Abstract
Introduction
SURE Netherlands (NCT03929679) evaluated the use of once-weekly (OW) semaglutide, a glucagon-like peptide 1 receptor agonist (GLP-1RA), in routine clinical care for individuals with type 2 diabetes (T2D).
Methods
Adults (age ≥ 18 years) with T2D were enrolled into the single-arm study. The primary endpoint was change from baseline to end of study (EOS; approx. 30 weeks) in glycated haemoglobin (HbA1c). Secondary endpoints were change from baseline to EOS in body weight (BW) and waist circumference (WC). Proportions of participants achieving predefined HbA1c targets and weight-loss responses at EOS, safety, health-related quality of life (HRQoL) and treatment satisfaction were assessed.
Results
In total, 211 participants (mean age 60.5 years; diabetes duration 13.3 years) initiated semaglutide; most were receiving metformin (82.9%) and/or basal insulin (59.2%) at baseline, and 6.2% switched from another GLP-1RA. Mean baseline HbA1c, BW and WC were 8.6%, 105.2 kg and 118.8 cm. In the 186 (88.2%) participants receiving semaglutide at EOS, mean reduction in HbA1c with semaglutide was − 1.2%-points (95% [confidence interval] CI − 1.3; − 1.0; p < 0.0001), with 124 (70.5%), 95 (54.0%) and 65 (36.9%) participants achieving HbA1c targets of < 8.0%, < 7.5% and < 7.0%, respectively. Mean reduction in BW was − 7.8 kg [95% CI − 8.7; − 6.8; p < 0.0001], corresponding to relative reduction of − 7.5% [95% CI − 8.4; − 6.6; p < 0.0001]. Improvements in WC (− 8.8 cm [95% CI − 10.4; − 7.2; p < 0.0001]), HRQoL and treatment satisfaction were observed, including across most Short-Form 36 Health Survey domains. One serious adverse drug reaction (cholecystitis) was reported. Eight participants (all receiving concomitant insulin) experienced severe or documented hypoglycaemia.
Conclusion
Individuals with T2D treated with OW semaglutide experienced significant and clinically relevant improvements in glycaemic control and BW from baseline. These results from a diverse real-world population in the Netherlands support the use of OW semaglutide in treating adults with T2D in routine clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In the SUSTAIN clinical trial programme, the glucagon-like peptide 1 receptor agonist semaglutide was shown to significantly improve glycaemic control and lower body weight (BW) in individuals with type 2 diabetes (T2D) versus placebo and active comparators. |
The SURE programme was designed to complement the findings of the SUSTAIN programme and investigated once-weekly (OW) semaglutide use in routine clinical practice across several countries. |
Herein, we present the first real-world clinical practice findings regarding OW semaglutide use in the Netherlands. |
After a mean follow-up of 35 weeks, the 186 (88.2%) participants still receiving semaglutide experienced mean reductions in glycated haemoglobin and BW of − 1.2%-points and − 7.8 kg (7.5%), and reported clinically relevant improvements in diabetes treatment satisfaction and health-related quality of life from baseline to end of study. |
This study emphasises the clinically relevant improvements in glycaemic control, BW and health-related quality of life associated with semaglutide in a diverse real-world T2D population, supporting its use in routine clinical practice. |
Introduction
In the Netherlands, more than 1.1 million people have diabetes, with type 2 diabetes (T2D) accounting for approximately 90% of cases [1,2,3]. The goals of T2D treatment comprise attaining good glycaemic control while minimising the risk of hypoglycaemia and managing cardiovascular (CV) risk factors, to prevent or delay complications and preserve quality of life [4,5,6].
Dutch guidelines for the management of T2D are largely consistent with the joint guidelines of the American Diabetes Association (ADA)/European Association for the Study of Diabetes (EASD) [4,5,6]. However, pharmacotherapy recommendations for achieving treatment goals differ somewhat between the two [4,5,6]. While Dutch guidelines for general practitioners (GPs) have adopted a stepwise approach to T2D treatment, in which people are prescribed metformin followed by a sulfonylurea (specifically gliclazide) and subsequent intensification with neutral protamine Hagedorn (NPH) insulin, ADA/EASD guidelines that adopt a more individualised approach to therapy have largely been followed in secondary care in the Netherlands. For example, ADA/EASD guidelines recommend therapy based on a person’s CV risk, and the recommended treatment for individuals with high CV risk is a glucagon-like peptide 1 receptor agonist (GLP-1RA) or sodium–glucose cotransporter inhibitor with proven CV benefits; in the Dutch guidelines for GPs, such individuals are not considered separately. In the Netherlands, GLP-1RAs have been available for the treatment of T2D since 2010. However, this class of medication has only been considered in individuals with glycated haemoglobin (HbA1c) > 7.0% (> 53 mmol/mol) who were already being treated with metformin alongside a sulfonylurea or basal insulin (NPH insulin is preferred as third-line therapy). Reimbursement was previously also limited to individuals with T2D and a body mass index (BMI) ≥ 35 kg/m2 [5, 6]. This limitation for the reimbursement of GLP-1RA therapy was revised at the end of 2019, by including individuals with T2D and BMI 30–35 kg/m2.
