Abstract
Introduction
Following hematopoietic stem cell transplantation or solid organ transplantation, patients are at risk of developing Epstein–Barr virus-positive post-transplant lymphoproliferative disease (EBV+ PTLD), which is an ultra-rare and potentially lethal hematologic malignancy. Common treatments for EBV+ PTLD include rituximab alone or combined with chemotherapy. Given specific considerations for this population, including severity of the underlying condition requiring transplant, the rigors of the transplant procedure, as well as risks to the transplanted organ, there is a group of patients with EBV+ PTLD for whom chemotherapy may be inappropriate; however, there is limited information characterizing these patients. This study aimed to reach expert consensus on the key characteristics of patients for whom chemotherapy may be inappropriate in a real-world setting.
Methods
A two-round modified Delphi study was conducted to reach consensus among clinicians with expertise treating EBV+ PTLD. Articles identified in a targeted literature review guided the development of round 1 and 2 topics and related statements. The consensus threshold for round 1 statements was 75.0%. If consensus was achieved in round 1, the statement was not discussed further in round 2. The consensus thresholds for round 2 were moderate (62.5–75.0%), strong (87.5%), or complete (100.0%).
Results
The panel was composed of a total of eight clinicians (seven hematologists/hemato-oncologists) from six European countries. The panel generated a final list of 43 consensus recommendations on the following topics: terminology used to describe patients for whom chemotherapy may be inappropriate; demographic characteristics; organ transplant characteristics; comorbidities that preclude the use of chemotherapy; EBV+ PTLD characteristics; and factors related to treatment-related mortality and morbidity.
Conclusions
This modified Delphi panel successfully achieved consensus on key topics and statements that characterized patients with EBV+ PTLD for whom chemotherapy may be inappropriate. These recommendations will inform clinicians and aid in the treatment of EBV+ PTLD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Recipients of allogeneic hematopoietic stem cell transplantation (HCT) or solid organ transplantation (SOT) are at risk of developing Epstein–Barr virus-positive post-transplant lymphoproliferative disease (EBV+ PTLD), an ultra-rare and potentially lethal hematologic malignancy. |
Standard-dose chemotherapy may not be well tolerated by transplant recipients and is associated with excessive toxicity and increased treatment-related mortality. |
No clinical guidelines or protocols currently describe the characteristics, risk factors, or recommended treatments for patients with EBV+ PTLD who may be ineligible for chemotherapy. |
The purpose of this modified Delphi panel study was to obtain clinical expert consensus on the characterization of patients with EBV+ PTLD for whom chemotherapy may be inappropriate. |
Introduction
Post-transplant lymphoproliferative disease (PTLD) is an ultra-rare and aggressive disease that may occur as a result of immunosuppression following allogeneic hematopoietic stem cell transplantation (HCT) or solid organ transplantation (SOT) [1,2,3]. Nearly all PTLD cases following HCT and 47–68% of PTLD cases following SOT are caused by the Epstein–Barr virus (EBV) [1], which is associated with immune system dysregulation and B cell hyperproliferation during immunosuppression [1, 3]. EBV-positive (EBV+) PTLD may occur via primary infection, when patients who are EBV-seronegative receive a transplant from EBV+ donors, or more frequently, when EBV reactivates in previously infected patients following transplantation [1, 3]. The life-long use of immunosuppressive therapy is a main risk factor for SOT recipients [1].
Treatment options for patients with EBV+ PTLD following HCT and SOT include reduction of immunosuppression (RI), surgery or radiation therapy in localized disease, rituximab monotherapy or rituximab with chemotherapy, use of antiviral agents, and cellular therapy [4,5,6,7,8]. Although there are no approved treatments by the US Food and Drug Administration or the European Medicines Agency for this disease, treatment guidelines from the American Society of Transplantation [9], British Society of Hematology (BSH) [10], European Conference on Infections in Leukemia (ECIL) [11], and the National Comprehensive Cancer Network (NCCN) [12] recommend the response-stratified sequential use of RI, rituximab, then chemotherapy. In patients with EBV+ PTLD following HCT, rituximab monotherapy is used as an established initial treatment; however, chemotherapy is usually reserved as a rescue treatment or is avoided completely as it is associated with high treatment-related mortality and poor outcomes [11, 13,14,15]. Rituximab administered with or without chemotherapy is the recommended therapy in patients with EBV+ PTLD following SOT [7, 9, 10]. The PTLD-1 trial, which included patients with PTLD following SOT, demonstrated safety and efficacy in the sequential treatment of rituximab followed by cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) chemotherapy [16]. A subsequent trial investigating risk-stratified sequential treatment demonstrated the role of rituximab monotherapy consolidation in patients who demonstrated complete remission following four weekly cycles of rituximab induction. Patients who did not exhibit a complete response after four cycles of rituximab received CHOP concomitantly [17,18,19].
