Abstract
Introduction
Studies evaluating patient and healthcare professional (HCP) preferences regarding long-acting injectable (LAI) antipsychotic agent attributes are lacking.
Methods
Surveys were administered to physicians, nurses, and patients who had at least two experiences with TV-46000, an investigational subcutaneous LAI antipsychotic agent for the treatment of schizophrenia, as part of the SHINE study (NCT03893825). Survey topics included preferences for route of administration, potential LAI dosing intervals (once-weekly, twice a month, once a month [q1m], every 2 months [q2m]), injection location, ease of use, syringe type, needle length, and need for reconstitution.
Results
Patients (n = 63) had a mean (SD) age of 35.6 (9.6) years, age at diagnosis of 18 (10) years, and were mostly male (75%). There were 49 HCPs: 24 physicians and 25 nurses. Patients rated “a short needle” (68%), a “choice of [q1m or q2m] dosing interval” (59%), and “injection instead of oral tablet” (59%) as the most important features. HCPs rated “single injection to initiate treatment” (61%), “flexible dosing interval” (84%), and “injection instead of oral tablet” (59%) as the most important features. Subcutaneous injections were rated “easy to [receive/administer]” by 62% of patients and 84% of HCPs. When choosing between subcutaneous injections and intramuscular injections, 65% of HCPs preferred subcutaneous injections and 57% of patients preferred intramuscular injections. It was important to most HCPs to have four dose strength options (78%), a prefilled syringe (96%), and no need for reconstitution (90%).
Conclusions
Patients had a range of responses, and on some issues patient and HCP preferences differed. Altogether, this suggests the importance of providing patients with a range of options and the importance of patient–HCP discussions on treatment preference for LAIs.
Plain Language Summary
Several medications for treating schizophrenia are available as long-acting injections. One advantage of these medications is that patients do not need to take pills daily. In this study, patients, doctors, and nurses were asked what medication characteristics they preferred. Question topics were similar to the following: “how often should it be taken?”; “what method of delivery do you prefer?”; “where on the body should it be injected?”; “how easy was it to use?”; “what physical properties do you like?”; and “do preparation steps matter?” Patients thought that being able to be given monthly or every other month was one of the most important features of an injection (59%). Patients also liked a short needle (68%) and an injection instead of an oral pill (59%). Doctors and nurses responded that it was important to have a single injection to start treatment (61%). They also liked having options for how often the medication was given (84%), and an injection instead of an oral pill (59%). An injection was “easy to [get/give]” for most patients (62%) and doctors and nurses (84%). Most doctors and nurses (65%) liked giving injections under the skin. Most patients (57%) liked injections into the muscle. Overall, patients and doctors/nurses agreed on most topics. There were, however, a range of patient responses; therefore, it is important for patients and doctors and nurses to talk about the available treatment options. Each individual patient may have their own preferences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In patients with schizophrenia, long-acting injectable antipsychotic agents (LAIs) can improve adherence over oral antipsychotic agents (OAs), and reduce relapse rates, hospital admissions, and exacerbation of psychotic symptoms, thus increasing the opportunity for patients to experience the full benefit of antipsychotic agents and a potentially substantial improvement of quality of life. |
To further understand patient and healthcare professional (HCP) preferences for LAI characteristics, we performed a survey of patients and HCPs focused on these preferences. |
The majority of patients preferred an injection over oral delivery, flexible dosing interval, and a short needle when selecting a long-acting injectable antipsychotic medication. |
The majority of HCPs valued having dosing options and flexibility of injection frequency and route of administration. |
Taken together, these results suggest the importance of providing a range of treatment options for patients and the need for shared decision-making between HCPs and patients. |
Introduction
Successful treatment of schizophrenia includes relapse prevention, as relapses can increase personal suffering, family burden, treatment resistance, and societal costs [1,2,3,4]. However, treatment nonadherence and discontinuation are reported in up to half of people with schizophrenia [5,6,7]. Possible reasons for nonadherence and discontinuation include severity of illness, antipsychotic therapy (AP) side effects, and poor illness insight [8], but may also include the ease of use of the medication.
Though oral antipsychotic therapies (OAs) can substantially improve symptoms and patient quality of life, they must be taken daily, which can prove challenging to patients with schizophrenia because of insight impairment associated with the illness. Long-acting injectable antipsychotic therapies (LAIs) provide alternative dosing schedules from once every 2 weeks up to once every 6 months [9,10,11]. LAIs can improve adherence over OAs, and reduce relapse rates, hospital admissions, and exacerbation of psychotic symptoms, thus increasing the opportunity for patients to experience the full benefit of APs and a potentially substantial improvement in quality of life [12,13,14,15,16,17,18].
Despite the potential benefits of LAIs, LAIs are prescribed less often than OAs. This indicates that there may be barriers to treatment with LAIs [19, 20]. One barrier may be the lack of confidence in and knowledge of LAI use by psychiatrists [21,22,23]. Other obstacles for patients and medical professionals to successful LAI implementation include the need for OA supplementation and/or loading doses, inflexible dosing regimens, and intramuscular (im) administration required for many LAIs [24,25,26,27], along with patient aversion to needles, a stigma associated with LAIs, and a general lack of understanding of their usefulness [22, 28]. In general, patients who prefer LAIs focus on empowerment and quality-of-life-related goals [29]. Perhaps underlying obstacles to LAI use is the understudied discordance between patient and healthcare professional (HCP) goals for treatment and expected responses to LAIs [30].
