Abstract
Introduction
Saudi Arabia has a high prevalence of obesity, which increases the risk of individuals experiencing multiple chronic complications. Only a few publications highlight the healthcare costs of obesity-related complications (ORCs) in Saudi Arabia.
Methods
A micro-costing approach was used to estimate the healthcare costs associated with 10 ORCs. Experienced clinicians in public and private practice across different geographical regions in Saudi Arabia were asked to estimate healthcare resource use associated with each ORC, and estimated unit costs were obtained from hospital administrators. Estimated overall annual costs per patient were calculated as a weighted average of separate public and private sector costs.
Results
Individuals in Saudi Arabia with any single ORC incurred overall average annual healthcare costs of 2165–7558 US dollars (USD). Heart failure, chronic kidney disease, dyslipidemia, and type 2 diabetes (T2D) were the most costly complications, mainly driven by monitoring and/or pharmacological treatment costs. In contrast, asthma, hypertension, and angina were the least costly complications. Costs in private healthcare were higher than in public healthcare; the largest differences (2359–2793 USD) were noted for dyslipidemia, T2D, and osteoarthritis, mainly explained by differences in pharmacological treatment costs.
Conclusions
These data suggest that ORCs result in a considerable financial burden to the healthcare system, and highlight the substantial cost savings that could be achieved by preventing or delaying the occurrence of ORCs in Saudi Arabia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study ? |
Saudi Arabia has a high prevalence of obesity, which increases the risk of individuals experiencing multiple chronic complications. |
Little published information is available on the costs of these complications. We used a micro-costing approach to estimate the healthcare costs associated with 10 obesity-related complications (ORCs). |
What was learned from this study ? |
ORCs result in a considerable financial burden on the healthcare system of Saudi Arabia, and substantial cost savings could be achieved by preventing or delaying the occurrence of ORCs. Healthcare resources used to manage these complications could be reassigned to other priorities, resulting in improved quality of care for all patients. |
A multifaceted nationwide approach, involving policy-makers as well as public and private healthcare providers, is needed to address both weight management and progression of existing complications in people with obesity. |
Introduction
Obesity is abnormal or excessive fat accumulation that presents a health risk [1]. Body mass index (BMI) is a simple weight-for-height index used to define and classify obesity: people with a BMI of at least 30 kg/m2 are considered to have obesity [1]. Obesity is highly prevalent worldwide, and its prevalence continues to increase, particularly in regions with a relatively high gross domestic product (GDP) per capita, such as Western Europe [2], the United States of America (USA) [3], and the Gulf Cooperation Council region [4].
The World Health Survey estimated the overall prevalence of obesity in Saudi Arabia in 2019 as 20.2% [5]. The self-reported rate of obesity in Saudi Arabia in 2020 was approximately 25% [6]. This can be compared to the prevalences in neighboring countries of 27.8% in the United Arab Emirates (2017–2018), 30.7% in Oman (2017), 35.1% in Qatar (2016), 36.9% in Bahrain (2018), 43.7% in Kuwait (2018), as reported by the World Health Organization [7] or the Global Obesity Observatory [8].
Obesity is associated with complications that can have a major impact on health, productivity, and healthcare costs [9,10,11]. For example, type 2 diabetes (T2D) and cardiovascular disease are associated with substantial direct healthcare costs as well as indirect costs arising from impaired productivity [12]. Although the age-adjusted comparative prevalence of diabetes in Saudi Arabia (18.7%) is lower than in Qatar (19.5%) for 2021 [13], the higher population count in Saudi Arabia [14] means that the overall number of people with diabetes is much higher in Saudi Arabia than in Qatar. Evidence from the USA indicates that costs associated with these obesity-related complications (ORCs) are higher in individuals with higher BMI [11]. ORCs such as T2D and hypertension are highly prevalent in Saudi Arabia [15], but there is little information about their impact on healthcare and societal costs. A recent microsimulation analysis predicted there will be over one million new cases of obesity-attributable T2D by 2040 amongst working-age adults in Saudi Arabia, with the cumulative healthcare costs expected to exceed 84.4 billion US dollars (USD) [16]. Obesity and its complications are also a focus of Saudi Vision 2030 [17], a strategic plan to transform multiple sectors, including healthcare, with initiatives to reduce the burden of chronic diseases and their risk factors.
