Abstract
Introduction
Triptorelin is available as 1- and 3-month prolonged-release (PR) formulations; at the time of the study, only the former was approved for central precocious puberty (CPP) in China. This study assessed the efficacy and safety of the triptorelin 3-month PR formulation in Chinese children with CPP.
Methods
In this 12-month, prospective, open-label, multicentre, single-arm study (NCT04736602), Chinese children (mean age [standard deviation (SD)], 7.6 ± 0.8 years) with CPP received triptorelin pamoate 15 mg on day 1 and at months 3, 6 and 9. The primary endpoint was the proportion with luteinizing hormone (LH) suppression (stimulated peak LH ≤ 3 IU/L after gonadotropin-releasing hormone [GnRH] stimulation) at month 3. Secondary endpoints included changes from baseline in hormone levels and clinical parameters, as well as safety assessments.
Results
Overall, 32 children were enrolled, including three boys. LH suppression to prepubertal levels (≤ 3 IU/L) after GnRH stimulation was observed in 100%, 93.5% and 93.5% of participants at months 3, 6 and 12, respectively. Basal and peak LH and follicle-stimulating hormone levels were substantially suppressed at months 3, 6 and 12, and most participants showed sex hormone suppression. At months 6 and 12 respectively 92.9% and 89.3% of girls had stable breast development, and all boys had stable genital development. There was a decrease in mean growth velocity from baseline (8.96 cm/year) to months 3, 6 and 12 (8.07, 5.24 and 6.94 cm/year, respectively). The mean difference between bone and chronological age decreased from baseline (2.85 years) to month 12 (2.39 years). In girls, uterine length was stable or reduced at month 12; in boys, testicular volume was reduced. Triptorelin was well tolerated.
Conclusion
The triptorelin 3-month PR formulation demonstrated similar efficacy to that previously reported in non-Chinese patients with CPP and had an acceptable safety profile. This supports triptorelin 3-month PR as a viable option for Chinese children with CPP.
Plain Language Summary
Central precocious puberty (CPP) occurs when the reproductive organs and secondary sexual characteristics develop too early in children (before 8 years old in girls or 9 years old in boys). It can cause significant psychological harm and may lead to health problems later in life. Triptorelin is a type of treatment designed to suppress the hormonal activity responsible for CPP and therefore slow down early pubertal development. Triptorelin can be given as an injection into muscle every month or every 3 months; the 3-monthly formulation is commonly used in many countries but at the time of this study it was not licensed for patients with CPP in China. Our trial assessed the effect of triptorelin treatment every 3 months for 1 year in 32 Chinese children with CPP. For all patients who had measurements available, 3-monthly triptorelin suppressed luteinizing hormone—a key hormone involved in CPP—to below typical prepubertal levels. Other hormones involved in puberty were also suppressed. Children experienced a slowing down of the development of secondary sexual characteristics (breasts, genitals and pubic hair), and stabilization or reduction in the size of internal sexual organs (uterine length in girls and testicular volume in boys). Their height also increased less rapidly than previously. There were no concerning side effects of triptorelin treatment, and the safety profile matched that seen in other countries where triptorelin is widely used for CPP. Overall, our study findings suggest that the 3-monthly triptorelin formulation may be a good option for Chinese children with CPP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? | |
Central precocious puberty (CPP) is a paediatric endocrine disease in which rapid development of the reproductive organs and secondary sexual characteristics occurs before the age of 8 years in girls or 9 years in boys. | |
Triptorelin, used in the treatment of CPP, is available as 1- and 3-month prolonged-release (PR) formulations, but at the time of this study only the former was approved for CPP in China. | |
This phase 3, 12-month, prospective, open-label, multicentre, single-arm study assessed the efficacy and safety of triptorelin pamoate 3-month PR formulation in Chinese children with CPP. | |
What was learned from the study? | |
The triptorelin 3-month PR formulation suppressed luteinizing hormone to prepubertal levels (≤ 3 IU/L) after gonadotropin-releasing hormone stimulation in all study participants and had an acceptable safety profile. | |
This study confirmed the efficacy and safety profile of triptorelin 3-month PR formulation in this setting and supports its use as a viable treatment option in Chinese children with CPP. |
Introduction
Central precocious puberty (CPP) is a paediatric endocrine disease in which rapid development of the reproductive organs and secondary sexual characteristics occurs before the age of 8 years in girls or 9 years in boys, due to early activation of hypothalamic–pituitary–gonad (HPG) axis function [1]. Specific genetic alterations, central nervous system lesions and social stressors are major drivers of CPP, but a significant number of patients with CPP have no identified aetiology [1]. The prevalence of CPP in China has been estimated at approximately 5% of a school-based population [2, 3].
