Abstract
Introduction
Immediate-release sodium oxybate (SXB) has been Food and Drug Administration (FDA)-approved to treat narcolepsy since 2002; in 2020, a mixed-salt oxybates formulation was also approved. Both are taken at bedtime with a second dose taken 2.5–4 h later. A third oxybate option, an investigational extended-release SXB, may soon be available. This study was undertaken to understand clinicians’ preferences between these 3 different oxybate treatments.
Methods
Clinicians in active clinical practice for 3–35 years and experience treating patients with narcolepsy were recruited. A 30-min web-based survey quantified narcolepsy disease-state attitudes, treatment perceptions, and satisfaction with oxybates on 9-point scales. A discrete choice experiment (DCE) of 12 choice sets, with 2 hypothetical treatment profiles in each, was used to capture clinician preferences about overall oxybate therapy preference, impact on patient quality of life (QoL), and patient anxiety/stress. Attributes associated with current therapies and those expected to be available in the near future were included in the design.
Results
The clinicians surveyed (n = 100) indicated that narcolepsy has a negative impact on patient QoL (mean rating, 7.7) and rated impact on QoL and treatment efficacy as the most important aspects of a narcolepsy treatment (mean rating, 7.3–7.7). Clinicians with experience prescribing oxybates had moderately high satisfaction with SXB and mixed-salt oxybates efficacy (mean ratings, 6.5–6.9) and safety (mean ratings, 6.1–6.7) and lower satisfaction with nightly dosing frequency (mean rating, 5.9 and 6.3, respectively). In the DCE, dosing frequency was the most important attribute driving overall product choice, patient QoL, and reducing patient anxiety/stress (relative attribute importance, 46.1, 41.7, and 44.0, respectively), with once nightly preferred over twice nightly.
Conclusion
Clinicians indicated a significantly higher preference for the once-at-bedtime dosing schedule versus twice nightly in selecting oxybate therapies overall and when aiming to improve patient QoL or reduce patient anxiety.
Plain Language Summary
Current medications for narcolepsy include immediate-release sodium oxybate and mixed-salt oxybates. People taking these oxybates for narcolepsy take 1 dose at bedtime and must wake up 2.5–4 h later for the second dose. An investigational sodium oxybate, designed as a single bedtime dose, has been tentatively approved by the US Food and Drug Administration. This study used a 30-min web-based survey to learn what clinicians think about narcolepsy and narcolepsy medicines. A discrete choice experiment was used to identify which properties of current/future oxybate medicines are most important in a narcolepsy treatment. In this exercise, relevant properties of current/future oxybate medicines were mixed and matched to create hypothetical medicine profiles. Clinicians selected from these profiles which medication they preferred overall, which would improve patient quality of life, and which would reduce patient anxiety when thinking about taking the treatment. Clinicians were moderately satisfied with the effectiveness and safety of current narcolepsy medications. They strongly preferred oxybate treatments with fewer nightly doses and agreed that waking up for the second oxybate dose causes stress for patients. In the discrete choice experiment, the number of doses each night was the product characteristic that had the biggest impact on clinicians picking a medicine for narcolepsy. This was true for overall medicine choice, choosing a medicine that would improve patient quality of life, and choosing one that would reduce patient anxiety/stress. If granted marketing approval, extended-release sodium oxybate will be a once-at-bedtime option that may overcome challenges with current oxybate therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Understanding clinician perspectives on the narcolepsy treatment landscape can help identify unmet needs. |
Data are limited on clinician perspectives about narcolepsy disease burden, treatment options, and oxybate therapy satisfaction. |
If a third oxybate option becomes available to treat narcolepsy, understanding quantified clinician-preferred oxybate treatment attributes is relevant for patient care. |
What was learned from the study? |
Overall, clinicians reported moderate to high satisfaction with immediate-release oxybate treatments; however, clinicians thought that twice-nightly dosing was a significant stressor for patients. |
The frequency of oxybate treatment dosing (once nightly over twice nightly) was the most important driver for overall product choice, improved patient quality of life, and reduced patient anxiety/stress. Other important attributes included adverse reactions, clinical efficacy, and sodium content. |
There is a burden for patients taking the second dose of immediate-release, twice-nightly oxybate due to the need to awaken in the middle of the night for the second dose. |
If granted marketing approval, the extended-release, once-nightly formulation of sodium oxybate (ON-SXB) may fulfill an unmet need for an oxybate treatment that does not require middle-of-the-night dosing. |
Introduction
Narcolepsy is a chronic neurological disorder characterized by excessive daytime sleepiness (EDS), cataplexy, disrupted nighttime sleep, sleep paralysis, and hypnagogic hallucinations [1, 2]. Individuals diagnosed with narcolepsy experience reduced quality of life (QoL) [3, 4] and negative socioeconomic outcomes. Symptoms of narcolepsy are managed by a combination of behavioral and pharmacologic therapies. Most individuals with narcolepsy will require lifelong medication to treat their symptoms [5,6,7].
