Abstract
TMPRSS6 is a serine protease highly expressed in the liver. Its role in iron regulation was first reported in 2008 when mutations in TMPRSS6 were shown to be the cause of iron-refractory iron deficiency anemia (IRIDA) in humans and in mouse models. TMPRSS6 functions as a negative regulator of the expression of the systemic iron-regulatory hormone hepcidin. Over the last decade and a half, growing understanding of TMPRSS6 biology and mechanism of action has enabled development of new therapeutic approaches for patients with diseases of erythropoiesis and iron homeostasis.
ClinicalTrials.gov identifier NCT03165864.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Iron is essential for erythropoiesis, and the restriction of iron supply inhibits erythropoiesis. |
Hepcidin, the principal hormone of iron homeostasis, controls dietary iron absorption and plasma iron concentration. |
Hepcidin is negatively regulated by the membrane protease TMPRSS6. |
TMPRSS6 is an attractive target for the treatment of iron and erythrocyte disorders. |
The membrane-associated serine protease TMPRSS6 (also called matriptase 2 or MT2) is predominantly expressed in the liver. Its essential role in iron regulation was established when mutations in TMPRSS6 were shown to be the cause of iron-refractory iron deficiency anemia (IRIDA) in humans and in mouse models [1, 2]. In hepatocytes, TMPRSS6 negatively regulates the expression of the systemic iron-regulatory hormone hepcidin. Increasing understanding of TMPRSS6's biology and mechanism of action has enabled development of new therapeutic approaches for patients with diseases of erythropoiesis and iron homeostasis.
Erythropoiesis
Erythroid Maturation
Erythropoiesis [3] is the process of cell division and differentiation that produces red blood cells (erythrocytes). Erythrocytes are small, specialized end-stage cells which in humans and other mammals are biconcave and full of hemoglobin but lacking a nucleus or other organelles. In the bone marrow, hematopoietic stem cells sequentially divide and differentiate to ultimately generate, among a variety of hematopoietic progenitor cells, the first erythroid lineage-committed progenitors named erythroid burst-forming unit-erythroid (BFU-E) and colony-forming unit-erythroid (CFU-E). These progenitor cells undergo terminal erythroid differentiation, starting with the first morphologically recognizable proerythroblast stage, which sequentially divide to produce basophilic, polychromatic, and orthochromatic erythroblasts. Eventually, orthochromatic erythroblasts expel their nuclei and other organelles to generate reticulocytes that enter blood circulation and rapidly mature to erythrocytes.
Erythropoiesis Is Regulated by the Concentration of Erythropoietin
An essential driver and regulator of erythropoiesis is the cytokine/hematopoietic hormone erythropoietin (EPO). Circulating EPO binds its cognate receptor (EPOR) on erythroid progenitors, triggering multiple signaling pathways that control the survival and maturation of erythroid progenitors. EPO is secreted by specialized hypoxia-sensing interstitial cells in the kidney. Changes in hemoglobin concentration affect oxygen delivery to the kidney, which modulates stability of Hypoxia Inducible Factor-2α (HIF2α), the transcription factor that controls the synthesis and secretion of EPO. This pathway has been targeted with drugs that inhibit prolyl hydroxylases and therefore increase stability of HIFs for treatment of anemia in chronic kidney disease and other inflammatory conditions [4].
EPO-Independent Hormonal Regulation of Erythropoiesis
Although essential for erythropoiesis, EPO is not the only erythropoietic hormone regulating this process. Another unanticipated pathway controlling erythropoiesis has been identified by the use of activin receptor trap ligands (namely sotatercept and luspatercept) that were initially designed to target TGF-ß ligands and improve osteoporosis [5]. These drugs can increase RBC production in normal individuals and patients affected by β-thalassemia and myelodysplastic syndromes (MDS) by a pathway distinct from that of EPO and affecting predominantly the erythroblasts [6]. The molecular mechanisms that underlie the activity of activin traps are not clear. While GDF11-SMAD-mediated signaling was initially hypothesized as the pathway inhibited by activin receptor ligand traps, more recently it has been shown that lack of GDF11 does not improve anemia in WT animals or mice affected by β-thalassemia. Nevertheless, published data suggest strongly that the drugs are likely to target one or more members of the TGFβ superfamily.
Erythropoiesis Is Regulated by the Concentration of Iron
The other principal regulator of erythropoiesis is the amount of iron available to erythroid precursors in the form of diferric or monoferric transferrin (collectively referred to as iron-transferrin or Fe-Tf). Tf is an 80-kDa glycoprotein predominantly synthesized by the liver. Under normal circumstances, 20–45% of the iron-binding sites on transferrin are occupied by ferric iron. The concentration of iron in blood plasma and the storage and distribution of iron in the organism are subject to homeostatic regulation. The main function of Tf is to deliver iron to cells by receptor-mediated endocytosis, carried out by the transferrin receptor TfR1. Although all cells require iron to maintain vital processes, most Fe-Tf is utilized for erythropoiesis, and most TfR1 receptors are located in erythroid precursors. Tf also plays an important role in modulating the sensitivity of the erythroid precursors to EPO, likely by interaction with the second transferrin receptor, TfR2 [7, 8]. Compared to the production of white cells and platelets, the rate of erythrocyte production appears to be preferentially inhibited by decreases in Fe-Tf concentration. The coupling of erythropoiesis to iron supply is achieved through multiple mechanisms that prominently include iron modulation of lineage commitment in bipotent megakaryocytic/erythroid progenitors (MEP) [9] and the modulation by Fe-Tf of EPOR delivery to (pro)erythroblast membranes [10]. Additionally, the production of hemoglobin, by far the predominant protein of erythrocytes, is also sensitive to the concentration of Fe-Tf, which is the sole source of intracellular iron for heme synthesis in erythroblasts. Intracellular iron controls heme synthesis via the iron-regulatory proteins that inhibit translation by binding to the 5′-untranslated region of the mRNA encoding the rate-limiting enzyme of heme synthesis, erythroid-specific 5-aminolevulinate synthase (eALAS, a.k.a., ALAS2) [11]. The intracellular concentration of heme in turn translationally regulates the synthesis of globin chains, coordinating the stoichiometric requirements for normal Hb production [12]. Accordingly, erythrocytes produced under iron-deficient conditions contain less hemoglobin per cell than those produced under iron-sufficient conditions.