The physical implications of CPP may include accelerated bone maturation (often resulting in shorter final height) and health problems later in life (e.g. an increased risk of metabolic comorbidities, such as obesity, type 2 diabetes and hypertension) [1]. CPP can also result in significant negative psychological effects for both patients and their caregivers [1, 4]. In a case–control study of 210 children in China, children with idiopathic CPP demonstrated lower quality of life and greater family impact than healthy controls [5].
Gonadotropin-releasing hormone (GnRH) analogues are widely used in the treatment of CPP, resulting in downregulation and suppression of the HPG axis [6]. The most common treatments for CPP in China are monthly formulations of triptorelin or leuprorelin [7,8,9,10].
Triptorelin is a synthetic GnRH analogue characterized by replacement of the l-glycine in the sixth position by a d-tryptophan. This modification increases resistance to enzymatic degradation and affinity for the pituitary receptor, thereby prolonging plasma half-life and increasing potency. In China, triptorelin is available as 1-month and 3-month prolonged-release (PR) formulations; however, the latter was not approved for CPP at the time of this study (although it had been approved for locally advanced or metastatic prostate cancer since 2008, and for endometriosis since 2021) [7, 8].
Several studies conducted in other countries have established the efficacy and safety of the triptorelin 3-month PR formulation in CPP [11,12,13,14]. In a meta-analysis of trial data from 153 children with CPP who received triptorelin 3-month PR (140 female, 13 male), 87.6% had a suppressed peak luteinizing hormone (LH) response to the GnRH test at 3 months, and 92.8% at 6 months [15]. Follicle-stimulating hormone (FSH) peak, oestradiol and testosterone were also suppressed in most patients at 3 months.
However, clinical data were previously lacking for this formulation among patients with CPP in China. This phase 3 study assessed the efficacy and safety of the triptorelin 3-month PR formulation in Chinese children with CPP to investigate if the treatment effect was the same or showed a similar trend to that observed in non-Chinese CPP populations.
Methods
Study Design
This was a prospective, open-label, multicentre, single-arm, interventional study evaluating the efficacy and safety of the triptorelin 3-month PR formulation in Chinese children with CPP (NCT04736602). The study was conducted at six investigational sites in China between March 2021 and September 2022. Patients received four doses of triptorelin pamoate 15 mg (Diphereline®, Ipsen; delivering 11.25 mg of triptorelin to the patient), given on day 1 and months 3, 6 and 9 of this 12-month study. Doses were administered by intramuscular injection in the upper outer quadrant of the right or left buttock.
The study was conducted in accordance with the provisions of the Declaration of Helsinki and Good Clinical Practice of China and in compliance with local ethics committees and informed consent regulations. The study protocol (including amendments) and informed consent form were reviewed and approved by an ethics committee prior to commencement of the study, and during the study where applicable. Written informed consent was obtained from one or both of each child’s parents/guardians, and signed assent was obtained from the child when applicable, prior to study entry.
Participants
Eligible patients were required to show evidence of CPP, as listed below:
-
Onset of development of secondary sex characteristics before 8 years of age (girls) or before 9 years of age (boys), according to the Tanner method (for girls, Tanner staging ≥ 2 for breast development, enlarged uterine length, and several follicles with diameter > 4 mm in the ovary on pelvic type B ultrasound; for boys, testicular volume ≥ 4 mL on testicular type B ultrasound).
-
A pubertal response of LH to the GnRH stimulation test (stimulated peak LH ≥ 5 IU/L).
-
A difference between bone age and chronological age of greater than 1 year.