Current US Food and Drug Administration (FDA)-approved treatments for cataplexy or EDS in narcolepsy are twice-nightly immediate-release oxybates [sodium oxybate (SXB) and calcium, magnesium, potassium, and sodium oxybates (mixed-salt oxybates) [8, 9]] and pitolisant [10]. Additional daytime medications for EDS [central nervous system (CNS) stimulants (e.g., dextroamphetamine, methylphenidate), modafinil, armodafinil, and solriamfetol] are also FDA-approved [11,12,13,14,15,16]. The only treatments taken at night are oxybates; owing to a short half-life and immediate-release formulations, patients must take 2 doses nightly: the first dose at bedtime and the second, middle-of-the-night dose 2.5–4 h later [8, 9, 17, 18]. In a 3-year follow-up study of 23 patients with narcolepsy type 1 (NT1) receiving immediate-release SXB, 56.5% (n = 13) discontinued treatment with the reasons for discontinuing treatment cited as the two nightly doses, insufficient compliance, mild or severe side effects, comorbidities, and pregnancy [19]. Peraita-Adrados et al. [19] concluded that SXB would be more acceptable with a better pharmacokinetic profile. Adherence is well documented to have an inverse relationship with dosing frequency in myriad therapeutic areas [20,21,22]. Moreover, patients with narcolepsy are often prone to disrupted nocturnal sleep; only oxybates have been shown to improve sleep, but immediate-release formulations require long-term middle-of-the-night awakening [23,24,25].
In a prior discrete choice experiment (DCE) comparing immediate-release and extended-release SXB, patients (n = 75) reported that the dosing frequency was the most critical attribute in overall oxybate treatment choice, medication adherence, and reduction of stress and anxiety associated with taking the treatment [26]. FT218 is an extended-release, once-nightly formulation of SXB (ON-SXB; LUMRYZ™; Avadel Pharmaceuticals, Chesterfield, MO, USA) that has received tentative approval from the FDA for the treatment of EDS or cataplexy in adults with narcolepsy [27, 28]. In the phase 3 REST-ON clinical trial, ON-SXB effectively improved narcolepsy symptoms, including EDS, cataplexy, global improvement as determined by the clinician, nocturnal arousals, sleep stage shifts, and overall sleep quality [23, 29].
The original DCE only included patients with narcolepsy [26]. Recognizing that people living with a chronic disease and clinicians prescribing treatment may have discordant perspectives, another DCE was undertaken, expanded to include clinicians as well as a larger group of patients (n = 120); results of the patient DCE will be reported elsewhere. Mixed-salt oxybates was added to this DCE but not included in the original DCE because it was not approved for narcolepsy treatment, and no published information was available at the time of the study. This study aimed to evaluate clinician perspectives on narcolepsy disease burden, treatment approaches, and overall satisfaction with available treatment options, and to characterize and quantify the preferred attributes of oxybate treatments for narcolepsy from the perspective clinicians who treat individuals with narcolepsy.
Methods
Study Design
A 30-min web-based survey was used to capture heterogeneous clinician perspectives toward current treatments for patients with narcolepsy. This study was reviewed and approved by Advarra (Columbia, MD, USA), an independent Institutional Review Board, and was performed in compliance with the principles of the 1964 Declaration of Helsinki. A healthcare provider recruitment agency was used to recruit clinicians, who received monetary compensation for their time. All participants in the study provided informed consent.
Participant Inclusion and Exclusion Criteria
Board-certified or board-eligible physicians with sleep medicine, neurology, pulmonology, and psychiatry specialties, as well as nurse practitioners and physician assistants practicing in sleep medicine, were eligible to participate in the study. Physicians with a primary specialty of pulmonology and nurse practitioners were required to have a subspecialty in sleep medicine. Clinicians must have had an active clinical practice for 3–35 years, spent ≥ 70% of professional time providing direct patient care (including surgeries), and managed ≥ 200 unique patients and ≥ 5 unique narcolepsy patients in the previous 1 month. Participants affiliated with a pharmaceutical or medical equipment manufacturer, contract research organization, national regulatory body (e.g., FDA), or market/advertising firm were excluded. Participants were also excluded if they were involved in market research on narcolepsy within 1 month before the study.
Survey
Surveys comprised 3 main sections: (1) demographic characteristics, (2) disease-state attitudes, and (3) treatment perceptions and satisfaction.
Demographic Characteristics
Clinicians were asked to respond to questions related to demographics and the clinical setting used to treat patients with narcolepsy.
Disease-State Attitudes
Clinician attitudes toward the disease state were evaluated based on their level of agreement regarding the treatment of narcolepsy on a scale from 1 (“strongly disagree”) to 9 (“strongly agree”). Clinicians were asked to select statements with which they would likely agree regarding compliance and dosing concerns.
