Abstract
Introduction
Prior studies have found considerable disparities in prevalence and outcomes for patients with peripheral arterial disease (PAD). This study compared rates of diagnostic testing, treatment patterns, and outcomes after diagnosis of PAD among commercially insured Black and White patients in the United States.
Methods
Optum’s de-identified Clinformatics® Data Mart Database (1/2016–6/2021) were used to identify Black and White patients with PAD; first PAD diagnosis was deemed study index date. Baseline demographics, markers of disease severity, and healthcare costs were compared between cohorts. Patterns of medical management and rates of major adverse limb events (MALE; including acute or chronic limb ischemia, lower-limb amputation) and cardiovascular (CV) events (stroke, myocardial infarction) during the available follow-up period were described. Outcomes were compared between cohorts using multinomial logistic regression models, Kaplan–Meier survival analysis, and Cox proportional hazards models.
Results
A total of 669,939 patients were identified, with 454,382 White patients and 96,162 Black patients. Black patients were younger on average (71.8 years vs. 74.2 years), but had higher comorbid burden, concomitant risk factors, and CV medication use at baseline. Prevalence of diagnostic testing, revascularization procedures, and medication use was numerically higher among Black patients. Black patients were also more likely than the White patients to receive medical therapy without a revascularization procedure [adjusted odds ratio with 95% confidence interval (CI) = 1.47 (1.44–1.49)]. However, Black patients with PAD had higher incidence of MALE and CV events than White patients [adjusted hazard ratio for composite event (95% CI) = 1.13, (1.11–1.15)]. Except myocardial infarction, the hazards of individual components of MALE and CV events were also significantly higher among Black patients with PAD.
Conclusions
Results of this real-world study suggest that Black patients with PAD have higher disease severity at the time of diagnosis and are at increased risk of experiencing adverse outcomes following diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? | |
Peripheral artery disease (PAD) is a common condition with significant racial variation in the rate of diagnosis, treatment, and outcomes. | |
To build upon the existing literature, we conducted a comprehensive, retrospective study evaluating trends in diagnostic testing, treatment patterns, and patient health outcomes after diagnosis of PAD between commercially insured Black and White patients in the United States. | |
What was learned from the study? | |
Compared to White patients, Black patients were observed to have higher disease severity leading up to the PAD diagnosis and increased risk of long-term cardiovascular and limb complications, despite increased diagnostic testing and medication use following PAD diagnosis. | |
The findings suggest that Black patients with PAD experience substantial disease burden under the current standard of care. Future interventions should be tailored to facilitate earlier diagnosis of PAD and to improve the standard of care for Black patients with PAD, which, in turn, could reduce disparate adverse outcomes following diagnosis. |
Introduction
Peripheral artery disease (PAD) is a common condition in which vessels of the lower limb are narrowed due to atherosclerotic occlusion. In the United States (US), approximately 8.5 million people live with PAD [1]. The disease is associated with elevated risks of major adverse cardiovascular (CV) events, including stroke, myocardial infarction (MI), or CV death; and major adverse limb events (MALE), including acute limb ischemia (ALI), chronic limb threatening ischemia, and limb amputation [2, 3].
Management of PAD is critical to minimizing future risk of adverse CV events, and may involve pharmacologic options and/or revascularization therapies [4, 5]. Pharmacologic treatment includes antiplatelet agents (e.g., aspirin) and anticoagulant agents (e.g., vitamin K antagonist), or a combination of the two (i.e., dual pathway inhibition). In recent years, direct-acting oral anticoagulants, such as direct Factor Xa inhibitor, have also emerged as promising options [6,7,8,9]. As PAD progresses, endovascular or surgical revascularization may be required [4, 5].
Recent studies have shown significant differences in the rate of PAD diagnosis, treatment, and outcomes by race. Matsushita and colleagues found that the lifetime risk of PAD was significantly greater among Black Americans than those with White or Hispanic ethnicity [10]. Moreover, Soden and colleagues found that Black Americans with PAD interventions have more severe disease at the time of initial major vascular operation compared to non-Hispanic White Americans [11]. Studies have also found that Black Americans are less likely to be offered and to undergo revascularization procedures to salvage the effected limb and avoid amputation [12,13,14,15].
