Abstract
Introduction
The SARS-CoV-2 virus pandemic has accelerated the growing trend towards using home- and remote-based medical testing (H/RMT). The aim of this study was to gather insights and explore the opinions of patients and healthcare professionals (HCPs) in Spain and Brazil regarding H/RMT and the impact of decentralised clinical trials.
Methods
This qualitative study consisted of in-depth open question interviews of HCPs and patients/caregivers followed by a workshop that aimed to determine the advantages and barriers to H/RMT in general, and in the context of clinical trials.
Results
There were 47 participants in the interviews (37 patients, 2 caregivers, 8 HCPs) and 32 in the validation workshops (13 patients, 7 caregivers, 12 HCPs). The main advantages for the use of H/RMT in current practice were the comfort and convenience, the ability to improve the relationship between HCPs and patients and personalise patient care, and the increased patient awareness towards their disease. Barriers to H/RMT included accessibility, digitalisation, and the training requirements for both HCPs and patients. Furthermore, according to the Brazilian participants, there is a general distrust in the logistical management of H/RMT. Patients indicated that the convenience of H/RMT did not influence their decision to participate in a clinical trial, with the main reason for participating in a clinical trial being to improve health; however, H/RMT in clinical research does aid adherence to the long-term follow-up associated with trials and provides access to patients living far from the clinical sites.
Conclusion
Insights from patients and HCPs suggest that the advantages of H/RMT may outweigh the barriers, and that social, cultural and geographical factors and the HCP–patient relationship are critical aspects to be considered. Moreover, the convenience of H/RMT does not appear to be a driver for participating in a clinical trial but can facilitate patient diversity and study adherence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Why carry out this study? |
Facilitating patient participation in their treatment and clinical research, and increasing patient diversity is of utmost importance for clinical research performance. |
One way to facilitate patient participation is to accelerate the digitalisation of healthcare systems and telemedicine. |
The aim of this qualitative study was to gather insights and explore the opinions of patients and healthcare professionals (HCPs) on using home- and remote-based medical testing (H/RMT) in current practice, as well as in clinical trials. |
What was learnt from the study? |
The main advantages for the use of H/RMT were the comfort and convenience to patients, the ability to improve the relationship between HCPs and patients and personalise patient care, and to increase patient awareness towards their disease. |
Barriers to H/RMT included accessibility, and the training requirements for both HCPs and patients. |
The advantages of H/RMT outweigh the barriers, and social factors as well as the HCP–patient relationship, are important aspects of H/RMT. |
Moreover, the convenience of H/RMT does not appear to be a driver for participating in a clinical trial but can facilitate patient diversity and study adherence. |
Introduction
Facilitating patient participation in clinical research and increasing patient diversity in clinical trials is of utmost importance for clinical research performance. The SARS-CoV-2 virus pandemic has changed healthcare (including clinical trial research) in many ways, including accelerating the digitalisation of healthcare systems and telemedicine. These changes can also be seen in clinical trials, which, over the last few years, have moved from the traditional investigator/site-centric approach to a more patient-centric approach that allows remote patient participation [1,2,3,4]. With the rise of partially or fully decentralised clinical trials [5], it is essential to know patients’ preferences for their care. The rate of technological failure when digitalising healthcare processes can be high, while studies have shown that the involvement of patients and other users may help reduce the risk of these failures [6,7,8]. For this reason, it seems reasonable to determine whether a patient has a preference for home- or remote-based medical testing (H/RMT), and their acceptance of these testing methods, or whether tests performed in the traditional way (in hospital) are more desirable and the reasons behind these opinions.
While several articles describe how the trial process is changing and the benefit of patient involvement in the design of clinical trials [1,2,3,4, 6,7,8,9,10,11,12], little evidence describes the actual experiences of patients in clinical trials [13, 14] and none describe the experience of patients in clinical trials with H/RMT. Instead, there is abundant literature on home-based rehabilitation, as well as home-based monitoring of symptoms and delivery of medicines [15,16,17,18].
To explore patients’ views on H/RMT and decentralised clinical trials, and the impact of different healthcare systems, cultures, geographic areas, ethnic diversity, and digital access on patient experiences with these, a qualitative study was conducted in Spain, a country with a universal social security-funded healthcare system, and Brazil, a country with lower per capita income. The aim of this study was to (1) explore the emotional, technological, and socio-cultural barriers that might discourage patients from undergoing medical tests at home, as well as the positive aspects of H/RMT identified by the patient; (2) understand the motivational components and expectations of patients who agree to participate in a remote clinical trial; (3) understand how this change to decentralised clinical trials with H/RMT influences patients’ expectations, as well as their willingness to participate in these trials; (4) understand the implications for participants in clinical trials conducted at home and/or remotely; (5) explore whether, in the context of a clinical trial, the acceptability of H/RMT may change; and (6) explore the implications of H/RMT for healthcare professionals (HCPs) and their organisations.
