Abstract
Introduction
Differences in class or molecule-specific effects between renin–angiotensin–aldosterone system (RAAS) inhibitors have not been conclusively demonstrated. This study used South African data to assess clinical and cost outcomes of antihypertensive therapy with the three most common RAAS inhibitors: perindopril, losartan and enalapril.
Methods
Using a large, South African private health insurance claims database, we identified patients with a hypertension diagnosis in January 2015 receiving standard doses of perindopril, enalapril or losartan, alone or in combination with other agents. From claims over the subsequent 5 years, we calculated the risk-adjusted rate of the composite primary outcome of myocardial infarction, ischaemic heart disease, heart failure or stroke; rate of all-cause mortality; and costs per life per month (PLPM), with adjustments based on demographic characteristics, healthcare plan and comorbidity.
Results
Overall, 32,857 individuals received perindopril, 16,693 losartan and 13,939 enalapril. Perindopril-based regimens were associated with a significantly lower primary outcome rate (205 per 1000 patients over 5 years) versus losartan (221; P < 0.0001) or enalapril (223; P < 0.0001). The risk-adjusted all-cause mortality rate was lower with perindopril than enalapril (100 vs. 139 deaths per 1000 patients over 5 years; P = 0.007), but not losartan (100 vs. 94; P = 0.650). Mean (95% confidence interval) overall risk-adjusted cost PLPM was Rands (ZAR) 1342 (87–8973) for perindopril, ZAR 1466 (104–9365) for losartan (P = 0.0044) and ZAR 1540 (77–10,546) for enalapril (P = 0.0003).
Conclusion
In South African individuals with private health insurance, a perindopril-based antihypertensive regimen provided better clinical and cost outcomes compared with other regimens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Hypertension prevalence in sub-Saharan Africa is among the highest in the world and is commonly treated with inhibitors of the renin–angiotensin–aldosterone system (RAAS); however, whether cardiovascular benefit is derived from class or molecule-specific effects remains unknown and is confounded by patient variability. |
This retrospective observational study used a private medical insurance claims database to evaluate the clinical and cost benefits of the most commonly prescribed RAAS inhibitors in patients with hypertension in South Africa. |
What was learned from the study? |
Perindopril-based regimens were associated with a significantly lower risk-adjusted cardiovascular event rate (at least one claim for myocardial infarction, ischaemic heart disease, heart failure or stroke) over 5 years compared with losartan- or enalapril-based regimens. |
The overall mean risk-adjusted cost per life per month was also lower for perindopril than the other two agents, indicating that perindopril-based regimens offer improved clinical and socioeconomic outcomes. |
Further studies are warranted to confirm these results in a broader South African population, which may have significant implications for the choice of therapy in patients with hypertension. |
Introduction
Hypertension is estimated to cause 7.7–10.4 million deaths per year worldwide [1]. Although the age-standardised prevalence of hypertension does not appear to be increasing worldwide, the absolute number of affected adults doubled between 1990 and 2019 as the world’s population increased [2]. Of note, the burden of hypertension is higher in low- and middle-income countries, where 82% (i.e. more than 1 billion people) of the global hypertensive population live [2].
The prevalence of hypertension in sub-Saharan Africa is amongst the highest in the world [2]. In South Africa, approximately 45% of men and 48% of women had hypertension in 2016, an increase from 27 and 31%, respectively, in 1998 [3]. Moreover, estimates indicate that only 22% of men and 29% of women with hypertension in sub-Saharan Africa are receiving treatment, with blood pressure (BP) controlled to < 140/90 mmHg in 9% and 13%, respectively [2]. To reverse the low rate of BP control in Africa, the Pan-African Society of Cardiology developed a roadmap to achieve BP control in 25% of hypertensive individuals by 2025 [4]. In addition to supporting efforts in prevention, screening and diagnosis of hypertension, this roadmap emphasises the importance of ensuring that patients with hypertension are treated effectively.
The International Society of Hypertension guidelines recommend a single-pill combination therapy of an angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor blocker (ARB) plus a calcium channel blocker (CCB) for most patients as first-line treatment. Drug monotherapy is indicated for low-risk patients with grade one hypertension, or for very elderly (≥ 80 years) or frail patients [5]. These recommendations are based on high-quality evidence that these drug classes improve cardiovascular outcomes in patients with hypertension [6].