Treatment Perceptions and Satisfaction
Perceived importance of various aspects of current narcolepsy treatment related to efficacy, safety/adverse reactions, and taking the medication were evaluated on a scale from 1 (“not at all important”) to 9 (“extremely important”). Data on current and previous use of available narcolepsy treatments were collected. Overall, treatment satisfaction was measured for each pharmacologic therapy used by clinicians to treat narcolepsy on a scale from 1 (“not at all satisfied”) to 9 (“extremely satisfied”). The level of satisfaction with SXB and mixed-salt oxybates was evaluated for efficacy, safety/adverse reactions, and aspects related to taking the medication on a scale from 1 (“not at all satisfied”) to 9 (“extremely satisfied”).
Discrete Choice Experiment
The DCE used an orthogonal design of 7 efficacy, safety, and administration attributes with 2–3 levels each, which varied across the choice sets. Two additional attributes were also included in the DCE study, “additional administration considerations” and “pharmacokinetics”; these were restricted by dose frequency (i.e., they were the same attributes for both immediate-release oxybates). The combined attributes and levels were based on the prescribing information for both twice-nightly oxybates (Xyrem® and Xywav™; Jazz Pharmaceuticals, Palo Alto, CA, USA) [8, 9], and on ON-SXB draft labeling and pivotal trial data [29].
A 12-choice-set experimental design with 2 hypothetical treatment profiles in each choice set was used; participants were asked to make 3 decisions for each choice set. Clinicians were asked to consider only their narcolepsy patients who have not been diagnosed with congestive heart failure, refractory uncontrolled hypertension, or renal failure when responding to the following:
-
1.
“Which product do you prefer overall for your patients with narcolepsy?”
-
2.
“Which of these products would you select if you wanted to improve your patient’s quality of life impacted by their narcolepsy?”
-
3.
“With which of these products do you expect your patient would experience less anxiety/stress when thinking about taking the treatment?”
Data Collection, Management, and Analysis
Data entry checks were implemented in the survey responses to ensure that participants did not enter invalid responses, and character limits were imposed on open-ended questions. The data were reviewed to ensure that the checks minimized potential data entry errors. In the overall sample, descriptive analyses were used to describe the treatment attribute preferences in narcolepsy. Differences were compared using t tests (mean) and chi-squared tests (proportion). A multivariable logit model was used for the DCE to investigate clinician preferences for narcolepsy treatment attributes. However, owing to the complexity of DCE studies, traditional statistical-power calculations do not offer accurate sample size estimates. As an insight validation check, the DCE data for overall product preference (“Which product do you prefer overall for your patients with narcolepsy?”) were also analyzed using a hierarchical Bayesian model. The mean coefficients derived from this model were used to compare clinician treatment preferences between high (≥ 20 patients) and low (< 20 patients) SXB prescribers.
Results
Demographic Characteristics
In total, 100 clinicians completed the survey; participants were predominantly male (68%) with an age range of 30 to ≥ 70 years old (Table 1). Of the total, 37% were sleep medicine specialists, 30% were neurologists, and 6% were advanced practice providers. Approximately half of the clinicians (56%) worked in private practices, followed by community hospitals (27%), and half had practices in urban locations (50%). Clinicians’ responses were based on patients not diagnosed with heart failure, refractory uncontrolled hypertension, and/or renal failure; approximately 11% of patients were not considered owing to having these conditions.
Survey Results
Disease-State Attitudes
Overall, clinicians reported that narcolepsy has a negative impact on patient QoL (mean rating, 7.7) and preferred to prescribe a treatment with lower dose frequency (mean rating, 7.7; Table 2). Waking up in the middle of the night to take the second dose of oxybate medication was reported as a notable stressor for patients (mean rating 7.5; Table 2). Additionally, clinicians were concerned about the risk of their patients falling when waking up at night (mean rating, 7.2). Clinicians were less concerned with taste and prescribing a controlled substance (mean rating, 6.2).
Clinicians expressed concerns about patient compliance with narcolepsy treatments that require 2 doses. When asked to select statements they were likely to agree with, 25% of clinicians were likely to agree that their patients have accidentally taken the second dose of their narcolepsy medication before the prescribed time period, and 34% reported hearing of accidental intake of the second dose in patients managed by other clinicians. More than half of the clinicians (53%) were likely to agree that they advise their patients to follow a specific routine to avoid taking the second dose of medication before the prescribed time. Only 12% of clinicians were likely to agree that taking the second dose within a shorter time would not cause issues for the patient.
Treatment Perceptions and Satisfaction
When evaluating the importance of various aspects of narcolepsy treatment, attributes related to efficacy had the highest mean ratings compared to safety/adverse reactions or aspects of taking the medication (Table 3). The most important efficacy attributes were “Impact on quality of life” (mean rating, 7.7) and “Ability to reduce the frequency and/or intensity of EDS” (mean importance rating, 7.6). Moreover, clinicians generally found attributes related to safety/adverse reactions important (mean importance rating, 7.0–7.2). Factors related to taking the medication were all rated lower than efficacy and safety.
