Abstract
Introduction
Lung cancer accounts for approximately 20% of all cancer-related deaths and for the loss of 3.2 million disability-adjusted life years (DALYs) annually across Europe. The present study investigated the productivity losses resulting from premature deaths due to lung cancer in four European countries.
Methods
The human capital approach (HCA) was used to estimate indirect cost of productivity losses due to premature death due to lung cancer (ICD-10 codes C33–34 malignant neoplasm of trachea, bronchus, and lung) in Belgium, the Netherlands, Norway, and Poland. Years of productive life lost (YPLL) and present value of future lost productivity (PVFLP) were calculated using national age-specific mortality, wages, and employment rates. Data were sourced from the World Health Organization, Eurostat, and the World Bank.
Results
In 2019, there were 41,468 lung cancer deaths in the included countries resulting in 59,246 YPLL and more than €981 million in productivity losses due to premature mortality. From 2010 to 2015, the PVFLP of lung cancer decreased by 14% in Belgium, 13% in the Netherlands, 33% in Norway, and 19% in Poland. From 2015 to 2019, the PVFLP of lung cancer decreased by 26% in Belgium, 27% in the Netherlands, 14% in Norway, and 38% in Poland.
Conclusion
The results from this study illustrate a decreasing trend in productivity costs of premature mortality due to lung cancer, as illustrated by the decreasing PVFLP between 2010 and 2019. This trend could be driven by a shift in the distribution of deaths towards older age groups due to advancements in the preventative and treatment landscape. These results provide an economic measure of the lung cancer burden which may assist decision-makers in allocating scarce resources amongst competing priorities in the included countries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Lung cancer has a high mortality rate (20% of cancer-related deaths) and a high patient burden (3.2 million disability-adjusted life years annually in Europe) which results in substantial productivity costs. |
What was learned from the study? |
The results from this study illustrate a decreasing trend in productivity costs of premature mortality due to lung cancer, as illustrated by the decreasing present value of future lost productivity (PVFLP) between 2010 and 2019. |
The overall reduction in productivity losses due to lung cancer deaths from 2010 to 2019 was 40% (approximately €644 million). |
The indirect costs of lung cancer still remain very high. |
Introduction
Malignant neoplasms of the lung describe cancers which form in the lung tissue, usually in the cells lining the air passage. Primary lung cancers are divided into two main groups: small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC), the latter accounting for 85% of lung tumors [1]. Although NSCLC is more common, SCLC is more aggressive and rapidly spreads to other organs [2]. According to the World Health Organization (WHO), lung cancer is the second most common type of cancer worldwide with 2.21 million new cases and 1.8 million deaths reported in 2020 [3]. A study on the European cancer burden estimated 480,000 new cases of lung cancer in 2020 with more than 380,000 deaths [4]. With 1.9 million cancer-related deaths in 2020, lung cancer deaths accounted for approximately 20% of these total deaths [4]. According to the European Cancer Information System (ECIS), lung cancer is expected to continue to be the leading cause of cancer deaths in Europe [5].
Since the 1950s, it has been widely accepted that smoking is strongly correlated with lung cancer [6]. Not only does smoking increase the risk of lung cancer but it has also been shown to negatively impact cancer treatment outcomes through reduced survival, greater symptom burden, and increased probability of recurrence [7]. While tobacco control and smoking cessation policies are helping to reduce the mortality rate of lung cancer, smoking prevalence patterns and tobacco control policies vary across countries in Europe. In 2019, the smoking rates were 14.6% in Belgium and Netherlands, 18.1% in Norway, and 10.2% in Poland [8].
The high premature mortality rate seen in lung cancer outlined above could result in substantial loss in productivity. In Europe alone, lost productivity costs due to premature cancer-related mortality were estimated to be more than €75 billion in 2014, with the average cost of lost productivity per premature cancer death in Europe estimated at €219,241 [9]. According to a 2018 study, premature death from lung cancer alone resulted in a productivity loss of €21.7 billion in 31 European countries [10].
Premature mortality costs should be an important part of the overall cancer burden to shape cancer control plans by policymakers. This is because crude and age-adjusted mortality rates alone do not reflect temporal changes in mortality, primarily as these measures fail to account for the fact that death rates rise sharply with age. This is particularly important with lung cancer deaths where there is a strong correlation between mortality and age with approximately 50% of deaths occurring in patients aged 75 and over [11].