Recommended treatments for EBV+ PTLD following transplantation may have treatment-related adverse events. RI can lead to graft-versus-host disease (GvHD) and bone marrow rejection in HCT recipients and rejection of transplanted organs in SOT recipients [1, 2, 11, 13]. Standard-dose chemotherapy is not well tolerated by most HCT and some SOT recipients and is associated with excessive toxicity [6], infectious complications to longstanding immunosuppression in the SOT setting [10, 20], and increased treatment-related mortality in all transplant settings [7, 21, 22]. As a result, many patients will be considered to be ineligible for chemotherapy. Therefore, a challenge in the treatment of EBV+ PTLD is the balance between minimizing treatment-related toxicity and infection, and maintaining transplanted organ function while aiming to cure PTLD.
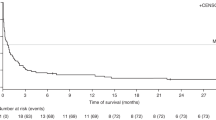
Treatment options are limited if patients have EBV+ PTLD that relapses or is refractory to rituximab and/or chemotherapy [23, 24]. Treatment outcomes in HCT recipients following rituximab treatment failure are usually very poor [25], with a median overall survival (OS) of 0.7 months [24]. Likewise, SOT recipients with EBV+ PTLD that has relapsed or is refractory to rituximab plus chemotherapy have a reported median OS of 4.1 months [23]. Therefore, urgency is required to identify effective, well-tolerated therapies for patients with EBV+ PTLD for whom rituximab and/or chemotherapy has failed.
No clinical guidelines or protocols characterize the specific patients with EBV+ PTLD who may be ineligible for chemotherapy, likely because of the complicated and challenging nature of the condition and the lack of prospective studies on the disease. To address this knowledge gap, the present study used the Delphi method, a structured communication technique that aims to develop consensus among a panel of experts in the presence of limited evidence or when the existing evidence is contradictory within the specific topic of interest. The purpose of this modified Delphi panel study was to obtain clinical expert consensus on the characterization of patients with EBV+ PTLD for whom chemotherapy may be inappropriate. The recommendations from this panel may help inform EBV+ PTLD clinical practice and future clinical trial designs.
Methods
Targeted Literature Review
A targeted literature review was conducted using MEDLINE® via PubMed to identify published practice guidelines, protocols, or epidemiological literature specific to patients with EBV+ PTLD who were unable to receive chemotherapy or for whom chemotherapy may be inappropriate. To retrieve relevant information, results were limited to English language only, human subjects only, and information published within the past 10 years. Identified articles were used to inform topic selection for round 1 discussion, which aimed to achieve consensus on how to characterize the target population. Study procedures are described in Fig. 1.
Modified Delphi Panel Process
Study Design and Panel Selection
This study used the modified Delphi method, a two-round structured process that utilizes surveys to reach consensus on complex issues while preserving participant anonymity [26, 27]. The modified Delphi method for this study was developed prior to panel selection and initiation. Eight clinicians with expertise treating EBV+ PTLD served as Delphi panelists. Panelists were invited on the basis of broad geographical representation and their specialty areas, and two experts served as panel chairs and assisted in selecting round 1 topics that would be suitable for wider panel discussion.
Round 1 Survey
The round 1 online survey consisted of 90 statements that focused on terminology and characteristics that describe patients with EBV+ PTLD who were unable to receive chemotherapy or for whom chemotherapy may be inappropriate. The survey included a mixture of open-ended and closed-ended statements that focused on five main topics: (1) terminology to describe the patient population of interest; (2) demographic characteristics; (3) organ transplant characteristics; (4) comorbidities that preclude the use of CHOP; and (5) factors related to chemotherapy-related mortality and morbidity. The results from the round 1 survey helped to determine the statements and wording of response options that were featured in the round 2 survey.
Round 2 Survey
The round 2 online survey consisted of 72 statements that aimed to achieve consensus on the terminology and characteristics that describe patients with EBV+ PTLD for whom chemotherapy may be inappropriate. In this round, the definition of chemotherapy was broadened from CHOP to standard-dose chemotherapy. Four main topics were included: (1) demographic characteristics and (2) organ transplant characteristics of patients for whom standard-dose chemotherapy is not appropriate; (3) comorbidities that preclude the use of standard-dose chemotherapy; and (4) factors related to chemotherapy-related mortality and morbidity.
