves endothelial dysfunction, reduces aortic stiffness and renal resistive index in Type 2 diabetic patients: a pilot study. Cardiovasc Diabetol. 2017;16:138.
Cherney DZ, Perkins BA, Soleymanlou N, et al. Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation. 2014;129:587–97.
Wheeler DC, Jongs N, Stefansson BV, et al. Safety and efficacy of dapagliflozin in patients with focal segmental glomerulosclerosis: a prespecified analysis of the dapagliflozin and prevention of adverse outcomes in chronic kidney disease (DAPA-CKD) trial. Nephrol Dial Transplant. 2022;37:1647–56.
Sternlicht HK, Bakris GL. Reductions in albuminuria with SGLT2 inhibitors: a marker for improved renal outcomes in patients without diabetes? Lancet Diabetes Endocrinol. 2020;8:553–5.
Kalay Z, Sahin OE, Copur S, et al. SGLT-2 inhibitors in nephrotic-range proteinuria: emerging clinical evidence. Clin Kidney J. 2022;16:52–60.
Cherney DZI, Dekkers CCJ, Barbour SJ, et al. Effects of the SGLT2 inhibitor dapagliflozin on proteinuria in non-diabetic patients with chronic kidney disease (DIAMOND): a randomised, double-blind, crossover trial. Lancet Diabetes Endocrinol. 2020;8:582–93.
Sano M, Takei M, Shiraishi Y, Suzuki Y. Increased hematocrit during sodium-glucose cotransporter 2 inhibitor therapy indicates recovery of tubulointerstitial function in diabetic kidneys. J Clin Med Res. 2016;8:844–7.
Maruyama T, Takashima H, Oguma H, et al. Canagliflozin improves erythropoiesis in diabetes patients with anemia of chronic kidney disease. Diabetes Technol Ther. 2019;21:713–20.
Ghanim H, Abuaysheh S, Hejna J, et al. Dapagliflozin suppresses hepcidin and Iicreases erythropoiesis. J Clin Endocrinol Metab. 2020;105:dgaa057.
Heerspink HJ, de Zeeuw D, Wie L, Leslie B, List J. Dapagliflozin a glucose-regulating drug with diuretic properties in subjects with Type 2 diabetes. Diabetes Obes Metab. 2013;15:853–62.
Inzucchi SE, Zinman B, Fitchett D, et al. How does empagliflozin reduce cardiovascular mortality? Insights from a mediation analysis of the EMPA-REG OUTCOME Trial. Diabetes Care. 2018;41:356–63.
Thiele K, Rau M, Hartmann NK, et al. Effects of empagliflozin on erythropoiesis in patients with Type 2 diabetes: Data from a randomized, placebo-controlled study. Diabetes Obes Metab. 2021;23:2814–8.
Bays HE, Weinstein R, Law G, Canovatchel W. Canagliflozin: effects in overweight and obese subjects without diabetes mellitus. Obesity (Silver Spring). 2014;22:1042–9.
Bonora BM, Avogaro A, Fadini GP. Extraglycemic effects of SGLT2 inhibitors: a review of the evidence. Diabetes Metab Syndr Obes. 2020;13:161–74.
Verma S. Are the cardiorenal benefits of SGLT2 inhibitors due to inhibition of the sympathetic nervous system? JACC Basic Transl Sci. 2020;5:180–2.
O’Neill J, Fasching A, Pihl L, et al. Acute SGLT inhibition normalizes O2 tension in the renal cortex but causes hypoxia in the renal medulla in anaesthetized control and diabetic rats. Am J Physiol Renal Physiol. 2015;309:F227–34.
Docherty KF, Curtain JP, Anand IS, et al. Effect of dapagliflozin on anaemia in DAPA-HF. Eur J Heart Fail. 2021;23:617–28.
Ferreira JP, Anker SD, Butler J, et al. Impact of anaemia and the effect of empagliflozin in heart failure with reduced ejection fraction: findings from EMPEROR-Reduced. Eur J Heart Fail. 2022;24:708–15.
Li J, Woodward M, Perkovic V, et al. Mediators of the effects of canagliflozin on heart failure in patients with Type 2 diabetes. JACC Heart Fail. 2020;8:57–66.
Hamilton SJ, Watts GF. Endothelial dysfunction in diabetes: pathogenesis, significance, and treatment. Rev Diabet Stud. 2013;10:133–56.