Methods
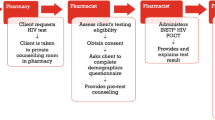
This qualitative, exploratory, and descriptive study was conducted in three stages (Fig. 1). Firstly, a literature review was carried out to identify any gaps in the current literature regarding decentralised clinical trials. This was followed by in-depth interviews of HCPs and patients regarding their experience of H/RMT, and a workshop to validate the findings of these interviews.
For this study, home-based medical tests were defined as tests in which an HCP goes to the patient to carry out the collection of biological material or the measurement of vital signs and other variables, while remote-based tests were defined as all tests where the patient collects their materials or measurements themselves. Tests and procedures that could be performed off-site and mentioned in the interviews or discussed during the workshops included sampling (blood, urine, faeces, saliva), procedures (electrocardiogram, ambulatory blood pressure measurement), teleconsultation, home delivery of medication, electronic questionnaires (patient reported outcomes [ePRO] or clinical outcome assessments [eCOA]), as well as collection of electronic informed consent forms. The clinical variables that could be assessed/measured via H/RMT that were mentioned in the interviews or workshops included vital signs and variables such as blood pressure, body temperature, heart rate, weight, and height.
Participants for these interviews and workshops were recruited through the research institution Instituto Experiencia Paciente (Spain) and the contract research organisation Patient Centricity Consulting (Brazil). The study complied with all national and international ethical recommendations and the ethical principles outlined in the Helsinki Declaration of 1964, and its later amendments. In Spain, the study protocol was approved by the Comité de ética de la Universidad Rey Juan Carlos (2505202114621). In Brazil, the study protocol was approved by the ethics committee of the University of Passo Fundo (opinion number 5.056.469 and CAAE 49172921.9.0000.534), as per the specifications of Resolution 466, of December 12, 2012. All participants provided written informed consent before study inclusion.
Literature Review
A literature review was performed between July 5 and July 30, 2021 using the PubMed and Google Scholar databases to identify any literature investigating patient or physician opinions on remote clinical trials, home- and remote-based medical tests, as well as the most commonly used home- and remote-based clinical trial procedures. Search terms included “hospital-at-home”, “home care”, “patient centred care”, “decentralised”, “decentralised clinical trial”, “clinical trial”, and “home based medical testing”. Papers were limited to those published from 2011 onwards.
The literature was filtered by Simón Balanza and Catalina Peña, from the Instituto Experiencia Paciente, and relevant studies were selected.
In-Depth Interviews
Interview 1: Healthcare Professionals
Based on the gaps in knowledge identified in the literature review, a semi-structured script for an interview was created to collect first-hand and up-to-date information on the opinions and experience of HCPs with H/RMT in Spain and Brazil (see Supplementary Materials S1 in the Electronic Supplementary Materials for the English translation of the script used). The duration of the interviews was approximately 45–60 min, and the interviews were conducted using the GoogleMeet® or Zoom® videoconference platforms.
These in-depth semi-structured interviews explored the level of knowledge and experience about how H/RMT could be performed, the conditions under which H/RMT could be carried out, the perceived advantages and disadvantages of H/RMT in clinical trials, the HCPs perception of patient experiences with H/RMT, and how this differs from conventional clinical trials. The aim of having open-ended questions was to encourage the collection of subjective data, perceptions and reasoning of the HCPs interviewed.
Interview 2: Patients and Caregivers
The interviews with HCPs led to the creation of a script for interviews with patients and caregivers (see Supplementary Materials S2 in the Electronic Supplementary Materials for the English translation of the interview script used). The duration of the interviews was approximately 60–75 min, and the majority of the patient interviews were conducted using GoogleMeet®, with the exception of some participants who did not have access to this platform and were interviewed in person.
Validation Workshops
To conclude the research, an online validation workshop was held to facilitate discussion among patients/caregivers and HCPs to identify which of the research insights were shared by the participants and which ones were not. Another aim of the workshops was to generate consensus between participants on the challenges of H/RMT in clinical trials.
The workshop was divided into three stages:
-
Stage 1 (situation analysis) Participants were separated into two working groups based on whether they were HCPs or patients/caregivers, with the aim of defining the problems and benefits of H/RMT in current practice and in the context of clinical trials.
-
Stage 2 (opportunity identification) Mixed groups of HCPs and parents/caregivers were created to identify causes of problems with H/RMT, describe the impact of these problems on patients, and to identify any opportunities to improve patient experiences and quality of life.