In addition, studies have documented that Black patients with PAD have worse clinical outcomes than White patients with PAD. For example, a study by Chen and colleagues reported that, compared with non-Hispanic White Americans, Black patients with PAD had nearly 50% higher odds of PAD with chronic limb ischemia (CLI), and over 70% higher odds of major limb amputation [16]. Fanaroff et al. similarly reported that markers of lower socioeconomic status and Black race were associated with higher rates of major lower extremity amputation [17]. Black patients with PAD may also be at an even greater risk of adverse CV events due to atherosclerotic occlusion [18]. A prospective study of patients with stable CAD found that symptomatic PAD was associated with a 70% increased risk of subsequent CV events, after adjustment for traditional risk factors [19].
The current study builds upon the existing literature by conducting a comprehensive evaluation of the trends in diagnostic testing, treatment patterns, and outcomes after diagnosis of PAD between commercially insured Black and White patients in the US.
Methods
Data Source
Optum’s de-identified Clinformatics® Data Mart (CDM) Database, spanning from January 1, 2016 to June 30, 2021, was used to meet the study objectives. Optum CDM includes 12–14 million annual covered lives in all census regions in the United States. The claims data contain more than 36 months of historical data on patient demographics, dates of eligibility and death, claims for inpatient and outpatient (OP) visits, costs of services, and laboratory tests and results. Race and ethnicity are reported based on a propriety algorithm derived using member geographic location and name. The Optum CDM data also include information on patients’ socio-economic characteristics, such as education level, federal poverty status, home ownership, household income, net worth, and occupation.
All patient data are de-identified and comply with the requirements of the Health Insurance Portability and Accountability Act. Because the current study relied exclusively on de-identified patient records and did not involve the collection, use, or dissemination of individually identifiable data, institutional review board approval was not necessary. Permission to access and use the data was granted by Optum.
Study Design and Population
A retrospective study design was used to evaluate and compare treatment patterns, diagnostic testing, revascularization procedures, and adverse outcomes among Black and White patients with PAD (Fig. 1). Patients were included if they had ≥ 2 medical visits with a diagnosis of PAD (the first visit was defined as the index date), ≥ 6 months of continuous health plan enrollment before the index date (i.e., baseline period), and ≥ 1 months of continuous health plan enrollment after the index date (i.e., follow-up period). Patients were also required to be ≥ 18 years of age and have complete information on race and geographic region. Patients were excluded if they had ≥ 1 diagnosis for major CV events (i.e., all-cause stroke, MI, ALI, and CLI), or lower limb amputation within 1 month prior to the index date, or ≥ 1 dispensing for oral anticoagulant therapy during the baseline period. Patients who met the selection criteria were stratified into mutually exclusive cohorts based on their race (Black or White race).
Study Outcomes
Demographics, comorbidities, healthcare resource use (HRU), healthcare costs, and severity profile at baseline [as inferred by the composite of the Quan–Charlson comorbidity index (Quan-CCI), PAD diagnosis with ALI, CLI, both, or neither at the index date, as well as the prevalence of PAD risk factors, baseline CV-related procedures, medication use, and level of diagnostic testing; with higher indices and prevalence indicating more severe disease] were reported. The specific outcomes evaluated were patterns of care and medical management before and after diagnosis, lower-limb amputation (overall and by high and low amputation), MALE (comprising of ALI, CLI, and lower-limb amputation), and CV events (MI and all-cause stroke) following the PAD diagnosis. Each study outcome was compared between Black and White patients.
Statistical Analysis
Differences in baseline characteristics between Black and White patients were assessed using standardized differences, with a standardized difference of less than 10% considered not clinically relevant. Descriptive statistics included mean, standard deviation (SD), and median values for continuous variables, and relative frequencies and proportions for categorical variables.
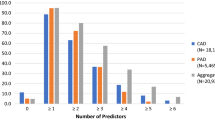
Medical management at 3-, 6-, 9-, and 12-month timepoints following the diagnosis of PAD was described to understand any changes in treatment patterns leading up to key outcomes of interest. Specifically, proportions of patients with PAD treated with prescription medications, revascularization, or both were described and compared using Chi-square tests. In addition, to minimize potential confounding, multivariable models were used to assess the statistical significance of differences in outcomes between cohorts, adjusting for age, gender, geographic region, Quan-CCI, PAD diagnosis type, and the number of concomitant comorbidities and risk factors for PAD. Proportions of patients receiving revascularization or medications were compared using multinomial logistic regression models, and odds ratios (ORs) with 95% confidence interval (CI) were reported. The frequency and type of diagnosis testing performed were also described.