Chilton R, Tikkanen I, Cannon CP, et al. Effects of empagliflozin on blood pressure and markers of arterial stiffness and vascular resistance in patients with type 2 diabetes. Diabetes Obes Metab. 2015;17:1180–93.
Li H, Shin SE, Seo MS, et al. The anti-diabetic drug dapagliflozin induces vasodilation via activation of PKG and Kv channels. Life Sci. 2018;197:46–55.
Cooper S, Teoh H, Campeau MA, Verma S, Leask RL. Empagliflozin restores the integrity of the endothelial glycocalyx in vitro. Mol Cell Biochem. 2019;459:121–30.
Shigiyama F, Kumashiro N, Miyagi M, et al. Effectiveness of dapagliflozin on vascular endothelial function and glycemic control in patients with early-stage Type 2 diabetes mellitus: DEFENCE study. Cardiovasc Diabetol. 2017;16:84.
Ferrannini E, Mark M, Mayoux E. CV protection in the EMPA-REG OUTCOME Trial: A “Thrifty Substrate” hypothesis. Diabetes Care. 2016;39:1108–14.
Verma S, Mazer CD, Yan AT, et al. Effect of empagliflozin on left ventricular mass in patients with Type 2 diabetes mellitus and coronary artery disease. Circulation. 2019;140:1693–702.
Dhingra NK, Mistry N, Puar P, et al. SGLT2 inhibitors and cardiac remodelling: a systematic review and meta-analysis of randomized cardiac magnetic resonance imaging trials. ESC Heart Fail. 2021;8:4693–700.
García-Ropero Á, Santos-Gallego CG, Badimon JJ. The anti-inflammatory effects of SGLT inhibitors. Aging (Albany NY). 2019;11:5866–7.
Muiesan ML, Agabiti-Rosei C, Paini A, Salvetti M. Uric acid and cardiovascular Disease: an update. Eur Cardiol. 2016;11:54–9.
Viazzi F, Parodi D, Leoncini G, et al. Serum uric acid and target organ damage in primary hypertension. Hypertension. 2005;45:991–6.
Xaplanteris P, Vlachopoulos C, Vyssoulis G, et al. Uric acid levels, left ventricular mass and geometry in newly diagnosed, never treated hypertension. J Hum Hypertens. 2011;25:340–2.
Davies MJ, Trujillo A, Vijapurkar U, Damaraju CV, Meininger G. Effect of canagliflozin on serum uric acid in patients with Type 2 diabetes mellitus. Diabetes Obes Metab. 2015;17:426–9.
Scholtes RA, van Raalte DH, Correa-Rotter R, et al. The effects of dapagliflozin on cardio-renal risk factors in patients with Type 2 diabetes with or without renin-angiotensin system inhibitor treatment: a post hoc analysis. Diabetes Obes Metab. 2020;22:549–56.
Verma S, Ji Q, Bhatt DL, et al. Association between uric acid levels and cardio-renal outcomes and death in patients with Type 2 diabetes: A subanalysis of EMPA-REG OUTCOME. Diabetes Obes Metab. 2020;22:1207–14.
McDowell K, Welsh P, Docherty KF, et al. Dapagliflozin reduces uric acid concentration, an independent predictor of adverse outcomes in DAPA-HF. Eur J Heart Fail. 2022;24:1066–76.
Sacks HS, Fain JN. Human epicardial adipose tissue: a review. Am Heart J. 2007;153:907–17.
Shimabukuro M, Hirata Y, Tabata M, et al. Epicardial adipose tissue volume and adipocytokine imbalance are strongly linked to human coronary atherosclerosis. Arterioscler Thromb Vasc Biol. 2013;33:1077–84.
Hatem SN, Sanders P. Epicardial adipose tissue and atrial fibrillation. Cardiovasc Res. 2014;102:205–13.
Yagi S, Hirata Y, Ise T, et al. Canagliflozin reduces epicardial fat in patients with Type 2 diabetes mellitus. Diabetol Metab Syndr. 2017;9:78.
Sato T, Aizawa Y, Yuasa S, et al. The effect of dapagliflozin treatment on epicardial adipose tissue volume. Cardiovasc Diabetol. 2018;17:6.
Dekkers CCJ, Sjöström CD, Greasley PJ, et al. Effects of the sodium-glucose co-transporter-2 inhibitor dapagliflozin on estimated plasma volume in patients with Type 2 diabetes. Diabetes Obes Metab. 2019;21:2667–73.
Verma S, Garg A, Yan AT, et al. Effect of empagliflozin on left ventricular mass and diastolic function in individuals with diabetes: an important clue to the EMPA-REG OUTCOME Trial? Diabetes Care. 2016;39:e212–3.