LAIs differ in their characteristics (e.g., route of administration, dosing interval, injection location, ease of use, syringe type, needle length, and need for reconstitution). Patient and HCP preferences about LAI characteristics may influence decisions about LAI treatment. Although studies on patient preferences for AP treatment have been done [31, 32], data on patient preferences about LAI characteristics are limited [33]. Regarding dosing interval, one study of 1402 patients who were enrolled in a clinical trial for paliperidone palmitate [29] found that once-monthly and once-every-3-months dosing was preferred by 38% and 50%, respectively.
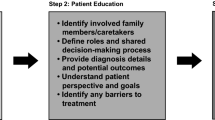
To further understanding of patient and HCP preferences of LAI characteristics, we performed a survey of patients and HCPs focused on LAI characteristic preferences. The survey included questions probing preferences for route of administration, dosing interval, injection location, syringe type, needle length, need for reconstitution, and need for a loading dose as well as perceptions of ease of use. By narrowly changing the perspective (i.e., from “receive” for patients to “administer” for HCPs) and keeping the other language similar, this survey aimed to compare group responses on these LAI characteristics.
Methods
Study Design
This was a cross-sectional survey of physicians, nurses, and patients who participated in the Safety in Humans of TV-46000 sc INjection Evaluation (SHINE; NCT03893825) study. During the SHINE study, patients aged 18 years or older with a clinical diagnosis of schizophrenia received TV-46000 either once monthly (q1m) or once every 2 months (q2m) (with placebo injections in alternating months). The survey, consent forms, and all patient-facing recruitment materials were approved by a central institutional review board (IRB), Advarra (Pro00044509). Patients and clinical trial staff participating in the clinical trial provided electronic informed consent before survey administration. This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Survey Design
To address the study objectives, three surveys (patient, physician, and nurse) were constructed, and covered five areas: (1) demographics or site description, (2) location and type of injection, (3) dosing characteristics, (4) treatment comparisons, and (5) treatment satisfaction (Supplementary Table 1).
Three sections were identical in all survey versions and varied lexically only by frame of reference (e.g., “to receive an injection” versus “to administer an injection”). All Likert scales were seven points (for standardization and adequate psychometrics) except one question where the survey measured a trade-off captured by the poles of the nine-point scale. No other questions required a similar trade-off to be made. A score of 1 corresponded to “least” and a score of 7 or 9 corresponded to “most.” Location and type of injection characteristic questions focused on rating the benefit of the ability to have a choice (or provide a choice) of location for injection, optimum location (abdomen, back of upper arm, or buttocks), preferred option between im injection and subcutaneous (sc) injection, and preference between a longer or shorter needle. Dosing characteristic questions asked about frequency of receiving (or administering) LAIs and rationale for that choice, desired options when switching from one LAI for schizophrenia to another, and most desirable features when receiving (or administering) an LAI for schizophrenia.
The two sections that were different in the patient and HCP surveys were the demographics or site description section and the treatment comparisons section. While the patient survey inquired about patient gender, race, employment status, age, age when first diagnosed with schizophrenia, and number of relapses in the past 12 months, the HCP survey inquired about the clinical trial site, who prescribes/administers injectable treatments, the individual HCP’s role at the site, and medical specialty (if a principal investigator at the site). The HCP survey inquired about individual preference regarding whether or not it was beneficial to require a loading dose and/or oral supplementation to initiate treatment, the advantage of a pre-filled syringe and/or having no need for reconstitution, and the importance of having four dose strengths available within each treatment interval (q1m or q2m). In the treatment comparisons section, the patient survey inquired about previous LAI use and administration frequency and how the clinical trial medication compared with previous AP use. Though there is no LAI antipsychotic agent approved for once-weekly administration, this option was included since a strong preference for it would provide evidence for development of a once-weekly medication.
Respondents
The sponsor sent a request to each site asking for participation; sites with affirmative responses were contacted, and patients and HCPs were recruited. All patient respondents must have participated in the SHINE study. HCP respondents could be either study physicians (i.e., investigators/physicians) or study nurses who routinely administer injectable medications to patients as part of their clinical practice. All physicians and nurses actively participated in clinical trial medication administration as part of the SHINE study. There was no attempt to pair patients with the HCP who treated them in the study.
Procedures
The survey was administered by electronic tablet to patients and by web application to physicians and nurses. Surveys were administered to physicians and nurses following a minimum of two experiences prescribing/administering clinical trial medication as part of the SHINE study. Surveys were administered to patients following a minimum of two experiences receiving clinical trial medication (week 8 or week 12). Patients were assisted at the clinical trial site by study coordinators to operate the electronic tablets when needed. The dosing arm was masked for this study, and the analyses were conducted with the masking intact.
