Abstract
Introduction
In the European Union (EU), the indication for the antifibrotic pirfenidone prior to April 2023 did not include patients with advanced idiopathic pulmonary fibrosis (IPF). This analysis compared the efficacy and safety of pirfenidone in advanced IPF versus non-advanced IPF.
Methods
Data were included from the following studies of pirfenidone: ASCEND (NCT01366209); CAPACITY (004 [NCT00287716] and 006 [NCT00287729]); RECAP (NCT00662038; advanced IPF defined as percent predicted forced vital capacity [%FVC] < 50% and/or percent predicted carbon monoxide diffusing capacity [%DLco] < 35% at baseline); PASSPORT (NCT02699879; advanced IPF defined as baseline %FVC < 50%); and SP-IPF (NCT02951429; patients with advanced IPF [defined as %DLco ≤ 40% at screening] at risk of group 3 pulmonary hypertension).
Results
In the pooled ASCEND/CAPACITY studies, the annual mean rate of FVC decline from baseline to Week 52 was significantly lower for pirfenidone versus placebo in advanced (p = 0.0035) and non-advanced IPF (p = 0.0001). Rate of all-cause mortality over 52 weeks was numerically lower for pirfenidone versus placebo in advanced and non-advanced IPF. In RECAP, the mean annual rate of FVC decline from baseline to Week 180 of pirfenidone treatment was similar in patients with advanced (− 141.5 mL) and non-advanced IPF (− 153.5 mL). In SP-IPF, the mean annual rate of FVC decline and rate of all-cause mortality from baseline to Week 52 in patients treated with placebo + pirfenidone were − 93.0 mL and 20.2%, respectively. No new safety signals were identified, and the safety profile of pirfenidone in patients with advanced IPF was generally consistent with that of non-advanced IPF.
Conclusions
These results highlight the benefit of pirfenidone treatment in patients with advanced and non-advanced IPF. As such, the indication for pirfenidone in the EU has now been updated to include the treatment of adult patients with advanced IPF.
Trial Registrations
ASCEND (NCT01366209), CAPACITY 004 (NCT00287716), CAPACITY 006 (NCT00287729), RECAP (NCT00662038), PASSPORT (NCT02699879), and SP-IPF (NCT02951429).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Idiopathic pulmonary fibrosis (IPF) is a chronic, fibrosing interstitial lung disease that has a poor prognosis. |
In the European Union (EU), the antifibrotic pirfenidone was first approved in 2011 for the treatment of IPF. On the basis of the available data at that time, the approval did not include patients with advanced IPF. |
With the aim of supporting the inclusion of patients with advanced IPF to the indication of pirfenidone in the EU, this post-hoc analysis compared the safety and efficacy of pirfenidone in patients with advanced IPF versus those with non-advanced IPF. |
What was learned from this study? |
The results of this post-hoc analysis highlight the benefit of pirfenidone treatment in patients with advanced and non-advanced IPF. The safety profile of pirfenidone was also generally consistent between patients with advanced IPF and non-advanced IPF. |
On the basis of these data, the indication for pirfenidone in the EU has been expanded to include the treatment of patients with advanced IPF. |
Introduction
Idiopathic pulmonary fibrosis (IPF) is a chronic, fibrosing interstitial lung disease that is characterized by progressive worsening of dyspnea and lung function, and has a poor prognosis [1,2,3]. In general, the progression of IPF is not linear [4,5,6]; some patients may experience rapid deterioration and progression to death, whereas others can experience periods of relative stability followed by periods of acute respiratory decline [1, 7]. There is no standardized definition for the staging of IPF [3, 4]; however, IPF staging has traditionally been defined by terms such as “mild,” “moderate,” and “severe” or “early” and “advanced,” and has typically been based on pulmonary function test results [4, 8,9,10]. Previous studies have generally classified patients with IPF as having mild-to-moderate lung impairment based on a percent predicted forced vital capacity (%FVC) of ≥ 50% to 55% and a percent predicted carbon monoxide diffusing capacity (%DLco) of ≥ 30% to 40%, while those with severe or advanced IPF have been classified as having %FVC and %DLco values lower than these thresholds [4, 11,12,13,14].
The inclusion criteria for clinical trials of patients with IPF have varied, and many clinical trials in IPF have excluded patients with advanced disease [11, 15,16,17,18]. For example, the multinational, placebo-controlled trial of interferon gamma-1b only included patients with %FVC 50–90% and %DLco ≥ 25% [18]; the pivotal Phase 3 trials of pirfenidone only included patients with %FVC ≥ 50%, %DLco ≥ 35%, and either %FVC or %DLco ≤ 90% (CAPACITY) [15], or %FVC 50–90% and %DLco 30–90% (ASCEND) [16]; and the Phase 3 trials of nintedanib (INPULSIS-1 and INPULSIS-2) only included patients with %FVC ≥ 50% and %DLco 30–79% [17].
Nintedanib and pirfenidone are the only two antifibrotics approved for the treatment of patients with IPF [19]. Pirfenidone was first approved for the treatment of IPF by the European Medicines Agency (EMA) in 2011 [20]; however, this approval was limited to patients with mild-to-moderate IPF based on available data at the time of approval. In 2014, the US Food and Drug Administration granted approvals for both pirfenidone and nintedanib for the treatment of patients with IPF regardless of disease severity [21, 22], and in 2015, the EMA also approved nintedanib for the treatment of patients with IPF regardless of disease severity [23]. No evidence of new safety concerns relating to the use of pirfenidone in specifically patients with advanced IPF has emerged in over 10 years of post-marketing experience outside the European Union (EU; i.e., in countries where it is approved for the treatment of patients with IPF regardless of severity), and several studies have highlighted that pirfenidone may have a favorable benefit–risk profile in patients with advanced IPF [24,25,26].