Hallow KM, Helmlinger G, Greasley PJ, McMurray JJV, Boulton DW. Why do SGLT2 inhibitors reduce heart failure hospitalization? A differential volume regulation hypothesis. Diabetes Obes Metab. 2018;20:479–87.
Zanchi A, Burnier M, Muller ME, et al. Acute and chronic effects of SGLT2 inhibitor empagliflozin on renal oxygenation and blood pressure control in nondiabetic normotensive subjects: a randomized, placebo-controlled trial. J Am Heart Assoc. 2020;9: e016173.
Omar M, Jensen J, Burkhoff D, et al. Effect of empagliflozin on blood volume redistribution in patients with chronic heart failure and reduced ejection fraction: an analysis from the Empire HF randomized clinical trial. Circ Heart Fail. 2022;15: e009156.
Nassif ME, Qintar M, Windsor SL, et al. Empagliflozin effects on pulmonary artery pressure in patients with heart failure: results from the EMBRACE-HF trial. Circulation. 2021;143:1673–86.
Petrie MC, Verma S, Docherty KF, et al. Effect of dapagliflozin on worsening heart failure and cardiovascular death in patients with heart failure with and without diabetes. JAMA. 2020;323:1353–68.
Karg MV, Bosch A, Kannenkeril D, et al. SGLT-2-inhibition with dapagliflozin reduces tissue sodium content: a randomised controlled trial. Cardiovasc Diabetol. 2018;17:5.
Packer M. Activation and inhibition of sodium-hydrogen exchanger is a mechanism that links the pathophysiology and treatment of diabetes mellitus with that of heart failure. Circulation. 2017;136:1548–59.
Packer M. Reconceptualization of the molecular mechanism by which sodium-glucose cotransporter 2 inhibitors reduce the risk of heart failure events. Circulation. 2019;140:443–5.
Hallow KM, Greasley PJ, Helmlinger G, et al. Evaluation of renal and cardiovascular protection mechanisms of SGLT2 inhibitors: model-based analysis of clinical data. Am J Physiol Renal Physiol. 2018;315:F1295–306.
Bell RM, Yellon DM. SGLT2 inhibitors: hypotheses on the mechanism of cardiovascular protection. Lancet Diabetes Endocrinol. 2018;6:435–7.
Avkiran M. Rational basis for use of sodium-hydrogen exchange inhibitors in myocardial ischemia. Am J Cardiol. 1999;83:10G–17G; discussion 17G–18G.
Baartscheer A, Schumacher CA, Wust RC, et al. Empagliflozin decreases myocardial cytoplasmic Na(+) through inhibition of the cardiac Na(+)/H(+) exchanger in rats and rabbits. Diabetologia. 2017;60:568–73.
Uthman L, Baartscheer A, Bleijlevens B, et al. Class effects of SGLT2 inhibitors in mouse cardiomyocytes and hearts: inhibition of Na(+)/H(+) exchanger, lowering of cytosolic Na(+) and vasodilation. Diabetologia. 2018;61:722–6.
Chung YJ, Park KC, Tokar S, et al. Off-target effects of SGLT2 blockers: empagliflozin does not inhibit Na+/H+ exchanger-1 or lower [Na+]i in the heart. Cardiovasc Res. 2021;117:2794–806.
Lehrke M, Marx N. Diabetes mellitus and heart failure. Am J Cardiol. 2017;120:S37–47.
Wilson AJ, Gill EK, Abudalo RA, et al. Reactive oxygen species signalling in the diabetic heart: emerging prospect for therapeutic targeting. Heart. 2018;104:293–9.
Lee TM, Chang NC, Lin SZ. Dapagliflozin, a selective SGLT2 inhibitor, attenuated cardiac fibrosis by regulating the macrophage polarization via STAT3 signaling in infarcted rat hearts. Free Radic Biol Med. 2017;104:298–310.
Quagliariello V, De Laurentiis M, Rea D, et al. The SGLT-2 inhibitor empagliflozin improves myocardial strain, reduces cardiac fibrosis and pro-inflammatory cytokines in non-diabetic mice treated with doxorubicin. Cardiovasc Diabetol. 2021;20:150.
Kang S, Verma S, Hassanabad AF, et al. Direct effects of empagliflozin on extracellular matrix remodelling in human cardiac myofibroblasts: novel translational clues to explain EMPA-REG OUTCOME results. Can J Cardiol. 2020;36:543–53.