Numerous ACE inhibitors and ARBs are now available for prescription, but there is ongoing debate about whether cardiovascular benefit is a class effect or a molecule-specific effect [7, 8]. Individual ACE inhibitors have different clinical properties, suggesting the possibility of molecule-specific benefits beyond BP lowering [9]. A meta-analysis performed in 2009 suggested that perindopril may be associated with superior cardiovascular outcomes compared with other ACE inhibitors in hypertensive patients [10].
The question of whether benefit is a class effect or molecule-specific is confounded by differences between patients included in randomised controlled trials (RCTs) and patients seen in real-world practice [11]. In addition, ACE inhibitors and ARBs are sometimes grouped together in analyses because they both inhibit the renin–angiotensin–aldosterone system (RAAS), when, in fact, ACE inhibitors prevent the formation of angiotensin with a downstream effect on tissue bradykinin levels, while ARBs block the interaction of angiotensin I with its tissue-specific angiotensin 2 receptor. As a result, these classes may not have comparable clinical outcomes [6, 12, 13]. Further, most patients often require more than one antihypertensive agent to control BP [14], making it difficult to ascribe benefit to a single agent.
Choice of antihypertensive treatment is also impacted by the patient’s comorbidities and by funding constraints. In South Africa, access to fully reimbursed medicines is often based on price rather than efficacy. Only about 15% of the South African population have access to insurance-based healthcare and thus access to more expensive medicines [15]; however, the antihypertensive medications analysed in the current study were all also available via the government-funded healthcare system.
The aim of this study was to establish if there are clinical and cost benefits associated with the ACE inhibitors and ARBs that are most commonly used in South African patients, using data from a large medical insurance claims database.
Methods
Study Design
This was a retrospective observational study of claims data from a database of health claims from a large private sector funder in South Africa, managed by Quantium. Anonymised patient-level claims from a 5-year period (January 2015 to December 2019) were analysed to measure clinical and cost outcomes according to the type of antihypertensive regimen received. A 5-year study period was selected to allow for observation of a sufficient number of long-term complication events of hypertension.
All work was carried out in accordance with the Helsinki Declaration of 1964, and its later amendments. Ethics approval was obtained by Professor Ntobeko A. B. Ntusi from the University of Cape Town Faculty of Health Sciences Human Research Ethics Committee for the use of the dataset. Informed consent was not required for this study.
Data Source
We used a private medical insurance claims database, which contains claims for approximately 3.5 million people insured with a large private medical insurance company in South Africa (estimated to include 39% of the total privately insured population in South Africa) [15]. The claims in the database cover the following healthcare services: hospital visits/admissions, drug prescriptions, medical devices, general practitioner (GP) and specialist visits, surgical procedures, radiology and pathology services, and care from allied health professionals. Patient data were anonymised, and each insured patient was assigned a single unique identifier that enabled individualised tracking of all health claims while maintaining privacy.
The database uses International Classification of Disease 10th edition (ICD-10) codes to identify specific reasons for healthcare claims. Since a disease state may be described by more than one ICD-10 code, the database also applies a unique funder-specific Disease Episode Grouper (DEG) field to each claim to apply a single disease descriptor to a group of relevant ICD-10 codes (see Supplementary Table S1 in the electronic supplementary material for details). DEG and ICD-10 codes were linked to provider codes, identifying whether the provider was a hospital, GP, specialist, or other type of healthcare professional. The World Health Organization Anatomical Therapeutic Chemical (ATC) codes were used for classifying medications according to the organ system they affect and their therapeutic, pharmacological and chemical properties [16]. A mortality indicator was used to identify patients who died during the study period.