Semaglutide (Novo Nordisk A/S, Denmark) is a long-acting human GLP-1RA [7,8,9]. The phase 3 SUSTAIN clinical trial programme explored the efficacy and safety of once-weekly (OW) semaglutide in a broad range of subjects with T2D [10,11,12,13,14,15,16,17,18]. There is a need for real-world evidence (RWE) to complement these clinical trial data. Real-world studies have less rigid inclusion and exclusion criteria than clinical trials and are able to investigate the use of a drug in a wider population and/or in a specific region. Thus, real-world studies can provide additional information on health outcomes after a given medication is used in routine clinical practice [19].
The Semaglutide Real-world Evidence (SURE) programme was designed to complement the findings of the SUSTAIN programme and consists of nine individual, observational RWE studies investigating OW semaglutide in routine clinical practice across several countries. Results from SURE Canada, Denmark/Sweden, Switzerland and the UK have already been reported [20,21,22,23]. Here we present findings from the SURE Netherlands study, which investigated OW semaglutide in individuals with T2D in routine clinical practice in the Netherlands.
Methods
Study Design
SURE Netherlands was an approximately 30-week, prospective, open-label, single-arm, observational study assessing OW semaglutide in adults with T2D in routine clinical practice in the Netherlands. The study was conducted in accordance with the Declaration of Helsinki and the Guidelines for Good Pharmacoepidemiology Practices [24, 25], and was approved by the Medical Ethical Review Committee of the University Medical Center Groningen (METC 2019/04/16). All participants provided their written informed consent. The study is registered on ClinicalTrials.gov (NCT03929679).
Participants were enrolled from 26 sites, of which 15 were primary care and 11 were secondary or tertiary care. The decision to initiate semaglutide was at the treating physician’s discretion and after discussion with the individual with T2D: it was separate from the decision to include the person in the study. Participants were treated with OW subcutaneous administration of (s.c.) commercially available semaglutide. Treating physicians determined the starting and maintenance dose of semaglutide, and any subsequent dosing changes; they could also prescribe or otherwise modify other glucose-lowering or obesity medications, or recommend diet and physical activity counselling, according to routine clinical practice.
Treatment discontinuation was allowed at any time during the study at the treating physician’s discretion. Discontinuation was recommended if a safety concern related to semaglutide occurred, or the participant became or intended to become pregnant. Participants were able to withdraw at any time.
Treatment was initiated at visit 1 (week 0). Visits 2 to 5 were intermediate visits, held according to local clinical practice. The end-of-study (EOS) visit (visit 6) was to be held between weeks 28 and 38. As a result of COVID-19 pandemic restrictions, consultation by telephone was permitted for the intermediate and EOS visits, and attendance for the EOS visit beyond the planned week 38 timepoint was also permitted.
Study Population
Adults (age ≥ 18 years) who had initiated OW s.c. semaglutide were enrolled. Participants were required to have been diagnosed with T2D at least 12 weeks prior to inclusion and have one or more documented HbA1c value(s) recorded within 12 weeks prior to initiation of semaglutide. Exclusion criteria included prior use of semaglutide; previous participation in the study; inadequate understanding of the study procedures or language barriers; and hypersensitivity to semaglutide or any of its excipients.
Endpoints
The primary endpoint was change from baseline to EOS in HbA1c (%-point and mmol/mol). HbA1c evaluations were provided by local laboratories on the basis of regular practice; methodology between laboratories was not standardised. Secondary supportive endpoints included change from baseline to EOS in body weight (BW; kg and %) and waist circumference (WC; cm); the proportion of participants at EOS achieving HbA1c targets of < 8.0% (64 mmol/mol), < 7.5% (59 mmol/mol) and < 7.0% (53 mmol/mol); a HbA1c reduction ≥ 1.0%-point; weight-loss responses ≥ 3.0% and ≥ 5.0%; and a composite endpoint of HbA1c reduction ≥ 1.0%-point and weight loss ≥ 3.0%.
Patient-reported outcomes were assessed in terms of change from baseline to EOS in health-related quality of life (HRQoL), using the Short-Form 36 Health Survey version 2 (SF-36®v2) score [26], and treatment satisfaction, using the Diabetes Treatment Satisfaction Questionnaire status (DTSQs) score [27] and the Diabetes Treatment Satisfaction Questionnaire change (DTSQc) score [28].
Exploratory assessments included evaluation of the weekly dose of semaglutide at EOS and whether participants stopped or added new glucose-lowering medications (other than semaglutide) during the study.
Safety
Safety was evaluated according to adverse event (AE) reporting by physicians; all AEs occurring between obtaining consent of participants and the EOS visit were systematically collected and reported. All episodes of participant-reported documented and/or severe hypoglycaemia were also to be recorded. Severe hypoglycaemia was defined as an episode requiring the assistance of another person to actively administer carbohydrate or glucagon, or to take other corrective action.
Statistical Analysis
Descriptive statistics were used to describe participant characteristics at the time of semaglutide initiation. Baseline characteristics were evaluated and sensitivity analyses for the primary endpoint performed for the full analysis set (FAS), which included all participants who provided their signed informed consent and initiated treatment with semaglutide. The primary analysis of the primary and secondary endpoints and analyses of the exploratory assessments were performed for the effectiveness analysis set (EAS), which included all participants in the FAS who were receiving treatment with semaglutide at EOS and who attended the EOS visit.
