Abstract
Introduction
Multidrug regimens for glaucoma treatment often result in adherence issues due to inconvenience; these issues may be improved with fixed-dose combination drugs. The ophthalmic solution of ripasudil–brimonidine fixed-dose combination (RBFC; K-232) is the first treatment combining a Rho kinase inhibitor and an α2-adrenoceptor agonist, and has demonstrated ability to lower intraocular pressure (IOP) and have various effects on conjunctival hyperemia and corneal endothelial cell morphology. This study evaluates the pharmacologic effects of RBFC treatment versus its separate components—ripasudil or brimonidine.
Methods
This single-center, prospective, randomized, open-label, blinded endpoint study with 3 × 3 crossover design randomly assigned healthy adult men to three groups (1:1:1) to undergo consecutive 8-day administration phases (with drug-free intervals of at least 5 days). Subjects received twice-daily instillation of RBFC → ripasudil → brimonidine (group A), ripasudil → brimonidine → RBFC (group B), or brimonidine → RBFC → ripasudil (group C). Endpoints included change in IOP, severity of conjunctival hyperemia, corneal endothelial cell morphology, pupil diameter, and pharmacokinetics.
Results
Eighteen subjects were assigned in total (six to each group). RBFC significantly reduced IOP from baseline at 1 h post-instillation on days 1 and 8 (12.7 vs. 9.1 and 9.0 mmHg, respectively; both P < 0.001), and provided significantly greater IOP reductions than ripasudil or brimonidine at several time points. The most common adverse drug reaction with all three treatments was mild conjunctival hyperemia, which transiently increased in severity with RBFC or ripasudil, peaking at 15 min post-instillation. In post hoc analyses, conjunctival hyperemia scores were lower with RBFC than with ripasudil at several time points. Transient morphologic changes in corneal endothelial cells occurred for up to several hours with RBFC or ripasudil, but not with brimonidine. Pupil diameter did not change with RBFC.
Conclusion
RBFC significantly reduced IOP compared with each agent alone. A combination of each agent’s pharmacologic profile was observed in that of RBFC.
Trial Registration
Japan Registry of Clinical Trials; Registration No. jRCT2080225220.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out the study? |
The ripasudil–brimonidine fixed-dose combination (RBFC; K-232) is the first combination topical therapy containing ripasudil (a Rho kinase inhibitor) and brimonidine (an α2-adrenoceptor agonist), with demonstrated ability to lower intraocular pressure (IOP) among various other pharmacologic effects. |
This single-center, prospective, randomized, open-label, blinded endpoint, crossover study evaluated the pharmacologic effects of a ripasudil–brimonidine fixed-dose combination on IOP, conjunctival hyperemia, and corneal endothelial morphology in healthy volunteers compared with ripasudil or brimonidine alone. |
What was learned from the study? |
RBFC significantly reduced IOP from baseline (reductions were greater than with ripasudil and brimonidine alone); RBFC and ripasudil were associated with mild conjunctival hyperemia (scores were lower with RBFC than with ripasudil), and transient morphologic changes in corneal endothelial cells were also observed. |
RBFC had a stronger efficacy and similar safety profile compared with the single agents; a combination of each agent’s pharmacologic profile was observed in that of RBFC. |
Introduction
Glaucoma is characterized by functional and/or structural abnormalities in the optic nerve associated with intraocular pressure (IOP)-related changes [1], and is the leading cause of irreversible blindness worldwide [1, 2].
On the basis of randomized clinical trial data [3,4,5,6,7,8,9,10,11], the only treatment approach proven to preserve visual function and slow the rate of visual deterioration is the lowering of IOP [12,13,14]. International guidelines recommend initiating medical treatment with monotherapy, with the addition of a second drug considered when the first choice of monotherapy is well tolerated and lowers the IOP but the target IOP is not reached [12,13,14]. However, as multidrug regimens for the treatment of glaucoma pose several important clinical problems, such as poor adherence and inconvenience, fixed-dose combination therapy, when available, is preferable to instillation of two separate agents [12,13,14]. Indeed, approximately 40% of Japanese patients with newly diagnosed glaucoma discontinue topical therapy within the first year of treatment [15], with the medication regimen being one of the significant barriers to treatment compliance [16]. Further, real-world data indicate that progression of glaucoma is significantly reduced when treatment adherence is increased [17].
The ripasudil–brimonidine fixed-dose combination (RBFC; development code K-232) is the first combination topical therapy containing ripasudil hydrochloride hydrate (ripasudil 0.4%), a Rho-associated coiled-coil containing protein kinase (Rho kinase; ROCK) inhibitor, and brimonidine tartrate 0.1% (brimonidine), an α2-adrenoceptor agonist. The efficacy and safety of RBFC was previously demonstrated in two multicenter, randomized, phase 3 clinical trials, in which RBFC significantly reduced IOP in patients with primary open-angle glaucoma or ocular hypertension and IOP levels of at least 18 mmHg [18]. Ripasudil reduces IOP by increasing aqueous humor outflow via the conventional outflow pathway through modulation of the trabecular meshwork cell cytoskeleton, production of extracellular matrix, and Schlemm’s canal endothelial cell permeability [19,20,21,22]. Brimonidine is a potent agonist of α2-adrenergic receptors, which reduces IOP by suppressing aqueous humor production and promoting uveoscleral outflow [23, 24]. The pharmacologic actions of ROCK inhibitors include modulating the motility, contractility, adhesion, and shape of most cell types, which can lead to smooth muscle relaxation and morphological changes in corneal endothelial cells in addition to IOP reduction [19, 25, 26]. The actions of brimonidine include ciliary body vasoconstriction [27] and pupillary miosis [24].