Therefore, in this study, we investigated the productivity losses due to premature deaths due to lung cancer, and restricted our analysis to four countries of interest—Belgium, the Netherlands, Norway, and Poland—as these countries represent a reasonable spread across different regions within Europe to test the consistency of trends. Additionally, to our knowledge, this is the first study that evaluates quantitatively the cost of lost productivity in lung cancer in these countries. More specifically, this study investigated years of productive life lost (YPLL), years of life lost (YLL), and present value of future lost productivity (PVFLP) due to premature mortality from lung cancer using mortality data from three timepoints (2010, 2015, and 2019). YLL and YPLL are measures of premature mortality which are particularly important when measuring societal burden of early death in the population [12]. In contrast to mortality rates which simply measure the number of deaths in the population, YLL and YPLL give more weight to deaths occurring in the younger population and should be considered by decision-makers when allocating scarce healthcare resources [12]. For this reason, YLL and YPLL are increasingly favored over crude and age-adjusted death rates when establishing public health priorities [13, 14].
Within the model, productivity loss is defined as loss of earnings caused by premature mortality due to lung cancer as this could represent the economic loss to society. As such, the results from this analysis may be used to inform priority setting for cancer control by decision-makers.
Methods
Model Structure
The human capital approach (HCA) was used to estimate productivity losses due to premature death from lung cancer (ICD-10 code C33–34) in Belgium, the Netherlands, Norway, and Poland. These countries were studied as they cover a range of different populations in Europe. The model has three main outcomes of interest: YLL, YPLL, and PVFLP. The model calculated these outcomes independently for each country to ensure disaggregated results were available. To calculate these outcomes, the analysis adopted a lifetime horizon and a societal perspective. Direct costs, such as treatment costs, were not considered as patients only entered the model at death.
Data inputs for this model were taken from the WHO, Eurostat, and the World Bank. The model uses Eurostat mortality data of patients with lung cancer who died in a single year (2010, 2015, and 2019), stratified by age groups to reflect age groups in the Eurostat database: 0–14, 15–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, and 70+ years old [15]. When YLL was calculated, deaths across all age categories were considered; however, the years of life lost after the retirement age were not included in the YPLL and PVFLP calculations as productivity losses are not incurred after retirement. The default model retirement ages are country- and gender-specific. Although PVFLP calculations only considered patients with lung cancer before the retirement age, the total mortality was obtained by summing the number of deaths across all the age groups in the Eurostat database. For each cancer-related death, the model used national life expectancy estimates to calculate the YLL (Fig. 1).
Model schematic illustrating years of life lost (YLL), years of productive life lost (YPLL), and present value of future lost productivity (PVFLP) calculations in the model. This was adapted with permission from Bencina et al., Lost productivity due to head and neck cancer mortality in Hungary, Poland, and Romania [16]
Model Calculations
To calculate YLL, YPLL, and PVFLP, the model first estimated expected life years remaining and expected productive life years remaining using the following formulae:
where i = 1, 2, 3…I are population age groups used in the model.
Years of Life Lost
YLL is a measure of premature mortality that considers both the frequency of deaths and the age at which death occurs. In the model, YLL for the population is calculated by multiplying the number of deaths by the expected life years remaining for an individual using the following formula:
where i = 1, 2, 3…I are population age groups used in the model.
YPLL is an estimate of the average years a person would have been in productive employment (defined in this model as earning a wage) had they not died prematurely of lung cancer, aggregated for the whole population who died of lung cancer in 1 year. It was assumed that the population would be in employment until the retirement age (unemployment is also taken into account throughout life), after which all labor participation ceases. In the model, YPLL is calculated using the following formula:
where i = 1, 2, 3…I are population age groups (see Sect. “Epidemiological Inputs” for more detail).
Present Value of Future Lost Productivity
In the model, PVFLP was calculated in two steps. The model first calculated the PVFLP (per person) by multiplying the productive life years remaining by country-, age-, and gender-specific annual wages (productive life years refer to those in employment, i.e., before the retirement age). The model then calculated the PVFLP (per country) by multiplying the PVFLP (per person) by the age-specific mortality data.
PVFLP was corrected for country-level unemployment rates (using labor force participation as a measure of unemployment in the base case) to reflect the actual labor force characteristics. Annual earnings were discounted to obtain the present value of future earnings. A discount rate of 3% was applied annually to account for the depreciation in value of money further into the future. This is crucial to account for the impact of time on how economic inputs are valued in the model.