The primary and secondary endpoints were assessed using an analysis of covariance (ANCOVA). Analysis of the primary endpoint excluded participants with missing information on HbA1c at EOS and was adjusted for baseline HbA1c (continuous), baseline use (within 12 weeks prior to semaglutide initiation) of GLP-1RA, dipeptidyl peptidase 4 inhibitor and insulin (yes/no), and number of oral blood glucose-lowering medications (0–1/≥ 2), T2D duration (continuous), age (continuous), BMI (continuous) and sex. Participants who discontinued treatment with another GLP-1RA no later than 4 weeks after initiation of semaglutide treatment were defined as having switched to semaglutide.
Prespecified sensitivity analyses were performed for the FAS using a mixed model for repeated measurements to assess the impact on the primary analysis of excluding data from participants who did not complete the study, discontinued treatment or for whom information on HbA1c at EOS was missing. A post hoc sensitivity analysis in the EAS was also conducted to assess whether the extension of the EOS window due to the COVID-19 pandemic had an impact on the results. This analysis was restricted to participants completing the study within the original visit window (28–38 weeks). Additional post hoc analyses were carried out to determine the proportion of patients achieving HbA1c targets at EOS of < 8.0% (64 mmol/mol), < 7.5% (59 mmol/mol) and < 7.0% (53 mmol/mol), among those who had HbA1c levels equal to or above these targets at baseline in the EAS. Post hoc analyses were also performed to investigate treatment outcomes (change in HbA1c and BW) when two patients with a diagnosis of type 1 diabetes (T1D) were excluded, and by subgroups according to type of prescriber (GP or endocrinologist), by baseline HbA1c subgroup, and by most frequently used baseline medication (metformin, basal insulin and sulfonylureas).
Results
Participant Disposition and Baseline Characteristics
The study was initiated with the first-participant first-visit on 28 May 2019 and was completed with last-participant last-visit on 24 November 2020. The majority of treating physicians (63%) were GPs working at 15 primary care sites and the remaining 37% were endocrinology specialists working at 11 secondary or tertiary care sites.
Participant disposition is shown in Fig. S1 in the supplementary material; the FAS consisted of 211 participants. A total of 200 (94.8%) participants completed the study, i.e. attended the EOS visit. Of the FAS, 19 participants (9.0%) discontinued semaglutide, primarily because of gastrointestinal (GI) side effects (n = 12; 5.7%). Participants who discontinued treatment before EOS or had unknown treatment status at EOS were not necessarily non-completers of the study. Fourteen (6.6% of the FAS) of the 19 participants who discontinued semaglutide completed the study; therefore, the EAS comprised 186 participants (88.2% of the FAS). Eleven participants (5.2%) did not complete the study; of these, four participants (1.9% of the FAS) withdrew or did not attend visit 6, and three (1.4% of the FAS) were lost to follow-up. Two participants (0.9% of the FAS) had previously been referred to secondary care with a suspected diagnosis of T1D. Following revision of these diagnoses to T2D, these participants were included in the study.
Baseline characteristics of the FAS are presented in Table 1. Overall, approximately half of the participants (53.1%) were female, mean age was 60.5 years and mean diabetes duration was 13.3 years. Mean baseline HbA1c was 8.6% (71 mmol/mol), BW 105.2 kg, WC 118.8 cm and BMI 35.9 kg/m2. Thirteen (6.2%) participants had an HbA1c level of < 7.0% at baseline. Most participants had hypertension (n = 147, 69.7%), 65.4% had dyslipidaemia (n = 138) and 18.5% (n = 39) had coronary heart disease (Table 1).
Overall, 175 participants (82.9%) were taking metformin at baseline (Table S1 in the supplementary material), 97 participants (46.0%) were taking a sulfonylurea and 125 participants (59.2%) were on basal insulin. Thirteen participants (6.2%) switched to semaglutide from another GLP-1RA.
The two most common reasons for initiating semaglutide were improving glycaemic control (n = 190, 90.0%) and weight reduction (n = 161, 76.3%); other reasons included addressing CV risk factors (n = 35, 16.6%) and simplifying current treatment regimens (n = 32, 15.2%; Table 1). Most participants (n = 204, 96.7%) were prescribed a starting semaglutide dose of 0.25 mg and seven (3.3%) initiated semaglutide at a dose of 0.5 mg (Table 1).
Baseline HbA1c and BW values by baseline medication are shown in Table S2 in the supplementary material.
HbA1c
In the EAS, the estimated mean change from baseline (8.6%/70 mmol/mol) to EOS in HbA1c was − 1.2%-points (95% confidence interval [CI] − 1.3; − 1.0; p < 0.0001), corresponding to − 13 mmol/mol (95% CI − 14.4; − 11.2; p < 0.0001; Table 2).
Reductions in HbA1c by baseline HbA1c subgroup are shown in Table S3 in the supplementary material.
When assessing HbA1c changes by baseline treatment (sulfonylurea, basal insulin, biguanides), we observed significant and clinically relevant reductions across all subgroups, with the greatest reductions observed in baseline users of sulfonylureas (n = 81: 1.3%-points [95% CI − 1.5; − 1.1]; p < 0.0001, corresponding to − 14 mmol/mol [95% CI − 17; − 12]; p < 0.0001), and the smallest reductions observed in baseline users of basal insulin (n = 104: 1.0%-point reduction [95% CI − 1.2; − 0.8]; p < 0.0001, corresponding to − 11 mmol/mol [95% CI − 12.6; − 8.7]; p < 0.0001) (Table S2 in the supplementary material).