In the current study, we evaluated the pharmacologic effects of the RBFC on IOP, conjunctival hyperemia, corneal endothelial cell morphology, pupil diameter, and pharmacokinetics compared with ripasudil or brimonidine alone in healthy volunteers.
Methods
Study Design
This was a single-center, prospective, randomized, open-label, blinded endpoint (PROBE) study, with a 3 × 3 crossover design.
The study was conducted at the Medical Corporation Heishinkai OPHAC Hospital in compliance with the principles of the Helsinki Declaration of 1964, and its later amendments and Good Clinical Practice guidelines, and the protocol was prospectively approved by the institutional review board of the participating site. Written informed consent was obtained from all subjects prior to study entry. This study is registered with the Japan Registry of Clinical Trials (Registration No. jRCT2080225220).
Subjects
The study enrolled healthy men, aged 20–35 years, who had an IOP of at least 15.0 mmHg in either eye (measured by noncontact tonometry) and a body mass index (BMI) of 17.6–26.4 kg/m2 at screening. Individuals were excluded if they had ocular diseases (except myopia, hyperopia, or astigmatism), best-corrected visual acuity of less than 20/25, Shaffer classification grade 0–2, difficulty in measuring IOP using a Goldmann applanation tonometer, corneal endothelial cell density of less than 2000 cells/mm2, cornea guttata, or corneal thickness of 620 μm or more in either eye. In addition, the use of drugs (including over-the-counter drugs), supplements, ophthalmic laser surgery, ophthalmic surgery, other nasolacrimal duct surgical procedures, and the wearing of contact lens were prohibited during the study period. Full exclusion criteria are provided in Table S1 in the Supplementary Material.
Randomization and Interventions
Eligible subjects who provided written informed consent were enrolled in administration phase 1 (Supplementary Material Fig. S1). Subjects underwent three consecutive administration phases (8 days of dosing followed by a drug-free period of at least 5 days) with RBFC, ripasudil, or brimonidine. An individual independent from the K-232 Clinical Study Group (see Appendix in the Supplementary Material) and sponsor used the permutation block method to randomly assign subjects (1:1:1) to one of three groups based on treatment order: group A received RBFC → ripasudil → brimonidine; group B received ripasudil → brimonidine → RBFC; and group C received brimonidine → RBFC → ripasudil (Supplementary Material Fig. S1). Treatment was masked throughout the study period for the investigator, sub-investigator, and sponsor. During each administration phase, one drop of the study drug was instilled into both eyes twice daily, in the morning (09:00) and evening (21:00) on each dosing day. Subjects were admitted to the hospital on the day prior to the first dose of study drug for each administration phase (day − 1) and discharged on day 9 after 8 days of twice-daily dosing (on day 8, morning dosing only) from day 1 (Supplementary Material Fig. S1).
Endpoints
The change from baseline in IOP (ΔIOP) with the RBFC compared with ripasudil or brimonidine was assessed.
Safety was assessed by the number and percentage of adverse events (AEs) and adverse drug reactions (ADRs), as well as the change in ophthalmologic parameters concerning the severity of conjunctival hyperemia, corneal endothelial cell morphology, and pupil diameter.
The pharmacokinetic properties of the RBFC were assessed after instillation by measuring the plasma concentrations, peak plasma concentrations (Cmax), area under the plasma concentration–time curve from time 0 to last observation (AUC0–τ), time to Cmax (tmax), and elimination half-life (t1/2) of unchanged ripasudil, its major metabolite (M1), and unchanged brimonidine.
Outcome Measures
IOP was measured in both eyes with a Goldmann applanation tonometer before and 1, 2, 4, 6, 9, and 12 h after the morning instillation on days 1 and 8.
The incidence of AEs and ADRs was collected for safety assessment.
The cornea, palpebral and bulbar conjunctivae, anterior chamber, lens, and iris were examined before and 15 min, 1, 2, 4, 6, 9, and 12 h after the morning instillation on days 1 and 8 using a slit lamp microscope. The palpebral and bulbar conjunctivae were evaluated for hyperemia using four grades: “–” = no findings or minimal findings but physiologic changes; “+” = several vasodilatations; “2+” = multiple vasodilatations or limbal vasodilatation; “3+” = vasodilatation in the whole conjunctiva (Supplementary Material Fig. S2) [28,29,30,31].
Assessments of corneal endothelial cell morphology and density and corneal thickness were performed before and 1, 2, 4, 6, 9, and 12 h after the morning instillation on days 1 and 8. Corneal endothelial cell morphology and density were examined by a noncontact specular microscope. Automated image capture and corneal cell count using the software associated with the device was performed. Corneal endothelial cell morphology was evaluated using noncontact specular microscopy and classified into one of four grades or as “undeterminable”: grade 0 = normal endothelial cell morphology (cells appear as white polygons with black borders) with no findings similar to guttae (corneal guttae findings are black irregularly shaped cells with white borders); grade 1 = many endothelial cells have clear borders, but at least 10% are partially blackened out with findings similar to guttae; grade 2 = endothelial cell borders are indistinct, with many having findings similar to guttae; grade 3 = endothelial cell borders cannot be identified; undeterminable = not applicable to any of grades 0–3 (Supplementary Material Fig. S3). Central corneal thickness was measured using Scheimpflug tomography.