Statistical Analysis
The study included a convenience sample with a minimum target of 60 patients, 30 physicians, and 30 nurses. Descriptive statistics were used to analyze differences between patient and HCP responses to survey questions. Confidence intervals at the 95% level were calculated using the normal approximation to the binomial. Statistical procedures conducted were t tests for continuous variables or a chi-squared test for categorical variables for comparison of patients surveyed after week 8 study visits versus after week 12 study visits. A chi-squared test was used to analyze patient and total HCP preference between q1m and q2m. When summarizing Likert scale responses, data tables include “proportion (%) positive,” which is the proportion of respondents who rated a question higher than the mid-point on the scale.
Compliance with Ethics Guidelines
Materials including the survey, electronic informed consent form, and all patient-facing recruitment materials were approved by a central IRB. All participants were aware of the objectives of the study and that the results of the study would be published. Patients and clinical trial staff participating provided electronic informed consent before survey administration. Patients were only included if they were competent to provide consent. Individuals’ data was protected by remaining with the clinical site, ensuring Health Insurance Portability and Accountability Act (HIPAA) compliance, and information provided to third-party organizations did not contain identifiable patient information and was encrypted and stored on a password-protected secure server.
Results
Respondents
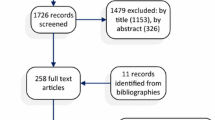
This survey was a companion study to the SHINE study, which had 336 participants in the intent-to-treat population from 60 sites in the USA and Bulgaria. Of the 53 clinical trial sites in the USA participating in the SHINE study, 15 agreed to participate in the survey study, and most of the 15 sites had at least three patients participating in the parent study. Of the 102 patients available for participation, 63 (62%) completed the survey. All patients received TV-46000 in the SHINE study. Comparisons were also made between patients who took the survey after week 8 and those who completed it after week 12. No significant differences were found between these groups. Because no differences were observed, there was no need to stratify data.
The mean (SD) age of patient respondents was 35.6 (9.6) years. The majority of survey respondents were male (n = 47; 75%). The mean (SD) age at diagnosis was 18 (10) years. Most patients surveyed were either Black or African American (51%) or Hispanic, Latino, Spanish origin (35%), and 13% of patients identified as white. Only 8% of patient respondents were currently employed full-time or part-time. Overall, very few patients (n = 6) had experienced a relapse in the 12 months prior to taking the survey (Table 1).
There were 49 HCPs that responded to the survey. Of these, 24 were physicians, all of whom served as principal investigators or sub-investigators in the SHINE study, and 25 nurses, all of whom served as a site nurse during the study. Study sites that participated in this companion study were overseen by psychiatrists or internal or general medicine physicians. Only 21% of physicians surveyed prescribe and administer injectable medicines in their routine practice. As expected, physicians were more likely to prescribe or delegate injectable treatments, whereas nurses were more likely to administer injections than physicians (Table 2). Twenty-three of the 25 nurses (92%) and 7 of the 24 (29%) physicians personally administered clinical trial medication to patients during the SHINE study. The majority of the site staff that completed surveys were from sites that did not recruit patients for this survey study (n = 31 HCPs). Surveys took 15–25 min to complete, and patients took longer than HCPs. There were no breakoffs during survey administration (respondents who began the survey and failed to complete it).
Injection Characteristics and Location Choice
The first section of the survey inquired about preferences for LAIs in general, including location on the body for administering or receiving the injection, as well as other injection characteristics. Overall, 72% of patients rated having a choice of injection site as a positive (i.e., score ≥ 5 on the seven-point scale), whereas 19% of patients rated it negatively (i.e., score < 4 on the seven-point scale) (Table 3). Similarly, 82% of HCPs rated having a choice of injection site as a positive, and only 8% rated it negatively. When asked about the benefits of having a choice for injection location, patients reported that the two greatest benefits were “not having to inject the same place [every time]” and “injecting the same place every time may make the area sensitive.” HCPs’ top two reported benefits for having a choice of sites were “injecting the same place every time may make the area sensitive” and “having a choice.” As shown in Supplementary Table 2, approximately half of patients (49% [95% CI 36.7–61.3]) selected the back of the upper arm as their preferred location to receive an injection. Among HCPs, 63% (95% CI 49.5–76.5) selected the back of the upper arm as their preferred location to give an injection. Both patients and HCPs selected the buttocks least often, 19% and 10%, respectively, as the preferred injection site.
The survey explored the ease or difficulty of administering or receiving an sc injection (Supplementary Table 2). An sc injection was rated “easy to receive” by 62% of patients (score ≥ 5 on the seven-point scale), and of those, 38% indicated it as “very easy” to receive (score 7 on the seven-point scale). Only 17% of patients rated an sc injection as being “difficult to receive” (score < 4 on the seven-point scale). The majority of HCPs (84%) rated an sc injection as being “easy to administer,” and 43% said they were “very easy to administer.” Most patients (94%) and HCPs (80%) would choose a short needle over a longer one.
When comparing sc and im injections, 38% of patients perceived sc injections to be more comfortable than im injections, 27% of patients preferred im injections, and 35% perceived no difference in comfort (Supplementary Table 2). Most HCPs (63%) perceived sc injections as more comfortable for patients than im injections, and 8% perceived no difference. Despite more patients perceiving sc injections as comfortable, 57% (95% CI 45–69) of patients reported they would choose an im injection over an sc injection. The majority of HCPs (65%) would choose to administer an sc injection over an im injection. When asked to select their rationale for choosing, patient rationales were similar for both injection types—they perceived one injection type to cause less discomfort than the other (44% for sc, 42% for im). The top reason HCPs chose an sc injection was “causes less discomfort” (59%) and the top reason for choosing an im injection was “easier” (29%).