The prespecified sensitivity analysis of the FAS showed similar results to the primary analysis (Table S4 in the supplementary material).
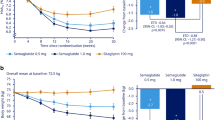
At EOS, 124 (70.5%), 95 (54.0%) and 65 (36.9%) participants achieved an HbA1c target of < 8.0%, < 7.5% and < 7.0%, respectively, and 102 (58.0%) achieved an HbA1c reduction of ≥ 1%-point (Fig. 1a). Of those participants with an HbA1c above or equal to thresholds at baseline, 69 of 119 (58.0%), 72 of 150 (48.0%) and 58 of 175 (33.1%) achieved HbA1c < 8.0%, < 7.5% and < 7.0%, respectively.
Body Weight and Waist Circumference
The estimated mean change from baseline to EOS in BW was − 7.8 kg (95% CI − 8.7; − 6.8; p < 0.0001), corresponding to a relative BW reduction of − 7.5% (95% CI − 8.4; − 6.6; p < 0.0001) (Table 2). Reductions in BW by baseline HbA1c subgroup are shown in Table S3 in the supplementary material.
When assessing BW changes by baseline treatment (sulfonylurea, basal insulin, biguanides), we observed significant and clinically relevant reductions across all subgroups, with the greatest relative reduction in BW observed in those using basal insulin (− 8.7% [95% CI − 9.8; − 7.5]; p < 0.0001), and the lowest reductions observed in those using a sulfonylurea (− 6.7% [95% CI − 8.1; − 5.3]; p < 0.0001) (Table S5 in the supplementary material). Overall, 123 (76.9%) and 103 (64.4%) participants achieved ≥ 3% and ≥ 5% weight loss, respectively (Fig. 1b). The estimated mean change from baseline to EOS in WC was − 8.8 cm (95% CI − 10.4; − 7.2; p < 0.0001) (Table 2).
Composite Endpoint
At EOS, 73 (44.5%) participants achieved the composite endpoint of both an HbA1c reduction ≥ 1%-point and a weight-loss response ≥ 3%.
HRQoL and Treatment Satisfaction Patient-Reported Outcomes
OW semaglutide treatment was associated with improvements in HRQoL. There were statistically significant and clinically relevant improvements in all SF-36®v2 domains except emotional functioning, with the greatest improvements observed in vitality, physical health, physical functioning, social functioning and bodily pain (Fig. 2).
Patients receiving OW semaglutide also reported improved treatment satisfaction. The observed mean DTSQs score at baseline was 27.9 and the estimated mean score at EOS was 31.6, resulting in an estimated change from baseline to EOS of 3.7 (95% CI 3.1; 4.4; p < 0.0001). At EOS, the estimated mean DTSQc score was 13.2 (95% CI 12.4; 13.9; p < 0.0001).
Semaglutide Dose at EOS
The mean dose of semaglutide at EOS was 0.83 ± standard deviation of 0.26 mg, with most participants (n = 130, 69.9%) receiving 1.0 mg. Forty-five (24.2%) participants were receiving a dose of 0.5 mg and 11 (5.9%) participants were receiving a dose of 0.25 mg. No participants were on a dose greater than 1.0 mg.
Insulin Dose and Glucose-Lowering Medication Use
In the EAS, the median (interquartile range) total insulin dose (bolus, basal and premixed) for all participants receiving insulin at baseline (n = 108) was 52.0 IU (38.0–83.0), decreasing to 40.0 IU (30.0–70.0) at EOS. In the EAS, 24 participants had stopped bolus insulin use by EOS. The mean number of glucose-lowering medications used by participants in the EAS was 2.4 ± 0.9 at baseline and 2.9 ± 0.9 at EOS. Because the number of drugs at EOS included semaglutide, the mean number of glucose-lowering medications (other than semaglutide) was lower at EOS than at baseline. The majority of participants (n = 148, 79.6%) were not prescribed any new glucose-lowering medications during the study period. Glucose-lowering medications at baseline and EOS are shown in Table S1 in the supplementary material.
Post Hoc Analyses
Two additional analyses—one that excluded two participants with a reported history of T1D and one that excluded 18 participants completing later than the original EOS window—showed similar HbA1c and BW reductions to the primary analysis (Table S4 in the supplementary material).
By Type of Prescriber
The 88 participants in the EAS being treated by a GP had lower baseline HbA1c (8.5%, 69 mmol/mol) and higher baseline BW (105.7 kg) than the 123 participants treated by an endocrinology specialist (baseline HbA1c 8.7%/72 mmol/mol and BW 104.9 kg). Participants treated by a specialist had longer diabetes duration, more extensive use of glucose-lowering medication (especially insulin) and generally had more comorbidities than those treated by a GP (Table S6 in the supplementary material).