Inclusion Criteria
The database was searched to identify patients who were receiving standard doses of perindopril, losartan or enalapril, alone or in combination with other agents, using ATC codes (see Supplementary Table S2 in the electronic supplementary materials) for the treatment of hypertension (based on the ICD-10 code I10) in January 2015 (the index date). These drugs were included in the analysis because they are the most commonly used RAAS inhibitors that are available within the private healthcare system in South Africa (see Supplementary Table S3 in the electronic supplementary materials). This makes them appropriate comparators and provides the rationale for investigating possible clinical differences between them under circumstances of real-world use. Claims in the preceding year (January to December 2014) were assessed, and adherence expressed as the number of prescriptions filled compared with the number expected (medicine possession ratio). Only patients with ≥ 80% adherence to perindopril, losartan or enalapril were included to minimise the number of poorly adherent patients in the analysis dataset. This approach was taken to ensure that any effects observed could reasonably be considered to be due to an effect of the patients’ drug treatment. Patients were grouped into the appropriate cohort (perindopril, losartan or enalapril). Claims over the next 5 years (January 2015 to December 2019) were assessed and analysed. Those who left the medical insurance scheme for reasons other than death within the 5-year period after the index date were excluded from the study. Patients were excluded from the analysis if they had < 80% exposure to the relevant drug-based regimen during the 5-year period of analysis based on < 80% of prescriptions filled (i.e. as a result of drug switching). Sensitivity analysis was carried out on all patients with no exclusions. Patients who died during the study period were included in the analyses, and their drug exposure adjusted accordingly.
Data Classification
Patients were assigned to three cohorts according to the antihypertensive agent they were receiving at the index date (January 2015) (i.e. perindopril, losartan or enalapril). Within each treatment cohort, patient baseline characteristics at the index date were extracted, including age, sex and health plan type. Comorbidities were identified using claims for DEG and ICD-10 codes (see Supplementary Table S1 in the electronic supplementary material) from the pre-index year (i.e. January 2014 to December 2014). All claims associated with hypertension and related conditions, specifically aneurysm (± dissection or rupture), diabetes (type 1 or 2), ischaemic or haemorrhagic stroke, ischaemic heart disease (IHD), heart failure (HF), myocardial infarction (MI), renal failure, hyperlipidaemia, vascular dementia and arrhythmias over the 5-year post-index period were also collected using DEG and ICD-10 codes for specific outcomes (see Supplementary Table S1 in the electronic supplementary material), and deaths were identified using the database mortality indicator.
Outcomes
The primary outcome was the composite of the risk-adjusted event rate of having at least one claim for MI, IHD, HF or stroke within the 5-year study period. Secondary clinical outcomes were risk-adjusted all-cause mortality rate and risk-adjusted rate of hospitalisation for any of the composite outcome events, both expressed as the rate per 1000 people over 5 years. An additional secondary outcome was the risk-adjusted rate of the first occurrence of the composite outcome over 5 years expressed as the percentage of patients in each cohort; first events were identified as those occurring in patients who had not had any claim for the same complication in the pre-index year (i.e. during 2014).
Outcomes were risk-adjusted to account for multiple cofounders following the cell-based approach described by Ellis et al [17]. Briefly, each patient was assigned to 1 of 351 risk cells based on their age, sex, health plan type (high, intermediate, low, hospital-only or other coverage), existing comorbidities and whether or not these comorbidities were a direct outcome of hypertension. The risk index for each cell was calculated by dividing the average healthcare claim costs for all patients in the risk cell by the average cost of all patients in the cohort. The overall risk index for each treatment cohort was calculated as the average risk index for all cells in that cohort. A higher risk index indicates that the cohort had a greater underlying risk profile and higher likelihood of worse clinical outcomes and higher costs.
Cost outcomes were defined as the total cost of claims paid [in South African Rands (ZAR) per life per month (PLPM)] that were linked to hypertension or a related condition as a comorbidity (aneurysm, diabetes, stroke, IHD, HF, MI, renal failure, hyperlipidaemia, vascular dementia and arrhythmias). Costs were disaggregated into hospital, GP, specialist and medication, based on identifiers in the claims data. All costs were calculated as a weighted average of the claims paid during the 5-year study period divided by exposure months (i.e. 60 months or less for a patient who died during the study) for each individual patient and averaged across all patients. Costs were adjusted by + 2.1% for inflation each year, which was the medical inflation rate in South Africa over this period, and standardised to 2019 ZAR. The average rate of exchange for the ZAR between 2015 and 2019 (the study period) was ZAR 13.70192 per $US 1 [18].