To assess the impact of obesity, we aimed to assess healthcare resource use (HCRU) patterns and the cost burden associated with individual ORCs in Saudi Arabia, using a micro-costing approach.
Methods
Few real-world data on HCRU patterns and the cost burden associated with individual ORCs in Saudi Arabia are currently available. Micro-costing exercises are therefore needed to derive information on the economic costs of ORCs [18], which will in turn assist in planning and executing targeted preventive measures. A micro-costing approach [19, 20], estimating HCRU and costs for 10 obesity comorbidities, was used to estimate the cost of ORCs in Saudi Arabia. Micro-costing utilizes HCRU information and unit cost data to generate detailed estimates of economic costs [19]. Costs in both public and private healthcare settings were estimated.
Complications and Cost Categories
ORCs and the types of costs included were validated using multiple systematic literature reviews and clinical practice guidelines. Treatment pathways, including screening, diagnostics, medications, and complications, were identified via a targeted literature review of recent global and regional clinical guidelines, where available. Keywords relating to each condition and “guidelines” or “systematic review” were used to identify relevant references in PubMed and Google Scholar, which were then used to determine the types of healthcare costs associated with each ORC.
The comorbidities included were T2D, heart failure, angina, hypertension, atrial fibrillation, dyslipidemia, sleep apnea, osteoarthritis, asthma, and chronic kidney disease (CKD). These complications were selected because they are known to be closely linked to obesity [21], and they have been assessed previously in a study from the United Kingdom (UK) examining the effect of weight loss on ORC rates [22]. These ORCs were included because they affect a broad range of organ systems (cardiovascular, metabolic, musculoskeletal, respiratory, and renal). HCRU and unit costs were estimated for the following cost categories: diagnostic tests per patient; scheduled outpatient visits per patient/year; treatments received (plus dose, frequency, and duration); consumables/devices per patient/year; health education programs per patient/year; monitoring tests per patient/year; treatment-related adverse events and complications per patient/year (including inpatient, outpatient, intensive care unit, and emergency room visits); and inpatient procedures per patient/year.
Contributors to Micro-Costing Exercise
HCRU estimates were obtained from medical providers, and unit cost estimates were obtained from hospital administrators or procurement specialists. Respondents were recruited via an independent team and existing networks, supplemented by snowball recruiting. All respondents were required to have been in their current role for 3–30 years. Medical providers were required to be responsible for the care of 10 or more relevant patients per month, and administrators/procurement specialists were required to be knowledgeable about costs in their hospital. Potential participants were screened to ensure that they met these inclusion criteria and were selected to allow a spread of public and private settings from different geographic regions. All respondents indicated that they practiced in hospitals, in public settings (including National Guard hospitals, Ministry of Health hospitals, and military hospitals), private practice, or mixed public/private settings. The surveys, which were internally validated and conducted in line with vendor quality guidelines and ESOMAR guidelines [23], were hosted on the Confirmit platform. They were either self-completed or completed with the assistance of an interviewer between 31 July and 30 September 2021 for medical providers and 13–27 September 2021 for administrators/procurement personnel.
Cost Calculations
Costs were recorded in Saudi Arabian riyals (SAR). The cost of each item within each cost category was calculated separately. For all items, except treatment, the annual cost per patient per item was calculated as the percentage of patients for each HCRU × number of HCRU units per year × unit cost.
The annual cost for each drug class per patient was calculated as the average consumption per day × (30 days × 12 months) × unit cost of treatment × percentage of patients receiving treatment. Averages across multiple medications and brands within each drug class were used to estimate average daily consumption and unit costs. Public sector unit costs were calculated using National Unified Procurement Company tender prices in Saudi Arabia as a reference. For private sector unit costs, if data were not reported in a usable form by the respondent, costs were calculated using the Saudi Food and Drug Authority registration prices.
Separate public and private cost estimates were developed and overall annual costs per patient for each cost item were also calculated as a weighted average of public and private sector annual costs, which were assumed, on the basis of data from health insurance policies, to be distributed 71.84%/28.16% [24]. A total Saudi Arabia population count of 35,013,414 was used in the calculations, based on published estimates for the year 2020 [25].