Iron Regulation
Normal Systemic Iron Metabolism
The concentration of circulating iron in blood plasma is maintained at 10–30 µM by balancing dietary absorption, storage, and recycling of iron by specialized cells against iron utilization for essential metabolic processes by all cells. The hormone hepcidin is the principal regulator of iron homeostasis [13]. Hepcidin (encoded by the HAMP gene) controls dietary iron absorption and iron recycling by binding, occlusion, and internalization of the sole known cellular iron exporter ferroportin (FPN1); this prevents iron egress from cells into blood plasma. Hepcidin is a small peptide secreted primarily by hepatocytes. The production of hepcidin is induced by iron loading and inflammation and suppressed by iron deficiency and ineffective erythropoiesis. At the cellular level, the regulation of hepcidin by iron is transcriptional and involves multiple interacting proteins, whose role in iron regulation was identified and verified by the disruptive effects of their mutation on iron homeostasis in humans and laboratory animals. These include the transferrin receptors TfR1 and TfR2, hemochromatosis-associated protein (HFE), hemojuvelin (HJV), bone morphogenetic proteins (BMPs), bone morphogenetic protein receptors (BMPR), neogenin and matriptase-2 (TMPRSS6) [14]. These components interact to regulate HAMP gene transcription through BMPR and its SMAD signaling pathway.
Hepcidin Regulation by Iron
Hepcidin regulation by extracellular iron involves Fe-Tf binding to hepatocyte TfR2 that, in part, potentiates the BMP/SMAD signaling pathway and hepcidin transcription in response to iron. The interaction of TfR1 and HFE on hepatocytes is disrupted by Fe-Tf, freeing HFE to enhance signaling through the BMP/SMAD signaling pathway. The specific interactions of the various components with each other and with BMPR are not yet understood in detail. Liver sinusoidal endothelial cells are the primary source of BMP2 and BMP6 and are stimulated to increase the production of BMPs as iron stores increase through mechanisms that are not yet understood. Thus, under high iron conditions BMP2 and BMP6 in the liver initiate heterodimerization between BMP receptors type I (ALK2/ALK3) and type II (BMPRII/ActRIIA).
The Role of TMPRSS6 in Iron Homeostasis
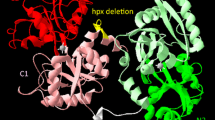
TMPRSS6 is a transmembrane serine protease which is primarily expressed in hepatocytes. TMPRSS6 is a critical negative regulator of the receptor complex that controls hepcidin transcription [15]. The exact mechanism of action of TMPRSS6 is still not understood, but TMPRSS6 interacts with HJV and possibly other components of the BMP receptor complex and acts as both an allosteric inhibitor and a protease that degrades components of the receptor complex [16,17,18]. As a result, TMPRSS6 decreases SMAD1/5/8 signaling and suppresses hepcidin transcription. This facilitates iron absorption and iron release from stores and increases systemic iron availability. Confirming the essential role of TMPRSS6 in iron homeostasis, genome-wide association study (GWAS) analyses have demonstrated that TMPRSS6 variants are associated with differences in red blood cell indices as well as biomarkers of iron homeostasis [19,20,21,22]. TMPRSS6 protein levels increase in response to chronic iron deficiency or erythropoietin treatment in rodents via a posttranscriptional mechanism [23], and this mechanism ensures appropriate hepcidin suppression in conditions of iron deficiency or stimulated erythropoiesis.
Role of the Intestine in Systemic Iron Homeostasis
The intestine is also a critical regulator of systemic iron homeostasis. In addition to renal EPO regulation, HIF2α also plays a major role in iron absorption in the duodenum, in the settings of iron deficiency, erythropoiesis, and in hepcidin deficiency [24,25,26]. Therefore, intestinal oxygen sensing is essential for adaptive increases in iron absorption. In fact, HIF2α, under condition of hypoxia, can upregulate transcription of key enzymes and transporters responsible for duodenal iron absorption, such as the duodenal cytochrome B (DcytB), divalent metal transporter 1 (DMT1), and FPN1 [27].
Iron Overload Disorders
Homozygous or compound heterozygous mutations in HFE, HJV, TFR2, and the HAMP cause the iron overload disease hemochromatosis [28], whose analysis has informed our understanding of iron homeostasis. The common feature of these disorders is inadequate or absent production of hepcidin, causing excessive iron absorption from the diet and dysregulated release of iron from macrophages that recycle iron from senescent erythrocytes. Transferrin may become saturated with iron, resulting in the appearance of non-transferrin-bound iron in circulation, a reactive form of iron wherein iron is bound to citrate or other polyanionic substances. This form of iron is taken up by various organs through alternative iron uptake mechanisms that are not subject to physiologic regulation, causing tissue iron overload and injury. Heterozygous mutations in ferroportin that cause resistance to hepcidin phenocopy the forms of hemochromatosis caused by hepcidin deficiency.
Iron-Refractory Iron Deficiency Anemia (IRIDA)
Mutations in both copies of TMPRSS6 cause a phenotype opposite to hemochromatosis [29]. In IRIDA, hepcidin concentrations in blood are inappropriately high when considered in the context of serum iron concentrations or iron stores. Patients with this genetic disorder are severely iron deficient as indicated by very low serum iron and transferrin saturation. Their erythrocytes are very small (microcytosis) and their hemoglobin concentration is abnormally low. Attempts to treat their iron deficiency and anemia with oral or intravenous iron are at most partially effective as iron is poorly absorbed in the duodenum, becomes trapped in macrophages and is unavailable for erythropoiesis. Although the reported number of cases is relatively small, it appears that erythropoiesis is disproportionately affected, and, despite the severity of iron deficiency in many cases, to our knowledge there have not been any reports of nonhematologic developmental abnormalities in children with IRIDA.