Pupil diameter was measured using a Haab’s pupilometer before and 2, 4, 6, 9, and 12 h after morning instillation on days 1 and 8.
Visual acuity, fundoscopy, physiology (height, weight, BMI, blood pressure, heart rate, and temperature), and laboratory tests (hematologic, biochemical, and urinalysis) were also performed.
For the pharmacokinetic analysis, blood samples were collected before the morning instillation on days 1, 6, and 7. On day 8, blood samples were collected before the morning instillation and 5, 15, and 30 min, and 1, 1.5, 2, 3, 4, 5, 6, 9, and 12 h after the morning instillation.
Statistical Analysis
The sample size of 18 subjects (six in each group) was determined as a reasonable number of subjects to provide adequate pharmacokinetic information of the RBFC, ripasudil, and brimonidine in each administration phase. No hypothesis testing was performed for power calculation as this was not a confirmatory study.
Descriptive statistics were used to summarize the study outcomes. Continuous variables were presented as the number of subjects (percentage), mean ± standard deviation (SD), and median unless otherwise noted.
For the ΔIOP at each time point, the least squares (LS) mean and the LS mean ± standard error (SE) difference between the RBFC and ripasudil or brimonidine were determined using a marginal model that included the pre-dose IOP, preceding treatment, current study drug, and administration phase as fixed effects and had a compound symmetry (CS) covariance structure for subjects. The inferences for degrees of freedom were performed on the basis of the Kenward–Roger approach [32]. Change from baseline in conjunctival hyperemia grade in each administration phase (post hoc analysis) was evaluated using the same marginal model as for ΔIOP, with the preceding treatment, current study drug, and administration phase included as the fixed effects. Change from baseline in pupil diameter in each administration phase was evaluated by Wilcoxon signed rank test.
The two-sided significance level was 0.05 and the two-sided confidence interval (CI) of the safety endpoints was 95%. All statistical analyses were conducted at Kowa Company, Ltd. using SAS, version 9.4 (SAS Institute, Cary, NC, USA).
Results
Subject Disposition and Characteristics
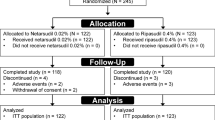
The study was conducted from June 13 to September 20, 2020; consent was obtained from 50 healthy male volunteers, and 18 subjects were assigned in total, six to each group (A, B, or C). All assigned subjects received at least one dose of the study drug, and 17 completed the study (Fig. 1). The subject demographics and characteristics are summarized in Table 1. At enrollment, subjects had a mean ± SD age of 26.2 ± 3.3 years and IOP of 14.1 ± 2.1 mmHg.
Disposition of subjects. aRipasudil–brimonidine fixed-dose combination → ripasudil → brimonidine. bRipasudil → brimonidine → ripasudil–brimonidine fixed-dose combination. cBrimonidine → ripasudil–brimonidine fixed-dose combination → ripasudil. dOne subject in group B had a fever on day 2 in administration phase 1 and a COVID-19 infection could not be ruled out; treatment was discontinued at the discretion of the investigator (ripasudil–brimonidine fixed-dose combination and brimonidine were not administered). COVID-19 coronavirus disease 2019
Change in IOP
With the RBFC, mean ± SD IOP decreased from 12.7 ± 2.4 mmHg at baseline to 9.1 ± 2.8 mmHg and 9.0 ± 2.0 mmHg at 1 h post-instillation on days 1 and 8, respectively, after which the IOP-lowering effect of the RBFC diminished over time (Fig. 2). A significantly greater ΔIOP was observed with RBFC versus ripasudil at 1 h post-instillation on day 1 (LS mean ± SE difference, − 1.0 ± 0.3 [P = 0.006]). RBFC also significantly reduced IOP compared with brimonidine at 1, 2, and 6 h post-instillation on day 1 (LS mean ± SE difference, − 2.0 ± 0.3 [P < 0.001], − 1.4 ± 0.4 [P = 0.006], and − 1.2 ± 0.5 [P = 0.024], respectively) and at 1 and 2 h post-instillation on day 8 (LS mean ± SE difference, − 1.6 ± 0.5 [P = 0.005] and − 1.2 ± 0.6 [P = 0.046], respectively; Fig. 2).
Change in intraocular pressure over time on days 1 and 8. The difference in the adjusted mean between ripasudil–brimonidine fixed-dose combination and ripasudil or brimonidine at each time point was determined using a marginal model. All values are presented as mean ± SD. *P < 0.05, **P < 0.01, ***P < 0.001 vs. baseline in each administration phase; ††P < 0.01 vs. ripasudil; ‡P < 0.05, ‡‡P < 0.01, ‡‡‡P < 0.001 vs. brimonidine. n = 18 at day 1 for ripasudil; n = 17 at days 1 and 8 for ripasudil–brimonidine fixed-dose combination and brimonidine and at day 8 for ripasudil. IOP intraocular pressure, n number of patients, SD standard deviation
Safety
AEs were observed in all 17/17 subjects (100.0%) during RBFC treatment, 18/18 (100.0%) with ripasudil, and 12/17 (70.6%) with brimonidine. ADRs were reported in 17/17 subjects (100.0%) with RBFC, 18/18 (100.0%) with ripasudil, and 10/17 (58.8%) with brimonidine.