-
Stage 3 (solution proposals) Mixed groups of participants prioritised some of the opportunities identified in stage 2 and used digital tools (online medical solutions, apps, digital self-care solutions) to propose solutions to these problems.
Statistical Analysis
All data were collected, anonymised, and analysed by the contract research organisations who recruited the patients/caregivers and HCPs for the interviews and validation workshops. Descriptive statistics were used to summarise the characteristics of the HCPs and patients/caregivers who participated in the interviews and included number and proportion of individuals. All other data were collated in a qualitative manner.
Results
Literature Review
Overall, 47 articles were identified during the literature search. After filtering, 30 were assessed and 16 considered relevant [1,2,3,4, 6,7,8, 15,16,17, 19,20,21,22,23,24]. The literature review identified some articles discussing decentralised clinical trials [2, 3], where H/RMT was used for data collection [24]; however, limited literature allowed for understanding the value of H/RMT for patients. The scientific literature identified that focuses on H/RMT does so from the perspective of HCPs. Furthermore, there were limited data on patient barriers to H/RMT. The main advantages of H/RMT were related to patient comfort and working with older patients. However, how this concept of comfort is constructed and what it implies in the context of clinical trials was not explored in detail in the literature identified.
In-Depth Interviews
HCP interviews were conducted between July 30 and September 7, 2021 in Spain and between September 28 and October 7, 2021 in Brazil, and patient/caregiver interviews between October 27 and November 20, 2021 in Spain and in Brazil. Overall, eight HCPs (n = 4 each in Spain and Brazil), 37 patients (n = 19 in Spain; n = 18 in Brazil) and two caregivers (in Spain) were interviewed (Table 1). Of the eight HCPs, four were nurses, two were physicians and two were biomedical professionals. The majority (n = 5; 62.5%) practiced in a private healthcare setting. Oncology was the most common area of specialty (n = 4; 50%). Only three HCPs had previous experience of clinical trials (all from Brazil).
The thematic analysis of the interviews with HCPs and patients/caregivers from Spain and Brazil allowed us to group the multiple aspects regarding H/RMT into five different themes: (1) perception of H/RMT as costly from the healthcare system perspective; (2) ability of H/RMT to foster HCP–patient relationships; (3) the impact of H/RMT on communication and follow-up; (4) implications for patient participation in clinical trials; and (5) comfort and work–life balance with H/RMT.
Perception of Home- and Remote-Based Medical Testing as Costly from the Healthcare System Perspective
Participants generally believe that H/RMT is more expensive than traditional testing and, therefore, less readily available. In Spain, it is rare for health institutions to inform patients of H/RMT or to offer it to their patients, and as a result the Spanish patients interviewed believed that this service is reserved for individuals with a disability and, therefore, perceived H/RMT as a privilege.
“I’m telling you, for example, in my case, I can move around, so I don’t think about it either, but I do see that it is a convenience that you can do them at home, right? It’s always a convenience, but that’s what I said before. As I can move around [...] So doing tests at home is a very good step forward for all people who have reduced mobility.”
-Oncology patient with no experience in H/RMT
In Brazil, patients had a similar perception and labelled H/RMT as a luxury and typically did not consider requesting this service.
Furthermore, patients feel responsible for the costs being spent on helping them when they do not see themselves in need of help. Even when doctors offer them home care, some patients in Spain reported that they have refused it in order to spare the healthcare system unnecessary expenditure.
Ability of Home- and Remote-Based Medical Testing to Foster HCP–Patient Relationships
Participants in our interviews spoke about how H/RMT better facilitates the fostering of a positive relationship between patients/caregivers and HCPs than consultations/testing conducted in the traditional hospital setting as it is a less stressful environment for the patient/caregiver. In addition, more time is usually devoted to consultations in the home setting. The change in the HCP–patient relationship and the longer consultation time have an impact on the patient’s peace of mind. As this relationship of trust and reassurance is established between HCPs and patients when undergoing H/RMT, patients are more likely to raise any concerns they may have than during hospital consultations, and these can also be addressed more easily. It should be acknowledged that the HCPs conducting home visits are not likely to be the same HCPs as those working in the hospital setting administering in-hospital testing. Nevertheless, the relationship that develops in the setting of the home is one of the aspects of H/RMT most appreciated by both patients and HCPs. In Brazil, the need for instructional, logistical and technological support was also mentioned as important for patient acceptance of H/RMT. In Spain, the doctor–patient relationship seems to be very important for the acceptance of H/RMT and, in Brazil, human contact is seen as essential.
“In fact, I would say that it is better at home. I don’t know why, I also told the nurses who came to see me that they were very nice, very attentive and so on. They treat you, you are seen as a number as you do there (at the hospital), there they go from one room to another, here it’s much more personal [...] Here they come into your house and a conversation takes place, however small it may be. That’s why I tell you that the contact is much more personal, much more, much better at home than there.”