Therefore, this post-hoc analysis aimed to compare the efficacy and safety of pirfenidone in patients with advanced IPF versus those with non-advanced IPF using data from six studies of pirfenidone in patients with IPF.
Methods
Study Designs
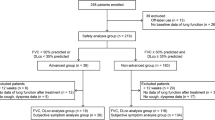
This post-hoc analysis included data from the ASCEND (NCT01366209), CAPACITY (004 [NCT00287716] and 006 [NCT00287729]), RECAP (NCT00662038), PASSPORT (NCT02699879), and SP-IPF (NCT02951429) studies of pirfenidone (Fig. 1). The designs and inclusion/exclusion criteria for these studies have been previously reported in detail [15, 16, 25, 27, 28]. Briefly, the ASCEND study was a 52-week Phase 3 trial of pirfenidone (2403 mg/day) versus placebo (1:1) in 555 patients with IPF with %FVC 50–90% and %DLco 30–90% [16]. The CAPACITY studies (004 and 006) were pivotal 72-week Phase 3 trials of pirfenidone versus placebo in 779 patients with IPF with %FVC ≥ 50%, %DLco ≥ 35%, and either %FVC or %DLco ≤ 90%. In CAPACITY 004, patients were randomized 2:1:2 to pirfenidone 2403 mg/day, pirfenidone 1197 mg/day, or placebo, and in CAPACITY 006, patients were randomized 1:1 to pirfenidone (2403 mg/day) versus placebo [15]. The RECAP study was an open-label extension (OLE) study for patients who completed the ASCEND or CAPACITY studies (n = 1058), during which they could continue or start to receive pirfenidone (≤ 2403 mg/day) [27]. PASSPORT was a multicenter, prospective, post-authorization study of 1009 patients (99.7% with IPF) who were followed for up to 2 years after initiating treatment with pirfenidone [28]. As a result of the real-world nature of the PASSPORT study, the inclusion/exclusion criteria were minimally restrictive, and patients were not included/excluded on the basis of their %FVC and %DLco. Lastly, the SP-IPF study was a Phase 2b 52-week trial of sildenafil (60 mg/day) plus pirfenidone (2403 mg/day) (sildenafil + pirfenidone) versus placebo with added pirfenidone (2403 mg/day) (placebo + pirfenidone) in patients with advanced IPF (DLco ≤ 40% predicted at screening) at risk of group 3 pulmonary hypertension (PH) [25]. No prospective data were collected during this post-hoc analysis; therefore, ethical approval was not required. However, during the original trials, all patients provided informed consent, the protocols were approved by the institutional review boards or ethics committees at each participating center, and the trials were conducted in accordance with the Declaration of Helsinki.
Overview of the studies and patient populations included in the post-hoc analysis. No imputation was performed for missing data. aEfficacy data were pooled for the ASCEND and CAPACITY studies. The RECAP and SP-IPF studies were analyzed separately. bAssessment at 12 months was chosen for the pooled ASCEND/CAPACITY population since this is the duration of ASCEND for which data were available to be pooled with data from CAPACITY. cThe pooled safety population included data from ASCEND, CAPACITY, RECAP, and SP-IPF. Data from PASSPORT were analyzed separately. dExposure-adjusted data were used for this analysis to account for the differences in study duration and follow-up. 6MWD 6-min walk distance; FVC forced vital capacity, IPF idiopathic pulmonary fibrosis, OLE open-label extension, TEAE treatment-emergent adverse event
Patient Populations
This post-hoc analysis included patients who participated in the ASCEND, CAPACITY (004 and 006), and RECAP trials, split by those with advanced IPF (defined as %FVC < 50% and/or %DLco < 35%) or non-advanced IPF (defined as %FVC ≥ 50% and %DLco ≥ 35%) at baseline for ASCEND and CAPACITY or at time of enrollment for RECAP; patients who participated in the PASSPORT study with advanced IPF (defined as baseline %FVC < 50% only, because no %DLco data were collected in this study); and patients with advanced IPF (defined as %DLco ≤ 40% at screening) at risk of group 3 PH who participated in the SP-IPF study (Fig. 1).
Differences in study designs prevented any direct comparisons between all patients in a pooled efficacy population; therefore, three separate patient populations were used for the efficacy analyses. The first efficacy population included patients randomized to pirfenidone or placebo in the pooled ASCEND/CAPACITY studies. The second population included patients who had %FVC and/or %DLco data available at baseline and received pirfenidone up to 180 weeks in RECAP, and the third population included patients with advanced IPF at risk of group 3 PH who received placebo + pirfenidone over 52 weeks in SP-IPF. Given that PASSPORT was a safety study, no efficacy data were collected in that study.