Conjunctival hyperemia was the most common AE, occurring in 17/17 subjects (100.0%) with RBFC, 18/18 (100.0%) with ripasudil, and 10/17 (58.8%) with brimonidine, and the most common ADR, occurring in 100.0% of subjects with RBFC, 100.0% with ripasudil, and 8/17 (47.1%) with brimonidine (Supplementary Material Table S2). All cases of conjunctival hyperemia were mild and recovered without treatment, and most cases occurred transiently post-instillation, with the exception of one subject with ripasudil and two with brimonidine.
With the exception of conjunctival hyperemia and morphologic changes in corneal endothelial cells, no other clinically meaningful changes were observed in ophthalmic, physiological, or laboratory tests.
Conjunctival Hyperemia
Both palpebral and bulbar conjunctival hyperemia showed a transient increase in severity with RBFC or ripasudil, peaking at 15 min post-instillation and then decreasing over time. By visual inspection, palpebral conjunctival hyperemia was less severe and had a lower incidence with RBFC than with ripasudil at most time points (Fig. 3a), and bulbar conjunctival hyperemia was less severe and had lower incidence with RBFC than with ripasudil at 1 h post-instillation on day 1 (Fig. 3b).
Hyperemia scores for a palpebral and b bulbar conjunctival hyperemia after the first and the last instillations. The number of cases of conjunctival hyperemia is shown for each evaluation criteria (–, +, 2+, 3+; Supplementary Material Fig. S2). n = 18 at day 1 for ripasudil; n = 17 at days 1 and 8 for ripasudil–brimonidine fixed-dose combination and brimonidine and at day 8 for ripasudil. h hour, L left eye, n number of patients, R right eye
A post hoc analysis examined the differences in the effects on hyperemia between RBFC and ripasudil. This analysis found significant differences in the mean grade scores of both eyes for palpebral and bulbar conjunctival hyperemia between RBFC and ripasudil at some time points. The post hoc analysis indicated a carryover effect for palpebral conjunctival hyperemia; therefore, this endpoint was evaluated by t test to compare RBFC with ripasudil or brimonidine in administration phase 1. For palpebral conjunctival hyperemia, mean ± SD grade scores were significantly lower with RBFC versus ripasudil at 15 min (0.7 ± 0.8 vs. 1.4 ± 0.6, respectively) and 1 h (0.3 ± 0.4 vs. 0.9 ± 0.7, respectively) post-instillation on day 1 (LS mean ± SE difference, − 0.9 ± 0.4 [P = 0.028] and − 0.8 ± 0.3 [P = 0.011], respectively for group comparisons; Fig. 4a). For bulbar conjunctival hyperemia, mean ± SD grade scores were significantly lower with RBFC versus ripasudil at 1 h (0.4 ± 0.5 vs. 0.9 ± 0.5, respectively) post-instillation on day 1 (LS mean ± SE difference, − 0.6 ± 0.1 [P < 0.001]; Fig. 4b). Mean grade scores for palpebral and bulbar conjunctival hyperemia in both eyes were lower with brimonidine alone than with RBFC (Fig. 4a, b).
Change in clinical grade score for a palpebral conjunctival hyperemia and b bulbar conjunctival hyperemia. The change in score from baseline in each administration phase using quantified criteria for evaluation of conjunctival hyperemia (– = 0, + = 1, 2+ = 2, 3+ = 3; Supplementary Material Fig. S2) and were analyzed using a marginal model. Clinical grade scores for palpebral conjunctival hyperemia were evaluated in administration phase 1. All values are presented as mean ± SD. *P < 0.05, **P < 0.01, ***P < 0.001 vs. baseline in each administration phase; †P < 0.05, †††P < 0.001 vs. ripasudil; ‡P < 0.05, ‡‡‡P < 0.001 vs. brimonidine. n = 18 at day 1 for ripasudil; n = 17 at days 1 and 8 for ripasudil–brimonidine fixed-dose combination and brimonidine and at day 8 for ripasudil. SD standard deviation
Corneal Endothelial Cells
Changes in corneal endothelial cell morphology were observed after instillation of RBFC or ripasudil, which resolved to grade 0 in all subjects at 6 h post-instillation (Fig. 5). Some subjects developed grade 1 or 2 morphologic changes after instillation with RBFC or ripasudil, but none developed grade 3 changes. No morphologic changes were observed with brimonidine.
Morphologic changes in corneal endothelial cells after first and last instillations of study drug (grade evaluation). The evaluation criteria for corneal endothelial cell morphology were grade 0–3 and undeterminable (Supplementary Material Fig. S3), and the number of subjects in each grade are shown over time. h hour, L left eye, R right eye
The corneal endothelial cell density, which was automatically measured by the noncontact specular microscope, appeared to be reduced in cells with morphologic changes; however, cell density returned to pre-instillation values after the morphologic changes resolved. There were no clinically significant changes in corneal thickness and no remarkable findings on corneal examination.
Pupil Diameter
Mean pupil diameter decreased significantly from baseline after instillation with brimonidine at 2, 4, and 12 h post-instillation on day 1 and at 2, 4, and 6 h post-instillation on day 8. Similar reductions in mean pupil diameter were only observed with ripasudil at the first point post-instillation on day 1. No significant changes were observed with RBFC (Fig. 6). There were no clinically relevant changes with any of the three treatments, and no subjects developed abnormal light responses.