Erythropoiesis Promotes Iron Absorption and Mobilization
Erythropoiesis Modulates Iron Homeostasis
Studies of humans and mice subjected to erythropoietic stimuli such as blood loss or the administration of EPO show that the erythropoietic stimulus results in a sustained decrease of serum hepcidin concentration that begins within hours [30, 31]. By contrast, the decrease in serum iron concentration is relatively minor and transient, indicating that the increased demand for iron induced by the erythropoietic stimulus is met by increased iron mobilization from stores and increased iron absorption, promoted by the drop in hepcidin concentration. The response requires both EPO and a marrow that is capable of erythropoietic response [32], suggesting that the substance that suppresses hepcidin in this setting originates in the marrow. An unbiased search for this substance led to the discovery of erythroferrone (ERFE) [31], a member of the C1q-TNF superfamily of glycoproteins, as an erythroid suppressor of hepcidin. ERFE is secreted by EPO-stimulated erythroblasts and acts on the liver to suppress hepcidin transcription. ERFE appears to act by trapping BMPs secreted by sinusoidal endothelium in the liver [33], and the consequent loss of BMP signaling then decreases hepcidin transcription in hepatocytes. Increase in TMPRSS6 levels after stimulation of erythropoietic activity is likely important for the full ERFE effect considering that loss of TMPRSS6 [34] severely blunts the suppressive effect of EPO and ERFE on hepcidin expression.
Ineffective Erythropoiesis as a Cause of Pathological Hepcidin Suppression and Iron Overload
Ineffective erythropoiesis is defined as decreased production of erythrocytes caused by cell death of differentiating erythroblasts in the marrow so that relatively few erythroblasts reach maturity. The resulting anemia stimulates EPO production, which causes immature erythroblast populations to expand and secrete excessive amounts of ERFE and other erythrokines [35]. High ERFE concentrations suppress hepcidin and cause the hyperabsorption of dietary iron and eventual systemic iron overload. Anemias with prominent ineffective erythropoiesis include β-thalassemia, congenital dyserythropoietic anemias, sideroblastic anemias, and pyruvate kinase deficiency. In these diseases, iron overload develops even in patients who do not receive blood transfusions. Blood transfusions are a rich source of iron (200–250 mg/unit) and become the predominant cause of iron overload in those patients who receive them. By lowering EPO, blood transfusions also transiently decrease ineffective erythropoiesis.
Iron Deficiency Restricts Erythropoiesis
Inhibition of Erythropoiesis by Hypoferremia
Compared to other tissues with proliferating cell populations, erythropoiesis is uniquely sensitive to the supply of transferrin-bound iron [36]. During iron deficiency, the rate of production of erythrocytes is decreased, and the erythrocytes become smaller and contain less hemoglobin. When iron sufficiency is restored by the administration of parenteral iron, the number of erythroblasts in the marrow increases within days followed by the release of reticulocytes into the circulation [37]. The mechanisms that underlie the tight coupling of erythropoiesis to iron availability are still incompletely understood.
Iron Regulates Erythroid Lineage Commitment
Many patients with iron deficiency anemia have an increased number of circulating platelets. Recent studies in mouse models and human hematopoietic progenitors revealed that MEPs exposed to an iron-deficient environment develop metabolic changes that result in MEP bias towards differentiating to megakaryocytes rather than erythrocytes [9, 38]. The receptor that senses iron deficiency in this setting is TfR2, also involved in iron sensing by hepatocytes.
Iron Regulates Erythroid Precursor Sensitivity to EPO
Restriction of iron supply to the erythroid marrow reduces the erythropoietic response to EPO. In this setting, iron deficiency again appears to be sensed by TfR2 [39], which in turn interacts with the receptor control element Scribble [10] to reduce EPO sensitivity by limiting cell surface display of EPOR, impairing erythroid proliferation and survival.
Iron Regulates the Synthesis of Hemoglobin and Other Erythrocyte Proteins
The production of both heme and globin chains is decreased during iron deficiency so that the normal stoichiometry of hemoglobin composition is maintained without excess (potentially cytotoxic) production of any of the components. The production of heme is regulated by iron availability at the level of the first component of the heme synthetic pathway in erythroblasts, the erythroid form of aminolevulinic acid synthase, ALAS2, whose translation is inhibited during cellular iron deficiency by iron-regulatory proteins IRP1 and IRP2 [40]. Under the same conditions, the translation of globin chains and some other erythrocyte proteins is inhibited by heme-regulated inhibitor (HRI, heme-regulated eIF2α-kinase) [41]. Here HRI also cross-talks with the mammalian target of rapamycin (mTOR) pathway to inhibit erythroblast protein synthesis during iron deficiency [12].
Targeting TMPRSS6 for Iron-Restrictive Therapy in Hematologic Disorders
Rationale for Iron-Restrictive Therapy
Iron-restrictive therapy is defined as an intervention that inhibits the absorption of dietary iron and the release of stored iron from macrophages and hepatocytes. This can be achieved by therapeutically raising hepcidin concentrations or by inhibiting ferroportin on the cell membranes in tissues that deliver iron to blood plasma. The expected effect of these interventions is to lower serum iron and transferrin saturation, with secondary effects on erythropoiesis depending on the degree of iron restriction. These pharmacologic effects can be achieved by the administration of hepcidin or hepcidin analogs, or other inhibitors of ferroportin function or expression, or the administration of compounds that stimulate the endogenous production of hepcidin. Approaches taken by different groups (Table 1) differ in mode of action, route, and frequency of administration. In the past years, hepcidin mimetics, RNA and DNA therapeutics against TMPRSS6 including antisense oligonucleotide (ASO) and siRNA, and small molecule ferroportin inhibitor have been tested in various preclinical models of iron overload and hematologic disorders. Several programs have announced promising data in human clinical trials.
Hepcidin Agonists
Hepcidin, or compounds that mimic its action on ferroportin, have been developed for the treatment of diseases characterized by hepcidin deficiency and for diseases where iron restriction is expected to offer therapeutic benefits (Table 1). As a class they validate the targeting of the TMPRSS6 pathway at the level of its sole known nonredundant effector. Rusfertide, a hepcidin-like peptide administered by subcutaneous injection, has shown efficacy in preclinical models of β-thalassemia [42] and polycythemia vera (PV). In Phase 2 trials in human PV, rusfertide was well tolerated and effectively replaced phlebotomy for the control of hematocrit [43]. Patients reported improved symptoms, and adverse events consisted mainly of nonserious injection site reactions. Vamifeport is an orally administered small molecule drug which binds to ferroportin, blocks cellular iron export, and causes ferroportin internalization [44]. Vamifeport induced iron restriction and ameliorated β-thalassemia in preclinical models [45]. In healthy human volunteers, the drug was well tolerated and induced the expected hypoferremic response. LJPC-401 is a peptide drug chemically identical to human hepcidin but formulated for rapid absorption after subcutaneous administration. Treatment of hemochromatosis patients with LJPC-401 significantly decreased the need for phlebotomy, but in another trial in patients with transfusion-dependent β-thalassemia, LJPC-401 did not reduce cardiac iron (primary endpoint) or decrease serum iron concentrations (one of several secondary endpoints). It is possible that LJPC-401 failed to induce iron restriction because of inadequate dosing. Mild to moderate injection site reactions were reported with the drug [46].