Statistical Analysis
Standard descriptive statistics were used to describe outcomes. Continuous variables were summarised as means and 95% confidence intervals (CIs), and categorical variables as frequency per 1000 patients and percentage of patients per category over the 5-year study period. Two-way statistical comparisons between the perindopril group and losartan or enalapril groups were conducted using the stratified non-parametric bootstrap method for continuous variables [19], and a Chi-squared test or the z-test equal proportions were used for categorical variables. All-cause mortality and event rates were analysed using the Kaplan–Meier estimator to provide a time–treatment analysis. Cost data were analysed using the non-parametric bootstrap method, which is well established as a primary statistical analysis when making inferences about arithmetic means for moderately sized samples of highly skewed data, such as real-world costs [19]. The bootstrap method involves taking random samples of data (bootstrap samples), with each replaced back into the dataset before a subsequent sample is taken, and uses these samples to model the overall dataset. For this test, we chose 10,000 bootstrap samples with replacement for each of the groups separately, and then compared the difference in the means of the bootstrap sample groups with the observed difference in the means of the groups in the actual dataset.
Sensitivity analyses for selected clinical and cost outcomes (primary composite event rate and proportion of patients with such an event, and total cost of claims) were conducted with no exclusion criteria applied (i.e. including all patients taking perindopril, losartan or enalapril).
All analyses were performed using R version 1.1.456 and Python version 2.7.
Results
Study Population
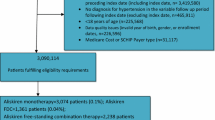
We identified 108,820 patients who were taking one of the designated antihypertensive agents in January 2015, of whom 63,489 (58.3%) met the study eligibility criteria after exclusion of patients who had < 80% adherence prior to entry and those who lived for 5 years but did not have 5 years of continuous health plan enrolment after the index date (Fig. 1). The mean [standard deviation (SD)] age of patients was 62.6 (12.6) years, and 49% were female (Table 1). Patients in the perindopril treatment cohort tended to be younger (mean age 61.8 years) than those receiving enalapril (63.8 years) or losartan (63.2 years) and were less likely to be female (45.3% vs. 51.9% and 53.8%, respectively; P < 0.001), but had a higher incidence of IHD as a comorbidity (14.5% vs. 9.9% and 12.5%, respectively; P < 0.001). A higher proportion of patients in the perindopril group (48.4%) had the highest level of health insurance coverage compared with the enalapril group (32.2%) or losartan group (42.9%; P < 0.001). Risk index values were 1.03 for the perindopril cohort, 1.01 for losartan and 0.94 for enalapril (P < 0.001). The majority of patients in each of the cohorts was receiving additional antihypertensive drug classes; overall, similar proportions of patients in each group were receiving diuretics, CCBs and beta-blockers as the only adjunctive agent and as combination adjunctives (see Supplementary Table S6 in the electronic supplementary materials).
Cardiovascular Events
The risk-adjusted rate of at least one claim for MI, IHD, HF or stroke within the 5-year study period (primary outcome) was 205 events per 1000 patients with perindopril compared with 221 events per 1000 patients with losartan (P < 0.001) and 223 events per 1000 patients with enalapril (P < 0.001). A breakdown of each of the specific cardiovascular events such as MI, IHD, HF or stroke has been provided (Table 2). Overall, 15.2% of patients receiving perindopril had a first primary outcome event during the study period compared with 16.7% of those receiving losartan (P < 0.001) and 17.2% receiving enalapril (P < 0.001). The risk-adjusted Kaplan–Meier curve also demonstrated a difference in the rate of first composite outcome complications over time (log-rank P < 0.005; Fig. 2a).
All-Cause Mortality
The risk-adjusted all-cause mortality rate over 5 years was 100 deaths per 1000 patients with perindopril compared with 139 deaths per 1000 patients with enalapril (P = 0.007) and 94 deaths per 1000 patients with losartan (P = 0.650) (Fig. 2b). A combined all-cause mortality and cardiovascular event rate was 305 events per 1000 patients with perindopril and 362 events per 1000 patients with enalapril (P < 0.001) and 315 events per 1000 patients with losartan (P = 0.034). Non-risk-adjusted outcomes are shown in Supplementary Table S5 in the electronic supplementary materials.