-Oncology patient with experience in H/RMT
“They treated me as my mother, my father, my sister could have treated me. A very affectionate and very professional and very close treatment. For me it is the most important thing.”
-Oncology patient with experience in H/RMT
Impact of Home- and Remote-Based Medical Testing on Communication and Follow-up
The patients interviewed believe that if teleconsultation was used more widely, avoiding the requirements for the physical presence of a doctor, this would help avoid overcrowding in healthcare centres. In patients with chronic illnesses, teleconsultation also positively affects people’s working lives because they are better able to accommodate teleconsultations around their work schedule, typically with no loss of working hours, and teleconsultations allow them to discretely manage their disease, experience less fatigue, and maintain a better social environment at work. Teleconsultation also alleviates the need for elderly or immobile patients to depend on their caregivers or children to go to the doctor’s office.
On the other hand, patients who have had continuous follow-up via telephone said that teleconsultations are fine, provided they were complemented with face-to-face visits. During our interviews, we found that patients undergoing remote medical testing were often afraid of misinterpreting their results without a doctor present. In addition, patients with experience in teleconsultation said that at times they need human contact, for example when a physical examination is needed, and that a combination of both teleconsultation and in-person consultations is ideal. For patients with chronic illnesses—where the need for consultations is long-lasting—it is essential that patients have frequent communication with their doctors to resolve queries.
Telemedicine has become a fundamental way to provide regular and reliable patient monitoring by performing periodic or repetitive tests at home without the presence of an HCP, and without the need to always go to the hospital. However, elderly patients have mentioned that it is difficult for them to deal with technology.
“I would like the consultations to be like you and me, online. For example, I live a bit far away, but this Tuesday I had to go to the hospital, the consultation lasted 8–10 minutes and it was only about how the drug was, how the blood and stool tests went. And the doctor said “Fine, fine. We continue like this”. It would be a great saving of money and time… doctors who can dedicate themselves to other things and provide a better service. I would choose telemedicine, if there is no need to go on-site.”
-Crohn’s patient with no experience in H/RMT
Implications for Patient Participation in Clinical Trials
Participants in our interviews cited a desire to improve their health as the main reason for participating in a clinical trial. The need to find a solution to their health problem is so strong that patients tend to worry less about possible treatment side effects or study burden. However, the use of H/RMT in clinical trials could increase patients’ access, as well as adherence to the study, particularly in long-term follow-up.
“I think the decision to participate in the clinical trial does not depend on whether the study is at home. If they want to participate, they come to the centre. We talk about patients participating, even if the main motive is to help science [...] The main motive is ‘I need a treatment because, for this problem I have, there is no other solution’.”
-HCP with clinical trial experience
“It can be better coordinated with our life without so much disruption. In the end it’s a thousand kilometres of displacement what we would be doing with it... Better remotely, because it disrupts your life less. No, you don’t have to travel. It’s easier to coordinate with everything.”
-Patient with clinical trial experience
Comfort and Work–Life Balance with Home- and Remote-Based Medical Testing
“Comfortable” was the main adjective used by patients to describe H/RMT. Patients perceived this comfort as a way to counteract the feelings of being overwhelmed or anxious that can be associated with repeated testing. But, it is also linked simply to the possibility of staying at home and not having to move around, which can be stressful, especially for patients with mobility problems, as well as for individuals who rely on the assistance of others (such as minors or the elderly). Finally, the idea of being able to return to their daily life as soon as possible adds to the comfort of H/RMT.
While the loss of comfort does not affect the decision to participate in a clinical trial, it can be an important factor in deciding whether to continue in a clinical trial when the patients’ expectations are not being met.
Participation in clinical trials with home-based blood collection and vital sign testing allows for participating patients to take their children to school. Also, in the case of patients without other dependents and with work responsibilities, the use of H/RMT helps avoid testing interfering with work because it is less time consuming than travel to/from a clinic/hospital.
“Listen sir, it’s very comfortable, to be honest, because you get him up and then he’s at home, you put his breakfast on, you don’t have to be there, come on, get dressed, come on, run. All that adds stress. It’s really not the same to be at home waiting for someone to come and then [...] Come on, I’m going to get him dressed. ‘Come on, let’s go, get in the car, come on, get down, this...’ He’s already a bit nervous to see how everything is going to go, and if you have to move around, it’s better at home, because everything adds stress.”
-Caregiver with experience in H/RMT
Validation Workshops
The validation workshops were conducted online on November 19, 2021. Overall, 12 HCPs (n = 6 each in Spain and Brazil), 13 patients (n = 7 in Spain; n = 6 in Brazil) and seven caregivers (n = 4 in Spain; n = 3 in Brazil) participated in the validation workshops (Table 2).