Per person PVFLP was estimated using the following formula:
where i = 1, 2, 3…I are population age groups.
Secondly, the per person PVFLP was multiplied by the age-specific mortality data to obtain a per country PVFLP estimate.
where i = 1, 2, 3…I are population age groups.
The model used data from three different years (2010, 2015, and 2019) and calculated the outcomes for each timepoint separately using the calculations outlined above.
Inputs and Assumptions
The model included epidemiological data to estimate YLL and YPLL and economic inputs to estimate PVFLP [15, 17,18,19,20].
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors. Ethics approval was not required for this study as all data was available in the public domain. The data sets analyzed during the current study are available in the EUROSTAT repository, https://protect-eu.mimecast.com/s/zd-2C2g5kcVPq78zI10t9g?domain=ec.europa.eu.
Epidemiological Inputs
Epidemiological inputs included mortality data and life expectancy. Mortality data were derived from the Eurostat database, stratified by country, age group, gender, and cancer subtype (refer to Supplementary Material Tables 2–4). Mortality was assumed to be uniformly distributed within each age group.
Life expectancy data were used to determine the remaining years of life left at the age patients die of lung cancer. Country and sex-specific life expectancy estimates were sourced from the World Bank [17, 18] (refer to Supplementary Material Tables 5–7).
Economic Inputs
The model used economic inputs including mean annual earnings and labor force participation to estimate the PVFLP. The most recent available data before 2020 was used to account for the impact that COVID-19 has had on the labor market and annual earnings. Mean annual earnings (refer to Supplementary Material Tables 8 and 9) were reported in euros and labor force participation rates (refer to Supplementary Material Table 11) as percentages. Costs that could have been incurred (e.g., future medical costs) were not considered as these are not associated with productivity losses.
Eurostat was used for mean annual earnings [15], gross domestic product (GDP) [21], unemployment rates [22], and labor force participation rates [20]. Mean annual earnings by age and sex were used in the base case and were estimated as an average of 29 statistical classifications of economic activities in the European Union (EU). Where the age categories in the Eurostat database did not correspond to the age categories used in the model, a weighted average was used to populate the model. For instance, for the 15–39 years age category, a weighted average of the “less than 30” and the “30–49 years” age categories from the Eurostat data were taken.
Although GDP provides a lower estimation of PVFLP, annual earnings were used in the base case as by definition GDP per capita is the GDP of a country divided its total population. As such, if GDP is used as a measure of income for the working population, it will be an underestimation of their true productivity, as it also includes those who are not working. So, while it is not the most conservative assumption in terms of PVFLP, it is a more realistic assumption. In the model, individuals in the 0–14 age category were assumed to have a wage of zero. This assumption was based on the age category splits in the Eurostat mortality data where the model assumes the youngest age category (0–14) are unemployed but does not try to assume further splits in employment status in the next age category (15–39).
Unemployment rates represent the percentage of people within the labor force who are currently unemployed whereas the labor force participation rate considers everyone in the labor force including those who are currently unemployed but actively seeking employment. Labor force participation rates were included in the PVFLP calculations in the base case as this provides a more conservative estimate of productivity losses when compared to using unemployment rates. Country-level labor force participation rates were 54% for Belgium, 65% for Netherlands, 64% for Norway, and 56% for Poland. Labor force participation was assumed to remain constant until the retirement age, as the data source used to populate the model assumes a constant labor force participation rate across the population. As such, these rates were only applied to the working-age population, assumed to be 15+ in this model.
Sensitivity Analysis and Scenario Analysis
Deterministic sensitivity analysis (DSA) was used to determine the sensitivity of results to variations in inputs, namely mortality, life expectancy, retirement age, measures of income, and measures of unemployment. The univariate DSA varied parameters by a default range of ± 10%.
Scenario analyses included the use of alternative input sources for key data values. GDP per capita by country [8] were used in place of annual earnings, and unemployment rate [8], in place of labor force participation. It was assumed that GDP per capita was equal across age groups whereas unemployment rates were age-specific.
Results
For deaths recorded in 2010, there was a total of 41,475 deaths, 429,456 YLL and 105,238 YPLL in 2010 mortality from lung cancer in the four countries investigated (Table 1). Total PVFLP in 2010 was €1,626,119,115 across these four countries.