Frequency and rates of revascularization, MALE, and CV events during the follow-up period were reported. Rates were calculated as the number of events divided by the patient-years of observation and reported per 100 person-years. For each outcome, time to first event was assessed with Kaplan–Meier survival analysis. Patients who did not experience the event were censored at the end of their observation period. Time to first event was also modeled with multivariable Cox proportional hazards regression. The models adjusted for differences in age, gender, geographic region, Quan-CCI, PAD diagnosis type, and the number of concomitant comorbidities and risk factors for PAD. The probability of each outcome was expressed as a hazard ratio (HR), accompanied by 95% CI and P values to assess the statistical significance of the results.
Results
Study Population
After applying all eligibility criteria, 669,939 patients were included in the study population (Fig. 2). Patients were further stratified by race, with 454,382 (68%) categorized as White and 96,162 (14%) categorized as Black.
Baseline Patient Characteristics
Mean age at PAD diagnosis was lower among Black patients relative to White patients (71.8 vs. 74.2 years; standardized difference = 22.2%), and a higher proportion of Black patients were female (61.3% vs. 53.3%; standardized difference = 15.7%; Table 1). Socioeconomic factors, including education level (bachelor’s degree or higher: 4.1% vs. 15.2%; standardized difference = 37.5%) and household income (< $40 K: 54.6% vs. 31.7%; standardized difference = 46.4%) were largely different between Black and White patients, respectively. Mean Quan-CCI was higher among Black patients relative to White patients (1.7 vs. 1.5; standardized difference = 10.1%). The prevalence of several comorbidities and risk factors for PAD were also higher among Black patients, including hypertension, diabetes, renal failure or end stage renal disease (eGFR < 60 mL/min), and obesity (standardized difference > 10%). Moreover, the proportion of patients with three or more concomitant comorbidities and risk factors for PAD was higher among Black patients relative to White patients (44.6% vs. 37.3%; standardized difference = 14.8%). Use of CV-related medications was also higher among Black patients relative to White patients; with some of the largest differences observed in the use of antihypertensives and other CV agents (standardized difference = 27.3% and 30.7%, respectively). The most common CV procedures during the baseline period were cardiography and echocardiography procedures for both Black and White patients (39.4% and 37.3%, respectively), with similar prevalence of CV procedures between both cohorts. Prevalence of other selected procedures and diagnostic testing were low during the baseline period and largely similar between cohorts, with only dialysis procedures being more prevalent among Black patients relative to White patients (2.6% vs. 0.9%; standardized difference = 12.9%). Likewise, baseline HRU and costs were generally similar between both cohorts.
Medical Management
While prevalence of revascularization procedures was generally low across both cohorts and at all time intervals (range 0.6–3.4%), Black patients with PAD had a significantly higher prevalence of revascularization procedures relative to White patients across all time intervals (Table 2; P < 0.05). Diagnostic testing with vascular ultrasound, ankle brachial index, angiography, or aortography was numerically more prevalent among Black patients relative to White patients across nearly all time intervals. A substantial decrease in prevalence of diagnostic testing with vascular ultrasound, ankle brachial index, or angiography was observed across both cohorts in the 3–6 months following the PAD diagnosis (White patients: 1.2–2.2%; Black patients: 1.5–2.7%) relative to the 0–3 months prior (White patients: 5.0–15.7%; Black patients: 5.6–19.6%). The prevalence of diagnostic testing continued to decrease in the 6–9 and 9–12 months following the initial PAD diagnosis in both cohorts. Medication use was significantly higher among Black patients relative to White patients across all time intervals (P < 0.05), and prevalence remained generally consistent across all time intervals for both cohorts.
After adjusting for baseline differences, Black patients with PAD had significantly higher odds of being treated with only medications [OR (95% CI) = 1.47 (1.44–1.49); P < 0.001; Table 3] compared to White patients with PAD. Moreover, Black patients with PAD had double the odds of high amputations compared to White patients with PAD [OR (95% CI) = 2.01 (1.89–2.13); P < 0.001], significantly higher odds of low amputations [OR (95% CI) = 1.35 (1.28–1.43); P < 0.001], and numerically higher high-to-low amputation ratio (0.94 and 0.63, respectively; Table 3).