In Spain and Brazil, the workshops validated most of the content raised in the interviews. Both in current practice and in clinical trials, H/RMT is well accepted by patients, caregivers and HCPs. The ability of HCPs to personalise care to individual patients when using H/RMT versus traditional testing is desirable (with the obvious caveat of still meeting protocol criteria when a patient is participating in a clinical trial). Furthermore, the use of H/RMT requires that the overall reliability and quality of results from decentralised laboratories or in-house medical tests is improved, as well as HCPs competence in managing H/RMT. Shared decision-making between the patients/caregivers and their HCPs would be the most appropriate scenario to improve patients’ experience and care.
HCPs reported that home testing is advantageous to patients but can be difficult for HCPs to implement because of a lack of training and resources. Remote testing was regarded as positive, but more problematic than clinic-based testing as a result of the training needed for both the patients and HCPs. Home administration of intravenous medication is almost non-existent. Patients welcome it, but HCPs warned about the difficulties associated with patient self-administration. To improve adherence to both protocols and treatments in clinical trials, the HCPs highlighted the need to provide good information to patients and the importance of smart use of communication channels (such as apps, ad hoc study portals, phone reminders, etc.). Feedback on patient progress was also identified as a key element to help avoid patients from dropping out early from a clinical trial.
Patients in both countries mentioned that it is difficult to access H/RMT, and this represents the main administrative barrier to its more widespread use. Typically, hospitals and healthcare centres fail to inform patients about the option to use H/RMT or home drug delivery. Social barriers to the acceptance of H/RMT included stigmatisation of home-based medical care due to it typically being associated with palliative care, or lack of confidentiality when HCPs arrive in ambulances or branded home-care cars. Furthermore, when considering adopting H/RMT, many patients reported they felt the need to have a very clean home when HCPs arrive (which is seen as a stress factor), and that they felt a lack of privacy with an HCP in their home. Finally, logistical barriers to adopting H/RMT included that most patients do not want to have access to H/RMT in a clinical trial involving injectable medications, fear of side effects and, depending on the test or patient circumstances, whether patients would feel safer in a hospital. Furthermore, patients mentioned their insecurities in performing remote tests (mainly due to a lack of training). In Brazil, patients who had participated in clinical trials stated that they had mistrust concerning the handling and logistics of processing of H/RMT samples.
The main advantages for H/RMT are that HCPs have more time for resolving any doubts that a patient may have, and H/RMT allows for an increased patient awareness towards their disease. The social advantages are the sense of safety and comfort patients feel at home and the fact that home care seems more personal, allowing for personalised care as well as developing the patient–HCP relationship. Furthermore, H/RMT reduces the burden on patients in terms of balancing their personal and professional lives. The main logistic driver for accepting/adopting H/RMT is that the need to travel to hospital is avoided, which is important not only for elderly or disabled patients but also for those with chronic conditions who require frequent hospital visits or live far from the hospital.
“If they are one of those people who are afraid of needles, if I had to do an extraction they would relax, because as they are at home, they feel comfortable, because they are in their comfort zone. Their home is their comfort, at their temperature, in their comfortable clothes, and that’s where I adapt, isn’t it?”
-Physician
Differences Between Spain and Brazil in Accessibility and Perceptions of Home- and Remote-Based Medical Testing
In Brazil, the majority of the patients interviewed had private healthcare, while in Spain all patients had access to the national public healthcare system. Because of this, some differences in the perceived or actual difficulties in accessing H/RMT were seen between the countries, both in the general context and in the context of clinical studies. However, participants in both Spain and Brazil agreed on the convenience and privilege of H/RMT, with some believing that such services are only for certain people, such as the elderly, bedridden or disabled.
In Brazil, HCPs and patients do not fully trust the results of examinations in the context of clinical trials if they are not collected at the research centre involved in the trials, due to the problems with transport, risk of sample loss, misuse, etc. This differs from Spain where patients fully trust the process. In both countries, patients are grateful to be included in clinical trials, with the main motivation to participate being the possibility of better treatment for their disease/illness as well as better follow-up. Altruistic reasons were secondary to their desire to help themselves. In Brazil, patients mentioned that some family members and friends do not offer their support when the patients join a clinical trial, which was not disclosed by the participants in Spain. In Spain, patient associations are well established, and participants believed these associations have good knowledge of the specific disease and of patients’ rights. In contrast, there appears to be room for improvement in Brazil with regards to the creating and running of patient associations.