Healthcare Resource Utilisation
Over the 5-year study, the risk-adjusted mean (95% CI) health claims paid PLPM for hypertension and related conditions were ZAR 1341 (87–8973) in the perindopril group compared with ZAR 1465 (104–9365; P = 0.0044) for losartan and ZAR 1540 (77–10,546; P < 0.001) for enalapril (Fig. 3 and Table 3). The mean cost of claims in the perindopril cohort was therefore 8.5% lower than in the losartan cohort and 12.9% lower than in the enalapril cohort.
Risk-adjusted cost in South African Rands (ZAR) per life per month (PLPM) in each treatment cohort over 5 years. The box defines the lower (Q1) and upper (Q3) quartiles, where 50% of the data are found. The horizontal line that bisects the box is the median. The mean is indicated by the black dot. The vertical lines above and below the box define the range. The average rate of exchange for the ZAR between 2015 and 2019 (the study period) was ZAR 13.70192 per $US 1 [18]
Hospital (inpatient) costs constituted the greatest proportion of the healthcare claims in these cohorts (Table 3). Mean (95% CI) hospital costs were highest in the group receiving enalapril [ZAR 911 (0–8810)], intermediate in the group receiving losartan [ZAR 799 (0–7586)] and lowest in the perindopril group [ZAR 748 (0–7452)0); the difference between perindopril and enalapril was statistically significant (P < 0.001), but the difference between perindopril and losartan was not (P = 0.113). The perindopril group also had lower mean claims paid for GP visits and for other services (radiology, pathology and allied healthcare services) compared with enalapril (P < 0.001 and P = 0.015, respectively) and losartan (P < 0.001 and P = 0.001, respectively), and lower pharmacotherapy costs compared with losartan (P < 0.001), but not compared with enalapril (P = 0.096). There was no significant difference in specialist costs between the perindopril group and either the losartan or the enalapril group.
Sensitivity Analyses
The results of the sensitivity analyses, in which all patients receiving one of the designated antihypertensive agents were included (n = 108,820), were consistent with those of the primary analyses. The use of other medicines, such as beta-blockers and CCBs, were evenly distributed and no additional benefit was attributed to these (see Supplementary Table S6 in the electronic supplementary material). The risk-adjusted rate of at least one claim for MI, IDH, HF or stroke within the 5-year study period (primary outcome) and the proportion of patients with the primary outcome were significantly lower in the perindopril group than in the losartan and enalapril groups (see Supplementary Table S4 in the electronic supplementary material), and the total cost of care was significantly lower in the perindopril group than in the losartan or enalapril groups (see Supplementary Table S5 in the electronic supplementary material).
Discussion
In a real-world setting of a large patient cohort of approximately 63,500 patients with hypertension in South Africa followed over 5 years, our retrospective analysis of health insurance medical claims revealed that: (1) while patients receiving perindopril were younger, there was significantly increased cardiovascular risk in this group, based on greater frequency of pre-existing IHD, higher health insurance coverage and higher risk index values compared with patients receiving enalapril or losartan; (2) the primary outcome of the risk-adjusted rate for a claim for cardiovascular events was lower in the perindopril treatment cohort, as was the rate of first occurrence of the composite outcome; (3) perindopril-based regimens were associated with significantly better cardiovascular and cost outcomes over a 5-year period; and (4) there was a significant mortality benefit relative to enalapril but not losartan. These data have important implications for clinical practice where full reimbursement for antihypertensive therapy should be based primarily on clinical efficacy and secondarily on total cost of care. Our study suggests that perindopril use was associated with both superior efficacy and lower total cost of care in this South African private health sector cohort.
There was a significantly lower rate of all-cause mortality in the perindopril group compared with the enalapril group, but not the losartan group. The reasons for this finding are not clear since we were unable to differentiate causes of death from the available mortality data. However, the finding is directionally consistent with data from a Taiwanese medical claims analysis that reported a significantly lower rate of all-cause mortality with ramipril, perindopril, lisinopril or imidapril compared with enalapril, captopril or fosinopril [20]. In an RCT of 1502 diabetic patients with known coronary artery disease but without HF (40% of them with hypertension), over a median follow-up of 4.3 years, perindopril treatment was associated with a non-significant reduction in the primary outcome of cardiovascular death, non-fatal MI and resuscitated cardiac arrest in the diabetic population [12.6% vs. 15.5%; relative risk reduction 19% (95% CI − 7 to 38%; P = 0.13)] [21]. More recently, when comparing ACE inhibitors and ARBs, a Cochrane meta-analysis of RCTs did not detect a difference between the two drug classes with respect to overall cardiovascular outcomes [12]. However, other meta-analyses suggested that ACE inhibitors may provide better outcomes for coronary heart disease and renal failure, whereas ARBs may be associated with improved stroke outcomes [6, 22], suggesting differential clinical outcomes within and between classes of RAAS antagonists.