Following the calculation of unit costs for each comorbidity, the total annual cost per patient per cost category was calculated by summing all cost items and the total annual cost per patient per comorbidity was calculated by adding all cost categories. Cost data are calculated as mean values in SAR or percentage of total costs and presented in USD.
SAR to USD conversions were based on the World Bank average official exchange rates for 2021 (1 USD = 3.75 SAR) [26].
Compliance with Ethics Guidelines
Informed consent was required for participation in surveys, as per the ESOMAR regulations. Participants were asked to provide consent for anonymized data to be included in publications, and were advised that any adverse events or product complaints raised would be reported to the relevant company.
Ethical approval for the survey was not required, according to the Rules Governing the Ethics of Scientific Research practice by King Saud University in Saudi Arabia [27], whereby ethical approval for certain types of studies is waived by the Institutional Review Board. These include studies that do not involve patients or patients’ data, and those where the privacy of the participants is preserved.
This study was performed in accordance with the Declaration of Helsinki (1964).
Results
Thirteen administrators or procurement specialists contributed estimates for unit costs. The numbers of consultants who contributed HCRU estimates for each complication are shown in Table 1, and a detailed overview of public/private settings and regions is provided in Table 2. Similar numbers of contributors from each field worked in the public and private sectors, ensuring that detailed cost estimates for both sectors were obtained. Although every region was represented by at least one contributor, the majority came from Mecca (23 consultants and 6 administration/procurement specialists) and Riyadh (14 consultants and 5 administration/procurement specialists).
Total Costs for Different Obesity-Related Complications
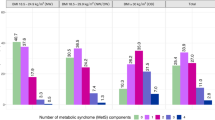
Individuals in Saudi Arabia with any ORC incurred average annual healthcare costs between 2165 and 7558 USD per patient, depending on the complication (Fig. 1). Heart failure was the most costly complication, with an annual per patient cost of 7558 USD. CKD, dyslipidemia, and T2D were each associated with yearly costs per patient of about 4000–5333 USD. Asthma, hypertension, and angina were the least costly complications, incurring approximately one-third to one-half of the costs of the four most expensive complications (Fig. 1).
Comparison of Costs in Public Versus Private Healthcare
For all ORCs, costs in private healthcare exceeded those in public healthcare (Fig. 1). Large disparities between public and private annual costs per patient were observed for some ORCs. For example, for dyslipidemia, T2D, and osteoarthritis, there was a difference of 2359–2793 USD per patient per year between public and private healthcare (Fig. 1). The largest difference between public and private healthcare costs was observed for osteoarthritis: private healthcare costs were 91% higher than public costs. Private costs were also 66% higher than public costs for dyslipidemia, and 61% higher for T2D. For all three complications, differences in pharmacological treatment costs accounted for the greatest disparities in total healthcare costs between public and private healthcare (Fig. 2). Pharmacological treatment costs were 4.8-fold higher in private than in public practice for osteoarthritis, 2.6-fold higher for dyslipidemia, and 2.9-fold higher for T2D.
For other complications, such as CKD, angina, or hypertension, the difference between private and public healthcare costs was smaller, amounting to 535–1222 USD per patient per year. The smallest difference between public and private costs was observed for angina and heart failure; private healthcare costs were 19% higher than public costs. Relative to public costs, private costs were 26% higher for CKD and 27% higher for hypertension. For these four conditions, the costs of treatment, outpatient visits, devices, and diagnostic testing were higher in private than in public healthcare, but this was offset by lower costs associated with treating complications and adverse events and lower costs for inpatient procedures. This resulted in a relatively small difference in total healthcare expenditure between public and private healthcare for these conditions (Table 3).
Cost Drivers
The contributions of different HCRU cost categories to overall total annual healthcare costs for each ORC are shown in Fig. 3. In general, the key cost drivers for most ORCs were treatment, inpatient procedures, outpatient visits, and monitoring tests, but there was substantial heterogeneity across ORCs (Fig. 2). The single largest contributor to heart failure and CKD costs among the nine cost categories was monitoring test costs, contributing 36% of total annual costs per patient for heart failure and 23% of CKD costs. Treatment was the largest cost contributor for dyslipidemia (31% of total costs), T2D (28%), and atrial fibrillation (26%). The largest contributor to sleep apnea costs was inpatient procedures (27% of total costs), whereas outpatient visits were the main cost drivers in angina (34% of total costs), hypertension (32%), and asthma (26%).