In 2010, Norway had the lowest lung cancer mortality rate of the four countries. In 2010, Norway had a lung cancer crude mortality rate of 0.044%, compared to 0.062%, 0.061% and 0.059% in Belgium, Netherlands, and Poland respectively.
For 2015, there was a total of 42,708 deaths, 458,933 YLL and 84,322 YPLL in a single year’s mortality from lung cancer in the four countries investigated (Table 2). Total PVFLP in 2015 was €1,376,127,018 across these four countries.
In 2015, Norway had the lowest lung cancer mortality rate of the four countries. Norway had a lung cancer mortality rate of 0.042%, compared to 0.056%, 0.062%, and 0.063% in Belgium, Netherlands, and Poland, respectively.
A small reduction in the total number of deaths from lung cancer was observed in Belgium (6% reduction) and Norway (0.32% reduction) from 2010 to 2015. In 2015, Netherlands and Poland saw an increase in the number of lung cancer deaths compared to 2010 (although less than 10% in each country); however, population growth also occurred in all four countries. Despite this increase in the number of lung cancer deaths in Netherlands and Poland, YPLL decreased in each country compared to 2010 as the deaths were occurring in an older age group. The same trend was observed with PVFLP.
In 2019, there were 41,468 deaths, 452,413 YLL, and 59,246 YPLL in a single year’s mortality from lung cancer in the four countries investigated (Table 3). Total PVFLP in 2019 was €981,973,042 across these four countries.
Lung cancer deaths decreased in 2019 compared to 2015 across the four countries. In 2019, the lung cancer mortality rate was 0.051%, 0.059%, 0.040%, and 0.061% in Belgium, Netherlands, Norway, and Poland, respectively.
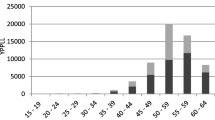
The results of the analysis illustrate an overall stable trend in the number of deaths and YLL; however, a decreasing trend in YPLL and PVFLP is observed over time. The decrease in YPLL and PVFLP is a result of the shift in population demographics and a greater proportion of deaths occurring in the older population who are retired (Supplementary Material Tables 2 and 4). The model estimated that the PVFLP associated with premature mortality due to lung cancer in the four countries in 1 year exceeded €1.6 billion in 2010 and €1.3 billion in 2015, while in 2019, productivity losses were estimated to be approximately €982 million.
Considering the total number of deaths across the four countries, this resulted in an average premature mortality cost per lung cancer-related death of €39,207, €32,222, and €23,680 in 2010, 2015, and 2019, respectively. There was therefore a 40% reduction in the PVFLP per lung cancer death from 2010 to 2019 (18% reduction from 2010 to 2015 and 27% reduction from 2015 to 2019). Of the three countries investigated, Poland had the highest YPLL across the three timepoints. Despite this, Netherlands reported the highest PVFLP across the three timepoints reflective of the higher annual earnings of the population (refer to Supplementary Material Tables 8 and 9).
As expected, the DSA (Fig. 2) showed that the PVFLP for lung cancer-related deaths was most sensitive to changes in the retirement age. This is because the decreasing trend in PVFLP observed is due to a large proportion of deaths occurring in the older population who are retired. This was observed across the three timepoints investigated. No change in results was observed when mortality or life expectancy were varied, for two reasons: when mortality is increased by a range of ± 10%, costs and deaths are also increased proportionally and therefore no impact is seen in results; secondly, even when life expectancy is increased by a range of ± 10%, it never drops below the retirement age and therefore it does not change the impact on the YPLL and hence the PVFLP. PVFLP estimates at the lower and upper values of the input parameters varied for the three timepoints are shown in Table 4.
A scenario analysis using GDP and unemployment rate resulted in a higher PVFLP compared to the base case model settings which used annual earnings and labor for participation to calculate PVFLP. In 2019, PVFLP across the four countries exceeded €1.4 billion when using the alternative inputs, as opposed to €982 million in the base case. Nonetheless, the same decreasing trend was still observed from 2010 to 2015 to 2019. Results by country in the base case compared to scenario analysis for the three timepoints are presented in the Table 5.