Discussion
This qualitative study explored the experiences of HCPs and patients/caregivers in Spain and Brazil with H/RMT and their perception of the utility of H/RMT in general and in clinical trials (Fig. 2). The main advantages for the use of H/RMT were the comfort and convenience for patients, the facilitating of contact with an HCP and personalising patient care, the increased patient awareness towards their disease, and limitation of geographical barriers to the hospital. Barriers to H/RMT included difficulty accessing H/RMT services, as well as the training requirements for both HCPs and patients. Furthermore, in Brazil, there is a general distrust among clinical trials participants in the logistical management of H/RMT. Patients indicated that the convenience of H/RMT hardly influences their decision to participate in a clinical trial, because the main reason for participating in a clinical trial is to improve their health; however, they acknowledged it helps with adherence to the long-term follow-up associated with trials.
One of the main issues identified in this study was the need for good interpersonal communication and trust between HCPs and their patients, and the need to maintain the continuity of the HCP attending the patient. This has also been demonstrated in the literature; for example, a qualitative study investigating the experience of patients with diabetes reported that in the absence of a good relationship with their doctor, patients were reluctant to talk to their doctor about their self-care behaviour because of embarrassment and their fear of being judged for their diet and weight [23]. In other cases, poor communication between patients and HCPs may result in patients not attending medical appointments [25,26,27].
It is important to encourage patients to take responsibility for H/RMT in current practice in order for it to be a success. In this respect, we found that a personable and understanding approach by HCPs can be decisive in making patients more willing to use H/RMT and committed to their self-care. The available evidence shows that this is especially important for patients with chronic illness, such as chronic obstructive pulmonary disease [19]. In addition to the improvement in communication between HCPs and patients, there is a need to improve the messages and information conveyed by HCPs. If patients feel that their HCPs do not provide clear information or are indecisive, the safety of the patient can be compromised, and this may lead to doubts and insecurities in the patient [20].
Fraze and colleagues [21] have emphasised that home visits are seen as an opportunity for caregivers to be more supportive, to establish a care plan, to address questions about medication that the patient may have, and to adapt the home environment to the patients’ needs. The present study further explores this aspect by highlighting that the participants believed that H/RMT humanises patients, allows patients and HCPs more time to develop a personal relationship, and provides a better avenue for patients to ask any questions they may have about their illness or disease. In this sense Kannai and Alon [22] report that HCPs have to leave their comfort zone and get to know the patient’s home, culture, and worldview.
Our research identified some practical implications for future clinical trials. When designing a study, considering patients’ needs is essential. A hybrid trial model, which provides a combination of H/RMT and on-site medical testing, is ideal. The hybrid model can employ either a pre-defined plan for H/RMT and on-site visits based on the study chronology (for example by prioritising first visits as on-site visits, and then moving to remote visits for follow-up) or leave it up to the HCPs and patients to work out the balance between H/RMT and face-to-face visits. It is essential that study procedures are not complex when using H/RMT in a clinical trial, and that use of H/RMT does not require adaptation of the study phase or endpoints. As noted by other investigators [28,29,30], there is evidence that H/RMT can be used to assess adverse effects as well as efficacy in clinical trials; this use of H/RMT should be considered in future trials. Furthermore, when implementing H/RMT in clinical trials, it is important to consider cultural differences between countries (including the trust patients have in their healthcare system and accessibility to technology), as well as differences in participating patients’ profiles (indication, age). In general, and in the context of clinical trials, training of both HCPs and patients in H/RMT is essential and should include methods to improve communication between both parties to increase trust. Finally, use of a tool, such as the Patient Group Engagement Prioritization Tool that was developed by the Clinical Trials Transformation Initiative to assist in the development of medicinal products [12], may facilitate collaboration between clinical trial sponsors and patient groups, leading to meaningful and mutually beneficial collaboration in the context of decentralised clinical trials.
Our study has some limitations, some of which are inherent in the qualitative nature of this study, as well as its relatively small sample size. The majority of patients included in this study did not have prior experience in clinical trials or with H/RMT, similar to patients who typically participate in such trials; thus, any opinions expressed in the interviews and workshop were based on expectations rather than experience. Furthermore, the patients who participated in this study generally had good access to technology, which may not be representative of the whole population of their respective countries, although this is difficult to assess because of limited data on patient characteristics, and should be considered in a new model. An additional barrier that we did not investigate was the impact of patient literacy level on the ability of patients to follow instructions provided by the medical team. Also, the inclusion of HCPs in the workshops may have had some influence on the opinions expressed by the patients. Finally, the perspective of children regarding H/RMT was not investigated (although interviews with two caregivers of children with fibrodysplasia ossificans progressiva who participated in clinical trials indicated that the use of home tests meant that the children’s routine was not markedly interrupted). Taken together, these limitations reduce the generalisability of our findings to patients with different indications, ages, literacy levels, access to technology, ethnicity, and from different countries and healthcare systems versus the patients included in our study.