Direct comparison of the frequency of treatment-emergent adverse events (TEAEs) between patients with advanced and non-advanced IPF in the pooled safety population was deemed inappropriate because of the different study designs and duration of follow-up between studies. Instead, exposure-adjusted data were used to account for the differences in study duration and follow-up, and TEAE rates were calculated as a rate per 100 patient-years (PY). Additionally, analyses of clinical safety were split by patients who were pirfenidone treatment naïve and those who were pre-treated with pirfenidone at baseline, to control for any potential confounders caused by prior exposure to pirfenidone. Therefore, the pooled safety population included pirfenidone treatment-naïve patients with advanced and non-advanced IPF enrolled in the ASCEND, CAPACITY, and RECAP studies, pirfenidone pre-treated patients with advanced and non-advanced IPF enrolled in the RECAP study, and pirfenidone pre-treated patients with advanced IPF enrolled in the SP-IPF study. Patients who were treated with pirfenidone in the ASCEND or CAPACITY studies, and subsequently enrolled in RECAP, were considered pre-treated for this analysis. As a result of differences in study assessments, safety data from the PASSPORT study were reported separately to the pooled safety population.
Efficacy Endpoints
To assess the efficacy of pirfenidone in patients with advanced IPF versus non-advanced IPF, the annual rate of change from baseline in FVC volume (mL) and rate of all-cause mortality were assessed in all three efficacy populations. Outcomes were assessed at Week 52 for the pooled ASCEND/CAPACITY studies and the SP-IPF study, and at Week 180 for RECAP. Additionally, categorical change in FVC ≥ 10% or death, mean change in 6-min walk distance (6MWD), and categorical change in 6MWD ≥ 50 m or death from baseline to Week 52 for pirfenidone versus placebo were assessed in the pooled ASCEND/CAPACITY studies only (Fig. 1).
Safety Endpoints
To assess the safety of pirfenidone in patients with advanced IPF and those with non-advanced IPF, exposure-adjusted rate of TEAEs, defined as adverse events with an onset date from first date of study drug administration until last date of study drug administration, were assessed in the pooled safety population. Additionally, the safety profile of pirfenidone versus placebo patients with advanced IPF was assessed in the pooled ASCEND/CAPACITY studies only. Ancillary safety data from the PASSPORT study were reported separately, as this study collected adverse drug reactions (ADRs), i.e., only AEs deemed causally related to pirfenidone, rather than all TEAEs regardless of causality (Fig. 1).
Statistical Analyses
Data from the pooled ASCEND/CAPACITY studies were analyzed until Week 52 for efficacy in order to provide comparable results because of differences in study length (52 weeks for ASCEND and 72 weeks for the CAPACITY trials). Linear slope analysis of change from baseline to Week 52 in FVC volume (mL) was performed using a mixed model, and slopes were calculated on the basis of observed data using actual observation times. Categorical change in FVC ≥ 10% or death was calculated using the difference between baseline and Week 52% FVC values; if a patient died before Week 52, their death was counted as an event. Mean change in 6MWD from baseline to Week 52 was calculated using the observed values at the two time points; patients who died before Week 52 were excluded from the analysis. Categorical change in 6MWD ≥ 50 m or death was calculated using change in 6MWD between baseline and Week 52; if a patient died before Week 52, their death was counted as an event. All-cause mortality was compared between pirfenidone and placebo using the log rank test. A proportional hazards model, with treatment as a fixed effect, was used to estimate the hazard ratio (HR) and 95% confidence intervals (CI). Kaplan–Meier curves were used to display event times and the number of patients at risk. Patients without an event were censored at or prior to 52 weeks, as appropriate, for each outcome and 52-week completion status. All p values reported for the efficacy endpoints are of exploratory nature, as all analyses were performed retrospectively.
In patients from the RECAP study, decline in FVC volume over 180 weeks was measured using change from baseline and linear slope analysis of annual rate of decline. Annual FVC decline was estimated using a single-arm repeated-measures model for patients with advanced and non-advanced IPF.
In patients from the SP-IPF study, change from baseline in FVC volume at 52 weeks was measured using linear slope analysis.
TEAEs in the safety population were summarized descriptively. Descriptive comparison of TEAEs between patients with advanced and non-advanced IPF was performed at the system organ class (SOC) level, followed by an investigation of preferred terms for SOCs with a higher frequency in patients with advanced versus non-advanced IPF.
Results
Patients
The efficacy analysis population included 1247 patients from the pooled ASCEND/CAPACITY studies, of whom 170 had advanced IPF (pirfenidone, n = 90; placebo, n = 80) and 1077 had non-advanced IPF (pirfenidone, n = 533; placebo, n = 544); 596 patients who received pirfenidone in the RECAP study, of whom 187 had advanced IPF and 409 had non-advanced IPF; and 89 patients with advanced IPF and risk of group 3 PH who received placebo + pirfenidone in the SP-IPF study (Fig. 1).
Baseline demographics for the efficacy population were generally similar for patients with advanced and non-advanced IPF across the pooled ASCEND/CAPACITY population and the RECAP population, regardless of disease severity or treatment received (Table 1). However, some notable differences in other baseline characteristics were observed. For example, prior to enrollment in these studies, patients with advanced IPF had a shorter duration of treatment, and a longer time from diagnosis to treatment versus those with non-advanced IPF. Other observed differences in baseline characteristics between the severity groups were consistent with the selection criteria and natural history of IPF. Baseline characteristics from patients with advanced IPF in the SP-IPF study have been published previously [25].
The pooled safety analysis population included a total of 1308 patients treated with pirfenidone. Overall, 894 patients were classified as treatment naïve (advanced IPF, n = 177; non-advanced IPF, n = 717) and 414 patients were classified as pre-treated (advanced IPF, n = 189; non-advanced IPF, n = 225). Additionally, 1009 patients (144 patients with advanced IPF) from the PASSPORT study were included in the separate safety analysis (Fig. 1). Baseline characteristics for the pooled safety analysis population are presented in the Supplementary Material.