Data Analysis
A five-point Likert scale was used in rounds 1 and 2 to assess panelist alignment on closed-ended questions. Likert scale agreement was met if clinicians responded with “agree” or “strongly agree”, or “disagree” or “strongly disagree.” For open-ended questions, clinician responses were coded using qualitative methods to merge similar concepts and determine consensus.
Consensus thresholds used in this study were established a priori and aligned with those used in previous Delphi panels [27]. The consensus threshold for the round 1 survey was 75.0% of panelist responses. If a statement or concept in round 1 reached this threshold, it was considered to have reached consensus and was not subsequently voted on during round 2. Three consensus thresholds were used for the round 2 survey: moderate (62.5–75.0%), strong (87.5%), or complete (100.0%).
The goal of both surveys was to reach consensus on subtopic statements (e.g., impaired heart function and impaired liver function) within a main topic (e.g., comorbidities that may preclude the use of chemotherapy). Survey data and panelist demographic information were summarized descriptively.
Compliance with Ethics Guidelines
This article is based on a modified Delphi panel study, which collated confidential online survey responses on a specific topic from eight clinicians who served as panelists. Approval from an ethics committee or an internal review board was not required as this study was considered as a consensus development technique and did not involve research on patients. All participating clinicians agreed to serve as panelists, agreed with the modified Delphi panel study objectives, participated in manuscript development, and agreed to the publication of this manuscript.
Results
Publications from Literature Review
Of the 110 abstracts identified via a PubMed MEDLINE® search, 21 articles were selected for full article review, and 15 were selected for in-depth review and analysis based on the inclusion and exclusion criteria. This review yielded limited information on the characterization of patients with EBV+ PTLD for whom chemotherapy may be inappropriate. Findings and key questions identified in the review were summarized by topic (demographics, organ transplant characteristics, PTLD characteristics, comorbidities that preclude the use of CHOP chemotherapy, and factors related to treatment-related mortality and morbidity) and subtopic (e.g., age or type of organ; Supplementary Material Table S1).
Panelists’ Clinical Expertise
Given the rarity of EBV+ PTLD, panelists were selected from a small pool of clinicians with expertise in the treatment and management of EBV+ PTLD. Eight clinical experts were invited to serve on the study panel. All panelists participated in and completed round 1 and 2 surveys. The panel was mostly composed of hematologists/hemato-oncologists (n = 7, 87.5%), with all panelists having expertise in treating EBV+ PTLD. Expertise was based on the number of years treating patients with EBV+ PTLD (mean [range] 17.1 [5–30]) and the number of patients managed for PTLD in the previous 2 years (mean [range] 21 [10–50]). On average, 42.5% of managed patients with PTLD were EBV+. Additional information on the panelists’ demographic characteristics and clinical expertise can be found in Supplementary Material Table S2.
Delphi Panel Survey Results
Survey topics included in rounds 1 and 2 are presented in Table 1. Statements that achieved consensus in round 1 were not discussed further in round 2.
Round 1 Survey Results
Panelists reviewed 42 statements on the following topics: terminology to describe the relevant patient population; age ranges of pediatric, adult, and geriatric patients; socio-economic demographics; and patient clinical status assessments and characteristics. Overall, 23 (54.8%) statements reached a consensus of at least 75.0%, and 17 statements did not reach consensus.
Terminology and Demographic Characteristics to Describe Target Patients
Panelists agreed that the terms “CHOP-inappropriate” and “CHOP-ineligible” can be used interchangeably to describe patients who receive rituximab treatment, do not achieve a complete response, and those who would not be recommended to receive CHOP chemotherapy (Table 2). Additionally, panelists agreed on the minimum and maximum ages that define pediatric and geriatric patients. Panelists also achieved consensus on specific patient characteristics (e.g., Eastern Cooperative Oncology Group [ECOG] performance and Karnofsky performance criteria) and clinical assessments that should be used to determine chemotherapy treatment eligibility (Table 2).
Round 2 Survey Results
Open-ended responses and subsequent discussion from round 1 generated 70 statements for round 2 review. At this stage, the definition of chemotherapy was broadened from CHOP to standard-dose chemotherapy. These statements aimed to achieve consensus on recommendations regarding patient demographics, organ transplant characteristics, comorbidities, and risk of chemotherapy-related mortality and morbidity. Of the 70 statements generated, 42 (60.0%) reached complete, strong, or moderate consensus, and 28 did not reach consensus.