Discussion
On the basis of this analysis, a total of 41,475 deaths from lung cancer were reported in Belgium, Netherlands, Norway, and Poland in 2010. A small reduction in the total number of deaths was observed in 2019 compared to 2010 (an overall 3% decrease). Of the three countries, Poland reported the highest absolute number of total deaths across the three timepoints, reflective of its large population size; however, population-adjusted rates were similar across the four countries [23]. On the basis of these mortality data, 429,456 years of life across the four countries were lost in 2010 and 452,413 in 2019. Although the analysis showed an increase (approximately 5%) in YLL from 2010 to 2019 across the four countries, the trends observed per country were variable, whereby Belgium and Norway showed a decrease in YLL compared to Netherlands and Poland where an increase was observed. This is due to the nature of the country-specific mortality data used in the model and the shift in population demographics across the countries, including increased life expectancy in Netherlands and Poland compared to Belgium and Norway. Despite this small increase in YLL, a 44% reduction in YPLL was observed from 2010 to 2019 across the four countries. This reduction in YPLL was observed in each of the four countries included in the analysis with a 39%, 35%, 42%, and 50% reduction observed in Belgium, Netherlands, Norway, and Poland, respectively. This trend is observed because there is a shift in the distribution of deaths towards people dying of lung cancer at older ages, which are closer to retirement and therefore have fewer productive years remaining.
Consistent with the YPLL result, PVFLP showed a decreasing trend from 2010 to 2015 (15% reduction) and 2015 to 2019 (29% reduction). The overall reduction in productivity losses due to lung cancer deaths from 2010 to 2019 was 40%. Although there was a small increase in the YLL from 2010 to 2019, the considerable reduction in PVFLP is expected as life expectancy increased between these two timepoints and a higher number of deaths occurred above the retirement age. Given that PVFLP calculations give more weight to deaths occurring prior to the retirement age, PVFLP estimates were lower in 2019 compared to 2010. This decreasing trend in PVFLP was observed across each of the individual countries included in the analysis. From 2010 to 2015, productivity losses due to premature lung cancer mortality decreased by 27% in Belgium, 13% in the Netherlands, 31% in Norway, and 22% in Poland. From 2015 to 2019, productivity losses due to premature lung cancer mortality decreased by 26% in Belgium, 27% in the Netherlands, 15% in Norway, and 38% in Poland. For example, in Belgium (total population of 11.5 million people in 2019), on average from 2015 to 2019, yearly savings in indirect costs of lung cancer amounted to almost €17 million.
An observational analysis on lung cancer mortality in Europe and the USA between 2000 and 2017 demonstrated a decreasing trend in lung cancer mortality in male individuals whereas an increase in lung cancer mortality was observed in female individuals in many of the EU countries investigated. Despite lung cancer mortality rates being higher in male individuals, the death rates are decreasing at a faster rate in male compared to female individuals [24]. This could be partially driven by the larger reduction in smoking rates in male compared to female individuals, as smoking is the single most well established risk factor for lung cancer, accounting for 90% of cases [25]. Given these statistics, measures aimed at reducing tobacco consumption including optimizing tobacco control campaigns and the banning of flavored cigarettes could play a crucial role in reducing lung cancer mortality.
Improvements in diagnostic techniques and advancements in the treatment landscape could also be major contributing factors to the decreasing trend in PVFLP between 2010 and 2019 illustrated in this study. Analyses of 5-year survival rates have demonstrated improvements in many cancer types in Europe between 1995 and 2014 [26, 27]. This improvement has been seen alongside the approval of several treatment options for patients with lung cancer including approvals for the use of immunotherapy as a first-line treatment, particularly for the treatment of NSCLC [28]. In 2015, the Food and Drug Administration (FDA) approved the first immunotherapy for the treatment of NSCLC [28] and in 2018, for the treatment of SCLC. From 2015 to 2019, there was a 4–5% annual decrease in mortality rates in lung cancer in the USA [29]. The research indicates that this decline in mortality is due to the reduction in smoking rates and the advancements in diagnostic processes and treatment options [29]. These results align with the findings of our study where a small reduction in mortality rates was observed between 2015 and 2019 across the four countries investigated. As the improved patient outcomes observed with new treatments have an impact on productivity losses in both the short and longer term, it is important that these treatments are utilized effectively. Nonetheless, these new treatment modalities typically require additional healthcare spending, and so priority setting for healthcare spending is essential.
Across the three timepoints, the total PVFLP was considerably higher in the scenario analysis where unemployment rate and GDP were used as inputs, suggesting a conservative approach in the base case. Despite the conservative approach adopted, the lost productivity losses are still substantial thereby highlighting the high economic burden associated with lung cancer in these countries. These results are aligned with a study measuring societal burden of cancer in 2008 which estimated lost productivity of €17 billion due to premature lung cancer-related mortality [9].