Conclusions
There is a high acceptance among patients and HCPs of the relevance of H/RMT in current practice. Although some barriers were identified, these tend to be related to administrative or logistical issues related to testing, rather than to patient or HCP acceptance of using H/RMT. Sometimes accessibility to H/RMT is limited, and the support patients require may be increased with H/RMT, particularly if patients do not receive sufficient information or access to telemedicine if they need to resolve any questions or doubts they may have. In our view, the interviews and workshop highlight that training of both HCPs and patients on how to conduct H/RMT is essential, as well as ensuring consistency between HCPs with whom patients have contact. In the context of clinical trials, we have observed that there is great acceptance of the implementation of home testing; however, it is not a priority for patients. In this case, the prevailing priority is the search either for medicines to improve their health or for better treatment of their illness. Nevertheless, while H/RMT does not appear to influence a patient’s decision to participate in a clinical trial, it does provide an incentive for them not to drop out of the clinical trial if they do participate. An important factor for the implementation of H/RMT in the clinical trial context is that, in general, patients and caregivers should have confidence in the conditions under which the trial is run, although in Brazil this confidence is not as complete as in Spain. The capacity to adapt to different patient expectations appears to be a definitive factor for the success of decentralised clinical trials in the future.
References
Brezing CA, Luo SX, Mariani JJ, Levin FR. Digital clinical trials for substance use disorders in the age of COVID-19. J Addict Med. 2020;14:e297–302.
Dahne J, Tomko RL, McClure EA, Obeid JS, Carpenter MJ. Remote methods for conducting tobacco-focused clinical trials. Nicotine Tob Res. 2020;22:2134–40.
Goldsack JC, Izmailova ES, Menetski JP, Hoffmann SC, Groenen PMA, Wagner JA. Remote digital monitoring in clinical trials in the time of COVID-19. Nat Rev Drug Discov. 2020;19:378–9.
Izmailova ES, Ellis R, Benko C. Remote monitoring in clinical trials during the COVID-19 pandemic. Clin Transl Sci. 2020;13:838–41.
Parkins K, Hillman A. 2022 forecast: decentralised trials to reach new heights with 28% jump. 2021. https://www.clinicaltrialsarena.com/analysis/2022-forecast-decentralised-trials-to-reach-new-heights-with-28-jump/. Accessed 16 Aug 2022.
Stichler JF. Patient-centered healthcare design. J Nurs Adm. 2011;41:503–6.
Woods L, Cummings E, Duff J, Walker K. Design thinking for mHealth application co-design to support heart failure self-management. Stud Health Technol Inform. 2017;241:97–102.
Zapata BC, Fernández-Alemán JL, Idri A, Toval A. Empirical studies on usability of mHealth apps: a systematic literature review. J Med Syst. 2015;39:1.
Levitan B, Getz K, Eisenstein EL, et al. Assessing the financial value of patient engagement: a quantitative approach from CTTI’s patient groups and clinical trials project. Ther Innov Regul Sci. 2018;52:220–9.
Lee DJ, Avulova S, Conwill R, Barocas DA. Patient engagement in the design and execution of urologic oncology research. Urol Oncol. 2017;35:552–8.
Sundquist S, Batist G, Brodeur-Robb K, et al. CRAFT-a proposed framework for decentralized clinical trials participation in Canada. Curr Oncol. 2021;28:3857–65.
Perry B, Dombeck C, Smalley JB, et al. Development and application of a patient group engagement prioritization tool for use in medical product development. Ther Innov Regul Sci. 2021;55:324–35.
Lucas R, Wang SF, Riley J, Pepper J, Cowie M. Patient experience in clinical trials: results of a survey. Eur J Heart Fail. 2018;20:612–4.
Bangs R, Crispino T. From the other side: the patient perspective on cancer clinical trials. Urol Oncol. 2019;37:331–5.
Dávila Castrodad IM, Recai TM, Abraham MM, et al. Rehabilitation protocols following total knee arthroplasty: a review of study designs and outcome measures. Ann Transl Med. 2019;7:S255.
Siddiq MAB, Rathore FA, Clegg D, Rasker JJ. Pulmonary rehabilitation in COVID-19 patients: a scoping review of current practice and its application during the pandemic. Turk J Phys Med Rehabil. 2020;66:480–94.
Tverdal CB, Howe EI, Røe C, et al. Traumatic brain injury: patient experience and satisfaction with discharge from trauma hospital. J Rehabil Med. 2018;50:505–13.
Kesavadev J, Basanth A, Krishnan G, et al. A new interventional home care model for COVID management: Virtual Covid IP. Diabetes Metab Syndr. 2021;15: 102228.
Booker R. Effective communication with the patient. Eur Respir Rev. 2005;14:93–6.