The narcolepsy treatment most frequently prescribed by clinicians was modafinil (20%), followed by twice-nightly immediate-release oxybates [SXB (17%) and mixed-salt oxybates ([12%)] and armodafinil (15%; Fig. 1). Clinicians reported medium to high satisfaction levels with twice-nightly oxybates (SXB: mean rating, 6.8; mixed-salt oxybates: mean rating, 7.1; Fig. 2). The CNS stimulants dextroamphetamine and methylphenidate had mean satisfaction ratings of 5.8 and 5.7, respectively. Fluoxetine [30], used off-label for cataplexy, was associated with low treatment satisfaction (mean rating, 5.2).
Patient current and past use of existing narcolepsy treatments. Clinicians indicated the percentage of their patients with narcolepsy that have currently or ever used the specified treatment. The figure depicts treatments for which ≥ 10% of clinicians’ patients with narcolepsy ever used; other treatments were not specified
Clinician satisfaction rating with the most commonly used narcolepsy treatments. Clinicians rated their satisfaction with the pharmacologic treatments that they have previously or currently prescribed to their patients with narcolepsy on a scale from 1 (“not at all satisfied”) and 9 (“extremely satisfied”). Other treatments were not specified
When evaluating satisfaction with treatment efficacy of twice-nightly SXB and twice-nightly mixed-salt oxybates, both were highly rated for reducing frequency and/or intensity of EDS (mean rating, 6.9 vs. 6.9, respectively), cataplexy (mean rating, 6.7 vs. 6.8, respectively), sleep disturbances (mean rating, 6.7 vs. 6.8, respectively), and ability to remain asleep throughout the night (mean rating, 6.5 vs. 6.8, respectively; Table 4). Among twice-nightly oxybate formulations, clinicians were slightly less satisfied with safety/adverse reaction attributes for SXB (mean rating 6.1–6.3) than mixed-salt oxybates (mean rating, 6.4–6.7). Clinicians were less satisfied with dosing frequency (twice nightly vs. once nightly) for both twice-nightly oxybate treatments (SXB: mean rating, 5.9; mixed-salt oxybates: mean rating, 6.3) compared to treatment efficacy attributes.
Discrete Choice Experiment
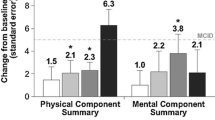
Although the baseline survey only included currently available treatments, the DCE introduced attributes of investigational extended-release SXB, as well as twice-nightly oxybate treatments (e.g., SXB and mixed-salt oxybates; Fig. 3). Once-nightly dosing was strongly preferred over a twice-nightly dosing schedule for overall product choice, patient QoL, and patient anxiety/stress (relative preference weight, + 43.6 vs. − 43.6, + 38.5 vs. − 38.5, + 41.6 vs. − 41.6, respectively; Fig. 4). In the DCE analysis, dosing frequency was the most important attribute of oxybate treatment in overall product choice, patient QoL, and patient anxiety/stress (relative attribute importance, 46.1, 41.7, 44.0, respectively; Fig. 5). Other important attributes for overall product choice were adverse reactions and sodium content (relative attribute importance, 19.7 and 18.6, respectively). Adverse reactions and sodium content were also associated with reducing patient anxiety/stress (relative attribute importance, 18.2 and 14.2, respectively). Following dosing frequency, adverse reactions and clinical efficacy were other important attributes associated with patient QoL (relative attribute importance, 21.5 and 18.6, respectively).
Discrete choice experiment grid. Attribute levels can be shown with any other combination of attribute levels. Levels are restricted by dosage (dose frequency), i.e., “sleep is not disturbed as patient does not need to wake up for a second dose” was always shown with “one dose at bedtime a night.” In each choice set, the same 9 attributes were viewed by the respondent, but with a different mix of level 1, level 2, and level 3 from each attribute that did not have restrictions. For example, clinician A may see the dosage from level 1, sodium content from level 2, administration from level 1, PK and administration from level 2, adverse reactions from level 3, and efficacy from level 2 as a hypothetical product profile, which is then paired to a different product profile, with attributes similarly mixed among the 3 levels. After making selections between the 2 profiles, clinician A would have seen 2 additional profiles until 12 choice sets had been evaluated
Relative preference weight across all 3 levels. A Relative preference weight for drivers of overall product choice. B Relative preference weight for product attributes associated with improving patient quality of life. C Relative preference weight for product attributes expected to reduce patient anxiety. Relative preference weight shown as Level 1 (blue) vs. Level 2 (green) vs. Level 3 (red). Attribute descriptions have been abbreviated for simplicity (see Fig. 3 for complete descriptions of attributes). The error bars around each relative preference weight denote lower and upper 95% CI
Oxybate treatment attribute preferences of clinicians. Relative importance of treatment attributes driving overall product choice, improving patient QoL, and reducing patient anxiety/stress when thinking of taking their medication. Dashed line represents the average attribute importance if all attributes were equally important, calculated as 100/number of attributes. Values above the dashed line indicate an attribute that is more important, whereas those below the line indicate an attribute that is less important. QoL quality of life
The hierarchical Bayesian model used to validate insights for overall product preference also resulted in comparable results, with dosing frequency being the most important attribute of oxybate treatment (mean relative attribute importance, 29.0), followed by adverse reactions (20.7) and sodium content (14.7). There were no statistically significant differences between the mean relative attribute importance for high versus low oxybate prescribers.