Discussion
To address a gap in the evidence on the economic costs of ORCs in Saudi Arabia, we utilized a micro-costing approach to estimate the annual per patient healthcare costs of 10 complications. Data from experts in both public and private settings were collected, and a weighted average was calculated on the basis of recent population estimates for Saudi Arabia [25]. The complications, ordered from the most to least costly, were heart failure, CKD, dyslipidemia, T2D, osteoarthritis, sleep apnea, atrial fibrillation, angina, hypertension, and asthma. For all ORCs, costs in private healthcare exceeded those in public healthcare, but the extent of the differences between public and private costs and the main factors driving these disparities varied by complication.
For most ORCs, the healthcare cost estimates obtained for Saudi Arabia were similar to published estimates from other countries with a relatively high GDP per capita. For example, we estimated the annual per person healthcare costs of CKD to be 5130 USD; costs for the USA have been reported as 7374 USD for 2016/2017 [28], and costs equivalent to 2750 USD were reported in a study in Spain in 2019 [29]. Estimates for asthma in Saudi Arabia in the present study are also similar to those from the USA [30], Greece [31], and Singapore [32]. However, our estimates for asthma [33] and CKD [34] are substantially higher than published estimates from the UK, even considering the earlier dates of the UK estimates. However, costs for heart failure are similar to costs previously observed in the UK [35]. Our estimates for T2D and hypertension are also in line with recently reported global average direct costs for these conditions [36, 37]. Overall, a comparison against published literature suggests that the micro-costing approach utilized in the present study yielded relatively accurate estimates of healthcare expenditure associated with ORCs in Saudi Arabia. Such comparisons, however, should be interpreted with caution, taking into account disparities in healthcare systems, societal factors, and population characteristics between different regions. Future studies comparing the costs of obesity or ORCs between countries or regions should ideally be conducted simultaneously, using a similar approach for gathering and analyzing cost data, and should be adjusted for potential confounding factors.
As expected, the major contributors to the more costly complications in the present study (heart failure, CKD, dyslipidemia, T2D) were costs associated with pharmacological treatment or monitoring. Outpatient visits were the main cost drivers for asthma and hypertension, contributing one-quarter to one-third of total costs, which is in line with observations in other countries [38, 39]. Costs in private healthcare in Saudi Arabia exceeded public healthcare costs for all complications, but the magnitude of difference varied widely, from 19% to 91%, across the different complications. For example, the overall difference between private and public healthcare costs for heart failure was relatively small (19%); costs associated with diagnosis, outpatient visits, and treatment were higher in private than in public healthcare, but costs incurred from inpatient procedures and treatment of complications and adverse events were lower. For osteoarthritis, dyslipidemia, and T2D, costs in private healthcare were 61–91% higher than those in public healthcare, primarily driven by higher treatment costs. Further investigation is warranted into whether the economic disparities across public and private healthcare are associated with differences in clinical outcomes for patients with different ORCs.
The micro-costing approach that we used in this study has recently been described as the preferred approach for settings where direct cost data are unavailable [19]. It has been suggested that micro-costing is superior to the more commonly used gross-costing method because it generates more accurate estimates appropriate for policy purposes [19]; however, a future comparison of these two approaches to assess ORCs specifically would help to strengthen confidence in our approach. Micro-costing in the current study was based on extensive data collection exercises, comprising a nationwide survey with stringent inclusion criteria for participating healthcare providers. Given the current lack of real-world data from Saudi Arabia, these estimates address a key evidence gap, and highlight the broader burden and challenges of obesity and its complications. The details of these estimates, including the public–private disparities and the main cost drivers for the different complications, are relevant to patients, physicians, and payers. These estimated costs may be helpful as model inputs to assess the impact of ORCs in Saudi Arabia and, as such, can be used to direct future research and inform targeted preventive measures against obesity and its complications.