Dosing Characteristics
The next section of the questionnaire explored choice for LAI dosing intervals and how patients and HCPs prefer to start a new injectable medication or switch from one injectable medication to another. When choosing between injections once weekly, once every 2 weeks, once monthly, or once every 2 months, patients reported that they would prefer to receive an LAI every month (75%) or every 2 months (21%) (Table 4). HCPs were evenly split between desiring to administer an LAI every month (49%) versus every 2 months (47%). Few patients or HCPs would choose to use a weekly (if available) or every-2-weeks injection schedule.
These results were consistent with responses to the next question: when asked if they prefer once monthly or once every 2 months dosing if medication effectiveness was the same in either case, patients were significantly (p < 0.05) more likely to want q1m injections (73%), whereas HCPs were more likely to choose the q2m option (61%) (Supplementary Table 3). Physicians were more likely than nurses to choose a q2m injectable treatment option. When asked about their preference for either q1m or q2m dosing, patients most frequently selected “only [6 or 12] injections per year” and “no need for daily medications”. HCPs chose the same two benefits most frequently, but HCPs also ranked “not a daily reminder of sickness” as a benefit for q2m dosing. Fewer patients and HCPs chose “no need for doctor visits as often” as a q2m benefit (40% and 53%, respectively) than patients and HCPs who chose it as a benefit of q1m dosing (54% and 67%). Overall, 84% of patients and 80% of HCPs reported that it was important to have a choice for dosing interval (q1m versus q2m) (Table 4).
When asked how they would prefer to switch from one schizophrenia treatment to another, 86% of patients and 90% of HCPs would prefer to switch from one medication to another via a single injection, rather than via oral supplementation or a loading dose of the injectable medication (Supplementary Table 3). Survey participants were asked to indicate the three most important features of an LAI for schizophrenia (Table 4). Patients most often selected “a short needle” (68%), “can be given either every month or every other month” (59%), and “it is an injection rather than an oral tablet” (59%). “Sc versus im injection” was chosen least often as an important feature by patients. When HCPs were asked for the three most important features of an LAI, they selected “can be given either every month or every other month” (84%), “only needing a single injection to initiate therapy” (61%), and “it is an injection rather than an oral tablet” (59%). “Choice of injection site” was selected least often as an important medication feature by HCPs.
Importance of Treatment Options
The majority of HCPs (78%) indicated that it was very important (score ≥ 5 on the seven-point scale) to have four dosing options for an LAI (Table 5). Only 8% of HCPs felt having four dosing options was not important. Similarly, 90% of HCPs claimed that it was beneficial (score ≥ 5 on the seven-point scale) to not require a loading dose during initiation of or while switching schizophrenia treatment (Supplementary Table 4). Only one HCP felt that lack of loading dose was not beneficial. HCPs favored using prefilled syringes, which 96% of HCPs believed was an advantage for an LAI medication for schizophrenia. Most HCPs (90%) believed that having no reconstitution was an advantage for an LAI medication for schizophrenia (Table 5). A greater proportion of physicians (96%) than nurses (84%) indicated that having no need for reconstitution was an advantage.
Clinical Trial Medication Versus Previous Treatments
Of the ten patients who had previous experience with an LAI, nine received their previous LAI once monthly, and seven indicated the “clinical trial medication had better injection experience” than their previous LAI (Supplementary Table 5). All patients (N = 63) were asked whether they would choose to continue using the investigational medicine from the SHINE study or return to the medication that they received before the study (oral or LAI); 90% of patients reported that they would opt to use the clinical trial medication. Overall, 89% of patients and 92% of HCPs responded that it was easy to receive/administer the study medication in its current form. Similarly, 92% of patients and 96% of HCPs were satisfied with the clinical trial medication.
Discussion
This study examined patient and HCP preferences for LAI features, including ease of use and treatment satisfaction, in a specific, structured, and systematic way. It was designed as a companion to the SHINE study, which evaluated the safety and tolerability of TV-46000, currently under investigation for the treatment of schizophrenia. Overall, this companion study provided insight into patient and HCP preferences and attitudes towards various characteristics of LAI APs. This information may be useful for educating HCPs about LAIs and for patient–HCP discussions about LAIs as a treatment option.
The majority of patients (72%) and HCPs (82%) valued having a choice of injection location. Patients and HCPs had similar preferences for injection locations, with the order from most to least popular being back of the upper arm, the abdomen, and the buttocks. This is consistent with other studies that compared im injections in the deltoid and gluteal muscles and found that patients prefer the buttocks the least [29].