Efficacy Outcomes
All efficacy data for patients with advanced and non-advanced IPF are presented in Table 2.
Pooled ASCEND/CAPACITY Studies
The annual mean rate of FVC decline from baseline to Week 52 was significantly lower for pirfenidone versus placebo in patients with advanced IPF (− 150.9 vs − 277.6; p = 0.0035) and in patients with non-advanced IPF (− 128.7 vs − 216.7; p < 0.0001). The absolute and relative treatment differences for pirfenidone versus placebo did not differ in a clinically meaningful way between patients with advanced IPF (126.7 mL and 45.6%, respectively) and non-advanced IPF (88.0 mL and 40.6%, respectively). Furthermore, there were significantly fewer patients in the pirfenidone group versus the placebo group who experienced a categorical decline in FVC ≥ 10% or death in both the advanced (18.9% vs 42.5%; p = 0.0008) and non-advanced (14.1% vs 23.9%; p < 0.0001) groups (Table 2).
In both the advanced IPF and non-advanced IPF groups, mean change in 6MWD from baseline to Week 52 was significantly lower for pirfenidone versus placebo (advanced IPF, − 62.7 m vs − 112.4 m, p = 0.0477; non-advanced IPF, − 25.7 m vs − 45.5 m, p = 0.0031), and there were significantly fewer patients in the pirfenidone group versus the placebo group who experienced a categorical decline in 6MWD ≥ 50 m or death (advanced IPF, 43.3% vs 60.0%, p = 0.0305; non-advanced IPF, 21.4% vs 30.5%, p = 0.0006; Table 2).
Of note, a greater rate of progression (in terms of change in FVC and 6MWD over 52 weeks) was observed for patients with advanced IPF versus non-advanced IPF. Moreover, in the advanced IPF and non-advanced IPF groups, the proportion of patients who had FVC ≥ 50% at baseline but progressed to FVC < 50% at Week 52 was lower for pirfenidone versus placebo (advanced IPF, 24.4% vs 35.0%; non-advanced IPF, 10.1% vs 14.7%).
The rate of all-cause mortality over 52 weeks was numerically lower in patients who received pirfenidone versus those who received placebo in the advanced IPF group (4.4% vs 15.0%). In the non-advanced IPF group, the rate of all-cause mortality over 52 weeks was generally similar for pirfenidone versus placebo (3.4% vs 5.5%). In time-to-event analyses, patients with advanced IPF who received pirfenidone had a significantly lower risk of all-cause mortality over 52 weeks versus those treated with placebo (HR 0.28 [95% CI 0.09, 0.88]; p = 0.0194) (Fig. 2a), whereas the risk of all-cause mortality over 52 weeks in patients with non-advanced IPF was not significantly different for pirfenidone versus placebo (HR 0.61 [95% CI 0.34, 1.09]; p = 0.090) (Fig. 2b).
RECAP Study
The mean annual rate of FVC decline from baseline to Week 180 was similar with longer-term pirfenidone treatment in patients with advanced IPF (− 141.5 mL) and non-advanced IPF (− 153.5 mL). The rate of all-cause mortality over 180 weeks was numerically higher in patients with advanced IPF (27.8%) versus those with non-advanced IPF (12.0%).
SP-IPF Study
In patients with advanced IPF at risk of group 3 PH treated with placebo + pirfenidone, the mean annual rate of FVC decline from baseline to Week 52 was − 93.0 mL and the rate of all-cause mortality over 52 weeks was 20.2%.
Safety Outcomes
Exposure-Adjusted Safety Profile Summary (Pooled Safety Patient Population)
Overall, in both pirfenidone treatment-naïve and pirfenidone pre-treated patients, similar rates of TEAEs occurred in patients with advanced IPF compared with non-advanced IPF (868.5/100 PY versus 816.7/100 PY, respectively; and 675.2/100 PY versus 673.1/100 PY, respectively; Table 3). However, the exposure-adjusted event rates of serious TEAEs, severe TEAEs, TEAEs leading to death, and TEAEs leading to treatment discontinuation in pirfenidone treatment-naïve patients and pre-treated patients were higher in patients with advanced IPF than in patients with non-advanced IPF (Table 3).
Distribution of TEAEs by SOC (Safety Patient Population)
Pirfenidone Treatment-Naïve Patients
When TEAEs were analyzed in treatment-naïve patients by SOC, two SOCs showed a higher TEAE rate (defined as a rate difference of ≥ 10/100 PY) in patients with advanced IPF versus non-advanced IPF: respiratory, thoracic, and mediastinal disorder; and cardiac disorders (Fig. 3a). The exposure-adjusted event rate difference between patients with advanced IPF and non-advanced IPF observed in the respiratory, thoracic, and mediastinal disorders SOC was primarily driven by the preferred term IPF (rate difference 14.9/100 PY), followed by other events directly or indirectly related to the higher severity of the underlying disease, such as dyspnea (rate difference 9.5/100 PY), pulmonary hypertension (9.1/100 PY), and hypoxia (5.5/100 PY). The CIs for the exposure-adjusted rates of IPF and dyspnea were not overlapping in both pirfenidone treatment-naïve and pre-treated patients, which is expected for events worsening in the advanced stages of IPF. For PH and hypoxia, the CIs were not overlapping in pirfenidone treatment-naïve patients only; however, the number of such reports was too small for a robust assessment. The exposure-adjusted event rate difference between patients with advanced IPF and non-advanced IPF observed in the cardiac disorders SOC was mainly driven by atrial fibrillation (rate difference 2.8/100 PY) and tachycardia (2.3/100 PY). Atrial arrhythmias are the most commonly seen arrhythmias in patients with IPF, and supraventricular tachycardia and multifocal atrial tachycardia are known to be cardiac manifestations of IPF [29].