TMPRSS6 as a Therapeutic Target
Inhibition of TMPRSS6, the negative regulator of hepcidin transcription, is an attractive option because its effects in humans are exemplified by studies of IRIDA, a genetic disease in which the function of TMPRSS6 is impaired as a result of mutations, most often involving both copies of the gene. From the studies of these patients and related mouse models, it appears that iron restriction is the sole clinical effect of the loss of TMPRSS6 function. As protease activity is not required for hepcidin suppression by TMPRSS6 [16], therapeutic targeting of TMPRSS6 will likely have to focus on decreasing the overall levels of TMPRSS6 or interfering with its allosteric function rather than solely on inhibiting its protease activity. SLN124 and sapablursen target TMPRSS6 by suppressing its synthesis through hepatocyte-targeted siRNA and antisense mechanisms, respectively.
Hemochromatosis
As described in previous sections, hemochromatosis is a group of genetic diseases most commonly caused by absolute or relative hepcidin deficiency culminating in whole-body iron overload. Removal of iron through phlebotomy remains the mainstay of treatment for this disease and consists of an intensive deironing phase with weekly or biweekly removal of 1 unit of blood (approximately 200–250 mg of iron each), typically for a year or more, followed by a maintenance phlebotomy regimen once accumulated iron excess is removed [47].
Mouse Models of Hemochromatosis
In the most common forms of hemochromatosis, pharmacologic restoration of normal hepcidin concentrations is expected to stop the progression of the disease, as has been demonstrated in various mouse models of hemochromatosis. Thus, early replacement of hepcidin in hepcidin-deficient patients, before substantial iron accumulation occurs, would effectively cure this disease. However, because of the low natural rate of iron loss from the body, therapeutic hepcidin replacement does not significantly reverse the lifetime accumulation of iron in various organs. In mouse models of the most common form of hemochromatosis caused by the C282Y mutation in HFE, genetic ablation of TMPRSS6 or its decrease by administration of ASOs or siRNAs prevented development of iron overload [48,49,50,51]. These studies provide the proof of concept that decreasing TMPRSS6 levels is a rational therapeutic approach to increase hepcidin and prevent iron loading in patients with hemochromatosis.
Thalassemias
Forms of anemia such as β- or α-thalassemia are characterized by active proliferation of erythroid progenitors and low hepcidin expression [52, 53]. In particular, in β-thalassemia, mutations in the β-globin gene lead to a relative excess of α-globin, which, together with heme, forms hemichromes, molecules with toxic potential to trigger generation of reactive oxygen species (ROS), apoptosis of erythroid progenitors, and short-lived erythrocytes [54]. This results in anemia, chronically high levels of erythropoietin, and ineffective erythropoiesis—overproduction of erythroid progenitors that fail to generate mature erythrocytes [55]. β-Thalassemia is currently categorized as either transfusion-dependent (TDT) or non-transfusion dependent (NTDT). However, even when transfusions are not required, the manifestations of the disease can be severe, including chronic anemia and splenomegaly as well as pulmonary hypertension and an increased risk of thrombosis [56]. Anemia and ineffective erythropoiesis also cause increased intestinal iron absorption mediated by duodenal hypoxia and erythroid-mediated suppression of the iron regulator hepcidin [27, 55, 57]. The resulting iron overload adds to morbidity by promoting cirrhosis, cardiomyopathy, diabetes, and hepatocarcinoma and exacerbating erythroid cell damage, apoptosis, and ineffective erythropoiesis [54]. Even NTDT patients with β-thalassemia may require iron chelation to avoid the morbidity and mortality associated with severe iron overload [54, 56]. Similar features are also observed in some patients affected by α-thalassemia.
Mouse Models of Non-Transfusion-Dependent β-Thalassemia
The Hbbth3/+ mouse model of β-thalassemia mimics the NTDT condition, showing increased proliferation and decreased differentiation of the erythroid progenitors, apoptosis of erythroblasts due to the presence of toxic hemichromes, reticulocytosis, shorter life span of RBCs in circulation, splenomegaly, extramedullary hematopoiesis, anemia, and iron overload [48, 52]. Treatment of Hbbth3/+ mice with TMPRSS6-ASO (an antisense oligonucleotide directed to TMPRSS6) decreased the formation of insoluble membrane-bound globins, ROS, and apoptosis and improved anemia. These animals also exhibited a significant amelioration of liver iron overload, ineffective erythropoiesis, and splenomegaly and an increase in total hemoglobin levels [48]. Similar results were observed with hepcidin mimetics and siRNA against TMPRSS6 [45, 49, 58, 59]. In addition, TMPRSS6-ASO in combination with iron chelators and erythropoietin-stimulating agents ameliorated ineffective erythropoiesis and iron overload in this model [60, 61]. These data suggest that ASOs targeting TMPRSS6 could be beneficial in individuals with β-thalassemia and related disorders, such as α-thalassemia.
Sickle Cell Disease
In sickle cell disease (SCD), a single base mutation in the globin gene (HBB) generates sickle hemoglobin (HbS), which upon deoxygenation can polymerize within the cell producing the characteristic sickle-shaped erythrocyte that defines the disease. Hemoglobin polymerization, leading to erythrocyte rigidity and vaso-occlusion, is central to the pathophysiology of this disease, but chronic anemia, hemolysis, and vasculopathy also contribute to chronic morbidity and premature mortality. In SCD, there is a delay between deoxygenation and the initiation of sickling that is dependent on the intracellular concentration of HbS [62]. Case reports and small studies have suggested associations among iron deficiency, decreased mean corpuscular Hb concentration (MCHC), and improvement in several clinical parameters, including decreased sickling and hemolysis and decreased hospitalization for pain crises [63, 64].