Lopaschuk GD, Ussher JR, Folmes CD, Jaswal JS, Stanley WC. Myocardial fatty acid metabolism in health and disease. Physiol Rev. 2010;90:207–58.
Janardhan A, Chen J, Crawford PA. Altered systemic ketone body metabolism in advanced heart failure. Tex Heart Inst J. 2011;38:533–8.
Daniele G, Xiong J, Solis-Herrera C, et al. Dapagliflozin enhances fat oxidation and ketone production in patients with Type 2 diabetes. Diabetes Care. 2016;39:2036–41.
Lopaschuk GD, Verma S. Empagliflozin’s fuel hypothesis: not so soon. Cell Metab. 2016;24:200–2.
Tahara A, Kurosaki E, Yokono M, et al. Effects of sodium-glucose cotransporter 2 selective inhibitor ipragliflozin on hyperglycaemia, oxidative stress, inflammation and liver injury in streptozotocin-induced Type 1 diabetic rats. J Pharm Pharmacol. 2014;66:975–87.
Mudaliar S, Alloju S, Henry RR. Can a shift in fuel energetics explain the beneficial cardiorenal outcomes in the EMPA-REG outcome study? A unifying hypothesis. Diabetes Care. 2016;39:1115–22.
Santos-Gallego CG, Requena-Ibanez JA, San Antonio R, et al. Empagliflozin ameliorates adverse left ventricular remodeling in nondiabetic heart failure by enhancing myocardial energetics. J Am Coll Cardiol. 2019;73:1931–44.
Dąbek A, Wojtala M, Pirola L, Balcerczyk A. Modulation of cellular biochemistry, epigenetics and metabolomics by ketone bodies. Implications of the ketogenic diet in the physiology of the organism and pathological states. Nutrients. 2020;12:788.
Chakraborty S, Galla S, Cheng X, et al. Salt-responsive metabolite, β-hydroxybutyrate, attenuates hypertension. Cell Rep. 2018;25:677–89.
Parzych KR, Klionsky DJ. An overview of autophagy: morphology, mechanism, and regulation. Antioxid Redox Signal. 2014;20:460–73.
Avogaro A, Fadini GP, Del Prato S. Reinterpreting cardiorenal protection of renal sodium-glucose cotransporter 2 inhibitors via cellular life history programming. Diabetes Care. 2020;43:501–7.
Packer M. SGLT2 inhibitors produce cardiorenal benefits by promoting adaptive cellular reprogramming to induce a state of fasting mimicry: A paradigm shift in understanding their mechanism of action. Diabetes Care. 2020;43:508–11.
Zannad F, Ferreira JP, Butler J, et al. Effect of empagliflozin on circulating proteomics in heart failure: mechanistic insights into the EMPEROR programme. Eur Heart J. 2022;43:4991–5002.
Geraldes P, King GL. Activation of protein kinase C isoforms and its impact on diabetic complications. Circ Res. 2010;106:1319–31.
Harris AL. Hypoxia–a key regulatory factor in tumour growth. Nat Rev Cancer. 2002;2:38–47.
Zhang Y, Ling Y, Yang L, et al. Liraglutide relieves myocardial damage by promoting autophagy via AMPK-mTOR signaling pathway in zucker diabetic fatty rat. Mol Cell Endocrinol. 2017;448:98–107.
Zhou Y, Wang H, Man F, et al. Sitagliptin protects cardiac function by reducing nitroxidative stress and promoting autophagy in zucker diabetic fatty (ZDF) rats. Cardiovasc Drugs Ther. 2018;32:541–52.
Kato MF, Shibata R, Obata K, et al. Pioglitazone attenuates cardiac hypertrophy in rats with salt-sensitive hypertension: role of activation of AMP-activated protein kinase and inhibition of Akt. J Hypertens. 2008;26:1669–76.
Juszczak F, Caron N, Mathew AV, Declèves AE. Critical role for AMPK in metabolic disease-induced chronic kidney disease. Int J Mol Sci. 2020;21:7994.
Rahadian A, Fukuda D, Salim HM, et al. Canagliflozin prevents diabetes-induced vascular dysfunction in ApoE-deficient mice. J Atheroscler Thromb. 2020;27:1141–51.
Hess DA, Terenzi DC, Trac JZ, et al. SGLT2 inhibition with empagliflozin increases circulating provascular progenitor cells in people with Type 2 diabetes mellitus. Cell Metab. 2019;30:609–13.