Pirfenidone Pre-treated Patients
When TEAEs were analyzed in pre-treated patients by SOC, two SOCs showed a higher TEAE rate (defined as a rate difference of ≥ 10/100 PY) in patients with advanced IPF versus non-advanced IPF: respiratory, thoracic, and mediastinal disorders; and infections and infestations (Fig. 3b). The exposure-adjusted event rate difference between patients with advanced IPF and non-advanced IPF observed in the respiratory, thoracic, and mediastinal disorders SOC was primarily driven by IPF (rate difference 21.8/100 PY), followed by other events directly or indirectly related to the higher severity of the underlying disease, such as dyspnea (9.4/100 PY), respiratory failure (3.2/100 PY), and pulmonary hypertension (2.1/100 PY). The exposure-adjusted event rate difference between patients with advanced IPF and non-advanced IPF observed in the infections and infestations SOC was mainly due to respiratory tract infections (lower respiratory tract infection, rate difference 9.5/100 PY; bronchitis, 4.8/100 PY; upper respiratory tract infection, 4.8/100 PY; respiratory tract infection, 3.6/100 PY; and pneumonia, 2.0/100 PY).
Safety Profile of Pirfenidone in Patients with Advanced IPF (Pooled ASCEND/CAPACITY Studies Only)
Overall, similar rates of TEAEs were observed for patients with advanced IPF who received pirfenidone or placebo (100% versus 97.5%; Table 4). However, lower rates of serious TEAEs, severe TEAEs, and TEAEs leading to death were observed for patients with advanced IPF who received pirfenidone versus placebo. In addition, patients with advanced IPF who received placebo experienced a higher frequency of respiratory TEAEs versus those who received pirfenidone. The TEAEs reported more frequently in patients with advanced IPF who received pirfenidone versus placebo were either established reactions associated with pirfenidone [20] (e.g., gastrointestinal [GI] disorders [80.0% vs 62.5%]; Table 4) or non-serious events assessed to be unrelated to pirfenidone by the investigator.
ADRs in PASSPORT
Of 144 patients with advanced IPF in the PASSPORT study, 91 (63.2%) experienced a total of 213 ADRs of special interest (serious and non-serious). The predominant category of ADRs of special interest was GI symptoms (63 [43.8%] patients with 104 events), followed by weight loss (30 [20.8%] patients with 35 events), fatigue (28 [19.4%] patients with 31 events), and photosensitivity reactions and skin rashes (23 [16.0%] patients with 31 events).
In the total population, including patients with advanced and non-advanced IPF, 693/1009 (68.7%) patients experienced a total of 1577 ADRs of special interest. The predominant category of ADRs of special interest was GI symptoms (38.3%), followed by photosensitivity reactions and skin rashes (29.0%), fatigue (24.2%), and weight loss (16.1%) [28].
Discussion
The efficacy and safety profile of pirfenidone has previously been confirmed in patients with less advanced IPF in several studies [15, 16, 27]. However, a more recent study and post-hoc analyses have provided evidence to suggest that pirfenidone is also efficacious, with an acceptable safety profile, in patients with advanced IPF [24,25,26]. Therefore, this post-hoc analysis aimed to compare the efficacy and safety of pirfenidone in patients with advanced IPF versus non-advanced IPF using data from six studies of pirfenidone.
The results presented here highlight the benefit of pirfenidone treatment in patients with advanced and non-advanced IPF. In the pooled ASCEND/CAPACITY studies, both patients with advanced IPF and non-advanced IPF who received pirfenidone had a significantly reduced decline in lung function and exercise capacity versus those who received placebo. It is also important to acknowledge that in the pooled ASCEND/CAPACITY studies, a greater rate of progression was observed for patients with advanced IPF versus non-advanced IPF, which is consistent with the natural history of IPF. Moreover, patients with advanced IPF who received pirfenidone had a lower rate of all-cause mortality versus those who received placebo. Although no significant difference in mortality rate was found for pirfenidone versus placebo in the non-advanced group, by better preserving their lung function, pirfenidone was successful in reducing the proportion of patients who progressed to advanced IPF based on %FVC (and who would then have had an increased risk of mortality). Additionally, in RECAP, the longer-term treatment benefit of pirfenidone on lung function decline was similar in patients with advanced IPF versus those with non-advanced IPF. Furthermore, consistent with the natural history of IPF, the all-cause mortality rates in the RECAP study were higher in patients with advanced IPF compared with those with non-advanced IPF. In SP-IPF, patients with advanced IPF who received placebo + pirfenidone experienced less deterioration in lung function versus the advanced and non-advanced patient populations from the other studies in this analysis; however, this may be due to the differences in how advanced IPF was defined in the different studies (e.g., SP-IPF was the only study that also had being at risk of group 3 PH as an inclusion criterion, and also did not consider baseline %FVC) and so direct comparisons are not appropriate. The rate of all-cause mortality in the SP-IPF study was slightly higher in patients with advanced IPF at risk of PH who received placebo + pirfenidone compared with the advanced patient population who received pirfenidone in the pooled ASCEND/CAPACITY trials; however, this is consistent with current understanding of increased mortality rates among patients with IPF and PH [30, 31]. Overall, these results demonstrate the treatment benefit of pirfenidone versus placebo in patients with advanced IPF by highlighting that placebo-treated patients have poorer outcomes versus pirfenidone-treated patients, regardless of disease severity.