Overall, patients (84%) and HCPs (80%) felt it was important to have the choice to receive medication either every month or every 2 months, and of those, 67% and 33%, respectively, rated it as “very important.” These results support the concept of providing patients and their HCPs with options for administration frequency. When offered four different frequency options (once weekly, once every 2 weeks, q1m, or q2m), patients preferred q1m (75%) and HCPs were split between q1m (49%) and q2m (47%). When pinned between either an injectable medication administered once monthly or once every 2 months, even if medication effectiveness was the same, patient and HCP preferences differed. Patients (73%) would choose once monthly, whereas HCPs (61%) would choose once every 2 months. Interestingly, previous data on patient preference for LAI injection frequency showed a range of preferences, with 50% preferring every 3 months, 38% preferring every month, and 9% having no preference [29]. For patients, perceived benefits of receiving once-monthly injections centered around timing, including “no need to go to the doctor’s office or clinic as often,” “easier to manage time,” and “no need to remember to take this medication daily.” For HCPs, the highest perceived benefit for once-every-2-months dosing was “no need for patient to remember to take this medication daily” (92%). Of note, this was also listed as the highest perceived benefit for medication taken once monthly (86%), suggesting that receiving medication once monthly or once every 2 months is preferred compared with oral medications. Interestingly, in another study [30], among 20 treatment goals identified by focus groups and then ranked by patients and psychiatrists, “frequency of visits to the doctor/hospital” ranked in the bottom half (15 and 16, respectively) of both group priorities. Thus, it may be that though patients would prefer less frequent doctor visits, once it becomes as infrequent as once monthly, further reduction is not prioritized by patients.
Despite 62% of patients rating “injection under the skin but not into the muscle” as “easy to receive,” when asked to choose sc or im injection, 57% of patients preferred im. This discrepancy may be because both types of injection were perceived as easy to receive or because patients were inexperienced with either or both types of injection, though this is ultimately unknown. In this regard, when responding to a nine-point scale ranging from “into muscle much more comfortable” to “into under skin much more comfortable” with “no difference” between, 35% of patients chose “no difference.” Though the proportion of patients responding that sc injection was more comfortable (38%) was higher than the proportion responding that im injection was more comfortable (27%), the group responding “no difference” was a substantial proportion of patients. In addition, comparable proportions of patients rated “it causes less discomfort” as the primary rationale for favoring im or sc injection (42% and 44%, respectively), regardless of which they listed as their preference. The largest difference in patient rationale for selection of injection type was “it is faster,” which was chosen by 25% of patients that preferred im and 7% of patients that preferred sc. In contrast, a study of women’s preference between regular treatment with sc or im injections found that 79% preferred sc injections [34]. When HCPs were asked whether they preferred to administer an im or sc injection, 65% preferred sc over im because they felt it causes less discomfort for the patient, and this result aligned with previous literature [34].
Only HCPs were asked about the number of dose strengths available. The majority of HCPs (78%) responded that it was important to have four dose strengths available. The rationale for this likely centers around being able to tailor treatment to a particular patient’s needs, including being able to increase or decrease doses as needed. Most HCPs (90%) felt it was beneficial not to require oral or injectable supplementation or a loading dose to initiate treatment, which likely corresponds to a desire to simplify treatment or challenges with remembering to take medication faced by patients with schizophrenia [7, 8, 35].
Limitations of this study include the lack of caregiver data. Although the study design included a survey for caregivers, no caregivers could be recruited to participate. Data about their perceptions would add valuable insight to this analysis, as caregivers are extremely important in maintenance of care and management of schizophrenia symptoms. This study was a companion to the SHINE study, which means HCPs and patients were willing to partake in a clinical trial that involved consenting to injections. This may produce bias in the HCP population for the overall acceptance of LAIs as a treatment option and the perceptions around injection parameters. Additionally, this was a companion to the SHINE study in which patients received TV-46000 as an sc LAI once monthly or once every 2 months (with placebo injections interleaved). Therefore, our data may not generalize to patients with schizophrenia who have received other LAI antipsychotic therapies with various dose intervals. Though all 53 US sites from the SHINE study were contacted, only 15 participated in this survey study; however, those 15 sites accounted for 43% of the total patients who participated in the trial. Furthermore, the majority of the sites were dedicated research sites, which limits representation of patients in real-world clinics. While the study population does not represent the population of patients treated with antipsychotics in the USA, it does reflect the diversity present in the US population.
Conclusion
Insights from this companion study provide a better understanding of HCP and patient preferences regarding LAI characteristics. Of note, patients had a range of preferences on some of our survey questions and for some issues their preferences differed from those of HCPs. This highlights the importance of providing patients with information on the range of LAI options and obtaining their individual preferences when considering LAI treatment. On the whole, finding the right therapeutic regimen for patients with schizophrenia is a highly individualized process that should include shared decision-making between patients and HCPs. The information from our survey may aid in the patient–HCP conversation.
References
Correll CU, Rubio JM, Kane JM. What is the risk-benefit ratio of long-term antipsychotic treatment in people with schizophrenia? World Psychiatry. 2018;17(2):149–60. https://doi.org/10.1002/wps.20516.
Pennington M, McCrone P. The cost of relapse in schizophrenia. Pharmacoeconomics. 2017;35(9):921–36. https://doi.org/10.1007/s40273-017-0515-3.