Albiero M, Tedesco S, Amendolagine FI, et al. Inhibition of SGLT2 rescues bone marrow cell traffic for vascular repair: role of glucose control and ketogenesis. Diabetes. 2021;70:1767–79.
Terenzi DC, Trac JZ, Teoh H, et al. Vascular regenerative cell exhaustion in diabetes: translational opportunities to mitigate cardiometabolic risk. Trends Mol Med. 2019;25:640–55.
Hess DA, Terenzi DC, Verma S. Heal thyself: SGLT2 inhibition limits regenerative cell exhaustion and heals damaged vessels. Diabetes. 2021;70:1620–2.
Thirunavukarasu S, Jex N, Chowdhary A, et al. Empagliflozin treatment is associated with improvements in cardiac energetics and function and reductions in myocardial cellular volume in patients with Type 2 diabetes. Diabetes. 2021;70:2810–22.
D’Elia JA, Segal AR, Bayliss GP, Weinrauch LA. Sodium-glucose cotransporter-2 inhibition and acidosis in patients with Type 2 diabetes: a review of US FDA data and possible conclusions. Int J Nephrol Renovasc Dis. 2017;10:153–8.
Diaz-Ramos A, Eilbert W, Marquez D. Euglycemic diabetic ketoacidosis associated with sodium-glucose cotransporter-2 inhibitor use: a case report and review of the literature. Int J Emerg Med. 2019;12:27.
Zhang L, Tamilia M. Euglycemic diabetic ketoacidosis associated with the use of a sodium-glucose cotransporter-2 inhibitor. CMAJ. 2018;190:E766–8.
Wang KM, Isom RT. SGLT2 Inhibitor-Induced Euglycemic Diabetic Ketoacidosis: A Case Report. Kidney Medicine. 2020;2:218–21.
Nasa P, Chaudhary S, Shrivastava PK, Singh A. Euglycemic diabetic ketoacidosis: A missed diagnosis. World J Diabetes. 2021;12:514–23.
Ata F, Yousaf Z, Khan AA, et al. SGLT-2 inhibitors associated euglycemic and hyperglycemic DKA in a multicentric cohort. Sci Rep. 2021;11:10293.
Hsia DS, Grove O, Cefalu WT. An update on sodium-glucose co-transporter-2 inhibitors for the treatment of diabetes mellitus. Curr Opin Endocrinol Diabetes Obes. 2017;24:73–9.
National Institute for Health and Care Excellence (NICE). Type 2 diabetes in adults: management. Published Dec 2015; Updated June 2022. Available at: https://www.nice.org.uk/guidance/ng28.
Neuen BL, Cherney DZ, Jardine MJ, Perkovic V. Sodium-glucose cotransporter inhibitors in Type 2 diabetes: thinking beyond glucose lowering. CMAJ. 2019;191:E1128–35.
Medical Writing and Editorial Assistance
The authors would like to acknowledge Parita Sheth, inScience Communications, London, UK, for assistance in the writing and editing of this manuscript and preparation of figures. This support was funded by AstraZeneca.
Funding
The publication of this article was funded by AstraZeneca, including funding for the Journal’s Rapid Service and Open Access Fees.
Author information
Authors and Affiliations
Contributions
Subodh Verma, Sunder Mudaliar and Peter J. Greasley contributed to identifying the data to be included in this manuscript, and in the critical review, approval and submission of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Subodh Verma holds a Tier 1 Canada Research Chair in Cardiovascular Surgery; and reports receiving research grants and/or speaking honoraria from Amarin, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly, EOCI Pharmacomm Ltd, HLS Therapeutics, Janssen, Novartis, Novo Nordisk, Pfizer, PhaseBio, Sanofi, Sun Pharmaceuticals, and the Toronto Knowledge Translation Working Group. He is the President of the Canadian Medical and Surgical Knowledge Translation Research Group, a federally incorporated not-for-profit physician organization. Sunder Mudaliar has received speaker fees from AstraZeneca, has acted as a consultant for Bayer and has received research support from NIH/National Institute of Diabetes and Digestive and Kidney Diseases. Peter J. Greasley is an employee and shareholder of AstraZeneca.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Verma, S., Mudaliar, S. & Greasley, P.J. Potential Underlying Mechanisms Explaining the Cardiorenal Benefits of Sodium–Glucose Cotransporter 2 Inhibitors. Adv Ther 41, 92–112 (2024). https://doi.org/10.1007/s12325-023-02652-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02652-5