Incidence of MALE and CV Events
Kaplan–Meier estimates of time to first MALE or CV event overall in the 12 months following PAD diagnosis were low across both cohorts, but numerically higher among Black patients relative to White patients and by individual MALE and CV events (Supplementary Figs. 1–6). Compared to White patients, the adjusted hazard of any MALE or CV event was significantly higher among Black patients [HR (95% CI) = 1.13 (1.11–1.15); P < 0.001; Table 4]. Except myocardial infarction, the adjusted hazards of all CV and limb events were also significantly higher among Black patients than White patients (Table 4). Black patients with PAD had a significantly higher hazard of both high and low amputations compared to White patients with PAD [high amputation: HR (95% CI) = 1.68 (1.58–1.79); P < 0.001, low amputation: HR (95% CI) = 1.15 (1.09–1.22); P < 0.001; Table 4]. Incidence of events of interest were further supported by numerically higher rates per 100 person-years among Black patients with PAD relative to White patients.
Discussion
Compared to White patients, Black patients were observed to have higher disease severity leading up to the PAD diagnosis and worse long-term CV and limb complications following the PAD diagnosis. More specifically, Black patients had a numerically higher Quan-CCI on average, a higher prevalence of comorbidities and PAD risk factors, as well as more widespread use of CV medications relative to White patients prior to diagnosis with PAD. Following PAD diagnosis, prevalence of medical management with diagnostic testing, revascularization procedures, and medication use was numerically higher among Black patients across all time intervals for up to 12 months post-diagnosis relative to White patients. Black patients were more likely than the White patients to receive medical therapy without a revascularization procedure. Black patients with PAD also had numerically higher time to first lower-limb revascularization and significantly higher hazards of lower-limb peripheral revascularization compared to White patients, further suggesting that Black patients present with more severe disease requiring earlier interventional management, which is recommended for patients with inadequate response to guideline-directed management and therapy, including structured exercise and pharmacotherapy (Class 1) [5]. With the exception of myocardial infarction, Black patients with PAD consistently had higher Kaplan–Meier rates of time to first MALE and CV events compared to White patients, which was further corroborated by significantly higher hazards of each outcome after adjusting for baseline confounders as well as higher rates of each outcome per 100 person-years.
Contrary to prior studies [12, 20, 21], this study found that Black patients had higher rates of diagnostic testing, CV medication use, and revascularization procedures than White patients, both before and after the diagnosis of PAD. This finding may be explained by the fairly homogenous population of commercially insured patients who were evaluated in this study, and all of whom had continuous health plan coverage during the study period. In a retrospective study of racial disparities in PAD before and after the 2006 Massachusetts health reform, which provided the framework for the Affordable Care Act, disparities in the probability of receiving revascularization procedures between non-White and White patients admitted with PAD were no longer statistically significant after insurance expansion as they were prior to expansion, underscoring the impact that inequities in health insurance coverage have on racial disparities in healthcare [22]. A different study of more than 115,000 hospitalizations among racial and ethnic minorities with lower extremity complications of diabetes reported a 33% reduction in high level amputations amongst early adopting Medicaid expansion states versus non-adopters [23]. Additional exploration is needed to further understand the implications of the synergy between ethnicity, diabetes, vascular disease, and access to care on medical management and outcomes among people with PAD [24].
Furthermore, Black patients were observed to have a higher severity of disease (as indicated by higher Quan-CCI scores and greater proportions of patients with multiple risk factors for PAD), and higher likelihood of all adverse outcomes over time (except for myocardial infarction), even after adjusting for baseline confounders. Similar findings were observed in a registry study of Black and non-Hispanic White Americans with infrainguinal PAD interventions, where Black patients presented with more advanced disease, including more diabetes, hypertension, congestive heart failure, and dialysis dependence, at time of initial major vascular operation [11]. Another registry study of the 1-year risk of MALE, major amputation, and death for patients undergoing elective revascularization for claudication or chronic limb-threatening ischemia found that the hazards of MALE and amputation were significantly higher among Black patients relative to White patients [25]. A different study of claims data from fee-for-service Medicare beneficiaries ≥ 66 years of age also found that Black beneficiaries were significantly more likely to experience adverse events after peripheral endovascular intervention compared to White beneficiaries [26].