Change in pupil diameter after the first and the last instillations in the a left eye and b right eye. All values are presented as mean ± SD. *P < 0.05, **P < 0.01 vs. baseline in each administration phase (Wilcoxon signed-rank test). n = 18 at day 1 for ripasudil; n = 17 at days 1 and 8 for the ripasudil–brimonidine fixed-dose combination and brimonidine and at day 8 for ripasudil. SD standard deviation
Pharmacokinetics
After instillation of RBFC, the Cmax points of unchanged ripasudil and brimonidine (0.3461 ng/mL and 33.751 pg/mL, respectively) were reached at 0.083 h, and that of the ripasudil metabolite M1 (0.7379 ng/mL) was reached at 0.500 h. Plasma concentrations then rapidly decreased, with the t1/2 of unchanged ripasudil, M1, and unchanged brimonidine being 0.325, 3.096, and 1.903 h, respectively. The AUC0–τ of unchanged ripasudil, M1, and unchanged brimonidine was 0.1064 ng·h/mL, 2.4998 ng·h/mL, and 59.983 pg·h/mL, respectively (Supplementary Material Table S3).
Discussion
In this randomized, 3 × 3 crossover study of healthy male volunteers, the RBFC was associated with a significant decrease in mean IOP from baseline at 1 h post-instillation on days 1 and 8, decreasing from 12.7 to 9.1 mmHg and 9.0 mmHg, respectively, which is close to the episcleral venous pressure (8 mmHg) [33]. These reductions in IOP with RBFC were significantly greater than those observed with each individual agent (ripasudil or brimonidine). Previously, two phase 3 randomized clinical trials in patients with primary open-angle glaucoma or ocular hypertension demonstrated that RBFC had a greater IOP-lowering effect than ripasudil or brimonidine alone over 8 weeks of treatment [18]. These results suggest that the combination of ripasudil and brimonidine has an additive effect due to the three mechanisms of action, i.e., the enhancement of aqueous outflow via the conventional outflow [19,20,21,22] and uveoscleral outflow pathways, and the inhibition of aqueous humor production [23, 24].
Studies in healthy adults and patients with glaucoma have reported transient conjunctival hyperemia with ripasudil therapy that peaks 5–15 min after instillation [28,29,30, 34,35,36]. Given that one of the main actions of ROCK inhibitors is vascular smooth muscle relaxation [26], it has been suggested that the conjunctival hyperemia associated with ripasudil treatment is due to this pharmacologic effect, although an allergic response to ripasudil in some patients may cause conjunctival hyperemia. Topical brimonidine, on the other hand, reportedly causes vasoconstriction in the ciliary body [27], thus having the opposite effect on blood vessels to that of ripasudil, which may explain the slightly reduced conjunctival hyperemia observed with RBFC.
In a previous study in healthy subjects, Lee and colleagues found that the mean score for conjunctival hyperemia was significantly lower with combined instillation of ripasudil and brimonidine than with ripasudil alone at 2 h after instillation [37]. In this study, subjects received a single instillation of four patterns of ripasudil and brimonidine (no instillation, ripasudil alone, brimonidine alone, and a combination of ripasudil and brimonidine), with a gap of at least 1 week between instillations [37]. This suggests that, when used in combination with ripasudil, brimonidine suppresses ripasudil-associated conjunctival hyperemia. Similarly, our study found that both palpebral and bulbar conjunctival hyperemia transiently increased in severity with the RBFC and ripasudil, peaking at 15 min post-instillation and thereafter decreasing over time. The incidence, severity, and duration of palpebral and bulbar conjunctival hyperemia appeared to be lower with the RBFC than with ripasudil, similar to that observed in the previous study [37]. It is possible that the vasoconstrictive effects of brimonidine prevent the conjunctival hyperemia caused by the vasodilatory effects of ripasudil.
Ripasudil has been reported to cause transient changes in corneal endothelial cell morphology within a few hours after instillation in healthy volunteers [25] and in patients with glaucoma [38] that recovered 6 h after instillation. Our study also observed for the first time transient morphologic changes in corneal endothelial cells after RBFC instillation. Following instillation of RBFC, corneal endothelial cell density also appeared to be reduced for several hours, but returned to baseline levels over time. Because of the morphological impact of topical ROCK inhibitor therapy on cell boundaries of corneal endothelial cells, it is difficult to accurately evaluate cell density by a noncontact specular microscope with automated analysis. Therefore, it is important to be aware of the elapsed time post-instillation when evaluating corneal endothelial cell density.
Brimonidine has been shown to have a moderate miotic effect in healthy volunteers due to sympathetic α2-adrenergic receptor stimulation [39, 40]. On the other hand, ROCK inhibitors reportedly have a mydriatic effect in rabbits [41] and no effect on pupil diameter in healthy volunteers [42]. In the study by Lee et al., the pupil diameter significantly decreased after combined instillation of ripasudil and brimonidine or instillation of brimonidine alone, whereas no change in pupil diameter was found with ripasudil monotherapy [37]. In our study, mean pupil diameter was significantly decreased after brimonidine instillation at some time points; however, no significant changes in pupil diameter were observed following RBFC instillation. Hence, the miotic effect of RBFC was considered to be small.
Limitations
The main limitation of this study was its short duration (8 days) and that it was conducted in a small number of healthy adults. Therefore, a long-term study in a large population of patients with glaucoma or ocular hypertension is necessary to confirm the findings of this study. Moreover, this study was not placebo controlled and the comparisons were made between active drug groups.