Earlier studies utilizing a similar methodology have been conducted to illustrate the economic burden associated with cancer [9, 10]. According to one study, productivity losses amounted to €75 billion in 2008 in Europe alone [9]. A more recent study (2018) on the cost of cancers in Europe estimated a total productivity loss of €70 billion (€50 billion due to premature mortality and €20 billion due to morbidity) [30]. These results align with this study which suggests a decrease in the cost associated with premature cancer mortality with time.
A strength of this model was the approach to developing quantifiable evidence of the societal impact of lung cancer using reliable data sources. The model was based on publicly available data sets, including the WHO, the Eurostat database, and World Bank [31, 32]. Another strength of the model was the use of consistent data sources across the countries and timepoints to ensure internal validity. Additionally, the model uses gender-specific retirement ages and life expectancy inputs. This is particularly important in lung cancer, as there are several sex differences in lung cancer presentation between male and female individuals including a greater percentage of women in younger age groups. As the results from this analysis may be used to inform health policies in this area [33], it was important that these factors were considered when estimating productivity losses in the model.
Despite the robust modelling approach, there remain several assumptions in relation to the input parameters due to the complexity of real-world data. Although differences in inputs due to gender and age were incorporated in as much detail as the data allowed in practice, there may have been nuances which were not captured. For instance, the model does not account for the impact of sociodemographic factors on disease incidence and burden. Therefore, if lower income members of the population have a higher incidence of lung cancer, the model would have overestimated the overall burden of the disease as the model uses average earnings as a measure of income in the base case setting. Additionally, variations in lung cancer type which would likely have an impact on productivity losses were not accounted for in the model. A future study could employ this methodology to stratify the productivity losses by lung cancer subtype, e.g., SCLC and NSCLC, as this may provide greater specificity to specific population preventative policies.
This analysis did not model all costs associated with lung cancer. Firstly, direct costs to the healthcare system, such as drug or surgery costs, are not included, underestimating the overall economic burden of lung cancer. A cost analysis study on the economic burden of cancer across the EU showed that cancer cost amounted to €126 billion in 2009. Of this €126 billion, healthcare costs accounted for €51 billion (40%) [34]. Secondly, this analysis does not include productivity losses due to lung cancer morbidity. Morbidity in lung cancer has been shown to have a large impact on productivity, as patients experience long durations of sickness absence with only 45% of patients fully returning to work 2 years following diagnosis [35]. A study on the impact of cancer diagnosis on worker productivity found that 33% of patients with NSCLC and 15% of caregivers left the workforce post diagnosis [36]. Incorporating losses due to patient and caregiver absenteeism would have therefore increased the results in the long term. Despite this, the lost productivity estimates reported in this study are still high, illustrating the substantial economic burden resulting from lung cancer on both individuals and healthcare systems. It is therefore important that studies estimating the economic burden of lung cancer include both direct and indirect costs. Additionally, a wider approach to indirect costs that includes caregiver burden could be considered in future studies to ensure the overall burden of lung cancer is captured in the analysis to inform effective allocation and prioritization of limited healthcare budgets.
The model does not account for pension savings due to premature mortality as this raises ethical questions. Moreover, the model does not account for the fact that patients diagnosed with lung cancer could be replaced in the workforce, thereby overestimating the productivity losses resulting from the premature deaths.
Conclusions
The results from this study illustrate a decreasing trend in productivity costs of premature mortality due to lung cancer as illustrated by the PVFLP estimates between 2010 and 2019 in Belgium, the Netherlands, Norway, and Poland, highlighting the importance of policies and treatment advances to decrease premature lung cancer mortality, but that there is a long way to go. These results provide an economic measure of the lung cancer burden which may assist decision-makers in allocating scarce resources amongst competing priorities.
References
Paladini L, Veiga C, Cerqueira E, et al. Number needed to treat analysis applied to pembrolizumab plus chemotherapy for first-line treatment of non-squamous non-small cell lung cancer. J Med Econ. 2021. https://doi.org/10.1080/13696998.2021.1993864.
National Foundation for Cancer Research (NFCR). Small cell lung cancer vs. non-small cell lung cancer: what’s the difference? 2020. https://www.nfcr.org/blog/small-cell-lung-cancer-vs-non-small-cell-lung-cancer-whats-the-difference/. Accessed Aug 2022.