Taken together, these findings suggest that increased diagnostic testing and/or medication use—potentially due to access to insurance coverage—may not always be indicative of better care. On the contrary, Black patients continue to be diagnosed at more advanced stages of the disease and have higher concomitant risk factors for PAD, potentially limiting the effectiveness of subsequent medical interventions. Other reasons for the persistent differences in health outcomes after adjustments in observable characteristics could be attributable to institutional barriers, individual provider issues, and patient issues [27]. For example, Black patients may have suboptimal health insurance coverage before and/or during the study period compared to White patients, which could result in the adverse outcomes observed in this study. Factors such as lower education and household income observed among Black patients could also contribute to reduced awareness about PAD and its management, all of which could result in worse outcomes over time. For example, one cross-sectional survey study of adults ≥ 50 years of age found that only 13.0% of Black Americans were aware of PAD, compared to 25.7% and 16.6% of non-Hispanic White Americans and Hispanic Americans, respectively. Moreover, awareness of PAD was consistently lower among individuals with lower income and education level [28]. Future interventions should be tailored to facilitate earlier diagnosis of PAD and improve the standard of care for Black patients with PAD, which, in turn, could reduce disparate adverse outcomes following diagnosis.
The present study should be viewed in the context of certain limitations. Analyses of administrative claims data depend on correct diagnosis, procedure, and drug codes, and coding inaccuracies may lead to case misidentification. Race may be misclassified due to the imputation method, which had a sensitivity of 48% [29]. However, the method was validated and demonstrated 97% specificity and 71% positive predictive value for estimating Black race [29]. While the study evaluated patient comorbidities and risk factors for PAD as potential markers of disease severity, the data lack clinical information, and therefore limit the ability to assess certain metrics, such as disease severity inferred by the physician using laboratory and imaging results. In addition, the data may not contain all prescription-related information, particularly medications administered in inpatient settings, and over-the-counter medications, such as aspirin. Moreover, the data do not contain information on reasons for loss of follow-up, which may introduce informative censoring bias. Clinical events following the end of data availability or patient healthcare coverage were not observed in the data. The study used robust statistical methods to control for observable differences across patient cohorts, including markers for disease severity and CV medication use. However, these techniques cannot account for unobserved heterogeneity (e.g., in diet and exercise, details regarding insurance coverage before and during the study period) which could in turn affect the outcomes. Results are representative of the commercial and Medicare Advantage population in the US and, therefore, may not be generalizable to other patient populations (e.g., those enrolled in Medicaid or those without health insurance).
Conclusions
Results of this real-world study highlight the substantial disease burden experienced by Black patients with PAD compared to White patients with PAD, including a high prevalence of comorbidities and risk factors of PAD, as well as an increased risk of adverse outcomes following diagnosis. The findings underscore the need for timely diagnosis and more effective management of PAD among Black patients.
References
Kohlman-Trigoboff D. Update: diagnosis and management of peripheral arterial disease. J Nurse Pract. 2019;15(1):87–95.
Campia U, et al. Peripheral artery disease: past, present, and future. Am J Med. 2019;132(10):1133–41.
Malakar AK, et al. A review on coronary artery disease, its risk factors, and therapeutics. J Cell Physiol. 2019;234(10):16812–23.
Alonso-Coello P, et al. Antithrombotic therapy in peripheral artery disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e669S-e690S.
Gerhard-Herman MD, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: executive summary: a Report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation. 2017;135(12):e686–725.
Hess CN, et al. A Structured review of antithrombotic therapy in peripheral artery disease with a focus on revascularization: a TASC (InterSociety Consensus for the Management of Peripheral Artery Disease) initiative. Circulation. 2017;135(25):2534–55.
Hussain MA, et al. Antithrombotic therapy for peripheral artery disease: recent advances. J Am Coll Cardiol. 2018;71(21):2450–67.
Anand SS, et al. Rivaroxaban with or without aspirin in patients with stable peripheral or carotid artery disease: an international, randomised, double-blind, placebo-controlled trial. The Lancet. 2018;391(10117):219–29.
Eikelboom JW, et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017;377(14):1319–30.
Matsushita K, et al. Lifetime risk of lower-extremity peripheral artery disease defined by ankle-brachial index in the United States. J Am Heart Assoc. 2019;8(18):e012177.
Soden PA, et al. Black patients present with more severe vascular disease and a greater burden of risk factors than white patients at time of major vascular intervention. J Vasc Surg. 2018;67(2):549-556.e3.
Holman KH, et al. Racial disparities in the use of revascularization before leg amputation in Medicare patients. J Vasc Surg. 2011;54(2):420-426.e1.
Hughes K, et al. Racial/ethnic disparities in amputation and revascularization: a nationwide inpatient sample study. Vasc Endovasc Surg. 2013;48(1):34–7.