Mouse Models of Sickle Cell Disease
Additional support for iron restriction as a therapeutic approach has been obtained using mouse models of SCD, where the α- and β-globin genes are replaced by fragments of the human α- and sickle βS-globin loci [65]. In the first study, iron deficiency (consequent to an inactivating mutation of the intestinal Hif2α gene) led to better RBC survival and less severe anemia when compared with iron-sufficient wild-type mice [66]. In the second study, SCD mice were exposed to an iron-restricted diet. Compared to mice fed a standard diet, animals with an iron-restricted diet exhibited decreased serum iron concentrations, decreased MCHC, increased number of circulating RBCs, improved hematocrit (HCT), and reduced sickling under condition of hypoxia [67]. Administration of a small molecule inhibitor of ferroportin, vamifeport, in SCD mice also caused iron restriction and reduced sickling without worsening anemia [68]. Altogether, these observations and studies suggest that iron restriction may decrease the clinical complications arising from both sickling and hemolysis in SCD.
Polycythemia Vera
Polycythemia vera (PV) is a myeloproliferative neoplasm (MPN) characterized by erythrocytosis, thrombocytosis, leukocytosis, and splenomegaly [69]. Almost all patients have a single driver mutation (~ 95% JAK2 V617F) in the Janus kinase 2 (JAK2) gene. The JAK2 V617F mutation results in constitutive activation of hematopoietic signal transduction and exuberant hematopoiesis, leading to the PV-associated symptoms. It is a disorder of the elderly with a median age of onset of ~ 60 years old. PV is a chronic and progressive disorder, and patients often experience worsening of symptoms with time. The cardinal manifestation of PV is an increase in blood hemoglobin and corresponding increase in hematocrit.
PV management is focused on minimizing the thrombotic risk using aspirin and phlebotomy, along with cytoreduction therapies for high(er)-risk patients. Phlebotomy reduces iron availability to the erythroid cells and, as a result, reduces the rate of production of erythrocytes. Intensive treatment with phlebotomy to target hematocrit < 45% has been shown to reduce the composite endpoint of time to death from cardiovascular causes or major thrombotic events in patients with PV [70]. Almost all PV patients are iron deficient at presentation and/or during the course of their disease and may remain iron deficient because of high erythroid demand for iron and frequent phlebotomies [71]. Phlebotomy reduces hepcidin levels and in this sense counteracts the iron restriction produced by phlebotomy by facilitating iron absorption and re-cycling necessary for enhanced erythropoiesis. Some patients with PV experience a substantial symptom burden which may negatively affect patient health-related quality of life in areas such as inactivity, dizziness, headache, and fatigue [72] and which might be a function of iron deficiency. A recent exploratory analysis on the relationship between correction of iron deficiency and improvements in concentration problems, cognitive function, dizziness, fatigue, headaches, and inactivity during treatment with ruxolitinib showed a greater benefit in PV patients that were iron deficient at baseline [73].
Mouse Models of Polycythemia Vera
Controlling HCT is of critical importance in PV management. Pharmacologically induced iron-restricted erythropoiesis may be superior to intermittent phlebotomy, where the removal of RBCs is rapidly compensated. Such agents may treat the erythrocytosis of PV by limiting iron availability to erythroid precursors, thereby inhibiting JAK2-stimulated erythropoiesis and reducing RBC production. A mouse model of PV (carrying the JAK2V617F conditional knock-in allele [74]) has been utilized to test whether iron restriction would be beneficial in this disease. Administration of a hepcidin agonist or a TMPRSS6-ASO reverted erythrocytosis and normalized the HCT level in PV mice [59, 75]. These results suggest that TMPRSS6-ASO therapy could be used as a “medical phlebotomy” to provide continuous control of accelerated erythropoiesis to treat PV, while possibly avoiding the adverse consequences of total body iron depletion characteristic of chronic phlebotomy. Because of the association between high HCT levels and poor outcomes, continuous control of HCT levels using TMPRSS6-ASO could be highly clinically meaningful if clinical trials show that it can be done safely. Preliminary data from a clinical trial using a hepcidin mimetic developed by Protagonist Therapeutics [43] are encouraging in this regard.
Effects of TMPRSS6 Antisense Oligonucleotide Therapy in Healthy Human Volunteers
Sapablursen (ISIS 702843) is an N-acetylgalactosamine-modified antisense oligonucleotide (GalNAc-ASO) that targets TMPRSS6 mRNA. Sapablursen matches both human and monkey TMPRSS6 sequences perfectly. In non-human primates, sapablursen treatment was well tolerated after chronic dosing. Dose-dependent reduction of TMPRSS6 was accompanied by decreases in serum iron, transferrin saturation, and subsequent hemoglobin reduction, as expected for TMPRSS6 deficiency in non-human primates and mice [76].
The importance of TMPRSS6 inhibition in regulating hepcidin production in humans was assessed in healthy volunteers (NCT03165864). The study was approved by Institutional Review Board Services (Victoria, Australia) and conducted in compliance with the World Medical Association Declaration of Helsinki (October 2002), Good Clinical Practice (GCP) guidelines, and all national, state, and local laws of the appropriate regulatory authorities. All participants provided written informed consent prior to participation in the study. The treatment cohorts, n = 9 each, were well balanced in demographic and baseline characteristics. Overall, the mean age was 35 years (range 18–64); most subjects were male (91.7%), white (72.2%), and not Hispanic or Latino (91.7%) with a BMI 24.6 kg/m2 (range 17.2–31.8). Participants received a single dose of 20, 40, or 60 mg sapablursen (or placebo 0.9% saline) on day 1, followed by three additional doses of the same strength on days 22, 36, and 50. Each dose was administered by subcutaneous injection. The single dose of 60 mg sapablursen increased serum hepcidin compared to placebo (Fig. 1A). Subsequent administration of three additional doses of 40 or 60 mg on days 22, 36, and 50 caused dose- and time-dependent increases in serum hepcidin relative to placebo (Fig. 1A). In the repeated dose phase, serum iron and transferrin saturation were reduced in a time-dependent fashion by all three dose levels (Fig. 1B). The cellular concentration of hemoglobin in reticulocytes was reduced at the higher dose levels (40 and 60 mg) at later time points, indicating that the availability of iron to the erythroid was reduced (Fig. 1C). A trend towards a reduction in blood hemoglobin and hematocrit was observed but neither was significantly reduced in this short, healthy volunteer study (data not shown). While a reduction in blood hemoglobin is expected in healthy volunteers and PV patients, correcting ineffective erythropoiesis in patients with β-thalassemia might be expected to increase blood hemoglobin. No clinically significant changes were observed on other hematologic parameters, and platelet count was not changed. Three volunteers discontinued sapablursen because of a sustained reduction in transferrin saturation, and dosing was temporarily withheld in two additional volunteers for the same reason. Withholding the dose or discontinuing treatment with of sapablursen was mandated by the protocol if transferrin saturation was reduced to < 10% (absolute). Sapablursen was safe and well tolerated in healthy volunteers during both the single and repeated dose phases. The terminal pharmacokinetic half-life of sapablursen was 2–4 weeks, supporting once monthly dosing in further clinical studies.