In participants treated by a GP, the estimated mean change from baseline to EOS in HbA1c was comparable (− 1.1%-points [95% CI − 1.3; − 0.9; p < 0.0001], corresponding to − 12 mmol/mol [95% CI − 15; − 10; p < 0.0001]) to that in participants treated by a specialist (− 1.2%-points [95% CI − 1.4; − 1.0; p < 0.0001], corresponding to − 13 mmol/mol [95% CI − 16; − 11; p < 0.0001]). The proportion of participants who stopped basal and/or bolus insulin was greater for those treated by an endocrinology specialist than for those treated by a GP (Table S6 in the supplementary material).
Greater relative reductions in BW were observed in participants treated by a specialist compared with those treated by a GP: − 8.4% (95% CI − 9.7; − 7.2; p < 0.0001) versus − 6.4% (95% CI − 7.6; − 5.2; p < 0.0001), respectively.
Safety
A total of 447 AEs were reported for 154 participants in the FAS. This included 14 serious AEs (SAEs) in 11 participants and 433 non-serious AEs in 148 participants (Table S7 in the supplementary material). Of the 14 SAEs, three occurred in one participant prior to semaglutide initiation, and 10 (in nine participants) were considered unlikely to be related to OW semaglutide. One SAE (cholecystitis) was classified as a serious adverse drug reaction (SADR) possibly related to treatment with semaglutide (see Supplementary Appendix for further details).
There were 15 AEs in eight participants that led to permanent discontinuation of semaglutide; all were non-serious AEs. No AEs leading to death were reported.
Of the 433 non-serious AEs, most were GI (226 events), of which the most common were nausea (90 events), diarrhoea (30 events) and constipation (21 events). A total of 12 participants discontinued semaglutide because of unacceptable GI intolerability.
Fourteen hypoglycaemic episodes were reported by eight (4.3%) participants in the EAS during the study, all of whom were also receiving insulin. Only one hypoglycaemic episode was classified as severe; the participant who reported this episode also reported one other non-serious hypoglycaemic episode during the same month.
Discussion
In the SURE Netherlands study, participants treated with OW semaglutide experienced statistically and clinically significant reductions in HbA1c, BW and WC. Significant improvements were also observed in treatment satisfaction and HRQoL. The results from SURE Netherlands support the use of OW semaglutide in routine clinical practice for the treatment of T2D.
The HbA1c reduction of 1.2%-points observed in SURE Netherlands is consistent with observations from other SURE studies reported to date, in which reductions ranged from 0.8 to 1.5%-points [20,21,22,23]. While it is important to note the differing study designs and different participant populations, it is of interest to examine the findings of the SURE real-world studies in the context of those from the SUSTAIN randomised controlled clinical trials (RCTs). The mean HbA1c reduction (1.2%-points) observed with OW semaglutide (mean dose 0.83 mg at EOS) in the SURE Netherlands study was consistent with that observed with semaglutide 0.5 and 1.0 mg in the SUSTAIN programme (1.1–1.8%-points), both from a similar mean HbA1c at baseline (8.6% in SURE Netherlands versus 8.0–8.4% in the SUSTAIN programme). It should be noted that the SUSTAIN programme reported data for patients in the FAS, whereas SURE study data is for completers on semaglutide treatment [10,11,12,13,14,15,16,17,18, 29].
The reduction in HbA1c observed in a real-world setting during SURE Netherlands was at the lower end of the range observed in the phase 3 RCTs; several factors may account for this difference. The semaglutide dose was not maximised for all participants in the SURE studies [20,21,22,23] (reasons for not up-titrating the semaglutide dose were not collected), while the SUSTAIN trials used set maintenance doses of 0.5 and/or 1.0 mg [10,11,12,13,14,15,16,17,18]. SURE Netherlands included participants on different medications at baseline and background medication could be adjusted throughout the study. Many patients in SURE Netherlands were receiving insulin at baseline in whom insulin doses were reduced following the initiation of semaglutide. Additionally, a small number of participants in SURE Netherlands switched to semaglutide from another GLP-1RA. By contrast, the SUSTAIN trials did not include participants previously treated with a GLP-1RA [10,11,12,13,14,15,16,17,18], only the participants in SUSTAIN 5 were taking basal insulin [14], and baseline medication was largely maintained throughout the trials. The inclusion of a small number of participants in SURE Netherlands with a baseline HbA1c of < 7.0% may also have limited the extent of HbA1c reductions; inclusion criteria for the SUSTAIN trials were HbA1c of ≥ 7%. According to the current reimbursement guidance in the Netherlands, these participants (and those with a BMI of < 30 kg/m2) did not meet the criteria for starting OW semaglutide [5, 6].
The BW reductions observed in SURE Netherlands (− 7.8 kg/− 7.5%) were more pronounced than in the SUSTAIN programme, in which they ranged from − 3.5 kg (− 3.8%, with 0.5 mg semaglutide in SUSTAIN 4) [13] to − 6.5 kg (− 6.9%, with 1.0 mg semaglutide in SUSTAIN 7) [15], although it should be noted that mean baseline BMI was slightly higher in the SURE Netherlands study compared with studies in the SUSTAIN programme [10,11,12,13,14,15,16,17,18]. It should also be highlighted that data from the SUSTAIN RCTs and this present study are not entirely comparable; for example, there were differences in the frequency of and interval between follow-up visits. Follow-up visits in SUSTAIN 4 included BW, fasting blood glucose and HbA1c measurements and were performed every 4 weeks [13]. The reduction in BW in SURE Netherlands was also greater than that observed in the other SURE studies reported to date (− 4.3 to − 5.4 kg; relative reduction − 4.3% to − 5.5%) [20,21,22,23]. Notably, in SURE UK the mean reduction in BW was − 5.8 kg in a population with a higher baseline BMI (37.2 kg/m2) than in the present SURE study (35.9 kg/m2) [23].