In addition, included patients were required to be aged less than 9 years (girls) or less than 10 years (boys) on initiation of triptorelin treatment, and to weigh at least 20 kg. Girls who had already achieved menophania/menarche were also required to have a negative pregnancy test prior to the start of study treatment.
Key exclusion criteria included: gonadotropin-independent (peripheral) precocious puberty (extrapituitary secretion of gonadotropins or gonadotropin-independent gonadal or adrenal sex steroid secretion); non-progressing isolated premature thelarche; presence of an unstable intracranial tumour or an intracranial tumour requiring neurosurgery or cerebral irradiation (although patients with hamartomas not requiring surgery were eligible); any other condition or chronic illness or treatment possibly interfering with growth or other study endpoints (e.g. chronic steroid use except topical steroids, renal failure, diabetes, moderate-to-severe scoliosis); or prior or current therapy with a GnRH analogue, medroxyprogesterone acetate, growth hormone or insulin-like growth factor 1.
Procedures and Assessments
The main study consisted of; a screening visit (up to 4 weeks prior to treatment initiation); a day 1 visit for drug administration; a month 3 visit for efficacy and safety assessments and a further cycle of drug administration; and a month 6 visit (end of study/early withdrawal) for efficacy and safety assessments. Extension of the study provided the possibility for patients to continue with treatment (per investigator decision) for an additional 6 months—with drug administration at the month 6 and month 9 visits, and an ‘end of extension phase’ visit at month 12. Efficacy and safety assessments were made at each of these additional visits. The extension phase was optional. Each patient was therefore treated with the study drug for up to 12 months.
The primary efficacy analysis was the proportion of children with LH suppression, defined as stimulated peak LH of 3 IU/L or lower after GnRH stimulation at month 3. The GnRH stimulation test was performed using an intravenous injection of gonadorelin to stimulate gonadotrophin release; blood samples were collected prior to and 30, 60 and 90 min after the gonadorelin injection for central assessment of serum LH levels.
Secondary efficacy endpoints are listed in Table 1. Safety assessments included any treatment-emergent adverse events (TEAEs) occurring throughout the study, changes in laboratory parameters and measurements from physical examination/vital signs. All adverse events (AEs) were recorded and graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events Version 5.0.
As an exploratory pharmacokinetic (PK) endpoint, plasma triptorelin concentrations were assessed at day 1 (4 h post-injection to correlate with expected peak concentration of triptorelin [16]), month 3 and month 6, using a validated, specific and sensitive liquid chromatography–tandem mass spectrometry method. Sparse sampling was used to minimize invasive blood sampling in the children.
Statistics
Although no formal statistical testing was performed, the following assumptions were made on the basis of a previous global pivotal study [13] for determining the required sample size: the expected outcome for the proportion of children with a suppressed LH response to the GnRH stimulation test (stimulated peak LH ≤ 3 IU/L) at month 3 was 90%; the null proportion was 70%; an exact binomial test of a proportion with a one-sided nominal significance level of 0.05 and power of 85%; and an expected common dropout rate of 10%. Under these assumptions, enrolment of approximately 32 patients (28 with an additional 10% dropouts) was planned, including 3 boys.
The analysis sets used included:
-
Intention-to-treat (ITT) population: All patients who received at least one dose of study medication.
-
Modified ITT (mITT) population: All treated patients with at least one baseline and month 3 post-baseline assessment of the primary efficacy endpoint.
-
Per protocol (PP) set: All patients in the mITT set, excluding those with major protocol deviations that could potentially affect the primary efficacy endpoint.
-
Safety population: All patients who received at least one dose of study medication and had at least one post-baseline safety assessment.
-
PK set: All patients who received at least one dose of study medication and had at least one valid and quantifiable concentration during the study.
For the primary efficacy analysis, the two-sided 90% confidence interval (CI) was computed by SAS® (SAS Institute Inc., Cary, NC) using exact binomial distributions on the mITT population. Two-sided 90% CIs were also constructed for all secondary endpoints expressed as proportions. Where relevant, efficacy endpoints were also analysed in the PP set.