A–C Subcutaneous administration of sapablursen (ISIS 702843) increases serum hepcidin concentration (A), reduces transferrin saturation (B), and reduces cellular hemoglobin content in reticulocytes (C) in healthy volunteers. A single dose of 20, 40, or 60 mg was administered on day 1, followed by three additional doses of the same strength on days 22, 36, and 50. The planned administration schedule for sapablursen is indicated by a triangle on the x-axis. Deviations from the planned administration schedule occurred because of scheduling issues with individual volunteers and transient or sustained reduction of TSAT < 10% in five subjects receiving sapablursen. All cohorts included nine healthy volunteers; however, for various reasons (e.g., early/late sample collection, missed sample collection) the number of samples at different timepoints varies. Values are ± standard error of the mean [SEM] with n typically > 6 for all groups; however, individual values range from n = 1 to 9. The study was conducted in a dose-escalating fashion, with lower doses tested prior to testing higher doses. Some volunteers were administered placebo in each cohort. Data for these volunteers were pooled to form a single placebo group
Sapablursen is currently being assessed in two on-going clinical studies in patients with non-transfusion-dependent β-thalassemia (NCT04059406) and polycythemia vera (NCT05143957). The β-thalassemia study aims to assess the impact of sapablursen on blood hemoglobin and liver iron content over a treatment period of up to 2 years in 36 patients. The study is fully enrolled. The PV study is actively recruiting 40 patients and will assess the impact of two dose levels of sapablursen on the frequency of phlebotomy and the Myeloproliferative Neoplasm Symptom Assessment Form-Total Symptom Score (MPN-SAF-TSS) after 37 weeks of treatment. Additional indications are also being explored.
Conclusions
Iron restriction represents a unique precision medicine approach for treatment of hematologic disorders affecting the erythroid lineage. Erythrocyte precursors are exquisitely sensitive to iron restriction, conferring a high level of selectivity to the approach. Hepcidin is the key regulator of iron absorption and recycling, making modulation of hepcidin activity or expression a highly effective way to restrict iron availability to erythroid precursors. Targeting TMPRSS6 as a negative regulator of hepcidin expression has been shown to be effective in animal models of hematologic disease and shows promise in early clinical trials. The ongoing clinical trials will be critical to determine whether this approach can deliver new treatments with better risk-benefit profiles for patients with erythroid disorders.
References
Finberg KE, et al. Mutations in TMPRSS6 cause iron-refractory iron deficiency anemia (IRIDA). Nat Genet. 2008;40(5):569–71.
Du X, et al. The serine protease TMPRSS6 is required to sense iron deficiency. Science. 2008;320(5879):1088–92.
Zivot A, et al. Erythropoiesis: insights into pathophysiology and treatments in 2017. Mol Med (Cambridge, MA). 2018;24(1):11.
Haase VH. Hypoxia-inducible factor-prolyl hydroxylase inhibitors in the treatment of anemia of chronic kidney disease. Kidney Int Suppl (2011). 2021;11(1):8–25.
Suragani RN, et al. Transforming growth factor-beta superfamily ligand trap ACE-536 corrects anemia by promoting late-stage erythropoiesis. Nat Med. 2014;20(4):408–14.
Taher AT, Cappellini MD. Luspatercept for beta-thalassemia: beyond red blood cell transfusions. Expert Opin Biol Ther. 2021;21(11):1363–71.
Nai A, et al. The second transferrin receptor regulates red blood cell production in mice. Blood. 2015;125(7):1170–9.
Parrow NL, et al. Lobe specificity of iron binding to transferrin modulates murine erythropoiesis and iron homeostasis. Blood. 2019;134(17):1373–84.
Xavier-Ferrucio J, et al. Low iron promotes megakaryocytic commitment of megakaryocytic-erythroid progenitors in humans and mice. Blood. 2019;134(18):1547–57.
Khalil S, et al. Iron modulation of erythropoiesis is associated with Scribble-mediated control of the erythropoietin receptor. J Exp Med. 2018;215(2):661–79.
Maio N, et al. Mechanisms of cellular iron sensing, regulation of erythropoiesis and mitochondrial iron utilization. Semin Hematol. 2021;58(3):161–74.
Chen JJ, Zhang S. Translational control by heme-regulated elF2alpha kinase during erythropoiesis. Curr Opin Hematol. 2022;29(3):103–11.
Coffey R, Ganz T. Iron homeostasis: an anthropocentric perspective. J Biol Chem. 2017;292(31):12727–34.
Fisher AL, Babitt JL. Coordination of iron homeostasis by bone morphogenetic proteins: current understanding and unanswered questions. Dev Dyn. 2022;251(1):26–46.
Beutler E, et al. The mask mutation identifies TMPRSS6 as an essential suppressor of hepcidin gene expression, required for normal uptake of dietary iron. ASH Ann Meeting Abstr. 2007;110(11):3.
Enns CA, Jue S, Zhang AS. The ectodomain of matriptase-2 plays an important nonproteolytic role in suppressing hepcidin expression in mice. Blood. 2020;136(8):989–1001.
Silvestri L, et al. The serine protease matriptase-2 (TMPRSS6) inhibits hepcidin activation by cleaving membrane hemojuvelin. Cell Metab. 2008;8(6):502–11.
Krijt J, et al. Matriptase-2 and hemojuvelin in hepcidin regulation: in vivo immunoblot studies in mask mice. Int J Mol Sci. 2021;22(5):2650.
Bell S, et al. A genome-wide meta-analysis yields 46 new loci associating with biomarkers of iron homeostasis. Commun Biol. 2021;4(1):156.
Hu Y, et al. Whole-genome sequencing association analysis of quantitative red blood cell phenotypes: the NHLBI TOPMed program. Am J Hum Genet. 2021;108(5):874–93.
Benyamin B, et al. Common variants in TMPRSS6 are associated with iron status and erythrocyte volume. Nat Genet. 2009;41(11):1173–5.