No new safety signals were identified among patients with advanced IPF, and the safety profile of pirfenidone in patients with advanced IPF was generally consistent with the safety profile in patients with non-advanced IPF. In pirfenidone treatment-naïve patients and pre-treated patients, similar rates of TEAEs occurred in patients with advanced IPF compared with non-advanced IPF, and events that occurred at a higher rate in patients with advanced IPF were attributed, directly or indirectly, to the higher severity of the underlying disease. In the pooled ASCEND/CAPACITY studies, the rate of TEAEs in patients with advanced IPF was similar for those who received pirfenidone versus placebo. However, patients who received placebo experienced a higher frequency of respiratory TEAEs compared with those who received pirfenidone, whereas TEAEs that were reported more frequently in those who received pirfenidone were either established reactions associated with pirfenidone or non-serious events assessed to be unrelated to pirfenidone by the Investigator.
This post-hoc analysis was a thorough examination of existing data, and the results support the growing body of evidence suggesting that pirfenidone is efficacious and well tolerated in patients with advanced IPF. A previous post hoc analysis investigating the effect of pirfenidone versus placebo over 52 weeks in patients with IPF and more advanced lung function impairment (%FVC < 50% and/or %DLco < 35%) from the ASCEND and CAPACITY (004 and 006) trials showed that pirfenidone-treated patients had significantly reduced risks of all-cause mortality and significantly less deterioration in lung function, exercise capacity, and dyspnea compared with placebo-treated patients [24]. Similarly, results from a previous post-hoc analysis of the RECAP study demonstrated that long-term pirfenidone treatment was efficacious in both patients with more advanced IPF (%FVC < 50% and/or %DLco < 35%) and those with less advanced IPF (%FVC ≥ 50% and %DLco ≥ 35%) [26]. Additionally, the safety profile of pirfenidone was generally similar between patients with more and less advanced disease, with the exception of adverse events related to the higher severity of the underlying disease, which were experienced more frequently in patients with more advanced IPF [26]. Furthermore, evidence from the Phase 2b placebo-controlled SP-IPF study of sildenafil added to pirfenidone in patients with advanced IPF (%DLco ≤ 40% at screening) at risk of group 3 PH suggested a tolerability of pirfenidone in patients with advanced IPF similar to that shown in the ASCEND, CAPACITY (004 and 006), and RECAP studies [25].
Within the broader IPF treatment landscape, nintedanib was approved for the treatment of patients with IPF, regardless of disease severity, throughout the EU in 2015 based on two 52-week, Phase 3, placebo-controlled trials of nintedanib in patients with IPF (INPULSIS: NCT01335464 and NCT01335477) [17, 23]. Despite previous studies showing that pirfenidone may also be efficacious in patients with advanced IPF [24,25,26], the approval of pirfenidone in the EU remains limited to the treatment of mild-to-moderate IPF at the time of writing [20].
This analysis is limited by its post-hoc nature and the small number of patients with advanced IPF relative to those with non-advanced IPF. It should also be noted that although the criteria for advanced IPF were %FVC < 50% and/or %DLco < 35% in the ASCEND/CAPACITY and RECAP analyses, the patients in the advanced IPF groups for these studies had a mean baseline %FVC of 59.8–66.6%, thus suggesting that the efficacy findings may be generalizable only to patients with advanced IPF as defined by the DLco criterion and not necessarily to patients with both %DLco < 35% and %FVC < 50%. Furthermore, as a result of the different study designs and patient populations, it was not possible to pool together data from all studies, hence the use of several separate analyses.
Conclusions
Overall, the results from this post-hoc analysis highlight the benefit of pirfenidone treatment in patients with advanced and non-advanced IPF. On the basis of FVC and 6MWD, and mortality rates, pirfenidone was shown to be efficacious versus placebo in both patients with advanced IPF (baseline %DLco < 35%) and those with non-advanced IPF. The benefit of pirfenidone relative to placebo was comparable between patients with advanced and non-advanced IPF, and continued efficacy was observed during the OLE period of the RECAP study in both populations. Additionally, on the basis of the pooled ASCEND/CAPACITY data, a greater rate of progression (decline in FVC, decline in 6MWD, and rate of all-cause mortality) was observed for patients with advanced IPF versus non-advanced IPF; however, no statistical comparisons were performed between these groups. The safety profile of pirfenidone was generally consistent between patients with advanced IPF and those with non-advanced IPF, with the exception of adverse events related to the higher severity of the underlying disease, which were experienced more frequently in patients with advanced IPF. On the basis of these data, the indication for pirfenidone in the EU was expanded in April 2023 to include the treatment of adult patients with advanced IPF [32].
References
Ley B, Collard HR, King TE Jr. Clinical course and prediction of survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2011;183(4):431–40.