Results
Patient Characteristics
Forty-two patients were screened, of whom 10 were not suitable for enrolment (did not meet the entry criteria, n = 5; withdrawn by parent/guardian, n = 5) (Fig. 1). Thus, 32 patients were enrolled (Table 2). Twenty-nine patients (90.6%) were female and three (9.4%) were male, and the mean age was 7.6 ± 0.8 years. Mean baseline GnRH-stimulated peak values for LH and FSH were 24.66 ± 17.85 IU/L and 12.82 ± 4.59 IU/L, respectively.
Thirty-one patients completed the month 3 visit, and 30 and 29 patients completed the month 6 visit and the end of study month 12 visit, respectively. Three patients (all female) discontinued the study as a result of withdrawal by their parent/guardian. All 32 enrolled patients were included in the ITT and safety populations. The patient who did not complete the month 3 visit was excluded from the mITT population because of not having a primary efficacy endpoint assessment, and hence there were 31 patients in the mITT dataset. This child was also excluded from the PP population, along with one other who had a major protocol deviation (only one follicle > 4 mm, contrary to the inclusion criteria); hence, there were 30 patients in the PP dataset.
Hormonal Suppression
In the analysis of the primary endpoint, all 31 patients in the mITT population (100%; 90% CI 90.8–100.0) had LH suppression to prepubertal levels (≤ 3 IU/L) after GnRH stimulation at month 3 (Fig. 2). At months 6 and 12, 29 patients (93.5%; 90% CI 81.1–98.8) had LH suppression to prepubertal levels after GnRH stimulation; hormonal suppression data were missing for the remaining three of the 32 enrolled patients, due to study withdrawal by their parent/guardian.
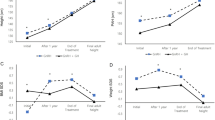
In both female and male participants, basal LH and FSH levels were substantially suppressed at month 3 and at all subsequent visits up to 12 months of treatment with triptorelin 3-month PR (mITT population; Fig. 3a, b). Mean basal LH decreased from 1.09 ± 1.65 IU/L at baseline to 0.40 ± 0.24 IU/L at month 3, 0.39 ± 0.31 IU/L at month 6 and 0.22 ± 0.20 IU/L at month 12. Similarly, mean basal FSH fell from 3.38 ± 1.92 IU/L at baseline to 1.02 ± 0.50, 1.24 ± 0.56 and 1.55 ± 0.90 IU/L at months 3, 6 and 12, respectively.
Hormonal suppression at months 3–12. Modified intention-to-treat population. All data are mean (standard deviation). Horizontal dotted lines represent the lower limit of quantification for each assay (testosterone, 0.12 ng/mL; oestradiol, 17.94 pg/mL). BLQ below the limit of quantification, FSH follicle-stimulating hormone, LH luteinizing hormone
Mean peak LH levels fell from 24.09 ± 17.85 IU/L at baseline to 1.00 ± 0.49 IU/L at month 3, 1.02 ± 0.63 IU/L at month 6 and 0.90 ± 0.63 IU/L at month 12 (Fig. 3c). In addition, mean peak FSH levels decreased from 12.68 ± 4.59 IU/L at baseline to 1.40 ± 0.72, 1.68 ± 0.74 and 2.33 ± 1.34 IU/L at months 3, 6 and 12, respectively (Fig. 3d).
With regard to sex hormones, at month 3, all 31 patients (100%) showed suppression to within the prepubertal range (oestradiol ≤ 20 pg/mL in girls or testosterone ≤ 0.3 ng/mL in boys) (Fig. 3e, f). At months 6 and 12, sex hormone suppression was evident in 30 patients (96.8%; 90% CI 85.6–99.8) and 29 patients (93.5%; 90% CI 81.1–98.8), respectively.
Similar levels of hormonal suppression were reported in the PP population (data not shown).
Clinical Efficacy
Pubertal stage was assessed during the study relative to baseline (mITT population; Table 3). At month 6, 92.9% (26/28) of female patients had a stable breast development stage (for one female, breast stage increased from Tanner puberty stage 2 [T2] at baseline to Tanner puberty stage 4 [T4] at month 6, but her pubic hair development stage was stable; a second female withdrew from the study), and all three male patients had a stable genital development stage; 96.4% (27/28) of girls and all boys had a stable pubic hair development stage. At month 12, 89.3% (25/28) of female patients still had stable breast development and 82.1% (23/28) had stable pubic hair development, and all boys still had stable genital and pubic hair development. Breast and pubic hair development stage data were missing for one female patient at month 6 and two female patients at month 12.