In the Netherlands, reimbursement for GLP-1RAs has been restricted; since 2020, these medications have only been reimbursed for individuals with a BMI ≥ 30 kg/m2 (until the end of 2019, this threshold had been ≥ 35 kg/m2). Because enrolment for SURE Netherlands commenced in May 2019 and the primary completion date was November 2020, these reimbursement restrictions may have affected which individuals’ physicians enrolled in the study [5, 6].
Clinically relevant improvements in glycaemic control and weight management were observed in SURE Netherlands: most participants achieved HbA1c reductions of ≥ 1.0% and BW reductions of ≥ 5.0%. This finding is consistent with previous real-world analyses on the use of OW semaglutide for patients with T2D [30,31,32,33].
The significant improvements in treatment satisfaction and HRQoL observed in this study are clinically relevant and consistent with the findings of the previous SURE studies and post hoc analyses of individuals with T2D treated with OW semaglutide in the SUSTAIN trials [20,21,22,23, 34].
Notably, 24 participants in SURE Netherlands were able to discontinue their bolus insulin therapy during the study, and the mean insulin dose in participants continuing insulin also decreased. Most participants did not initiate new glucose-lowering medications, other than semaglutide, during the study. These results are consistent with those from other SURE studies, in which the use of glucose-lowering medications other than semaglutide generally decreased over the study duration [20,21,22,23].
The treatment discontinuation rate in the SURE Netherlands study (9%) was lower than that observed in the SUSTAIN programme (12.3–20.3%) [10,11,12,13,14,15,16,17,18], indicating that OW semaglutide is well tolerated in routine clinical practice. The discontinuation rate was similar to that seen in the SURE Canada, Denmark/Sweden and Switzerland studies (8.4%, 9.0% and 9.4%, respectively), and lower than that observed in SURE UK (13.5%) [20,21,22,23].
Safety observations in SURE Netherlands were consistent with previous experience from clinical and real-world studies. One SADR (cholecystitis) was reported as possibly related to treatment in the SURE Netherlands study.
In the Netherlands, the initiation of a GLP-1RA in addition to metformin and basal insulin is recommended in patients with T2D with a BMI ≥ 30 kg/m2, and a health economic appraisal in this patient population has indicated a dominance of GLP-1RA therapies, compared with intensification with bolus insulin, in terms of both clinical benefits and cost [35]. Additionally, projections of outcomes over patient lifetimes suggest that OW semaglutide is likely to improve clinical outcomes for patients with T2D, in comparison with both insulin glargine and dulaglutide, another GLP-1RA [2].
The strengths of the SURE Netherlands study include a diverse study population that reflects real-world clinical practice, and the inclusion of participants from primary, secondary and tertiary care. Both of these aspects of the SURE Netherlands study increase its relevance for clinical practice. There are several limitations related to the study. The main limitation of the SURE studies relates to the single-arm observational design (the absence of a randomised comparator group). As such, the impact of other factors cannot be ruled out, nor can it be directly inferred that the estimated changes in outcomes are causal effects of study treatment. Data were collected as part of routine clinical practice, rather than through mandatory assessments at prespecified timepoints, which may have affected the robustness and completeness of the data. Additionally, the SURE Netherlands study had a relatively small study population compared with the SUSTAIN RCTs and the duration of the study was relatively modest.
Conclusion
In a real-world population in the Netherlands, individuals with T2D treated with OW semaglutide experienced significant and clinically relevant improvements in glycaemic control and reductions in WC from baseline, alongside pronounced reductions in BW. Participants also reported improvements in diabetes treatment satisfaction and HRQoL. Safety data collected during the study were consistent with the known safety profile of semaglutide. These findings from the SURE Netherlands study are consistent with those from the other studies in the SURE programme and support the use of OW semaglutide in treating adults with T2D in routine clinical practice in the Netherlands.
References
Rijksinstituut voor Volksgezondheid en Milieu. Diabetes Mellitus, 2018. https://www.volksgezondheidenzorg.info/onderwerp/diabetes-mellitus. Accessed Apr 2022.
Hunt B, Malkin SJP, Moes RGJ, et al. Once-weekly semaglutide for patients with type 2 diabetes: a cost-effectiveness analysis in the Netherlands. BMJ Open Diabetes Res Care. 2019;7: e000705. https://doi.org/10.1136/bmjdrc-2019-000705.
Moser A, van der Bruggen H, Widdershoven G, et al. Self-management of type 2 diabetes mellitus: a qualitative investigation from the perspective of participants in a nurse-led, shared-care programme in the Netherlands. BMC Public Health. 2008;8:91.
Buse JB, Wexler DJ, Tsapas A, et al. 2019 Update to: Management of hyperglycemia in Type 2 Diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2020;43:487–93.
Nederlands Huisartsen Genootschap (NHG). NHG-werkgroep Diabetes mellitus type 2. NHG-Standaard Diabetes mellitus type 2, www.nhg.org. 2018. https://richtlijnen.nhg.org/standaarden/diabetes-mellitus-type-2. Accessed June 2022.