World Health Organization. Cancer. 2022. https://www.who.int/news-room/fact-sheets/detail/cancer. Accessed Aug 2022.
Dyba T, Randi G, Bray F, et al. The European cancer burden in 2020: incidence and mortality estimates for 40 countries and 25 major cancers. Eur J Cancer. 2021;157:308–47. https://doi.org/10.1016/j.ejca.2021.07.039.
JRC. ECIS—European Cancer Information System. 2020. https://ecis.jrc.ec.europa.eu. Accessed Aug 2022.
Wynder EL, Muscat JE. The changing epidemiology of smoking and lung cancer histology. Environ Health Perspect. 1995;103(Suppl 8):143–8. https://doi.org/10.1289/ehp.95103s8143.
Minnix JA, Karam-Hage M, Blalock JA, Cinciripini PM. The importance of incorporating smoking cessation into lung cancer screening. Transl Lung Cancer Res. 2018;7(3):272–80. https://doi.org/10.21037/tlcr.2018.05.03. (Erratum in Transl Lung Cancer Res. 2018 Sep;7(Suppl3):S303).
Eurostat. Daily smokers of cigarettes by sex, age and educational attainment level. 2019. https://ec.europa.eu/eurostat/databrowser/view/HLTH_EHIS_SK3E__custom_1485589/bookmark/table?lang=en&bookmarkId=0085fd51-e4cc-41ca-818c-4aa94e917bbd. Accessed Aug 2022.
Hanly P, Soerjomataram I, Sharp L. Measuring the societal burden of cancer: the cost of lost productivity due to premature cancer-related mortality in Europe. Int J Cancer. 2015;136(4):E136–45.
Ortega-Ortega M, Hanly P, Pearce A, Soerjomataram I, Sharp L. Paid and unpaid productivity losses due to premature mortality from cancer in Europe in 2018. Int J Cancer. 2022;150(4):580–93. https://doi.org/10.1002/ijc.33826.
Cancer Research UK. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/lung-cancer/mortality#heading-One. Accessed Aug 2022.
Burnet N, Jefferies S, Benson R, et al. Years of life lost (YLL) from cancer is an important measure of population burden—and should be considered when allocating research funds. Br J Cancer. 2005;92:241–5. https://doi.org/10.1038/sj.bjc.6602321.
Perloff JD, LeBailly SA, Kletke PR, Budetti PP, Connelly JP. Premature death in the United States: years of life lost and health priorities. J Public Health Policy. 1984;5(2):167–84.
Romeder JM, McWhinnie JR. Potential years of life lost between ages 1 and 70: an indicator of premature mortality for health planning. Int J Epidemiol. 1977;6(2):143–51. https://doi.org/10.1093/ije/6.2.143.
Eurostat. Causes of death—deaths by country of residence and occurrence mortality data (2010, 2015 and 2019). https://ec.europa.eu/eurostat/web/health/data/database. Accessed Aug 2022.
Bencina G, Chami N, Hughes R, Weston G, Golusiński PJ. Lost productivity due to head and neck cancer mortality in Hungary, Poland, and Romania. J Cancer Policy. 2022;13:100366. https://doi.org/10.1016/j.jcpo.2022.100366.
The World Bank. Life expectancy at birth, male (years). https://data.worldbank.org/indicator/SP.DYN.LE00.MA.IN. Accessed Aug 2022.
The World Bank. Life expectancy at birth, female (years). https://data.worldbank.org/indicator/SP.DYN.LE00.FE.IN. Accessed Aug 2022.
Eurostat. Mean annual earnings by sex, age and economic activity, 2018. https://ec.europa.eu/eurostat/databrowser/view/EARN_SES18_27__custom_1501377/default/table?lang=en. Accessed Aug 2022.
The World Bank. Labor force participation rate, national estimate (2019). https://data.worldbank.org/indicator/SL.TLF.CACT.FE.ZS.
Eurostat. Gross domestic product at market prices, 2019. https://ec.europa.eu/eurostat/web/products-datasets/-/tec00001. Accessed Aug 2022.
Eurostat. Unemployment rate by age, 2019. https://ec.europa.eu/eurostat/databrowser/view/tepsr_wc170/default/table?lang=en. Accessed Aug 2022.