Changes from baseline in auxological parameters are provided in Table 3. There were mean increases in height (2.24, 3.55 and 6.54 cm), weight (1.28, 2.53 and 4.82 kg) and body mass index (BMI) (0.14, 0.47 and 0.90 kg/m2) at months 3, 6 and 12, respectively. The overall mean (SD) BMI observed at baseline (16.96 [1.84] kg/m2) and months 3, 6 and 12 (17.10 [2.14], 17.51 [2.05] and 17.90 [2.38] kg/m2, respectively) were within the normal range for Chinese children [17]. Mean growth velocity was reduced by − 0.90, − 3.77 and − 2.05 cm/year at months 3, 6 and 12. The overall mean (SD) growth velocity values observed at baseline and months 3, 6 and 12 were all within the normal range for Chinese children [18] (8.96 [2.24], 8.07 [2.19], 5.24 [2.51], 6.94 [2.82] cm/year, respectively) and therefore final adult height would not be expected to be impacted.
Bone age increased somewhat from baseline to months 6 and 12 (mean change 0.23 years and 0.59 years, respectively). However, the mean difference between bone and chronological age decreased from 2.82 years at baseline to 2.41 years at month 6 and 2.39 years at month 12.
In girls, uterine length was stable or reduced from baseline to months 6 and 12 (mean change − 0.40 cm and − 0.38 cm, respectively). Similarly, in boys, testicular volume was reduced on both the left (mean change − 2.40 mL and − 2.88 mL) and right sides (mean change − 4.73 mL and − 6.80 mL).
Safety
In the safety population, 27 patients (84.4%) reported a total of 90 TEAEs (Table 4). The most common TEAEs were upper respiratory tract infection (31.3%), abnormal weight gain (21.9%), bronchitis (9.4%), overweight (9.4%), vitamin D deficiency (9.4%), cough (9.4%) and rhinorrhoea (9.4%). Of the 90 TEAEs, 18 in 10 patients (31.3%) were considered to be drug-related, most commonly abnormal weight gain (n = 3; 9.4%). One patient (3.1%) experienced a grade ≥ 3 TEAE (dermatitis allergic; not related to the study treatment), and two participants (6.3%) had serious AEs (both pneumonia; not related to the study treatment). No TEAEs led to treatment discontinuation, and there were no deaths.
Laboratory parameters and vital signs remained stable throughout the study compared with baseline, and no potentially clinically significant abnormalities occurred. There were no abnormal physical examination findings.
Injections were well tolerated, and no local tolerability reactions were reported.
PK Analysis
At baseline (pre-dose), 31 of the 32 included patients had triptorelin plasma concentrations below the limit of quantification; 4 h post-injection, mean concentrations rose to 47.6 ± 23.9 ng/mL. At months 3 (pre-dose) and 6, the mean plasma concentrations of triptorelin were 70.4 ± 54.4 pg/mL and 66.1 ± 56.9 pg/mL, respectively.
Discussion
This prospective, single-arm phase 3 study evaluated the efficacy and safety of the triptorelin 3-month PR formulation in paediatric patients with CPP in China to identify if the outcomes were similar to those observed in non-Chinese patients with CPP [11,12,13,14]. LH suppression to prepubertal levels (≤ 3 IU/L) after GnRH stimulation was observed in all patients (apart from those with missing data) at months 3, 6 and 12, confirming treatment efficacy. The safety profile was acceptable and matched that observed previously in patients with CPP [11, 13]. There were no treatment-related grade ≥ 3 or serious TEAEs, no TEAEs leading to treatment or study discontinuation and no deaths. These findings confirmed the efficacy and safety profile of triptorelin 3-month PR formulation in this setting and support its use as a monotherapy treatment option in Chinese children.