Nederlandse Internisten Vereniging. Diabetes mellitus type 2 in the second line. https://richtlijnendatabase.nl/richtlijn/diabetes_mellitus_type_2_in_de_tweede_lijn/startpagina_bij_dm2_in_de_tweede_lijn.html. Accessed June 2022.
Lau J, Bloch P, Schaffer L, et al. Discovery of the once-weekly glucagon-like peptide-1 (GLP-1) analogue semaglutide. J Med Chem. 2015;58:7370–80.
European Medicines Agency. Ozempic 0.5 mg solution for injection in pre-filled pen. Summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/ozempic-epar-product-information_en.pdf. Accessed June 2022.
Food and Drug Administration. Ozempic 0.5 mg/1.0 mg injection prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/209637s003lbl.pdf. Accessed June 2022.
Sorli C, Harashima SI, Tsoukas GM, et al. Efficacy and safety of once-weekly semaglutide monotherapy versus placebo in patients with type 2 diabetes (SUSTAIN 1): a double-blind, randomised, placebo-controlled, parallel-group, multinational, multicentre phase 3a trial. Lancet Diabetes Endocrinol. 2017;5:251–60.
Ahrén B, Masmiquel L, Kumar H, et al. Efficacy and safety of once-weekly semaglutide versus once-daily sitagliptin as an add-on to metformin, thiazolidinediones, or both, in patients with type 2 diabetes (SUSTAIN 2): a 56-week, double-blind, phase 3a, randomised trial. Lancet Diabetes Endocrinol. 2017;5:341–54.
Ahmann AJ, Capehorn M, Charpentier G, et al. Efficacy and safety of once-weekly semaglutide versus exenatide ER in subjects with type 2 diabetes (SUSTAIN 3): a 56-week, open-label, randomized clinical trial. Diabetes Care. 2018;41:258–66.
Aroda VR, Bain SC, Cariou B, et al. Efficacy and safety of once-weekly semaglutide versus once-daily insulin glargine as add-on to metformin (with or without sulfonylureas) in insulin-I patients with type 2 diabetes (SUSTAIN 4): a randomised, open-label, parallel-group, multicentre, multinational, phase 3a trial. Lancet Diabetes Endocrinol. 2017;5:355–66.
Rodbard HW, Lingvay I, Reed J, et al. Semaglutide added to basal insulin in type 2 diabetes (SUSTAIN 5): a randomized, controlled trial. J Clin Endocrinol Metab. 2018;103:2291–301.
Pratley RE, Aroda VR, Lingvay I, et al. Semaglutide versus dulaglutide once weekly in patients with type 2 diabetes (SUSTAIN 7): a randomised, open-label, phase 3b trial. Lancet Diabetes Endocrinol. 2018;6:275–86.
Lingvay I, Catarig AM, Frias JP, et al. Efficacy and safety of once-weekly semaglutide versus daily canagliflozin as add-on to metformin in patients with type 2 diabetes (SUSTAIN 8): a double-blind, phase 3b, randomised controlled trial. Lancet Diabetes Endocrinol. 2019;7:834–44.
Zinman B, Bhosekar V, Busch R, et al. Semaglutide once weekly as add-on to SGLT-2 inhibitor therapy in type 2 diabetes (SUSTAIN 9): a randomised, placebo-controlled trial. Lancet Diabetes Endocrinol. 2019;7:356–67.
Capehorn MS, Catarig AM, Furberg JK, et al. Efficacy and safety of once-weekly semaglutide 1.0mg vs once-daily liraglutide 1.2mg as add-on to 1–3 oral antidiabetic drugs in subjects with type 2 diabetes (SUSTAIN 10). Diabetes Metab. 2020;46:100–9.
Blonde L, Khunti K, Harris SB, et al. Interpretation and impact of real-world clinical data for the practicing clinician. Adv Ther. 2018;35:1763–74.
Yale JF, Catarig AM, Grau K, et al. Use of once-weekly semaglutide in patients with type 2 diabetes in routine clinical practice: results from the SURE Canada multicentre, prospective, observational study. Diabetes Obes Metab. 2021;23:2269–78.
Ekberg NR, Bodholdt U, Catarig AM, et al. Real-world use of once-weekly semaglutide in patients with type 2 diabetes: results from the SURE Denmark/Sweden multicentre, prospective, observational study. Prim Care Diabetes. 2021;15:871–8.
Rudofsky G, Catarig AM, Favre L, et al. Real-world use of once-weekly semaglutide in patients with type 2 diabetes: results from the SURE Switzerland multicentre, prospective, observational study. Diabetes Res Clin Pract. 2021;178:108931. https://doi.org/10.1016/j.diabres.2021.108931.
Holmes P, Bell HE, Bozkurt K, et al. Real-world use of once-weekly semaglutide in type 2 diabetes: results from the SURE UK multicentre, prospective, observational study. Diabetes Ther. 2021;12:2891–905.
World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4.
International Society for Pharmacoepedimiology. Guidelines for Good Pharmacoepidemiology Practices (GPP). Revision 2 2007. https://www.pharmacoepi.org/resources/policies/guidelines-08027/. Accessed June 2022.