This study did not focus on the costs of treating or managing obesity, nor did it focus specifically on people living with obesity when estimating the costs of treating complications; rather, the analysis represents an attempt to estimate treatment costs for multiple conditions that are frequently comorbid with obesity. Real-world data for these conditions are, in some cases, scarce, but are vitally needed to inform economic assessments and policy relating to obesity and ORC management in Saudi Arabia. However, it should be noted that the costs derived in this study are estimates rather than database-derived actual costs across Saudi Arabia. Consequently, these estimates, which only cover 1 year, may not be generalizable to specific time periods or patient populations, and may also be affected by idiosyncrasies, recall bias, or missing data relating to specific hospitals and clinics where contributors are based. Although the study included a comprehensive range of ORCs, various conditions that are linked to obesity, such as cancer, gallstone disease, polycystic ovary syndrome, and non-alcoholic fatty liver disease, were not included. Obtaining cost estimates for these conditions in future would allow even more accurate characterization of the costs of obesity and ORCs. Finally, it should be noted that the present study only estimates the direct costs of ORCs and does not consider indirect costs due to lost productivity or early retirement. The indirect costs associated with many ORCs are of similar magnitude to direct costs; for example, the range of direct and indirect costs overlapped in systematic reviews of the costs of osteoarthritis [40] and T2D [41], and substantial indirect costs of ORCs were recently reported in Saudi Arabia [42]. In future, prospectively conducted studies using patient registries would be a valuable means of obtaining longitudinal data on the direct and indirect costs associated with a wider range of ORCs over time, and would allow for the collection of more detailed data on patient demographics and clinical characteristics, which would aid in identifying drivers of costs in obesity.
Conclusions
Based on the conservative approach adopted in this study, our findings suggest that ORCs result in a considerable financial burden to the healthcare system of Saudi Arabia. Significant cost savings could be achieved by preventing or delaying the occurrence of ORCs. Healthcare resources used in managing these complications could be reassigned to other priorities, resulting in improved quality of care for all patients in Saudi Arabia. A multifaceted nationwide strategy, involving policy-makers as well as public and private healthcare providers, is needed to address both weight management and progression of existing complications in people with obesity.
References
World Health Organization. Health topics—obesity. https://www.who.int/health-topics/obesity#tab=tab_1. Accessed 24 Mar 2022.
Janssen F, Bardoutsos A, Vidra N. Obesity prevalence in the long-term future in 18 European countries and in the USA. Obes Facts. 2020;13(5):514–27.
Mitchell NS, Catenacci VA, Wyatt HR, Hill JO. Obesity: overview of an epidemic. Psychiatr Clin North Am. 2011;34(4):717–32.
Balhareth A, Meertens R, Kremers S, Sleddens E. Overweight and obesity among adults in the Gulf States: a systematic literature review of correlates of weight, weight-related behaviours, and interventions. Obes Rev. 2019;20(5):763–93.
Ministry of Health. Kingdom of Saudi Arabia World Health Survey—Final Report Riyadh, Saudi Arabia (updated 2019). https://www.moh.gov.sa/en/Ministry/Statistics/Population-Health-Indicators/Documents/World-Health-Survey-Saudi-Arabia.pdf. Accessed 20 Aug 2022.
Althumiri NA, Basyouni MH, AlMousa N, et al. Obesity in Saudi Arabia in 2020: prevalence, distribution, and its current association with various health conditions. Healthcare (Basel). 2021;9(3):311.
World Health Organization. Prevalence of obesity among adults (age-standardized estimate); 2016. https://apps.who.int/gho/data/view.main.CTRY2450A. Accessed 16 Mar 2022.
World Obesity Federation. Global Obesity Observatory 2022. https://data.worldobesity.org/. Accessed 20 Aug 2022.
Lin X, Xu Y, Xu J, et al. Global burden of noncommunicable disease attributable to high body mass index in 195 countries and territories, 1990–2017. Endocrine. 2020;69(2):310–20.
World Bank Group Report. Obesity—health and economic consequences of an impending global challenge; 2020. https://openknowledge.worldbank.org/bitstream/handle/10986/32383/9781464814914.pdf. Accessed 17 Feb 2022.
Divino V, Ramasamy A, Anupindi VR, et al. Complication-specific direct medical costs by body mass index for 13 obesity-related complications: a retrospective database study. J Manag Care Spec Pharm. 2021;27(2):210–22.
Muka T, Imo D, Jaspers L, et al. The global impact of non-communicable diseases on healthcare spending and national income: a systematic review. Eur J Epidemiol. 2015;30(4):251–77.