The efficacy results were observed to be well aligned with those from previous studies [11,12,13,14,15]. As expected, and in line with previous studies solely assessing the 3-month sustained-release triptorelin [11,12,13], treatment with the triptorelin 3-month PR formulation in the current study was observed to efficiently suppress the pituitary–gonadal axis and pubertal development in children with CPP.
A retrospective study involving 106 Korean girls with CPP compared the efficacy of a triptorelin 11.25 mg 3-month depot with that of a 3.75 mg 1-month depot in suppressing pubertal development for the treatment of CPP [14]. The efficacy of the long-acting triptorelin 3-month formulation was comparable with the 1-month depot regarding hormonal suppression. At 6 months, 90.0% and 98.2% of the girls treated with the 3-month and 1-month depots exhibited suppressed levels of LH to the triptorelin injection (serum LH < 2.5 IU/L), respectively. In addition, after 12 months of treatment, LH suppression was observed in 93.5% and 100% of the girls treated with the 3-month and 1-month depots, respectively. Findings from the current study were in line with results for both treatment formulations in the population of Korean girls. The current results were also similar to those from previous studies performed in largely Caucasian populations; in a meta-analysis of earlier trials, the proportion of patients with a suppressed peak LH response after GnRH stimulation was 87.6% at 3 months and 92.8% at 6 months [15]—compared with 100% and 93.5% in the current study. Thus, it appears that there are no substantial differences in outcomes between Caucasian and Asian patients.
In addition to hormonal suppression, the present study demonstrated effects on several clinical measures, including stabilization of pubertal stage, deceleration of gonadal development and a reduction in the difference between bone and chronological age. These effects may have important psychological benefits to patients given the stress that can be associated with significant early alterations in physical appearance [4]. Findings observed for reductions in serum FSH and sex steroids and slowing of pubertal development were comparable with previous studies [11, 12, 14]. At baseline, 28/31 (90.3%) patients had a mean difference between bone and chronological age of at least 2 years and 18/31 (58.1%) patients exhibited breast/genital development stages III and IV. The presence of these two clinical features may indicate that the children with CPP included in the study had a relatively severe phenotype with rapid development of the reproductive organs and secondary sexual characteristics. The confirmed treatment efficacy of triptorelin 3-month PR formulation in the patients included in this study supports the use of this formulation in paediatric patients with CPP in China.
At month 12, although 82.1% of participants had stable pubic hair development, three girls did have an increase in pubic hair development stage from T1 to T2. This progression in pubic hair during therapy is not surprising because the appearance of pubic hair results from a rise in adrenal androgen concentrations [19], which are not under the control of LH and FSH. Similarly, breast development was stable in 89.3% of female patients, but one 8-year-old girl experienced a breast stage increase from T2 to T4, despite achieving hormonal suppression, a decrease in the difference between bone and chronological age and a reduction in uterine length. The reason for this increase in breast development stage is unclear but may be due to a relatively rapid increase in weight, with an observed change in weight of 3, 6.5, 8.5 and 11 kg at months 3, 6, 9 and 12, respectively. Of note, Tanner staging can be affected by excess fat, because this can be difficult to distinguish from true glandular breast tissue. The higher incidence of obesity associated with CPP does not usually appear to be related to GnRH agonist administration [20, 21], implying that other factors specific to this individual likely influenced her change in weight.
In general, the safety profile of the triptorelin 3-month PR formulation was similar to that observed in previous studies in patients with CPP. In the two European studies, the most frequent AEs reported were headache, rhinitis, abdominal pain, gastroenteritis, rash, hot flush, vomiting and injection site pain. In the current study, respiratory tract infections were most common, with two participants reported to have pneumonia as a serious AE; however, these were both considered unrelated to the study treatment. Other common TEAEs in the current study were abnormal weight gain, bronchitis, overweight, vitamin D deficiency, cough and rhinorrhoea. There were two treatment-related TEAEs that occurred in the current study that were not reported in the previous European studies, including upper respiratory tract infection (n = 2) and impaired fasting glucose (n = 1). However, these were all mild (grade 1–2) and overall no TEAEs led to treatment discontinuation, and there were no deaths.