Takeuchi H, Siu C, Remington G, et al. Does relapse contribute to treatment resistance? Antipsychotic response in first- vs. second-episode schizophrenia. Neuropsychopharmacology. 2019;44(6):1036–42. https://doi.org/10.1038/s41386-018-0278-3.
Yu Y, Liu ZW, Tang BW, Zhao M, Liu XG, Xiao SY. Reported family burden of schizophrenia patients in rural China. PLoS ONE. 2017;12(6):e0179425. https://doi.org/10.1371/journal.pone.0179425.
Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63(10):892–909. https://doi.org/10.4088/jcp.v63n1007.
MacEwan JP, Forma FM, Shafrin J, Hatch A, Lakdawalla DN, Lindenmayer JP. Patterns of adherence to oral atypical antipsychotics among patients diagnosed with schizophrenia. J Manag Care Spec Pharm. 2016;22(11):1349–61. https://doi.org/10.18553/jmcp.2016.22.11.1349.
Kane JM, Kishimoto T, Correll CU. Non-adherence to medication in patients with psychotic disorders: epidemiology, contributing factors and management strategies. World Psychiatry. 2013;12(3):216–26. https://doi.org/10.1002/wps.20060.
Birnbaum M, Sharif Z. Medication adherence in schizophrenia: patient perspectives and the clinical utility of paliperidone ER. Patient Prefer Adherence. 2008;2:233–40. https://doi.org/10.2147/ppa.s3346.
Lauriello J, Lambert T, Andersen S, Lin D, Taylor CC, McDonnell D. An 8-week, double-blind, randomized, placebo-controlled study of olanzapine long-acting injection in acutely ill patients with schizophrenia. J Clin Psychiatry. 2008;69(5):790–9. https://doi.org/10.4088/jcp.v69n0512.
Najarian D, Sanga P, Wang S, et al. A randomized, double-blind, multicenter, noninferiority study comparing paliperidone palmitate 6-month versus the 3-month long-acting injectable in patients with schizophrenia. Int J Neuropsychopharmacol. 2021;25(3):238–51. https://doi.org/10.1093/ijnp/pyab071.
Kane JM, Peters-Strickland T, Baker RA, et al. Aripiprazole once-monthly in the acute treatment of schizophrenia: findings from a 12-week, randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2014;75(11):1254–60. https://doi.org/10.4088/JCP.14m09168.
Nielsen RE, Hessellund KB, Valentin JB, Licht RW. Second-generation LAI are associated to favorable outcome in a cohort of incident patients diagnosed with schizophrenia. Schizophr Res. 2018;202:234–40. https://doi.org/10.1016/j.schres.2018.07.020.
Subotnik KL, Casaus LR, Ventura J, et al. Long-acting injectable risperidone for relapse prevention and control of breakthrough symptoms after a recent first episode of schizophrenia. A randomized clinical trial. JAMA Psychiat. 2015;72(8):822–9. https://doi.org/10.1001/jamapsychiatry.2015.0270.
Misawa F, Kishimoto T, Hagi K, Kane JM, Correll CU. Safety and tolerability of long-acting injectable versus oral antipsychotics: a meta-analysis of randomized controlled studies comparing the same antipsychotics. Schizophr Res. 2016;176(2–3):220–30. https://doi.org/10.1016/j.schres.2016.07.018.
Kishimoto T, Hagi K, Kurokawa S, Kane JM, Correll CU. Long-acting injectable versus oral antipsychotics for the maintenance treatment of schizophrenia: a systematic review and comparative meta-analysis of randomised, cohort, and pre-post studies. Lancet Psychiatry. 2021;8(5):387–404. https://doi.org/10.1016/S2215-0366(21)00039-0.
Emsley R, Oosthuizen P, Koen L, Niehaus DJH, Medori R, Rabinowitz J. Oral versus injectable antipsychotic treatment in early psychosis: post hoc comparison of two studies. Clin Ther. 2008;30(12):2378–86. https://doi.org/10.1016/j.clinthera.2008.12.020.
Ostuzzi G, Bertolini F, Del Giovane C, et al. Maintenance treatment with long-acting injectable antipsychotics for people with nonaffective psychoses: a network meta-analysis. Am J Psychiatry. 2021;178(5):424–36. https://doi.org/10.1176/appi.ajp.2020.20071120.
Kane JM, Schooler NR, Marcy P, et al. Effect of long-acting injectable antipsychotics vs usual care on time to first hospitalization in early-phase schizophrenia: a randomized clinical trial. JAMA Psychiat. 2020;77(12):1217–24. https://doi.org/10.1001/jamapsychiatry.2020.2076.
Robinson DG, Subramaniam A, Fearis PJ, et al. Focused ethnographic examination of barriers to use of long-acting injectable antipsychotics. Psychiatr Serv. 2020;71(4):337–42. https://doi.org/10.1176/appi.ps.201900236.
Kane JM, Schooler NR, Marcy P, Achtyes ED, Correll CU, Robinson DG. Patients with early-phase schizophrenia will accept treatment with sustained-release medication (long-acting injectable antipsychotics): results from the recruitment phase of the PRELAPSE trial. J Clin Psychiatry. 2019;80(3):18m12546. https://doi.org/10.4088/JCP.18m12546.