Data from two national surveys in 1998 and 2016 have demonstrated that there has been a rise in the prevalence of hypertension in South Africa, from 27% and 31% in men and women to 45% and 48%, respectively [3]. The cost implication of the rise in hypertension prevalence warrants determining the overall cost of therapies, rather than just a single expense such as the comparative costs of medications.
Randomised controlled trials have the benefit of providing clear evidence in support of different therapies, but they do not provide real-world evidence. The data from this study demonstrate both a health and cost benefit for the use of perindopril-based regimens in a real-world setting. Adherence is known to be higher in RCTs than in routine clinical practice [23], and is an important determinant of outcomes [24]. To mitigate the effects of adherence, patients were pre-selected based on > 80% adherence to their antihypertensive in the preceding year. As is common with real-world evidence, there are significant differences between the groups. The risk-cell approach has been used to adjust for these differences [25]. The insurance plan, which may reflect socioeconomic status and its impact on cardiovascular outcomes [26], was also included in the model.
Overall cost saving in the perindopril treatment group of 8.5% and 12.9% compared with losartan and enalapril equates to ZAR 124 and ZAR 198 per month, respectively. South Africa has the highest recorded Gini index and the average income in November 2020 for the country was ZAR 23,133 [27], indicating that these differences correspond to 0.5% and 0.9% of the average monthly salary, respectively. However, the most clinically relevant saving would be in disability-adjusted life years, for which cardiovascular disease is a rising cause in South Africa [28].
Our study has several limitations related to its design. Firstly, the data used in our study were extracted from medical claims from a single medical insurer in South Africa. Approximately 15.2% of the South African population have medical insurance [29], and patient demographics (including socioeconomic status and racial profile) and disease burden may differ between the insured and the uninsured populations [30]. Therefore, these findings may not be generalisable to the South African population treated in the public health sector, although it should be noted that all three of the drugs studied are included in the national health budget for patients cared for by the State. Also, because we analysed data from a single insurer, the data may not represent the insured population in the country in its entirety. Secondly, the data available did not allow for analysis of any potential impact of socioeconomic status on the outcomes of interest. Thirdly, this was a retrospective analysis of submitted claims, meaning that there was no randomisation or standardisation of groups, requiring statistical adjustment. In addition, the study will have all the inherent biases of such a design. Finally, the duration of hypertension was not accounted for. However, despite these limitations, this large, real-world study, which incorporated risk-adjustment to account for multiple cofounders, suggests that perindopril-based treatment for hypertension is associated with greater efficacy and cost effectiveness than losartan or enalapril.
Conclusion
Suboptimal therapies are still being used to manage hypertension, despite the availability of effective therapies. Employing effective antihypertensive treatment in patients is essential to reduce the morbidity and mortality associated with hypertension in sub-Saharan Africa, where BP control rates are alarmingly low. In this large-scale analysis of medical insurance claims in South Africa, perindopril-based antihypertensive treatment appears to be associated with a lower rate of cardiovascular events over a 5-year period compared with enalapril- or losartan-based regimens. Our analysis indicated that the clinical benefits of perindopril were coupled with significant cost benefits, both statistically and socioeconomically. These observations, which need to be confirmed in a broader South African population, may have significant implications for the choice of therapy in patients with hypertension.
Data Availability
Data that have been anonymized and aggregated to prevent individual identification along with other relevant material such as statistical analyses can be provided, upon reasonable request, to individuals with credible academic/research credentials willing to handle the data in a manner which is consistent with confidentiality requirements. Please contact the corresponding author or Alykhan.vira@quantium.com.
References
Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol. 2021;18:785–802.
NCD Risk Factor Collaboration. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80.