Chandra S, Mohammadnezhad M, Ward P. Trust and communication in a doctor-patient relationship: a literature review. J Healthc Commun. 2018;3:36.
Fraze TK, Beidler LB, Briggs ADM, Colla CH. “Eyes in the home”: ACOs use home visits to improve care management, identify needs, and reduce hospital use. Health Aff (Millwood). 2019;38:1021–7.
Kannai R, Alon A. Advantages of home visits in family medicine. Patient Educ Couns. 2018;101:2243–4.
Ritholz MD, Beverly EA, Brooks KM, Abrahamson MJ, Weinger K. Barriers and facilitators to self-care communication during medical appointments in the United States for adults with type 2 diabetes. Chronic Illn. 2014;10:303–13.
Khozin S, Coravos A. Decentralized trials in the age of real-world evidence and inclusivity in clinical investigations. Clin Pharmacol Ther. 2019;106:25–7.
Kaplan SH, Greenfield S, Ware JE Jr. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27:S110–27.
Asan O, Yu Z, Crotty BH. How clinician-patient communication affects trust in health information sources: temporal trends from a national cross-sectional survey. PLoS ONE. 2021;16: e0247583.
Blödt S, Müller-Nordhorn J, Seifert G, Holmberg C. Trust, medical expertise and humaneness: a qualitative study on people with cancer’ satisfaction with medical care. Health Expect. 2021;24:317–26.
Velikova G, Absolom K, Hewison J, et al. Electronic self-reporting of adverse events for patients undergoing cancer treatment: the eRAPID research programme including two RCTs. Southampton: NIHR Journals Library; 2022.
Levine DM, Paz M, Burke K, et al. Remote vs in-home physician visits for hospital-level care at home: a randomized clinical trial. JAMA Netw Open. 2022;5:e2229067.
Maguire R, McCann L, Kotronoulas G, et al. Real time remote symptom monitoring during chemotherapy for cancer: European multicentre randomised controlled trial (eSMART). BMJ. 2021;374:n1647.
Acknowledgements
We would like to thank the patients, caregivers and healthcare professionals for the time and quality of exchange they provided, which made possible the completion of this study.
Funding
Sponsorship for the interviews and validation workshops, medical writing support, and publication of the article including the journal’s Rapid Service and Open Access fees were funded by Servier.
Medical Writing, Editorial, and Other Assistance
Editorial assistance in the preparation of this article was provided by Simone Tait of Springer Healthcare Communications during the drafting of this manuscript, and by Kate Palmer during post-submission revisions. Support for this assistance was funded by Servier.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given final approval of the version to be published.
Author Contributions
Simón Lalanza contributed to the research design and co-ordination, interview design, in-depth interviews, workshop design and conducting, data analysis and report writing. Catalina Peña contributed to the interview design, in-depth interviews, workshop design and conducting, data analysis and report writing. Carlos Bezos contributed to project management and research design. Nancy Yamauchi and Viviane Taffner contributed to the recruitment of patients, in-depth interviews (patients and specialists), data collection, analysis, report writing, workshop co-facilitation and organisation. Viviane Taffner was the researcher responsible for communicating and interfacing with the ethical committee in Brazil. Kelly Rodrigues contributed to the general coordination of the study group in Brazil, workshop organisation and facilitation, and supervising the study reports. Marta García Manrique and Ana Rubio Jareño contributed to the research design and co-ordination and interview design. Andreia Lemos Gil and all other authors critically reviewed manuscript drafts and provided final approval for publication.
Disclosures
Marta García Manrique, Ana Rubio Jareño and Andreia Lemos Gil are full-time employees of Servier. Simón Lalanza, Catalina Peña, Carlos Bezos, Nancy Yamauchi, Viviane Taffner and Kelly Rodrigues declare that they have no competing interests.
Compliance with Ethics Guidelines
The study complied with all national and international ethical recommendations and the ethical principles outlined in the Helsinki Declaration of 1964, and its later amendments. In Spain, the study protocol was approved by the Comité de ética de la Universidad Rey Juan Carlos (2505202114621). In Brazil, the study protocol was approved by the ethics committee of the University of Passo Fundo (opinion number 5.056.469 and CAAE 49172921.9.0000.534), as per the specifications of Resolution 466, of December 12, 2012. All participants provided written informed consent before study inclusion.
Data Availability
Transcriptions of the interviews and the data sets generated and analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lalanza, S., Peña, C., Bezos, C. et al. Patient and Healthcare Professional Insights of Home- and Remote-Based Clinical Assessment: A Qualitative Study from Spain and Brazil to Determine Implications for Clinical Trials and Current Practice. Adv Ther 40, 1670–1685 (2023). https://doi.org/10.1007/s12325-023-02441-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02441-0