Conclusion
The RBFC provided significantly greater reductions in IOP with 8 days of short-term instillation compared with each agent as monotherapy in healthy adult volunteers. Although RBFC instillation was associated with transient conjunctival hyperemia, which peaked at 15 min, the incidence and severity of hyperemia was lower than after instillation of ripasudil alone. Transient morphologic changes in corneal endothelial cell were observed for up to several hours after instillation, after which the morphology returned to normal. RBFC had no significant effect on pupil diameter, and the safety profile of RBFC was similar to that of the individual agents. Pharmacokinetic analyses demonstrated rapid elimination of unchanged ripasudil, ripasudil metabolite M1, and unchanged brimonidine from the plasma following topical instillation of RBFC.
References
Allison K, Patel D, Alabi O. Epidemiology of glaucoma: the past, present, and predictions for the future. Cureus. 2020;12:e11686.
Flaxman SR, Bourne RRA, Resnikoff S, et al. Global causes of blindness and distance vision impairment 1990–2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e1221–34.
Collaborative Normal-Tension Glaucoma Study Group. Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Am J Ophthalmol. 1998;126:487–97.
Collaborative Normal-Tension Glaucoma Study Group. The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. Am J Ophthalmol. 1998;126:498–505.
The AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130:429–40.
Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:701–13 (discussion 829–30).
Heijl A, Leske MC, Bengtsson B, et al. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002;120:1268–79.
Leske MC, Heijl A, Hussein M, et al. Factors for glaucoma progression and the effect of treatment: the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2003;121:48–56.
Bengtsson B, Leske MC, Hyman L, Heijl A, Early Manifest Glaucoma Trial Group. Fluctuation of intraocular pressure and glaucoma progression in the Early Manifest Glaucoma Trial. Ophthalmology. 2007;114:205–9.
Krupin T, Liebmann JM, Greenfield DS, Ritch R, Gardiner S, Low-Pressure Glaucoma Study Group. A randomized trial of brimonidine versus timolol in preserving visual function: results from the Low-Pressure Glaucoma Treatment Study. Am J Ophthalmol. 2011;151:671–81.
De Moraes CG, Liebmann JM, Greenfield DS, et al. Risk factors for visual field progression in the Low-Pressure Glaucoma Treatment Study. Am J Ophthalmol. 2012;154:702–11.
European Glaucoma Society. European Glaucoma Society terminology and guidelines for glaucoma, 4th edition—chapter 3: treatment principles and options. Supported by the EGS Foundation. Br J Ophthalmol. 2017;101:130–95.
Kiuchi Y, Inoue T, Shoji N, Nakamura M, Tanito M, Glaucoma Guideline Preparation Committee, Japan Glaucoma Society. The Japan Glaucoma Society guidelines for glaucoma, 5th edition. Jpn J Ophthalmol. 2023;67:189–254.
Gedde SJ, Vinod K, Wright MM, et al. Primary open-angle glaucoma Preferred Practice Pattern®. Ophthalmology. 2021;128:P71–150.
Kashiwagi K, Furuya T. Persistence with topical glaucoma therapy among newly diagnosed Japanese patients. Jpn J Ophthalmol. 2014;58:68–74.
Tsai JC, McClure CA, Ramos SE, Schlundt DG, Pichert JW. Compliance barriers in glaucoma: a systematic classification. J Glaucoma. 2003;12:393–8.
Shu YH, Wu J, Luong T, et al. Topical medication adherence and visual field progression in open-angle glaucoma: analysis of a large US health care system. J Glaucoma. 2021;30:1047–55.
Tanihara H, Yamamoto T, Aihara M, et al. Ripasudil–brimonidine fixed-dose combination vs ripasudil or brimonidine: two phase 3 randomized clinical trials. Am J Ophthalmol. 2023;248:35–44.
Kaneko Y, Ohta M, Inoue T, et al. Effects of K-115 (ripasudil), a novel ROCK inhibitor, on trabecular meshwork and Schlemm’s canal endothelial cells. Sci Rep. 2016;6:19640.
Moshirfar M, Parker L, Birdsong OC, et al. Use of Rho kinase inhibitors in ophthalmology: a review of the literature. Med Hypothesis Discov Innov Ophthalmol. 2018;7:101–11.
Honjo M, Tanihara H. Impact of the clinical use of ROCK inhibitor on the pathogenesis and treatment of glaucoma. Jpn J Ophthalmol. 2018;62:109–26.
Suzuki M, Suzuki Y, Komori R, et al. Aqueous column changes in the episcleral veins after the instillation of ripasudil versus latanoprost: a randomized, double-blind, crossover clinical trial. Sci Rep. 2022;12:15255.
Burke J, Kharlamb A, Shan T, et al. Adrenergic and imidazoline receptor-mediated responses to UK-14,304-18 (brimonidine) in rabbits and monkeys. A species difference. Ann N Y Acad Sci. 1995;763:78–95.
Burke J, Schwartz M. Preclinical evaluation of brimonidine. Surv Ophthalmol. 1996;41(Suppl 1):S9-18.
Nakagawa H, Koizumi N, Okumura N, Suganami H, Kinoshita S. Morphological changes of human corneal endothelial cells after Rho-associated kinase inhibitor eye drop (ripasudil) administration: a prospective open-label clinical study. PLoS ONE. 2015;10: e0136802.