Kaunisto J, Salomaa E-R, Hodgson U, et al. Demographics and survival of patients with idiopathic pulmonary fibrosis in the FinnishIPF registry. ERJ Open Res. 2019;5(3):00170–2018.
Raghu G, Remy-Jardin M, Richeldi L, et al. Idiopathic pulmonary fibrosis (an update) and progressive pulmonary fibrosis in adults: an official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2022;205(9):e18–47.
Kolb M, Collard HR. Staging of idiopathic pulmonary fibrosis: past, present and future. Eur Respir Rev. 2014;23(132):220–4.
Martinez FJ, Safrin S, Weycker D, et al. The clinical course of patients with idiopathic pulmonary fibrosis. Ann Intern Med. 2005;142(12 Pt 1):963–7.
Kim DS, Collard HR, King TE Jr. Classification and natural history of the idiopathic interstitial pneumonias. Proc Am Thorac Soc. 2006;3(4):285–92.
Collard HR, Moore BB, Flaherty KR, et al. Acute exacerbations of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2007;176(7):636–43.
Nathan SD, Shlobin OA, Weir N, et al. Long-term course and prognosis of idiopathic pulmonary fibrosis in the new millennium. Chest. 2011;140(1):221–9.
Caminati A, Cassandro R, Torre O, Harari S. Severe idiopathic pulmonary fibrosis: what can be done? Eur Respir Rev. 2017;26: 170047.
Robbie H, Daccord C, Chua F, Devaraj A. Evaluating disease severity in idiopathic pulmonary fibrosis. Eur Respir Rev. 2017;26(145): 170051.
Richeldi L, Kolb M, Jouneau S, et al. Efficacy and safety of nintedanib in patients with advanced idiopathic pulmonary fibrosis. BMC Pulm Med. 2020;20(1):3.
Kolb M, Raghu G, Wells AU, et al. INSTAGE investigators: nintedanib plus sildenafil in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2018;379(18):1722–31.
Durheim MT, Bendstrup E, Carlson L, et al. Outcomes of patients with advanced idiopathic pulmonary fibrosis treated with nintedanib or pirfenidone in a real-world multicentre cohort. Respirology. 2021;26(10):982–8.
Yoon H-Y, Kim DS, Song JW. Efficacy and safety of pirfenidone in advanced idiopathic pulmonary fibrosis. Respiration. 2019;97(3):242–51.
Noble PW, Albera C, Bradford WZ, et al. Pirfenidone in patients with idiopathic pulmonary fibrosis (CAPACITY): two randomised trials. Lancet. 2011;377(9779):1760–9.
King TE Jr, Bradford WZ, Castro-Bernardini S, et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2014;370(22):2083–92.
Richeldi L, du Bois RM, Raghu G, et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med. 2014;370(22):2071–82.
Raghu G, Brown KK, Bradford WZ, et al. Idiopathic pulmonary fibrosis study group: a placebo-controlled trial of interferon gamma-1b in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2004;350(2):125–33.
Maher TM, Strek ME. Antifibrotic therapy for idiopathic pulmonary fibrosis: time to treat. Respir Res. 2019;20(1):205.
European Medicines Agency: Summary of Product Characteristics - Esbriet (pirfenidone). 2021. https://www.ema.europa.eu/en/documents/product-information/esbriet-epar-product-information_en.pdf. Accessed 27 January 2023.
Food and Drug Administration: Highlights of Prescribing Information - OFEV®. 2022. https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/205832Orig1s016lbl.pdf. Accessed 27 January 2023.
Food and Drug Administration: Highlights of Prescribing Information - ESBRIET®. 2022. https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/022535s015,208780s005lbl.pdf. Accessed 27 January 2023.
European Medicines Agency: Summary of Product Characteristics - Ofev (nintedanib). 2021. https://www.ema.europa.eu/en/documents/product-information/ofev-epar-product-information_en.pdf. Accessed 27 January 2023.
Nathan SD, Costabel U, Albera C, et al. Pirfenidone in patients with idiopathic pulmonary fibrosis and more advanced lung function impairment. Respir Med. 2019;153:44–51.
Behr J, Nathan SD, Wuyts WA, et al. Efficacy and safety of sildenafil added to pirfenidone in patients with advanced idiopathic pulmonary fibrosis and risk of pulmonary hypertension: a double-blind, randomised, placebo-controlled, phase 2b trial. Lancet Respir Med. 2021;9(1):85–95.
Costabel U, Albera C, Glassberg MK, et al. Effect of pirfenidone in patients with more advanced idiopathic pulmonary fibrosis. Respir Res. 2019;20(1):55.
Costabel U, Albera C, Lancaster LH, et al. An open-label study of the long-term safety of pirfenidone in patients with idiopathic pulmonary fibrosis (RECAP). Respiration. 2017;94(5):408–15.
Cottin V, Koschel D, Günther A, et al. Long-term safety of pirfenidone: results of the prospective, observational PASSPORT study. ERJ Open Res. 2018;4(4):00084–2018.
Agrawal A, Verma I, Shah V, Agarwal A, Sikachi RR. Cardiac manifestations of idiopathic pulmonary fibrosis. Intractable Rare Dis Res. 2016;5(2):70–5.
Nadrous HF, Pellikka PA, Krowka MJ, et al. Pulmonary hypertension in patients with idiopathic pulmonary fibrosis. Chest. 2005;128(4):2393–9.