Peer N, Uthman OA, Kengne A-P. Rising prevalence, and improved but suboptimal management, of hypertension in South Africa: a comparison of two national surveys. Glob Epidemiol. 2021;3: 100063.
Dzudie A, Rayner B, Ojji D, et al. Roadmap to achieve 25% hypertension control in Africa by 2025. Cardiovasc J Afr. 2017;28:262–72.
Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension global hypertension practice guidelines. J Hypertens. 2020;38:982–1004.
Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure-lowering on outcome incidence in hypertension: 5 head-to-head comparisons of various classes of antihypertensive drugs—overview and meta-analyses. J Hypertens. 2015;33:1321–41.
Wei J, Galaviz KI, Kowalski AJ, et al. Comparison of cardiovascular events among users of different classes of antihypertension medications: a systematic review and network meta-analysis. JAMA Netw Open. 2020;3: e1921618.
van Vark LC, Bertrand M, Akkerhuis KM, et al. Angiotensin-converting enzyme inhibitors reduce mortality in hypertension: a meta-analysis of randomized clinical trials of renin-angiotensin-aldosterone system inhibitors involving 158,998 patients. Eur Heart J. 2012;33:2088–97.
Comini L, Bachetti T, Cargnoni A, et al. Therapeutic modulation of the nitric oxide: all ACE inhibitors are not equivalent. Pharmacol Res. 2007;56:42–8.
Snyman JR, Wessels F. Perindopril: do randomised, controlled trials support an ACE inhibitor class effect? A meta-analysis of clinical trials. Cardiovasc J Afr. 2009;20:127–34.
Hopkins KL, Hlongwane KE, Otwombe K, et al. The substantial burden of non-communicable diseases and HIV-comorbidity amongst adults: screening results from an integrated HIV testing services clinic for adults in Soweto, South Africa. EClinicalMedicine. 2021;38: 101015.
Li EC, Heran BS, Wright JM. Angiotensin converting enzyme (ACE) inhibitors versus angiotensin receptor blockers for primary hypertension. Cochrane Database Syst Rev. 2014:CD009096.
Lv X, Zhang Y, Niu Y, Song Q, Zhao Q. Comparison of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers on cardiovascular outcomes in hypertensive patients with type 2 diabetes mellitus: a PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore). 2018;97: e0256.
Mancia G, Rea F, Corrao G, Grassi G. Two-drug combinations as first-step antihypertensive treatment. Circ Res. 2019;124:1113–23.
Council for Medical Schemes. Industry Report 2020: regulating through a pandemic. 2020. https://www.medicalschemes.co.za/cms-annual-report-2020-21/. Accessed July 18, 2022.
World Health Organization. ATC/DDD Index 2022. 2022. https://www.whocc.no/atc_ddd_index/. Accessed July 18, 2022.
Ellis RP. Risk adjustment in health care markets: concepts and applications In: Lu M, Jonsson E, editors. Financing health care: new ideas for a changing society. Wernheim: Wiley‐VCH Verlag GmbH & Co. KGaA; 2007. p. 177–222.
Nedbank. Average annual exchange rates. 2021. https://www.nedbank.co.za/content/dam/nedbank/site-assets/AboutUs/Economics_Unit/Forecast_and_data/Daily_Rates/Annual_Average_Exchange_Rates.pdf. Accessed July 18, 2022.
Barber JA, Thompson SG. Analysis of cost data in randomized trials: an application of the non-parametric bootstrap. Stat Med. 2000;19:3219–36.
Chang CH, Lin JW, Caffrey JL, Wu LC, Lai MS. Different angiotensin-converting enzyme inhibitors and the associations with overall and cause-specific mortalities in patients with hypertension. Am J Hypertens. 2015;28:823–30.
Daly CA, Fox KM, Remme WJ, et al. The effect of perindopril on cardiovascular morbidity and mortality in patients with diabetes in the EUROPA study: results from the PERSUADE substudy. Eur Heart J. 2005;26:1369–78.
Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–67.
van Onzenoort HA, Menger FE, Neef C, et al. Participation in a clinical trial enhances adherence and persistence to treatment: a retrospective cohort study. Hypertension. 2011;58:573–8.
Feng Y, Han M, Qie R, et al. Adherence to antihypertensive medications for secondary prevention of cardiovascular disease events: a dose-response meta-analysis. Public Health. 2021;196:179–85.