The World Bank. Population total—Poland. https://data.worldbank.org/indicator/SP.POP.TOTL?end=2010&locations=PL. Accessed 1 Aug 2022.
Jani C, Marshall DC, Singh H, et al. Lung cancer mortality in Europe and the USA between 2000 and 2017: an observational analysis. ERJ Open Res. 2021;7(4):00311-2021. https://doi.org/10.1183/23120541.00311-2021.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33. https://doi.org/10.3322/caac.21654.
Allemani C, Matsuda T, Di Carlo V, et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population based registries in 71 countries. Lancet. 2018;391(10125):1023–75.
Allemani C, Weir HK, Carreira H, et al. Global surveillance of cancer survival 1995–2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2). Lancet. 2015;385(9972):977–1010.
Cancer Research Institute. Immunotherapy for lung cancer. 2021. https://www.cancerresearch.org/en-us/immunotherapy/cancer-types/lung-cancer. Accessed 1 Aug 2021.
American Society of Clinical Oncology (ASCO) Lung cancer—non-small cell: statistics. 2022. https://www.cancer.net/cancer-types/lung-cancer-non-small-cell/statistics. Accessed 1 Aug 2021.
Hofmarcher T, Lindgren P, Wilking N, Jönsson B. The cost of cancer in Europe 2018. Eur J Cancer. 2020;129:41–9. https://doi.org/10.1016/j.ejca.2020.01.011.
The World Bank. Life expectancy at birth, female (years). https://data.worldbank.org/indicator/SP.DYN.LE00.FE.IN. Accessed Aug 2022.
The World Bank. Life expectancy at birth, male (years). https://data.worldbank.org/indicator/SP.DYN.LE00.MA.IN. Accessed Aug 2022.
Rivera MP, Stover DE. Gender and lung cancer. Clin Chest Med. 2004;25(2):391–400. https://doi.org/10.1016/j.ccm.2004.01.006.
Luengo-Fernandez R, Leal J, Gray A, Sullivan R. Economic burden of cancer across the European Union: a population-based cost analysis. Lancet Oncol. 2013;14(12):1165–74. https://doi.org/10.1016/S1470-2045(13)70442-X.
Roelen CA, Koopmans PC, Groothoff JW, van der Klink JJ, Bültmann U. Sickness absence and full return to work after cancer: 2-year follow-up of register data for different cancer sites. Psychooncology. 2011;20(9):1001–6. https://doi.org/10.1002/pon.1820.
May SG, Chiu K, MacEwan JP, et al. The impact of a cancer diagnosis on worker productivity: results from a survey of cancer patients and caregivers. J Clin Oncol. 2020;38(29):144–144. https://doi.org/10.1200/JCO.2020.38.29_suppl.
Acknowledgements
Funding
This study and its publication, including the journal’s Rapid Service and Open Access Fees, was funded by Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA.
Author Contributions
Goran Bencina designed the study, Goran Bencina, Nour Chami, Robert Hughes and Georgie Weston conducted the analysis, Goran Bencina, Nour Chami, Robert Hughes, Georgie Weston, Carl Baxter, Stina Salomonsson and Ingel Demedts interpreted the results of the study and developed the manuscript.
Disclosures
Goran Bencina, Carl Baxter and Stina Salomonsson are employees of MSD subsidiaries of Merck & Co., Inc., Rahway, NJ, USA and may own stocks and/or stock options in Merck & Co., Inc., Rahway, NJ, USA.
Nour Chami, Robert Hughes and Georgie Weston are employees of Adelphi Values (PROVE), paid consultants to MSD.
Ingel Demedts reports receiving research grants from BMS, MSD, Roche, Boehringer Ingelheim, Astra Zeneca; reports being a paid consultant for BMS, MSD, Roche, Boehringer Ingelheim, Astra Zeneca, Takeda; and reports receiving speakers bureau honoraria from BMS, MSD, Roche, Boehringer, Astra Zeneca.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors. Ethics approval was not required for this study as all data was available in the public domain.
Data Availability
The data sets analyzed during the current study are available in the EUROSTAT repository, https://protect-eu.mimecast.com/s/zd-2C2g5kcVPq78zI10t9g?domain=ec.europa.eu.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Bencina, G., Chami, N., Hughes, R. et al. Indirect Costs Due to Lung Cancer-Related Premature Mortality in Four European Countries. Adv Ther 40, 3056–3069 (2023). https://doi.org/10.1007/s12325-023-02509-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02509-x