International Diabetes Federation. IDF Diabetes Atlas. 10th ed. Diabetes data portal; 2021. https://www.diabetesatlas.org/data/en/. Accessed 24 June 2022.
The World Bank. Population total, Saudi Arabia, 1960–2020. https://data.worldbank.org/indicator/SP.POP.TOTL?locations=SA. Accessed 16 Mar 2022.
Alghnam S, Alessy SA, Bosaad M, et al. The association between obesity and chronic conditions: results from a large electronic health records system in Saudi Arabia. Int J Environ Res Public Health. 2021;18(23):12361.
Alqahtani SA, Saxton J, Coker T, et al. How could different obesity scenarios alter burden of diabetes and liver disease in Saudi Arabia? Poster 165: In: proceedings of the 39th Annual Meeting of the Obesity Society (Obesity Week 2021). Obesity. 2021;29(2):113.
Saudi Arabia Vision 2030, Healthcare Transformation. https://www.vision2030.gov.sa/v2030/vrps/hstp/. Accessed 16 Mar 2022.
Spacirova Z, Epstein D, Garcia-Mochon L, Rovira J, Olry de Labry Lima A, Espin J. A general framework for classifying costing methods for economic evaluation of health care. Eur J Health Econ. 2020;21(4):529–42.
Xu X, Lazar CM, Ruger JP. Micro-costing in health and medicine: a critical appraisal. Heal Econ Rev. 2021;11(1):1.
Frick KD. Microcosting quantity data collection methods. Med Care. 2009;47(7 Suppl 1):S76–81.
GBD Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27.
Haase CL, Lopes S, Olsen AH, Satylganova A, Schnecke V, McEwan P. Weight loss and risk reduction of obesity-related outcomes in 0.5 million people: evidence from a UK primary care database. Int J Obes. 2021;45(6):1249–58.
ESOMAR. Questions to help buyers of online samples; 2021. https://esomar.org/uploads/attachments/ckqqecpst00gw9dtrl32xetli-questions-to-help-buyers-of-online-samples-2021.pdf. Accessed 24 June 2022.
Council of Cooperative Health Insurance. Health insurance indicators. https://www.cchi.gov.sa/en/Pages/default.aspx. Accessed 10 Mar 2022.
General Authority for Statistics Kingdom of Saudi Arabia. Population estimates. Population by age groups, and gender mid year 2020. https://www.stats.gov.sa/en/43. Accessed 10 Mar 2022.
The World Bank. Official exchange rate (LCU per US$, period average)—Saudi Arabia. https://data.worldbank.org/indicator/PA.NUS.FCRF?locations=SA. Accessed 04 May 2022.
King Saud University. Rules governing the ethics of scientific research. As approved by the sixth meeting of the university council on 11/06/1436 H. https://dsrs.ksu.edu.sa/sites/dsrs.ksu.edu.sa/files/imce_images/aklaqyat-sfar-1437.pdf.
Nichols GA, Ustyugova A, Deruaz-Luyet A, O’Keeffe-Rosetti M, Brodovicz KG. Healthcare costs by type of expenditure across eGFR stages among patients with and without diabetes, cardiovascular disease, and heart failure. J Am Soc Nephrol. 2020;31(7):1594–601.
Escobar C, Palacios B, Aranda U, et al. Costs and healthcare utilisation of patients with chronic kidney disease in Spain. BMC Health Serv Res. 2021;21(1):536.
Nurmagambetov T, Kuwahara R, Garbe P. The economic burden of asthma in the United States, 2008–2013. Ann Am Thorac Soc. 2018;15(3):348–56.
Souliotis K, Kousoulakou H, Hillas G, et al. Direct and indirect costs of asthma management in Greece: an expert panel approach. Front Public Health. 2017;5:67.
Finkelstein EA, Lau E, Doble B, Ong B, Koh MS. Economic burden of asthma in Singapore. BMJ Open Respir Res. 2021;8(1):e000654.
Mukherjee M, Stoddart A, Gupta RP, et al. The epidemiology, healthcare and societal burden and costs of asthma in the UK and its member nations: analyses of standalone and linked national databases. BMC Med. 2016;14(1):113.