Arca M, Fusco D, Barone AP, Perucci CA. Risk adjustment and outcome research. Part I. J Cardiovasc Med (Hagerstown). 2006;7:682–90.
Havranek EP, Mujahid MS, Barr DA, et al. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132:873–98.
Statista. Average monthly earnings in South Africa from November 2015 to November 2020. 2021. https://www.statista.com/statistics/1227081/average-monthly-earnings-in-south-africa/. Accessed July 18, 2022.
Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–223.
Statistics South Africa. Statistical release (revised) P0301.4. Census 2011. 2012. https://www.statssa.gov.za/publications/P03014/P030142011.pdf. Accessed July 18, 2022.
Govender K, Girdwood S, Letswalo D, Long L, Meyer-Rath G, Miot J. Primary healthcare seeking behaviour of low-income patients across the public and private health sectors in South Africa. BMC Public Health. 2021;21:1649.
Medical Writing and Editorial Assistance
Editorial assistance in the preparation of this article was provided by Catherine Rees, who wrote the first draft of the manuscript on behalf of Springer Healthcare Communications. Support for this assistance was funded by Servier. We would also like to thank Shailav Bansal, Akhil Sakile and Lindsay Thomas of Quantium for their assistance with data and statistical analyses.
Funding
Open Access funding was provided by the University of Cape Town. Quantium Health South Africa is a healthcare consultancy that conducts independent outcome studies using real world data. The Rapid Service Fee and medical writing assistance was all funded by Servier.
Author information
Authors and Affiliations
Contributions
Conceptualization: Jacques R. Snyman, Olufunke A. Alaba, Alykhan Vira, Ntobeko A. B. Ntusi; Methodology: Jacques R. Snyman; Formal analysis and investigation: Freedom Gumedze, Erika S. W. Jones, Olufunke A. Alaba, Nqoba Tsabedze; Writing-original draft preparation: Alykhan Vira; Writing-review and editing: Jacques R. Snyman, Freedom Gumedze, Erika S. W. Jones, Olufunke A. Alaba, Nqoba Tsabedze, Alykhan Vira and Ntobeko A. B. Ntusi; Supervision: Alykhan Vira. Ntobeko A. B. Ntusi obtained ethics approval for usage of the dataset and takes overall responsibility for veracity of the manuscript and its contents. Jacques R. Snyman and Alykhan Vira have verified the underlying data. All authors confirm that they had permission to access/use all the data included in the study and approved the final draft of the manuscript for publication.
Corresponding author
Ethics declarations
Conflict of Interest
Jacques R. Snyman has received honoraria from Servier. Freedom Gumedze has received honoraria from Servier. Erika S. W. Jones has received sponsorship and honoraria from Servier and Pharmadynamics. Olufunke A. Alaba has received honoraria from Servier. Nqoba Tsabedze has received consultation fees from Novartis Pharmaceuticals, Novo Nordisk, Boston Scientific, Pfizer, Servier, Phillips, Takeda, AstraZeneca, Acino Health Care Group and Merck; and educational and travel grants from Medtronic, Biotronik, Boston Scientific and Vertice Health Care Group. Alykhan Vira is an employee of Quantium Health South Africa. Ntobeko A. B. Ntusi acknowledges support from the South African Medical Research Council (SA-MRC), National Research Foundation and the Lily and Ernst Hausmann Trust; unrestricted educational grants from Siemens, General Electric, Philips and CVI42; and honoraria from Novo Nordisk and Servier.
Ethical Approval
All work was carried out in accordance with the Helsinki Declaration of 1964, and its later amendments. Ethics approval was obtained by Professor Ntobeko A. B. Ntusi from the University of Cape Town faculty of Health Sciences Human Research Ethics Committee (HREC: 778/2021) for the usage of the dataset. Informed consent was not required for this study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Snyman, J.R., Gumedze, F., Jones, E.S.W. et al. Comparing Cardiovascular Outcomes and Costs of Perindopril-, Enalapril- or Losartan-Based Antihypertensive Regimens in South Africa: Real-World Medical Claims Database Analysis. Adv Ther 40, 5076–5089 (2023). https://doi.org/10.1007/s12325-023-02641-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02641-8