Patient Demographic and Clinical Characteristics
Two statements regarding patient demographic characteristics achieved moderate or complete consensus, with panelists agreeing that dose-adjusted chemotherapy should be considered for pediatric patients with EBV+ PTLD and for geriatric populations with poor clinical status (Table 2). Panelists were also asked to identify clinical assessments that may be used to determine eligibility for standard-dose chemotherapy. Experts agreed, with strong to complete consensus, on using the following assessments in patients with EBV+ PTLD: cardiological evaluation, Child–Pugh score, complete blood count, frailty assessments, glomerular filtration rate (GFR), hepatitis B/C tests using polymerase chain reaction, heart function assessment, and left ventricular ejection fraction. For geriatric patients, the panelists also recommended with moderate to complete consensus to use the Cumulative Illness Rating Scale–geriatric score, the comprehensive geriatric assessment, and performance assessments to determine eligibility for standard-dose chemotherapy.
Organ Transplant Characteristics
Five statements regarding organ transplant characteristics of patients who may be inappropriate for standard-dose chemotherapy achieved complete (n = 2), strong (n = 1), or moderate (n = 2) consensus (Table 2). Panelists agreed that patients with EBV+ PTLD who have reduced or compromised heart function, liver function, kidney allograft transplant function, or have had a bone marrow transplant with leukopenia should not receive standard-dose chemotherapy.
EBV+ PTLD Characteristics
Moderate consensus was achieved on the classifications of EBV+ PTLD that may be inappropriate for chemotherapy. Panelists agreed that patients with plasmacytic hyperplasia, infectious mononucleosis-like PTLD, florid follicular hyperplasia (non-destructive PTLD), and classic Hodgkin’s lymphoma EBV+ PTLD should not receive standard-dose CHOP chemotherapy (Table 2).
Patient Comorbidities
Twenty-two statements describing patient comorbidities that preclude the use of standard-dose chemotherapy reached complete (n = 4), strong (n = 10), and moderate (n = 8) consensus (Table 2). Panelists agreed that patients with EBV+ PTLD who are frail, have impaired organ function, or have a prior inadequate response to chemotherapy should not be treated using standard-dose chemotherapy.
Factors Associated with Chemotherapy-Related Mortality and Morbidity
In this study, 12 statements describing factors associated with chemotherapy-related mortality and morbidity achieved complete (n = 2), strong (n = 3), or moderate (n = 7) consensus (Table 2). Panelists agreed that adult patients who have an ECOG score of 0–2 should receive standard-dose chemotherapy. Additionally, panelists agreed that patients with EBV+ PTLD should not receive standard-dose chemotherapy because of an increased risk of treatment-related toxicity or mortality if they also exhibit the following: thrombocytopenia (< 100 platelets/nL); GFR < 10 mL/min/1.73 m2; or previous treatment-related toxicity (i.e., common toxicity criteria grade III/IV). Panelists also considered if a GFR < 30 mL/min/1.73 m2 would preclude the use of standard-dose chemotherapy for EBV+ PTLD but did not achieve consensus. Regarding post-treatment infection, panelists reached a strong consensus that all patients with EBV+ PTLD are at risk of developing infection post chemotherapy. Patients with existing or previous infections, or those who have undergone HCT, have an increased risk of developing an infection post chemotherapy.
Discussion
The modified Delphi panel is an established method that is used to achieve consensus on important topics where limited evidence exists. This study is the first to achieve expert consensus on detailed characteristics describing the EBV+ PTLD patient population for whom chemotherapy may be inappropriate. The panel agreed that the terms “CHOP-inappropriate” and “CHOP-ineligible” could be used to describe patients for whom standard-dose chemotherapy is not recommended, despite these patients not achieving an adequate response to rituximab treatment. The panel also agreed that clinical characteristics such as impaired organ function, a poor ECOG performance status score, and/or a prior inadequate response to chemotherapy would preclude treatment with standard-dose chemotherapy.
The panel provided further clarity on the limited information obtained from the target literature review. Overall, articles used for survey development indicated that patients with EBV+ PTLD are at a significant risk of treatment-related toxicity and mortality when undergoing chemotherapy [21, 28,29,30,31,32]. Chemotherapy also increases the risk of post-treatment infection and can exacerbate GvHD in EBV+ PTLD following HCT [33,34,35]. Similarly, panelists achieved strong or moderate consensus on four statements regarding post-chemotherapy mortality and morbidity, agreeing that all patients with EBV+ PTLD, especially HCT recipients, are at risk of developing infections post chemotherapy treatment. The literature suggests that patients with an aggressive form of EBV+ PTLD or with a rapidly declining clinical status, including pediatric populations, may benefit upfront from chemotherapy [11, 35]. However, guidance was not provided on dose. The panel provided additional clarification and recommended that pediatric and geriatric patients with poor clinical status should receive dose-adjusted chemotherapy.