Kerr M, Bray B, Medcalf J, O’Donoghue DJ, Matthews B. Estimating the financial cost of chronic kidney disease to the NHS in England. Nephrol Dial Transplant. 2012;27(Suppl 3):iii73–80.
Danese MD, Gleeson M, Griffiths RI, Catterick D, Kutikova L. Methods for estimating costs in patients with hyperlipidemia experiencing their first cardiovascular event in the United Kingdom. J Med Econ. 2017;20(9):931–7.
Alzaid A, Ladron de Guevara P, Beillat M, Lehner Martin V, Atanasov P. Burden of disease and costs associated with type 2 diabetes in emerging and established markets: systematic review analyses. Expert Rev Pharmacoecon Outcomes Res. 2021;21(4):785–98.
Wierzejska E, Giernas B, Lipiak A, Karasiewicz M, Cofta M, Staszewski R. A global perspective on the costs of hypertension: a systematic review. Arch Med Sci. 2020;16(5):1078–91.
Kirkland EB, Heincelman M, Bishu KG, et al. Trends in healthcare expenditures among US adults with hypertension: national estimates, 2003–2014. J Am Heart Assoc. 2018;7(11):e008731.
Al Mazrouei K, Almannaei AI, Nur FM, Bachnak N, Alzaabi A. Direct and indirect costs of asthma burden in Abu Dhabi: a retrospective analysis of insurance claims data from 2015 to 2018. Clinicoecon Outcomes Res. 2021;13:969–80.
Xie F, Kovic B, Jin X, He X, Wang M, Silvestre C. Economic and humanistic burden of osteoarthritis: a systematic review of large sample studies. Pharmacoeconomics. 2016;34(11):1087–100.
Seuring T, Archangelidi O, Suhrcke M. The economic costs of type 2 diabetes: a global systematic review. Pharmacoeconomics. 2015;33(8):811–31.
Malkin JD, Baid D, Alsukait RF, et al. The economic burden of overweight and obesity in Saudi Arabia. PLoS One. 2022;17(3):e0264993.
Acknowledgements
The authors would like to thank all the hospital consultants and administrators who have provided data for the study. The authors also thank Ipsos for their contribution to the micro-costing exercise under the guidance of the authors. The findings and views reported in this study are those of the authors.
Funding
This study, the Rapid Service fee and the Open Access fee were funded by Novo Nordisk Saudi Arabia.
Medical Writing and Editorial Assistance
Medical writing support under the direct guidance and contribution of all authors was provided by Amany Elshorbagy PhD of Oxford PharmaGenesis, Oxford, UK, funded by Novo Nordisk Saudi Arabia.
Author Contributions
Hussain A. Al-Omar, Ali Alshehri, Abdulmohsen Abanumay, Hana Alabdulkarim, Ali Alrumaih, Mahmoud S Eldin and Saleh A Alqahtani contributed to the study conceptualization and methods, data interpretation, and manuscript drafting, reviewing and editing.
Disclosures
Ali Alshehri has provided consultancy to Novo Nordisk. Abdulmohsen Abanumay and Mahmoud S.Eldin are employees of Novo Nordisk Saudi Arabia. Hussain A. Al-Omar, Hana Alabdulkarim, Ali Alrumaih, and Saleh A. Alqahtani have nothing to disclose.
Compliance with Ethics Guidelines
Informed consent was required for participation in surveys, as per the ESOMAR regulations. Participants were asked to provide consent for anonymized data to be included in publications, and were advised that any adverse events or product complaints raised would be reported to the relevant company. Ethical approval for the survey was not required, according to the Rules Governing the Ethics of Scientific Research practice by King Saud University in Saudi Arabia, whereby ethical approval for certain types of studies is waived by the Institutional Review Board. These include studies that do not involve patients or patients’ data, and those where the privacy of the participants is preserved. This study was performed in accordance with the Declaration of Helsinki (1964).
Data Availability
All supporting data for this analysis are presented in this manuscript, or are available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Al-Omar, H.A., Alshehri, A., Abanumay, A. et al. The Impact of Obesity in Saudi Arabia: Healthcare Resource Use and Costs Associated with Obesity-Related Complications. Adv Ther 40, 1430–1443 (2023). https://doi.org/10.1007/s12325-023-02426-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02426-z