Lettieri CJ, Nathan SD, Barnett SD, Ahmad S, Shorr AF. Prevalence and outcomes of pulmonary arterial hypertension in advanced idiopathic pulmonary fibrosis. Chest. 2006;129(3):746–52.
European Medicines Agency: Summary of Product Characteristics - Esbriet (pirfenidone). 2023. https://www.ema.europa.eu/en/documents/product-information/esbriet-epar-product-information_en.pdf. Accessed 9 May 2023.
Acknowledgements
We would like to thank the patients, their family members, and participating staff at all study centers. We would also like to thank Klaus-Uwe Kirchgaessler of F. Hoffmann-La Roche, Ltd. for his support and input into these analyses.
Funding
Open Access funding enabled and organized by Projekt DEAL. This post-hoc analysis was sponsored by F. Hoffman-La Roche, Ltd. The costs associated with Rapid Service and Open Access fees were funded by F. Hoffmann-La Roche, Ltd./Genentech, Inc.
Medical Writing, Editorial, and Other Assistance
Medical writing support, under the direction of the authors, was provided by Georgie Cowell and Leigh Clements of CMC AFFINITY, a division of IPG Health Medical Communications, funded by F. Hoffmann-La Roche, Ltd./Genentech, Inc.
Author Contributions
All authors (Jürgen Behr, Steven D. Nathan, Ulrich Costabel, Carlo Albera, Wim A. Wuyts, Marilyn K. Glassberg, Harold Haller Jr, Giuseppe Alvaro, Frank Gilberg, Katerina Samara, Lisa Lancaster) contributed to the manuscript from the outset, and read and approved the final draft. All authors vouch for the accuracy of the content included in the final manuscript.
Prior Presentation
Some data from this manuscript have been previously presented at the European Respiratory Society International Congress, September 4–6, 2022 in Barcelona.
Disclosures
Jürgen Behr reports sponsorship or research funds from BMBF, DFG, and LMU-KUM, and has received payment or other financial remuneration from Actelion, AstraZeneca, Bayer, Biogen, Bristol Myers Squibb, Boehringer Ingelheim, F. Hoffmann-La Roche, Ltd., Ferrer, Galapagos, MSD, Novartis, and Promedior, Inc. (acquired by Roche in February 2020). Carlo Albera has served as a consultant for, and received speakers’ bureau fees from, Boehringer Ingelheim, F. Hoffmann-La Roche, and FibroGen. Ulrich Costabel reports personal fees as a consultant or speaker from AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, F. Hoffmann-La Roche, Ltd./Genentech, Inc., FibroGen, Galapagos, Novartis, and Pliant Therapeutics. Marilyn K. Glassberg receives research funding from, and has served on advisory boards for, Boehringer Ingelheim, Bristol Myers Squibb, Esperion Therapeutics, F. Hoffmann-La Roche, Ltd./Genentech, Inc., Redx Pharma, and Surrozen, and has served on a steering committee for Bellerophon. Harold Haller Jr has served as a consultant or speaker for Boehringer Ingelheim, Mylan Specialties, and United Therapeutics, and has served as an investigator for Boehringer Ingelheim and United Therapeutics. Steven D. Nathan has served as a consultant for, received speakers’ bureau fees from, and received research funding from Bellerophon, Boehringer Ingelheim, F. Hoffmann-La Roche, Ltd., Galapagos, and United Therapeutics. Wim A. Wuyts reports grants paid to his institution by Boehringer Ingelheim, F. Hoffman-La Roche, Ltd., and Galapagos. Lisa Lancaster has served as a consultant for AstraZeneca, Bellerophon Therapeutics, Daewoong Pharmaceutical, Daiichi Sankyo, DevPro Biopharma, F. Hoffmann-La Roche, Ltd., Nashville Biosciences, Oxygenium, Pieris Pharmaceuticals, Senwha Biosciences, United Therapeutics and Veracyte; has served as a researcher for Boehringer Ingelheim, Bridge Biosciences, Bristol Myers Squibb, Celgene, CSL Behring, Fibrogen, Galecto Biotech, Genentech, Inc., Horizon Therapeutics, NeRRe Therapeutics, Novartis, and Pliant Therapeutics; and has been involved in disease state education with Boehringer Ingelheim, United Therapeutics, and Veractye. Giuseppe Alvaro, Frank Gilberg, and Katerina Samara are employees of F. Hoffmann-La Roche, Ltd.
Compliance with Ethics Guidelines
No prospective data were collected during this post-hoc analysis; therefore, ethical approval was not required. However, during the original trials, all patients provided informed consent, the protocols were approved by the institutional review boards or ethics committees at each participating center, and the trials were conducted in accordance with the Declaration of Helsinki.
Data Availability
Qualified researchers may request access to individual patient level data through the clinical study data request platform (https://vivli.org/). Further details on Roche’s criteria for eligible studies are available here (https://vivli.org/members/ourmembers/). For further details on Roche’s Global Policy on the Sharing of Clinical Information and how to request access to related clinical study documents, see here (https://www.roche.com/research_and_development/who_we_are_how_we_work/clinical_trials/our_commitment_to_data_sharing.htm).
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Behr, J., Nathan, S.D., Costabel, U. et al. Efficacy and Safety of Pirfenidone in Advanced Versus Non-Advanced Idiopathic Pulmonary Fibrosis: Post-Hoc Analysis of Six Clinical Studies. Adv Ther 40, 3937–3955 (2023). https://doi.org/10.1007/s12325-023-02565-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02565-3