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
Bradley C, Gamsu DS. Guidelines for encouraging psychological well-being: report of a working group of the World Health Organization Regional Office for Europe and International Diabetes Federation European Region St Vincent Declaration Action Programme for Diabetes. Diabet Med. 1994;11:510–6.
Bradley C, Plowright R, Stewart J, et al. The Diabetes Treatment Satisfaction Questionnaire change version (DTSQc) evaluated in insulin glargine trials shows greater responsiveness to improvements than the original DTSQ. Health Qual Life Outcomes. 2007;5:57.
Sorli C, Harashima S-I, Tsoukas GM, et al. Efficacy and safety of once-weekly semaglutide monotherapy versus placebo in subjects with type 2 diabetes (SUSTAIN 1). In: ENDO 2016—98th Annual Meeting of the Endocrine Society 2016;37:OR15–1.
Brown RE, Bech PG, Aronson R. Semaglutide once weekly in people with type 2 diabetes: real-world analysis of the Canadian LMC diabetes registry (SPARE study). Diabetes Obes Metab. 2020;22:2013–20.
Williams DM, Ruslan AM, Khan R, et al. Real-world clinical experience of semaglutide in secondary care diabetes: a retrospective observational study. Diabetes Ther. 2021;12:801–11.
Visaria J, Uzoigwe C, Swift C, et al. Real-world effectiveness of once-weekly semaglutide from a US commercially insured and medicare advantage population. Clin Ther. 2021;43:808–21.
Hansen KB, Svendstrup M, Lund A, et al. Once-weekly subcutaneous semaglutide treatment for persons with type 2 diabetes: real-world data from a diabetes out-patient clinic. Diabet Med. 2021;38: e14655. https://doi.org/10.1111/dme.14655.
Jendle J, Birkenfeld AL, Polonsky WH, et al. Improved treatment satisfaction in patients with type 2 diabetes treated with once-weekly semaglutide in the SUSTAIN trials. Diabetes Obes Metab. 2019;21:2315–26.
Zorginstituut Nederland. GVS advice extension 2016. https://www.zorginstituutnederland.nl/publicaties/adviezen/2016/09/22/gvs-advies-uitbreiding-bijlage-2-voorwaarden-glp-1-agonisten-bij-diabetes-mellitus-type-2. Accessed June 2022.
Acknowledgements
Funding
This study and the journal’s Rapid Service Fee was funded by Novo Nordisk A/S.
Medical Writing, Editorial and Other Assistance
The authors are thankful for the contribution of Sanskruti Jayesh Patel and Nick Fabrin Nielsen (Novo Nordisk A/S) to this manuscript. We thank all the participants, investigators and study-site staff, and Sam Brown (AXON Communications) for medical writing and editorial assistance (funded by Novo Nordisk A/S).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the interpretation of data, the writing and critical revisions of the manuscript at all stages of development. All authors approved the final submitted manuscript. In addition, Dr Andrei-Mircea Catarig contributed to the study design, study conduct and data curation; Miss Alice Clark to the study conduct, data curation and statistical analysis; Mr Maarten Kok to data collection and data curation; Professor Bruce Wolffenbuttel and Drs Michel Brugts, Aloysius G. Lieverse and Jaap van Soest to formal analysis and investigation within the study.
Disclosures
Dr Bruce H.R. Wolffenbuttel has received grant support for clinical studies and also consulting fees for serving on advisory boards and as a speaker for Amgen, Ascensia, AstraZeneca, Eli Lilly and Company, Novo Nordisk, Pfizer and Sanofi. He has also received consulting fees from Eli Lilly and Company as a member of the 4B study and of the DURABLE Trial Data Monitoring Committee, and from Novo Nordisk as principal investigator for the SURE Netherlands study. He is scientific advisor for Ancora Health and Nuevo Care. Dr Michel P. Brugts has received payments from partnerships that he is a member of and has received consulting fees from Novo Nordisk, Sanofi Aventis and Eli Lilly. Dr Andrei-Mircea Catarig is an employee of Novo Nordisk A/S and holds stock shares within the company. Miss Alice Clark is an employee of Novo Nordisk A/S. Mr Maarten Kok is an employee of Novo Nordisk and holds stock shares within the company. Dr Aloysius G. Lieverse has no conflicts of interest to declare. Dr Jaap van Soest has received consulting fees from Novo Nordisk and has received payment for presentations, and educational meetings and advisory boards organised by Novo Nordisk. Investigating physicians were reimbursed for their time spent on documentation and to support data collections and the running of the study.
Compliance with Ethics Guidelines
The study was conducted in accordance with the Declaration of Helsinki of 1964 and its later amendments, and the Guidelines for Good Pharmacoepidemiology Practices. All study materials were approved by the Medical Ethical Review Committee of the University Medical Center Groningen (METC 2019/04/16; reference number AC/nWMO/19.07) and individual study sites. All participants provided their written informed consent. The study is registered on ClinicalTrials.gov (NCT03929679).
Data Availability
The data sets generated during and/or analysed during the current study are available from the sponsor on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wolffenbuttel, B.H.R., Brugts, M.P., Catarig, AM. et al. Once-Weekly Semaglutide Use in Type 2 Diabetes: Real-World Data from the SURE Netherlands Observational Study. Adv Ther 40, 920–933 (2023). https://doi.org/10.1007/s12325-022-02385-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02385-x