Iyer S, Banks N, Roy MA, et al. A qualitative study of experiences with and perceptions regarding long-acting injectable antipsychotics: part II-physician perspectives. Can J Psychiatry. 2013;58(5 Suppl 1):S23–S29. https://doi.org/10.1177/088740341305805s04.
Patel MX, Haddad PM, Chaudhry IB, McLoughlin S, Husain N, David AS. Psychiatrists’ use, knowledge and attitudes to first- and second-generation antipsychotic long-acting injections: comparisons over 5 years. J Psychopharmacol. 2010;24(10):1473–82. https://doi.org/10.1177/0269881109104882.
Patel MX, Bent-Ennakhil N, Sapin C, et al. Attitudes of European physicians towards the use of long-acting injectable antipsychotics. BMC Psychiatry. 2020;20(1):123. https://doi.org/10.1186/s12888-020-02530-2.
Hasan A, Falkai P, Wobrock T, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia, part 1: update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J Biol Psychiatry. 2012;13(5):318–78. https://doi.org/10.3109/15622975.2012.696143.
Ascher-Svanum H, Zhu B, Faries DE, Furiak NM, Montgomery W. Medication adherence levels and differential use of mental-health services in the treatment of schizophrenia. BMC Res Notes. 2009;2:6. https://doi.org/10.1186/1756-0500-2-6.
Correll CU, Kim E, Sliwa JK, et al. Pharmacokinetic characteristics of long-acting injectable antipsychotics for schizophrenia: an overview. CNS Drugs. 2021;35(1):39–59. https://doi.org/10.1007/s40263-020-00779-5.
Correll CU, Litman RE, Filts Y, et al. Efficacy and safety of once-monthly Risperidone ISM® in schizophrenic patients with an acute exacerbation. NPJ Schizophr. 2020;6(1):37. https://doi.org/10.1038/s41537-020-00127-y.
Citrome L, Belcher E, Stacy S, Suett M, Mychaskiw M, Salinas GD. Management of schizophrenia with long-acting injectable antipsychotic medications: an assessment of the educational needs of clinicians [published correction appears in Schizophrenia]. Neuropsychiatr Dis Treat. 2022;18:111–23. https://doi.org/10.2147/NDT.S326299.
Blackwood C, Sanga P, Nuamah I, et al. Patients’ preference for long-acting injectable versus oral antipsychotics in schizophrenia: results from the patient-reported medication preference questionnaire. Patient Prefer Adherence. 2020;14:1093–102. https://doi.org/10.2147/PPA.S251812.
Bridges JFP, Slawik L, Schmeding A, Reimer J, Naber D, Kuhnigk O. A test of concordance between patient and psychiatrist valuations of multiple treatment goals for schizophrenia. Health Expect. 2013;16(2):164–76. https://doi.org/10.1111/j.1369-7625.2011.00704.x.
McCrone P, Mosweu I, Yi D, Ruffell T, Dalton B, Wykes T. Patient preferences for antipsychotic drug side effects: a discrete choice experiment. Schizophrenia Bull Open. 2021;2(1):sgab046.
Achtyes E, Simmons A, Skabeev A, et al. Patient preferences concerning the efficacy and side-effect profile of schizophrenia medications: a survey of patients living with schizophrenia. BMC Psychiatry. 2018;18(1):292. https://doi.org/10.1186/s12888-018-1856-y.
Levitan B, Markowitz M, Mohamed AF, et al. Patients’ preferences related to benefits, risks, and formulations of schizophrenia treatment. Psychiatr Serv. 2015;66(7):719. https://doi.org/10.1176/appi.ps.201400188.
Gandell DL, Bienen EJ, Gudeman J. Mode of injection and treatment adherence: results of a survey characterizing the perspectives of health care providers and US women 18–45 years old. Patient Prefer Adherence. 2019;13:351–61. https://doi.org/10.2147/PPA.S187120.
El Abdellati K, De Picker L, Morrens M. Antipsychotic treatment failure: a systematic review on risk factors and interventions for treatment adherence in psychosis. Front Neurosci. 2020;14:531763. https://doi.org/10.3389/fnins.2020.531763.
Acknowledgements
We thank the participants of the study.
Funding
The study sponsor, Teva Branded Pharmaceutical Products R&D, Inc., funded this study and the Rapid Service and Open Access Fees for this manuscript.
Medical Writing and/or Editorial Assistance
Medical writing support for the development of this manuscript, under the direction of the authors, was provided by Jeffrey A. Blair, PhD, and Jennifer C. Jaworski, MS, BCMAS, and editing support by Kelsey Hogan, MS, all of Ashfield MedComms, an Inizio Company, and funded by Teva Branded Pharmaceutical Products R&D, Inc.
Author Contributions
Participated in concept and design of the work: Mark Suett, Amanda Wilhelm, Nayla Chaijale, Kelli R. Franzenburg, Sanjay Gandhi, and Marko Mychaskiw. Participated in the acquisition and analysis of the work: Blaine Cloud. Participated in the interpretation of data for the work: Delbert G. Robinson, Mark Suett, Amanda Wilhelm, Nayla Chaijale, Kelli R. Franzenburg, Sanjay Gandhi, and Marko Mychaskiw. Participated in drafting and/or critical revision and approval of the final manuscript: Delbert G. Robinson, Mark Suett, Amanda Wilhelm, Nayla Chaijale, Kelli R. Franzenburg, Sanjay Gandhi, Blaine Cloud, and Marko Mychaskiw.