Uehata M, Ishizaki T, Satoh H, et al. Calcium sensitization of smooth muscle mediated by a Rho-associated protein kinase in hypertension. Nature. 1997;389:990–4.
Reitsamer HA, Posey M, Kiel JW. Effects of a topical α2 adrenergic agonist on ciliary blood flow and aqueous production in rabbits. Exp Eye Res. 2006;82:405–15.
Tanihara H, Inoue T, Yamamoto T, Kuwayama Y, Abe H, Araie M. Phase 2 randomized clinical study of a Rho kinase inhibitor, K-115, in primary open-angle glaucoma and ocular hypertension. Am J Ophthalmol. 2013;156(731–6): e2.
Tanihara H, Inoue T, Yamamoto T, et al. Intra-ocular pressure-lowering effects of a Rho kinase inhibitor, ripasudil (K-115), over 24 hours in primary open-angle glaucoma and ocular hypertension: a randomized, open-label, crossover study. Acta Ophthalmol. 2015;93:e254–60.
Tanihara H, Inoue T, Yamamoto T, et al. Additive intraocular pressure-lowering effects of the Rho kinase inhibitor ripasudil (K-115) combined with timolol or latanoprost: a report of 2 randomized clinical trials. JAMA Ophthalmol. 2015;133:755–61.
Japanese Society of Ocular Allergology Committee on Guidelines. Japanese guideline for the management of allergic conjunctival diseases (3rd edition) [in Japanese]. https://www.nichigan.or.jp/Portals/0/resources/member/guideline/ACD3rd_chap2-2.pdf. Accessed 24 Jan 2023.
Kenward MG, Roger JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53:983–97.
Nilsson SF. The uveoscleral outflow routes. Eye. 1997;11:149–54.
Terao E, Nakakura S, Fujisawa Y, et al. Time course of conjunctival hyperemia induced by a Rho-kinase inhibitor anti-glaucoma eye drop: ripasudil 0.4%. Curr Eye Res. 2017;42:738–42.
Sakamoto E, Ishida W, Sumi T, et al. Evaluation of offset of conjunctival hyperemia induced by a Rho-kinase inhibitor; 0.4% ripasudil ophthalmic solution clinical trial. Sci Rep. 2019;9:3755.
Tanihara H, Inoue T, Yamamoto T, Kuwayama Y, Abe H, Araie M. Phase 1 clinical trials of a selective Rho kinase inhibitor, K-115. JAMA Ophthalmol. 2013;131:1288–95.
Lee J, Komizo T, Ono T, et al. The effects of single combined administration of brimonidine and ripasudil on intraocular pressure, pupil diameter, and hyperemia in healthy subjects. J Jpn Ophthalmol Soc. 2018;122:453–9.
Maruyama Y, Ikeda Y, Mori K, et al. Morphological change and recovery of corneal endothelial cells after Rho-associated protein kinase inhibitor eye-drop (ripasudil 0.4%) instillation. Br J Ophthalmol. 2021;105:169–73.
Shemesh G, Moisseiev E, Lazar M, Kesler A. Effect of brimonidine tartrate 0.10% ophthalmic solution on pupil diameter. J Cataract Refract Surg. 2011;37:486–9.
Besada E, Reed K, Najman P, Shechtman D, Hardigan P. Pupillometry study of brimonidine tartrate 0.2% and apraclonidine 0.5%. J Clin Pharmacol. 2011;51:1690–5.
Honjo M, Tanihara H, Inatani M, et al. Effects of Rho-associated protein kinase inhibitor Y-27632 on intraocular pressure and outflow facility. Invest Ophthalmol Vis Sci. 2001;42:137–44.
Satou T, Ishikawa H, Asakawa K, Goseki T, Shimizu K. Effects of ripasudil hydrochloride hydrate instillation on pupil dynamics. Curr Eye Res. 2017;42:54–7.
Acknowledgements
Funding
This study, editorial assistance for the preparation of this article, the Rapid Service Fee, and the Open Access Fee were funded by Kowa Company, Ltd., Japan. The clinical trial was conducted as part of the development of the ripasudil–brimonidine fixed-dose combination (development code K-232) by Kowa Company, Ltd., who took part in the planning and implementation of the trial, data collection, analysis and interpretation of data, and preparation, review, and approval of this manuscript. Kowa Company, Ltd. received brimonidine ophthalmic solution from Senju Pharmaceutical Co., Ltd., who also approved this manuscript. The recruitment of subjects and data collection was carried out by Kowa Company, Ltd., Japan.
Medical Writing, Editorial, and Other Assistance
Editorial assistance in the preparation of this article was provided by Yoshiko Okamoto, PhD, and Sarah Grieg, PhD, CMPP, of inScience Communications, Springer Healthcare, who provided assistance with the outline and first draft of this manuscript, respectively. Support for this assistance was funded by Kowa Company, Ltd., Japan.
Authorship
All named authors attest that they meet the four criteria of authorship, as defined by the International Committee of Medical Journal Editors (ICMJE). All authors have participated sufficiently in the work and accept public responsibility for the appropriate portions of the content, as well as accepting responsibility for the integrity of their co-authors.