Chambers JC, et al. Genome-wide association study identifies variants in TMPRSS6 associated with hemoglobin levels. Nat Genet. 2009;41(11):1170–2.
Zhang AS, et al. Suppression of hepatic hepcidin expression in response to acute iron deprivation is associated with an increase of matriptase-2 protein. Blood. 2011;117(5):1687–99.
Taylor M, et al. Hypoxia-inducible factor-2alpha mediates the adaptive increase of intestinal ferroportin during iron deficiency in mice. Gastroenterology. 2011;140(7):2044–55.
Shah YM, et al. Intestinal hypoxia-inducible transcription factors are essential for iron absorption following iron deficiency. Cell Metab. 2009;9(2):152–64.
Mastrogiannaki M, et al. Deletion of HIF-2alpha in the enterocytes decreases the severity of tissue iron loading in hepcidin knockout mice. Blood. 2012;119(2):587–90.
Anderson ER, et al. Intestinal HIF2alpha promotes tissue-iron accumulation in disorders of iron overload with anemia. Proc Natl Acad Sci USA. 2013;110(50):E4922–30.
Xu Y, Alfaro-Magallanes VM, Babitt JL. Physiological and pathophysiological mechanisms of hepcidin regulation: clinical implications for iron disorders. Br J Haematol. 2021;193(5):882–93.
Heeney MM, Finberg KE. Iron-refractory iron deficiency anemia (IRIDA). Hematol Oncol Clin North Am. 2014;28(4):637–52.
Ashby DR, et al. Erythropoietin administration in humans causes a marked and prolonged reduction in circulating hepcidin. Haematologica. 2010;95(3):505–8.
Kautz L, et al. Identification of erythroferrone as an erythroid regulator of iron metabolism. Nat Genet. 2014;46(7):678–84.
Pak M, et al. Suppression of hepcidin during anemia requires erythropoietic activity. Blood. 2006;108(12):3730–5.
Arezes J, et al. Erythroferrone inhibits the induction of hepcidin by BMP6. Blood. 2018;132(14):1473–7.
Nai A, et al. Limiting hepatic Bmp-Smad signaling by matriptase-2 is required for erythropoietin-mediated hepcidin suppression in mice. Blood. 2016;127(19):2327–36.
Ganz T. Erythropoietic regulators of iron metabolism. Free Radic Biol Med. 2019;133:69–74.
Bullock GC, et al. Iron control of erythroid development by a novel aconitase-associated regulatory pathway. Blood. 2010;116(1):97–108.
Kimura H, Finch CA, Adamson JW. Hematopoiesis in the rat: Quantitation of hematopoietic progenitors and the response to iron deficiency anemia. J Cell Physiol. 1986;126(2):298–306.
Brissot E, et al. Iron and platelets: a subtle, under-recognized relationship. Am J Hematol. 2021;96(8):1008–16.
Forejtnikova H, et al. Transferrin receptor 2 is a component of the erythropoietin receptor complex and is required for efficient erythropoiesis. Blood. 2010;116(24):5357–67.
Dandekar T, et al. Identification of a novel iron-responsive element in murine and human erythroid delta-aminolevulinic acid synthase mRNA. Embo j. 1991;10(7):1903–9.
Chen JJ. Regulation of protein synthesis by the heme-regulated eIF2alpha kinase: relevance to anemias. Blood. 2007;109(7):2693–9.
Taranath R, et al. Regulation of iron homeostasis by PTG-300 improves disease parameters in mouse models for beta-thalassemia and hereditary hemochromatosis. Blood. 2019;134:3540.
Hoffman R, et al. Rusfertide (PTG-300) treatment in phlebotomy-dependent polycythemia vera patients. J Clin Oncol. 2022;40(16_suppl):7003.
Porter J, et al. Oral ferroportin inhibitor vamifeport for improving iron homeostasis and erythropoiesis in beta-thalassemia: current evidence and future clinical development. Expert Rev Hematol. 2021;14(7):633–44.
Manolova V, et al. Oral ferroportin inhibitor ameliorates ineffective erythropoiesis in a model of beta-thalassemia. J Clin Invest. 2019;130(1):491–506.
La Jolla Pharmaceutical Company: a study with LJPC-401 for the treatment of myocardial iron overload in patients with transfusion-dependent beta thalassemia; 2021. NIH National Library of Medicine. https://clinicaltrials.gov/ct2/show/results/NCT03381833?term=LJ401-BT01&draw=2&rank=1&view=results.
Kowdley KV, et al. ACG clinical guideline: hereditary hemochromatosis. Am J Gastroenterol. 2019;114(8):1202–18.
Guo S, et al. Reducing TMPRSS6 ameliorates hemochromatosis and beta-thalassemia in mice. J Clin Invest. 2013;123(4):1531–41.
Schmidt PJ, et al. An RNAi therapeutic targeting Tmprss6 decreases iron overload in Hfe(-/-) mice and ameliorates anemia and iron overload in murine beta-thalassemia intermedia. Blood. 2013;121(7):1200–8.
Finberg KE, Whittlesey RL, Andrews NC. Tmprss6 is a genetic modifier of the Hfe-hemochromatosis phenotype in mice. Blood. 2011;117(17):4590–9.
Booten S et al. Target TMPRSS6 for the treatment of hereditary hemochromatosis. In 53rd ASH annual meeting abstracts; 2011. p. 1047.
Gardenghi S, et al. Ineffective erythropoiesis in beta-thalassemia is characterized by increased iron absorption mediated by down-regulation of hepcidin and up-regulation of ferroportin. Blood. 2007;109(11):5027–35.
Parrow NL, et al. Decreased hepcidin expression in murine beta-thalassemia is associated with suppression of Bmp/Smad signaling. Blood. 2012;119(13):3187–9.
Rivella S. beta-thalassemias: paradigmatic diseases for scientific discoveries and development of innovative therapies. Haematologica. 2015;100(4):418–30.
Rivella S. Iron metabolism under conditions of ineffective erythropoiesis in β-thalassemia. Blood. 2019;133(1):51–8.
Musallam KM, et al. Revisiting the non-transfusion-dependent (NTDT) vs. transfusion-dependent (TDT) thalassemia classification 10 years later. Am J Hematol. 2021;96(2):E54–6.
Kautz L, et al. Erythroferrone contributes to hepcidin suppression and iron overload in a mouse model of beta-thalassemia. Blood. 2015;126(17):2031–7.