PK analysis confirmed plasma concentrations after 4 h were similar to maximum plasma concentrations reported in a previous study for triptorelin pamoate 3-month PR [22]. Quantification of triptorelin plasma concentrations revealed that levels remained detectable at months 3 and 6 and were similar to those observed in the pivotal European study which assessed the used of the triptorelin 3-month depot in children with CPP [11].
Strengths of this phase 3 study include the prospective, multicentre design and the inclusion of a substantial number of Chinese children, including boys. Limitations include the open-label and single-arm study design. However, this was similar to previous studies, thereby facilitating comparison between the current trial and findings from previously published work [11,12,13,14]. The open-label design would not be expected to significantly bias overall study outcomes given that most endpoints were based on objective measures (e.g. hormone levels).
In China, the most commonly used treatments for CPP are based on monthly administration [7]. Although the present study made no direct comparison with such formulations, it supported the efficacy and safety of triptorelin 3-month PR. Less frequent dosing has the potential to improve overall convenience and reduce the burden of treatment on patients and carers—which may be particularly relevant given that several years of treatment are often required.
Conclusions
This study confirms the treatment efficacy and safety profile of triptorelin 3-month PR formulation in paediatric patients with CPP in China and identified no substantial differences in outcomes to those reported in non-Chinese patients with CPP.
References
Maione L, Bouvattier C, Kaiser UB. Central precocious puberty: recent advances in understanding the aetiology and in the clinical approach. Clin Endocrinol (Oxf). 2021;95(4):542–55.
Liu Y, Yu T, Li X, et al. Prevalence of precocious puberty among Chinese children: a school population-based study. Endocrine. 2021;72(2):573–81.
Zhang Y, Ni J, Zhang L, et al. The prevalence of precocious puberty among children in Qufu City, Shandong Province, China, a population-based study. Front Endocrinol. 2022;13: 910119.
López-Miralles M, Lacomba-Trejo L, Valero-Moreno S, Benavides G, Pérez-Marín M. Psychological aspects of pre-adolescents or adolescents with precocious puberty: a systematic review. J Pediatr Nurs. 2022;64:e61–8.
Yang H, Luo S, Liang X, et al. The association between family impact and health-related quality of life of children with idiopathic central precocious puberty in Chongqing, China. Health Qual Life Outcomes. 2021;19(1):171.
Eugster EA. Treatment of central precocious puberty. J Endocr Soc. 2019;3(5):965–72.
Ipsen Limited. Patient information leaflet; Diphereline® Triptorelin Acetate for Injection Leaflet. 2022.
Ipsen Limited. Patient information leaflet; Diphereline® Triptorelin Pamoate for Injection Leaflet. 2022.
Ipsen Limited. Patient information leaflet; Leuprorelin Acetate Microspheres (3.75mg [CN]) for Injection Leaflet. 2021.
Ipsen Limited. Patient information leaflet; Leuprorelin Acetate Microspheres (11.25mg [CN]) for Injection Leaflet. 2021.
Carel JC, Blumberg J, Seymour C, Adamsbaum C, Lahlou N. Three-month sustained-release triptorelin (11.25 mg) in the treatment of central precocious puberty. Eur J Endocrinol. 2006;154(1):119–24.
Martínez-Aguayo A, Hernández MI, Beas F, et al. Treatment of central precocious puberty with triptorelin 11.25 mg depot formulation. J Pediatr Endocrinol Metab. 2006;19(8):963–70.
Zenaty D, Blumberg J, Liyanage N, et al. A 6-month trial of the efficacy and safety of triptorelin pamoate (11.25 mg) every 3 months in children with precocious puberty: a retrospective comparison with triptorelin acetate. Horm Res Paediatr. 2016;86(3):188–95.
Chung LY, Kang E, Nam HK, Rhie YJ, Lee KH. Efficacy of triptorelin 3-month depot compared to 1-month depot for the treatment of Korean girls with central precocious puberty in single tertiary center. J Korean Med Sci. 2021;36(34): e219.
Durand A, Tauber M, Patel B, Dutailly P. Meta-analysis of paediatric patients with central precocious puberty treated with intramuscular triptorelin 11.25 mg 3-month prolonged-release formulation. Horm Res Paediatr. 2017;87(4):224–32.