Huber TS, et al. Impact of race on the treatment for peripheral arterial occlusive disease. J Vasc Surg. 1999;30(3):417–26.
Guadagnoli E, et al. The influence of race on the use of surgical procedures for treatment of peripheral vascular disease of the lower extremities. Arch Surg. 1995;130(4):381–6.
Chen L, et al. Disparities in peripheral artery disease hospitalizations identified among understudied race-ethnicity groups. Front Cardiovasc Med. 2021;8:692236.
Fanaroff AC, et al. Geographic and socioeconomic disparities in major lower extremity amputation rates in metropolitan areas. J Am Heart Assoc. 2021;10(17):e021456.
Solaru KW. Peripheral Artery disease and african americans: review of the literature. Curr Cardiovasc Risk Rep. 2019;13(9):27.
Grenon SM, et al. Peripheral artery disease and risk of cardiovascular events in patients with coronary artery disease: insights from the Heart and Soul Study. Vasc Med. 2013;18(4):176–84.
Gober L, Bui A, Ruddy JM. Racial and gender disparity in achieving optimal medical therapy for inpatients with peripheral artery disease. Ann Vasc Med Res. 2020;7(4):1115.
Collins TC, et al. The prevalence of peripheral arterial disease in a racially diverse population. Arch Intern Med. 2003;163(12):1469–74.
Loehrer AP, et al. Impact of expanded insurance coverage on racial disparities in vascular disease: insights from Massachusetts. Ann Surg. 2016;263(4):705–11.
Tan TW, et al. Rates of diabetes-related major amputations among racial and ethnic minority adults following Medicaid expansion under the patient protection and affordable care act. JAMA Netw Open. 2022;5(3):e223991.
Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376(24):2367–75.
Kalbaugh CA, et al. Non-hispanic black and hispanic patients have worse outcomes than white patients within similar stages of peripheral artery disease. J Am Heart Assoc. 2022;11(1):e023396.
Krawisz AK, et al. Differences in comorbidities explain black-white disparities in outcomes after femoropopliteal endovascular intervention. Circulation. 2022;146(3):191–200.
Yancy CW, et al. The coalition to reduce racial and ethnic disparities in cardiovascular disease outcomes (credo): why credo matters to cardiologists. J Am Coll Cardiol. 2011;57(3):245–52.
Hirsch AT, et al. Gaps in public knowledge of peripheral arterial disease. Circulation. 2007;116(18):2086–94.
DeFrank JT, et al. Triangulating differential nonresponse by race in a telephone survey. Prev Chronic Dis. 2007;4(3):A60.
Acknowledgements
Funding
This study and the journal’s Rapid Service and Open Access Fees were funded by Janssen Scientific Affairs, LLC.
Medical Writing, Editorial, and Other Assistance
The authors thank Amanda McKinley, who was an employee of Analysis Group, Inc. at the time of the study, for her support with conducting the data analyses.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
KCF, KS, RB, UD, PL, FL, and DGA, contributed to the study design. Formal analyses were conducted by DL, MM, and LM. All authors contributed to the critical interpretation of data as well as drafting/editing the manuscript, have approved the final version of this manuscript, and take responsibility for the integrity of this research study.
Disclosures
Kay Sadik and Richard Browne are employees of Janssen Scientific Affairs. Urvi Desai, Patrick Lefebvre, Dominique Lejeune, Malena Mahendran, François Laliberté, and Lisa Matay are employees of Analysis Group, Inc., which received funding from the study sponsor to conduct this research. Keith C. Ferdinand and David G. Armstrong received consulting fees from Janssen Scientific Affairs for this study.
Compliance with Ethics Guidelines
Since this study relied exclusively on de-identified patient records which were compliant with the patient confidentiality requirements of the Health Insurance Portability and Accountability Act and did not involve the collection, use, or dissemination of individually identifiable data, approval from an ethics committee was not required. Permission to access and use of the data was granted by Optum.
Data Availability
The datasets generated and analyzed during the current study are not publicly available, as they are subject to a data use agreement between Analysis Group, Inc., and the data provider. The data are available through requests made directly to Optum.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ferdinand, K.C., Sadik, K., Browne, R. et al. Real-World Racial Variation in Treatment and Outcomes Among Patients with Peripheral Artery Disease. Adv Ther 40, 1850–1866 (2023). https://doi.org/10.1007/s12325-023-02465-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02465-6