Chessa R, et al. Administration of minihepcidins to animals affected by β-thalassemia major reduces anemia and splenomegaly. Blood. 2016;128(22):259–259.
Casu C, et al. Minihepcidin peptides as disease modifiers in mice affected by beta-thalassemia and polycythemia vera. Blood. 2016;128(2):265–76.
Casu C, et al. Combination of Tmprss6-ASO and the iron chelator deferiprone improves erythropoiesis and reduces iron overload in a mouse model of beta-thalassemia intermedia. Haematologica. 2016;101(1):e8–11.
Casu C, et al. Correcting β-thalassemia by combined therapies that restrict iron and modulate erythropoietin activity. Blood. 2020;136(17):1968–79.
Hofrichter J, Ross PD, Eaton WA. Kinetics and mechanism of deoxyhemoglobin S gelation: a new approach to understanding sickle cell disease. Proc Natl Acad Sci USA. 1974;71(12):4864–8.
Castro O, et al. Improvement of sickle cell anemia by iron-limited erythropoiesis. Am J Hematol. 1994;47(2):74–81.
Rao KR, et al. Iron deficiency and sickle cell anemia. Arch Intern Med. 1983;143(5):1030–2.
Ryan TM, Ciavatta DJ, Townes TM. Knockout-transgenic mouse model of sickle cell disease. Science. 1997;278(5339):873–6.
Das N, et al. Intestine-specific disruption of hypoxia-inducible factor (HIF)-2alpha improves anemia in sickle cell disease. J Biol Chem. 2015;290(39):23523–7.
Parrow NL, et al. Dietary iron restriction improves markers of disease severity in murine sickle cell anemia. Blood. 2021;137(11):1553–5.
Nyffenegger N, et al. The oral ferroportin inhibitor vamifeport improves hemodynamics in a mouse model of sickle cell disease. Blood. 2022;140(7):769–81.
Arber DA, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405.
Marchioli R, et al. Cardiovascular events and intensity of treatment in polycythemia vera. N Engl J Med. 2013;368(1):22–33.
Ginzburg YZ, et al. Dysregulated iron metabolism in polycythemia vera: etiology and consequences. Leukemia. 2018;32(10):2105–16.
Mesa R, et al. Patient-reported outcomes data from REVEAL at the time of enrollment (baseline): a prospective observational study of patients with polycythemia vera in the United States. Clin Lymphoma Myeloma Leuk. 2018;18(9):590–6.
Verstovsek S, et al. Markers of iron deficiency in patients with polycythemia vera receiving ruxolitinib or best available therapy. Leuk Res. 2017;56:52–9.
Mullally A, et al. Physiological Jak2V617F expression causes a lethal myeloproliferative neoplasm with differential effects on hematopoietic stem and progenitor cells. Cancer Cell. 2010;17(6):584–96.
Casu C, et al. Tmprss6-ASO as a tool for the treatment of polycythemia vera mice. PLoS ONE. 2021;16(12): e0251995.
Zanardi TA, et al. Safety, pharmacokinetic, and pharmacodynamic evaluation of a 2’-(2-methoxyethyl)-D-ribose antisense oligonucleotide-triantenarry N-acetyl-galactosamine conjugate that targets the human transmembrane protease serine 6. J Pharmacol Exp Ther. 2021;377(1):51–63.
Acknowledgements
The authors thank all of the participants, investigators, study staff, and Ionis clinical team that made the healthy volunteer study possible.
Funding
Ionis Pharmaceutical Inc. funded the healthy volunteer study and paid for the journal’s rapid publication service fee. No other funding was provided relating to the preparation of the manuscript.
Author Contributions
Tomas Ganz manuscript writing; Elizabeta Nemeth manuscript writing; Stefano Rivella manuscript writing; Paul Goldberg manuscript writing; Andy R. Dibble study design, conduct and reporting of the healthy volunteer study, manuscript writing; Shuling Guo manuscript writing; Brett P. Monia study design, manuscript writing; Terrance D. Barrett manuscript writing.
Disclosures
Tomas Ganz is a scientific cofounder and adviser to Intrinsic LifeSciences and Silarus Therapeutics, and is a consultant for Akebia, Avidity Bio, Pharmacosmos, FibrogenAstraZeneca. Ionis, Gossamer Bio, Global Blood Therapeutics, American Regent, Sierra Oncology, Disc Medicine, RallyBio, Rockwell Scientific and Vifor. Elizabeta Nemeth is a scientific cofounder and adviser to Intrinsic LifeSciences and Silarus Therapeutics and a consultant for Protagonist, Vifor, FibrogenAstraZeneca, RallyBio, Ionis, Shield Therapeutics, Disc Medicine, Novo Nordisk, Imara, and Chiesi. Stefano Rivella is a member of scientific advisory board of Ionis Pharmaceuticals, Meira GTx, Vifor and Disc Medicine, GSK and owns stock options from Disc Medicine. Stefano Rivella has been or is consultant for Incyte, Cambridge Healthcare Res, Celgene Corporation, Catenion, First Manhattan Co., FORMA Therapeutics, Ghost Tree Capital, Keros Therapeutics, Noble insight, Protagonist Therapeutics, Sanofi Aventis U.S., Slingshot Insight, Techspert.io and BVF Partners L.P., Rallybio, LLC, venBio Select LLC. Paul Goldberg holds share options in Ionis Pharmaceuticals and Prilenia Therapeutics, and has received consulting fees from Ionis Pharmaceuticals and Prilenia Therapeutics. Andy R. Dibble, Michael L. McCaleb, Shuling Guo, Brett P. Monia, Terrance D. Barrett are employees of Ionis Pharmaceuticals Inc.
Compliance With Ethics Guidelines
The study was approved by Institutional Review Board Services (Victoria, Australia) and conducted in compliance with the World Medical Association Declaration of Helsinki (October 2002), Good Clinical Practice (GCP) guidelines, and all national, state, and local laws of the appropriate regulatory authorities. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available as they contain data proprietary to Ionis Pharmaceutical Inc and mechanism and standards for sharing these data are not available institutionally.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ganz, T., Nemeth, E., Rivella, S. et al. TMPRSS6 as a Therapeutic Target for Disorders of Erythropoiesis and Iron Homeostasis. Adv Ther 40, 1317–1333 (2023). https://doi.org/10.1007/s12325-022-02421-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02421-w