Discussion
These data confirm that clinicians recognize the negative impact of narcolepsy on patient QoL. Clinicians had moderate to high satisfaction with treatment efficacy for both twice-nightly immediate-release oxybate formulations: mixed-salt oxybates (mean rating, 7.1), and SXB (mean rating, 6.8). However, they were less satisfied with the dosing frequency; they preferred prescribing treatments with less-frequent doses, and they regarded the second dose of oxybate as a notable stressor for patients with either of these twice-nightly formulations.
For more than 20 years, the only FDA-approved treatment given at bedtime to treat symptoms of narcolepsy was immediate-release SXB [31]; a mixed-salt oxybates formulation, also immediate release, was FDA approved in 2020 [32]. An extended-release formulation of SXB has been developed and received FDA tentative approval [28]; if marketing approval is granted, clinicians will have 3 oxybate treatment options from which to choose. DCEs are recognized to be a useful tool to quantify preferences and show the relative importance of the attributes in the experiment [33,34,35,36,37]. In the current DCE analysis, once-nightly versus twice-nightly dosing frequency was the most important attribute to clinicians for overall product choice, improving patient QoL, and reducing patient anxiety/stress. The second highest rated attribute was adverse reactions, whereas the third was sodium content for overall medication choice and patient stress/anxiety. For patient QoL, the most important attributes were less-frequent dosing, adverse reactions, and clinical efficacy. Level 3, which describes the clinical efficacy of the mixed-salt oxybates, was scored lower by clinicians than the clinical efficacy for ON-SXB or twice-nightly sodium oxybate (Fig. 4). Mixed-salt oxybates was approved based on a pivotal trial design with randomized withdrawal [38], in which efficacy is shown by a worsening of symptom control after randomization to placebo, which may have made efficacy, excerpted from product labeling, more challenging to understand. Overall, these data demonstrate that clinicians have less concern about the sodium content of oxybates than the dosing regimen when considering patients appropriate for SXB therapy (e.g., those without congestive heart failure, refractory uncontrolled hypertension, and/or renal failure).
In the previous DCE study comparing 2 SXB medications, patients preferred once-nightly over twice-nightly dosing frequency for overall product choice, taking the medication exactly as directed, and patient anxiety/stress in thinking of taking the medication [26]. In concurrence with the results of the current study, patients strongly preferred a treatment taken fewer times (mean rating, 7.4), and considered the ability of the treatment to reduce EDS to be very important (mean rating, 8.6) [26]. Overall, findings from the current study demonstrated that clinicians and individuals diagnosed with narcolepsy had similar perspectives on the narcolepsy treatment landscape. An analysis was undertaken to understand if clinicians who have more experience in prescribing oxybates versus those who are less experienced would yield different results; in both groups, dosing frequency was the most important oxybate attribute driving treatment choice.
Narcolepsy symptoms such as cataplexy and EDS have been effectively treated with twice-nightly SXB for the last 20 years [24, 39,40,41]. However, concerns associated with twice-nightly oxybate treatments include patient challenges with waking up in the middle of the night for the second dose [42], dosing errors, and adherence to the dosing regimen [43]. Treatment adherence can be suboptimal [44] for some patients with narcolepsy; in the current study, clinicians moderately agreed (mean rating, 6.5) that patients do not adhere to their narcolepsy medication (i.e., they often miss the second dose). The second oxybate dose was further problematic, with 1 out of 4 clinicians reporting that their patients accidentally took the second dose before the prescribed time period, which may be associated with adverse events [43, 45]. A once-at-bedtime oxybate formulation may be an appealing treatment option because it may reduce patient stress and anxiety associated with taking the medication, reduce nocturnal disruption related to waking up for the second dose, and increase treatment benefits patients may experience from adhering to the medication dosing schedule.