Author Contributions
Conceptualization: Hidenobu Tanihara, Tetsuya Yamamoto, Makoto Aihara, Noriko Koizumi, Hiroomi Minami, Satoshi Kojima, Tomoyuki Isobe, Mizuho Kanazawa, and Hideki Suganami; Methodology: Hidenobu Tanihara, Tetsuya Yamamoto, Makoto Aihara, Noriko Koizumi, Hiroomi Minami, Satoshi Kojima, Tomoyuki Isobe, and Hideki Suganami; Data curation: Tomoyuki Isobe and Hideki Suganami; Formal analysis and investigation: Hidenobu Tanihara, Hiroomi Minami, Satoshi Kojima, and Hideki Suganami; Writing-original draft: Hidenobu Tanihara, Hiroomi Minami, and Mizuho Kanazawa; Writing-review and editing: Hidenobu Tanihara, Tetsuya Yamamoto, Makoto Aihara, Noriko Koizumi, Hiroomi Minami, Satoshi Kojima, Tomoyuki Isobe, Mizuho Kanazawa, and Hideki Suganami; Visualization: Hiroomi Minami and Mizuho Kanazawa; Supervision: Hidenobu Tanihara, Tetsuya Yamamoto, Makoto Aihara, Noriko Koizumi, Hiroomi Minami, and Satoshi Kojima; Project administration: Satoshi Kojima and Hideki Suganami. All authors read and approved the final manuscript.
Study Investigators
Yasuko Owada, Hiroshi Mikami, Michio Yagi, Hidetoshi Furuie, Tomoko Hayashibara, and Eriko Kawai (Medical Corporation Heishinkai OPHAC Hospital, Osaka, Osaka, Japan); Kiyoshi Kano (Fukushima Eye Clinic, Osaka, Osaka, Japan); Hisashi Mashimo (Japan Community Health care Organization Osaka Hospital, Osaka, Osaka, Japan); Makoto Ando (Ando Eye Clinic, Toyonaka, Osaka, Japan); and Masashi Takata (Hyogo Medical University, Nishinomiya, Hyogo, Japan).
Prior Presentation
This manuscript is based on work that was previously presented as an abstract at the 76th Annual Congress of Japan Clinical Ophthalmology (Oct 13–16, 2022, Tokyo, Japan).
Disclosures
Hidenobu Tanihara has received consulting fees, lecture fees, financial support and drugs from Kowa Company, Ltd. Tetsuya Yamamoto has received consulting fees from Alcon Japan, Allergan Japan, Kowa Company, Ltd., and Santen Pharmaceutical; board membership fees from Kowa Company, Ltd., Otsuka Pharmaceutical, Rohto Pharmaceutical, and Santen Pharmaceutical; financial support from Pfizer Japan, Otsuka Pharmaceutical, Santen Pharmaceutical, and Senju Pharmaceutical; and lecture fees from Johnson & Johnson, Kowa Company, Ltd., Pfizer Japan, Nitto Medic, Novartis, Otsuka Pharmaceutical, Santen Pharmaceutical, Senju Pharmaceutical, and Viatris. Makoto Aihara has received consulting fees from Santen Pharmaceutical, Senju Pharmaceutical, Alcon Japan, Pfizer Japan, Kowa Company, Ltd., Otsuka Pharmaceutical, Wakamoto Pharmaceutical, HOYA, Glaukos, IRIDEX, CREWT Medical Systems, Inc., and Astellas Pharmaceutical; financial support from Santen Pharmaceutical, Senju Pharmaceutical, Alcon Japan, Novartis, Pfizer Japan, Kowa Company, Ltd., Otsuka Pharmaceutical, Wakamoto Pharmaceutical, Johnson & Johnson, Glaukos, TOMEY, Ono Pharmaceutical, CREWT Medical Systems, Inc., and Sato Pharmaceutical; and lecture and travel fees and drugs from Santen Pharmaceutical, Senju Pharmaceutical, Alcon Japan, Novartis, Pfizer Japan, Kowa Company, Ltd., Otsuka Pharmaceutical, Johnson & Johnson, HOYA, Glaukos, TOMEY, IRIDEX, CREWT Medical Systems, Inc., CANON, Carl Zeiss Meditec, and Sato Pharmaceutical. Noriko Koizumi has received consulting fees from Kowa Company, Ltd., and M's Science Corporation; lecture fees from Kowa Company, Ltd., Senju Pharmaceutical, and Santen Pharmaceutical; and financial support from ActualEyes Inc. Hiroomi Minami, Satoshi Kojima, Tomoyuki Isobe, Mizuho Kanazawa, and Hideki Suganami are employees of Kowa Company, Ltd.
Compliance with Ethics Guidelines
The study was conducted at the Medical Corporation Heishinkai OPHAC Hospital in compliance with the principles of the Helsinki Declaration of 1964, and its later amendments and Good Clinical Practice guidelines, and the protocol was prospectively approved by the institutional review board of the participating site. Written informed consent was obtained from all subjects prior to study entry. This study is registered with the Japan Registry of Clinical Trials (Registration No. jRCT2080225220).
Data Availability
The data from this study are not available for sharing due to patient confidentiality and ownership by Kowa Company, Ltd., Japan.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
The members of the K-232 Clinical Study Group are listed in the Supplementary material.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Tanihara, H., Yamamoto, T., Aihara, M. et al. Crossover Randomized Study of Pharmacologic Effects of Ripasudil–Brimonidine Fixed-Dose Combination Versus Ripasudil or Brimonidine. Adv Ther 40, 3559–3573 (2023). https://doi.org/10.1007/s12325-023-02534-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02534-w