Lebret T, Rouanne M, Hublarov O, et al. Efficacy of triptorelin pamoate 11.25 mg administered subcutaneously for achieving medical castration levels of testosterone in patients with locally advanced or metastatic prostate cancer. Ther Adv Urol. 2015;7(3):125–34.
Song P, Li X, Gasevic D, Flores AB, Yu Z. BMI, waist circumference reference values for Chinese school-aged children and adolescents. Int J Environ Res Public Health. 2016;13(6):589.
Chen L, Su B, Zhang Y, et al. Association between height growth patterns in puberty and stature in late adolescence: a longitudinal analysis in Chinese children and adolescents from 2006 to 2016. Front Endocrinol (Lausanne). 2022;13: 882840.
Abreu AP, Kaiser UB. Pubertal development and regulation. Lancet Diabetes Endocrinol. 2016;4(3):254–64.
Palmert MR, Mansfield MJ, Crowley WF Jr, et al. Is obesity an outcome of gonadotropin-releasing hormone agonist administration? Analysis of growth and body composition in 110 patients with central precocious puberty. J Clin Endocrinol Metab. 1999;84(12):4480–8.
Shiasi Arani K, Heidari F. Gonadotropin-releasing hormone agonist therapy and obesity in girls. Int J Endocrinol Metab. 2015;13(3): e23085.
Li X, Li H, Shi H, et al. Assessment of two formulations of triptorelin in Chinese patients with endometriosis: a phase 3, randomized controlled trial. Adv Ther. 2022;39(10):4663–77.
Acknowledgements
The authors thank all participants who took part in the study and their caregivers.
Medical Writing and/or Editorial Assistance
The authors thank Kirsty Walters (PhD) and Tamzin Gristwood (PhD) of Oxford PharmaGenesis, Oxford, UK, for providing medical writing support, which was sponsored by Ipsen in accordance with Good Publication Practice (GPP) guidelines.
Funding
Sponsorship for this study and the journal’s Open Access and Rapid Service fee were funded by Ipsen.
Author Contributions
All authors have provided substantial contributions to the conception and design of the study; acquisition, analysis and interpretation of data; drafting of the publication, or revising it critically for important intellectual content; and final approval of the article for publication.
Disclosures
Xiaoping Luo: No competing interests to disclose. Cai Zhang: No competing interests to disclose. Yu Yang: No competing interests to disclose. Xu Xu: No competing interests to disclose. Xinran Cheng: No competing interests to disclose. Haiyan Wei: No competing interests to disclose. Lanying Wang: No competing interests to disclose. Frank Huang, Xiaofeng Shi and Patrick Cabri are employees of Ipsen.
Compliance with Ethics Guidelines
The study was conducted in accordance with the provisions of the Declaration of Helsinki and Good Clinical Practice of China and in compliance with local ethics committees and informed consent regulations. The study protocol (including amendments) and informed consent form were reviewed and approved by an ethics committee prior to commencement of the study, and during the study where applicable. Written informed consent was obtained from one or both of each child’s parents/guardians, and signed assent was obtained from the child when applicable, prior to study entry.
Data Availability Statement
Qualified researchers may request access to patient-level study data that underlie the results reported in this publication. Additional relevant study documents, including the clinical study report, study protocol with any amendments, annotated case report form, statistical analysis plan and dataset specifications may also be made available. Patient-level data will be anonymized, and study documents will be redacted to protect the privacy of study participants. Where applicable, data from eligible studies are available 6 months after the studied medicine and indication have been approved in the US and EU or after the primary manuscript describing the results has been accepted for publication, whichever is later. Further details on Ipsen's sharing criteria, eligible studies and process for sharing are available here (https://vivli.org/members/ourmembers/). Any requests should be submitted to www.vivli.org for assessment by an independent scientific review board.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Luo, X., Zhang, C., Yang, Y. et al. Efficacy and Safety of Triptorelin 3-Month Formulation in Chinese Children with Central Precocious Puberty: A Phase 3, Open-Label, Single-Arm Study. Adv Ther 40, 4574–4588 (2023). https://doi.org/10.1007/s12325-023-02617-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02617-8