Although a DCE attempts to simulate realistic decision-making scenarios, the treatment options presented are hypothetical and may not reflect real-world treatment considerations, such as patient insurance coverage, cost, travel requirements, and other work/life scheduling disruptions, among others. In addition, clinicians’ responses regarding hypothetical treatment on the DCE were subjective, particularly with regards to patient anxiety/stress. Modest numerical fluctuations, such as a lower level of satisfaction with the dosing frequency of twice nightly SXB (5.9) versus twice-nightly mixed-salt oxybates (6.3), may be due to the newness of the latter formulation at the time that the DCE was undertaken, as the dosing regimens are identical. Clinician responses were not differentiated between patients with NT1 or type 2 (NT2); in clinical trials of oxybates, patients were historically enrolled based upon undifferentiated narcolepsy or NT1 only. Patients with NT2 may be perceived as having less sleep disturbances; however, stratification by narcolepsy type (NT1 and NT2) in the pivotal trial of extended-release SXB has shown similar baseline levels of measures of disrupted nighttime sleep with both narcolepsy subtypes [46]. Clinicians were not asked to specifically consider other sleep disorder comorbidities [e.g., obstructive sleep apnea (OSA), periodic limb movement disorder (PLM), REM sleep behavior disorder (RBD)] of their patients. However, entry criteria for trials of oxybate treatments for narcolepsy have excluded participants with untreated/inadequately treated sleep-disordered breathing, OSA, or moderate to severe OSA [29, 38, 39, 47]. There is no evidence or plausible basis that extended-release SXB would impact OSA, PLM, or RBD differently than immediate-release, twice-nightly oxybates, and therefore we would not expect the presence of these comorbidities to alter the DCE results that indicate an overwhelming preference for a product dosed once nightly when a clinician selects oxybate for the desired treatment. Furthermore, the sample may not reflect the overall demographics of clinicians treating narcolepsy, although the sample included various specialties, including advanced practice providers, and was diverse in practice settings and years of experience.
Conclusions
The results from this study indicate that clinicians are relatively satisfied with the efficacy/safety of oxybates, but they recognize the challenges associated with middle-of-the-night dosing for the current immediate-release oxybates. Decreased dosing frequency (once-nightly over twice-nightly dosing) was shown to be the most important attribute when considering overall product choice, improving patient quality of life, and reducing their anxiety/stress. If marketing approval is provided, ON-SXB may be a favorable oxybate treatment option for clinicians and their patients.
References
Dauvilliers Y, Arnulf I, Mignot E. Narcolepsy with cataplexy. Lancet. 2007;369(9560):499–511.
Kornum BR, Knudsen S, Ollila HM, et al. Narcolepsy. Nat Rev Dis Primers. 2017;3(1):16100.
Ingravallo F, Gnucci V, Pizza F, et al. The burden of narcolepsy with cataplexy: how disease history and clinical features influence socio-economic outcomes. Sleep Med. 2012;13(10):1293–300.
Weaver TE, Mathias SD, Crosby RD, et al. Relationship between sleep efficacy endpoints and measures of functional status and health-related quality of life in participants with narcolepsy or obstructive sleep apnea treated for excessive daytime sleepiness. J Sleep Res. 2021;30(3): e13210.
Scammell TE. Narcolepsy. N Engl J Med. 2015;373(27):2654–62.
Thorpy MJ, Dauvilliers Y. Clinical and practical considerations in the pharmacologic management of narcolepsy. Sleep Med. 2015;16(1):9–18.
Thorpy MJ. Recently approved and upcoming treatments for narcolepsy. CNS Drugs. 2020;34(1):9–27.
XYREM (sodium oxybate oral solution, CIII). Full Prescribing Information. Palo Alto: Jazz Pharmaceuticals; 2022.
XYWAV (calcium, magnesium, potassium, and sodium oxybates oral colution, CIII). Full Prescribing Information. Palo Alto: Jazz Pharmaceuticals; 2022.
Wakix (pitolisant). Full Prescribing Information. Plymouth Meeting: Harmony Biosciences, LLC; 2019.
Maski K, Trotti LM, Kotagal S, et al. Treatment of central disorders of hypersomnolence: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2021;17(9):1881–93.
SUNOSI (solriamfetol). Full Prescribing Information. Palo Alto: Jazz Pharmaceuticals; 2019.
RITALIN (methylphenidate hydrochloride). Full Prescribing Information. East Hanover: Novartis Pharmaceuticals Corporation; 2019.
PROVIGIL (modafinil). Full Prescribing Information. North Wales: Teva Pharmaceuticals; 2015.
NUVIGIL (armodafinil). Full Prescribing Information. North Wales: Teva Pharmaceuticals, Inc.; 2017.
DEXEDRINE (dextroamphetamine sulfate). Full Prescribing Information. Horsham: Amedra Pharmaceuticals; 2013.
Barateau L, Lopez R, Dauvilliers Y. Treatment options for narcolepsy. CNS Drugs. 2016;30(5):369–79.
Franceschini C, Pizza F, Cavalli F, Plazzi G. A practical guide to the pharmacological and behavioral therapy of narcolepsy. Neurotherapeutics. 2021;18(1):6–19.