Prior Presentation
This data has been previously presented at Robinson DG, Suett M, Chaijale N, et al. Patient and healthcare professional preferences and treatment experiences with TV-46000, a long-acting subcutaneous antipsychotic risperidone formulation. Presented at: 6th Annual Psych Congress Elevate; June 3–5, 2022; Las Vegas, Nevada. Robinson DG, Suett M, Wilhelm A, et al. Patient and healthcare professional preferences and treatment experiences with TV-46000, a long-acting subcutaneous antipsychotic (LASCA) risperidone formulation. Presented at: 4th Annual Congress of the Schizophrenia International Research Society; April 6–10, 2022; Florence, Italy. Robinson DG, Suett M, Wilhelm A, et al. Patient and healthcare professional preferences and treatment experiences with TV-46000, a long-acting subcutaneous antipsychotic (LASCA) risperidone formulation. Presented at: 25th Annual Meeting of the College of Psychiatric and Neurologic Pharmacists; April 24–27, 2022; San Antonio, Texas. Robinson D, Suett M, Wilhelm A, et al. Patient preferences and treatment experiences with TV-46000, a long-acting subcutaneous antipsychotic agent. Presented at: 27th Annual National Psychopharmacology Update; February 16–19, 2022; Las Vegas, Nevada. Robinson DG, Suett M, Wilhelm A, et al. Patient preferences and treatment experiences with TV-46000, a long-acting subcutaneous injectable risperidone formulation. Presented at: 34th Annual Psych Congress; October 29–November 1, 2021; San Antonio, Texas. Robinson D, Suett M, Wilhelm A, et al. Healthcare professional preferences and treatment experiences with TV-46000, a long-acting injectable risperidone formulation. Presented at: 27th Annual National Psychopharmacology update; February 16–19, 2022; Las Vegas, Nevada. Robinson DG, Suett M, Wilhelm A, et al. Healthcare professional preferences and treatment experiences with TV-46000, a long-acting injectable risperidone formulation. Presented at: 34th Annual Psych Congress; October 29–November 1, 2021; San Antonio, Texas. Robinson DG, Suett M, Wilhelm A, et al. Patient and healthcare professional preferences and treatment experiences with TV-46000, a long-acting subcutaneous antipsychotic risperidone formulation. Presented at: 6th Annual Meeting of the American Psychiatric Nurses Association; October 19–22, 2022; Long Beach, California. Robinson DG, Suett M, Wilhelm A, et al. Nurse preferences and treatment experiences with TV-4 6000, a long-acting subcutaneous antipsychotic (LASCA) agent. Presented at: 6th Annual Meeting of the American Psychiatric Nurses Association; October 19–22, 2022; Long Beach, California.
Disclosures
Delbert G. Robinson has been a consultant for/has received honoraria from Teva Pharmaceuticals. He has also been a consultant to Advocates for Human Potential, American Psychiatric Association, C4 Innovations, Costello Medical Consulting, Health Analytics, Innovative Science Solutions, Janssen, Lundbeck, Neurocrine, Neuronix, Otsuka, and US WorldMeds and has received grant support from Otsuka. Mark Suett, Nayla Chaijale, Kelli R. Franzenburg, Sanjay Gandhi, and Marko Mychaskiw are employees and shareholders of Teva Pharmaceuticals. Amanda Wilhelm was an employee of Teva Pharmaceuticals at the time of this research. Blaine Cloud was an employee of Clinical SCORE at the time of this research; Clinical SCORE received payments from Teva Pharmaceuticals in relation to this study. Amanda Wilhelm was in Teva Branded Pharmaceutical Products R&D, Inc., North America Medical Affairs at the time of this research. Blaine Cloud was in Clinical SCORE at the time of this research.
Compliance with Ethics Guidelines
Materials including the survey, electronic informed consent form, and all patient-facing recruitment materials were approved by a central IRB, Advarra (Pro00044509). All participants were aware of the objectives of the study and that the results of the study would be published. Patients and clinical trial staff participating provided electronic informed consent before survey administration. Patients were only included if they were competent to provide consent. Individuals’ data was protected by remaining with the clinical site, ensuring HIPAA compliance, and information provided to third-party organizations did not contain identifiable patient information and was encrypted and stored on a password-protected secure server. This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Data Availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request. Qualified researchers may request access to patient level data and related study documents, including the study protocol and the statistical analysis plan. Requests will be reviewed for scientific merit, product approval status, and conflicts of interest. Patient level data will be de-identified, and study documents will be redacted to protect the privacy of trial participants and to protect commercially confidential information. Please email USMedInfo@tevapharm.com to make your request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Robinson, D.G., Suett, M., Wilhelm, A. et al. Patient and Healthcare Professional Preferences for Characteristics of Long-Acting Injectable Antipsychotic Agents for the Treatment of Schizophrenia. Adv Ther 40, 2249–2264 (2023). https://doi.org/10.1007/s12325-023-02455-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02455-8