Peraita-Adrados R, Bellon JM, Lillo-Triguero L, Lopez-Esteban P, Medrano-Martinez P. Long-term follow-up on the effects of sodium oxybate on daytime sleepiness and sleep architecture in patients with narcolepsy type 1. Rev Neurol. 2023;76(2):35–40.
Coleman CI, Limone B, Sobieraj DM, et al. Dosing frequency and medication adherence in chronic disease. J Manag Care Pharm. 2012;18(7):527–39.
Weeda ER, Coleman CI, McHorney CA, Crivera C, Schein JR, Sobieraj DM. Impact of once- or twice-daily dosing frequency on adherence to chronic cardiovascular disease medications: a meta-regression analysis. Int J Cardiol. 2016;216:104–9.
Saini SD, Schoenfeld P, Kaulback K, Dubinsky MC. Effect of medication dosing frequency on adherence in chronic diseases. Am J Manag Care. 2009;15(6):e22–33.
Roth T, Dauvilliers Y, Thorpy MJ, et al. Effect of FT218, a once-nightly sodium oxybate formulation, on disrupted nighttime sleep in patients with narcolepsy: results from the randomized phase III REST-ON trial. CNS Drugs. 2022;36(4):377–87.
Black J, Pardi D, Hornfeldt CS, Inhaber N. The nightly use of sodium oxybate is associated with a reduction in nocturnal sleep disruption: a double-blind, placebo-controlled study in patients with narcolepsy. J Clin Sleep Med. 2010;6(6):596–602.
Morgenthaler TI, Kapur VK, Brown T, et al. Practice parameters for the treatment of narcolepsy and other hypersomnias of central origin. Sleep. 2007;30(12):1705–11.
Dubow J, Avidan AY, Corser B, Athavale A, Seiden D, Kushida C. Preferences for attributes of sodium oxybate treatment: a discrete choice experiment in patients with narcolepsy. Patient Prefer Adherence. 2022;16:937–47.
Seiden D, Tyler C, Dubow J. Pharmacokinetics of FT218, a once-nightly sodium oxybate formulation in healthy adults. Clin Ther. 2021;43(4):672.e1–672.e14.
Avadel Pharmaceuticals. Avadel Pharmaceuticals announces tentative approval of LUMRYZ™ (Sodium Oxybate) extended-release oral suspension. 2022. https://investors.avadel.com/news-releases/news-release-details/avadel-pharmaceuticals-announces-tentative-approval-lumryztm. Accessed 19 Jul 2022.
Kushida CA, Shapiro CM, Roth T, et al. Once-nightly sodium oxybate (FT218) demonstrated improvement of symptoms in a phase 3 randomized clinical trial in patients with narcolepsy. Sleep. 2022;45(6):zsab200.
PROZAC (fluoxetine). Full prescribing information. Indianapolis: Eli Lilly and Company Pharmaceuticals; 2017.
Jazz Pharmaceuticals. Jazz Pharmaceuticals, Inc. Release: Xyrem® receives FDA approval for the treatment of excessive daytime sleepiness in patients with narcolepsy. 2022. https://www.biospace.com/article/releases/jazz-pharmaceuticals-inc-release-xyrem-r-receives-fda-approval-for-the-treatment-of-excessive-daytime-sleepiness-in-patients-with-narcolepsy-/. Accessed 15 Jul 2022.
Jazz Pharmaceuticals. Jazz Pharmaceuticals Announces U.S. FDA approval of Xywav™ (calcium, magnesium, potassium, and sodium oxybates) oral solution for cataplexy or excessive daytime sleepiness associated with narcolepsy. 2020. http://investor.jazzpharma.com/news-releases/news-release-details/jazz-pharmaceuticals-announces-us-fda-approval-xywavtm-calcium. Accessed 15 Oct 2020.
Bridges JF, Hauber AB, Marshall D, et al. Conjoint analysis applications in health–a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14(4):403–13.
Heisen M, Baeten SA, Verheggen BG, et al. Patient and physician preferences for oral pharmacotherapy for overactive bladder: two discrete choice experiments. Curr Med Res Opin. 2016;32(4):787–96.
Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. BMJ. 2000;320(7248):1530–3.
van den Broek-Altenburg E, Atherly A. Using discrete choice experiments to measure preferences for hard to observe choice attributes to inform health policy decisions. Health Econ Rev. 2020;10(1):18.
Abiiro GA, Leppert G, Mbera GB, Robyn PJ, De Allegri M. Developing attributes and attribute-levels for a discrete choice experiment on micro health insurance in rural Malawi. BMC Health Serv Res. 2014;14:235.
Bogan RK, Thorpy MJ, Dauvilliers Y, et al. Efficacy and safety of calcium, magnesium, potassium, and sodium oxybates (lower-sodium oxybate [LXB]; JZP-258) in a placebo-controlled, double-blind, randomized withdrawal study in adults with narcolepsy with cataplexy. Sleep. 2021;44(3):zsaa206.
X. S. Xyrem Multicenter Study Group. A randomized, double blind, placebo-controlled multicenter trial comparing the effects of three doses of orally administered sodium oxybate with placebo for the treatment of narcolepsy. Sleep. 2002;25(1):42–9.
U. S. Xyrem Multicenter Study Group. Sodium oxybate demonstrates long-term efficacy for the treatment of cataplexy in patients with narcolepsy. Sleep Med. 2004;5(2):119–23.
Black J, Houghton WC. Sodium oxybate improves excessive daytime sleepiness in narcolepsy. Sleep. 2006;29(7):939–46.
Center for Drug Evaluation and Research (CDER). The Voice of the Patient: Narcolepsy. Silver Spring: US Food and Drug Administration; 2014.
Mayer G, Plazzi G, Iranzo A, et al. Long-term compliance, safety, and tolerability of sodium oxybate treatment in patients with narcolepsy type 1: a postauthorization, noninterventional surveillance study. Sleep. 2018;41(9):zsy128.
Pérez-Carbonell L, Lyons E, Gnoni V, et al. Adherence to wakefulness promoting medication in patients with narcolepsy. Sleep Med. 2020;70:50–4.
Gudeman J, Burroughs D. Evidence of accidental dosing errors with immediate-release sodium oxybate: data from the US Food and Drug Administration Adverse Event Reporting System. Drugs Real World Outcomes. 2023. [Epub ahead of print].
Dauvilliers Y, Roth T, Bogan R, et al. Efficacy of once-nightly sodium oxybate (ONSXB; FT218) by narcolepsy type: post-hoc analyses from the REST-ON trial. Ann Neurol. 2022;92(Suppl 29):S2222.
Xyrem International Study Group. A double-blind, placebo-controlled study demonstrates sodium oxybate is effective for the treatment of excessive daytime sleepiness in narcolepsy. J Clin Sleep Med. 2005;1(4):391–7.
Acknowledgements
The authors thank the survey participants. Trinity Life Sciences collected the data and performed statistical analysis, which was funded by Avadel Pharmaceuticals (Chesterfield, MO). David Seiden, MD, participated in conduct of the study and publication planning during his employment at Avadel Pharmaceuticals.
Funding
This study and the Rapid Service Fees for this publication were funded by Avadel Pharmaceuticals (Chesterfield, MO). Avadel was involved in the study design, in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Medical Writing and Editorial Assistance
Medical writing support was provided by Sejal Gunness, PhD, of The Curry Rockefeller Group, LLC (Tarrytown, NY), and was funded by Avadel Pharmaceuticals.
Author Contributions
Amod Athavale and Jennifer Gudeman made significant contributions to the study conception and design. Data collection and analysis were performed by Amod Athavale. Anne Marie Morse, Lois Krahn, Julie Flygare, Clete Kushida, Michael J. Thorpy, Amod Athavale and Jennifer Gudeman contributed to data interpretation and manuscript review and development. All authors also read and approved the final manuscript for submission.
Prior Presentation
Data from this study were originally presented at World Sleep in Rome, Italy, March 11–16, 2022.
Disclosures
Anne Marie Morse is a consultant for Harmony Biosciences and Jazz Pharmaceuticals; has served on advisory boards and speakers bureaus for Jazz Pharmaceuticals; has received grant funding from NIH/NIMH; has served as an advisor for Epilog, Neura Health, and the American Sleep Apnea Association; and was a REST-ON site PI for Avadel Pharmaceuticals. Lois Krahn is a consultant for and/or has served on advisory boards for Avadel Pharmaceuticals, Harmony Biosciences, and Takeda. Julie Flygare has received payment for consulting for Avadel Pharmaceuticals and Jazz Pharmaceuticals and speaking for Takeda Pharmaceuticals. Clete Kushida is a consultant for Avadel Pharmaceuticals, XW Pharma. Co., and Idorsia. Michael J. Thorpy is a consultant/advisory board member for Axsome, Balance Therapeutics, Eisai, Avadel Pharmaceuticals, Harmony Biosciences, Jazz Pharmaceuticals, NLS Pharmaceuticals, Suven Life Sciences Ltd, and Takeda Pharmaceutical Co., Ltd. Amod Athavale is an employee of Trinity Life Sciences. Jennifer Gudeman is an employee of Avadel Pharmaceuticals.
Compliance with Ethics Guidelines
This study was reviewed and approved by Advarra (Columbia, MD), an independent Institutional Review Board, and was performed in compliance with the principles of the Declaration of Helsinki. All participants in the study provided written informed consent. Trinity Partners, LLC (Waltham, MA) conducted clinician web-based cognitive interviews.
Data Availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Morse, A.M., Krahn, L., Flygare, J. et al. Clinician Preferences for Oxybate Treatment for Narcolepsy: Survey and Discrete Choice Experiment. Adv Ther 40, 3199–3216 (2023). https://doi.org/10.1007/s12325-023-02532-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02532-y