A number of statements in the round 2 survey, including demographic characteristics of patients who should receive dose-adjusted chemotherapy, socio-demographic factors determining CHOP eligibility, and the type of transplants that may make CHOP inappropriate for treatment, did not achieve panel consensus (Supplementary Material Table S3). These statements were based on open-ended responses that were submitted during round 1, and in general, panelists were not able to provide significant input on these based on varied clinical experience.
Certain clinical and demographic characteristics identified in this study (i.e., impaired organ or bone marrow function, a high ECOG score, or a history of HCT) would categorize a considerable number of patients as being inappropriate for standard-dose chemotherapy. Further, patients with EBV+ PTLD who do respond to chemotherapy may need multiple rounds of treatment [36], which may increase the risk of treatment-related adverse events and may lead to reduced quality of life with long-term adverse consequences [37]. Therefore, it is critical to provide these patients with well-tolerated, alternative treatments with reduced risk of treatment-related toxicity. There are a limited number of chemotherapy-sparing treatment options being studied for EBV+ PTLD following HCT or SOT, including the adoptive transfer of EBV-specific cytotoxic T lymphocytes (CTLs)—an approach that is already incorporated into the BSH, ECIL, and NCCN guidelines as a rescue therapy for this disease [10,11,12]. Cellular therapy using autologous and HCT donor-derived EBV-CTLs has resulted in complete and partial responses with minimal treatment-related toxicity [4, 38]. Although there are no therapies currently approved for EBV+ PTLD, the ongoing phase III ALLELE trial (NCT03394365) continues to evaluate the efficacy and safety of allogeneic EBV-CTL therapy in allogeneic HCT or SOT recipients with EBV+ PTLD following failure of rituximab or rituximab plus chemotherapy treatments.
This modified Delphi panel study has several potential limitations. The panel consisted of eight clinical experts, which is a slightly smaller number than the recommended 10–15 [39, 40]. EBV+ PTLD is an ultra-rare disease, with an incidence of less than 1 in 1 million. Given this ultra-rarity, these clinical experts are among the top treaters of the disease in Europe. Consensus recommendations have been outlined in this study by clinical experts for Europe; however, given that the treatment paradigm is similar in other regions and there are no treatment options in patients with relapsed/refractory EBV+ PTLD, the recommendations are applicable more globally.
Conclusion
This modified Delphi study achieved expert consensus on recommendations that characterize patients with EBV+ PTLD for whom chemotherapy may be inappropriate. These statements will provide guidance for assessing chemotherapy eligibility in a real-world clinical setting. This paper identifies important factors that should be accounted for when choosing a treatment regimen for patients with EBV+ PTLD.
References
Dierickx D, Habermann TM. Post-transplantation lymphoproliferative disorders in adults. N Engl J Med. 2018;378(6):549–62.
Nijland ML, Kersten MJ, Pals ST, Bemelman FJ, Ten Berge IJ. Epstein-Barr virus-positive posttransplant lymphoproliferative disease after solid organ transplantation: pathogenesis, clinical manifestations, diagnosis, and management. Transplant Direct. 2016;2(1):e48.
Ibrahim HA, Naresh KN. Posttransplant lymphoproliferative disorders. Adv Hematol. 2012;2012:230173.
Prockop S, Doubrovina E, Suser S, et al. Off-the-shelf EBV-specific T cell immunotherapy for rituximab-refractory EBV-associated lymphoma following transplantation. J Clin Invest. 2020;130(2):733–47.
Al Hamed R, Bazarbachi AH, Mohty M. Epstein-Barr virus-related post-transplant lymphoproliferative disease (EBV-PTLD) in the setting of allogeneic stem cell transplantation: a comprehensive review from pathogenesis to forthcoming treatment modalities. Bone Marrow Transplant. 2020;55(1):25–39.
Craddock J, Heslop HE. Adoptive cellular therapy with T cells specific for EBV-derived tumor antigens. Update Cancer Ther. 2008;3(1):33–41.
Choquet S, Trappe R, Leblond V, Jager U, Davi F, Oertel S. CHOP-21 for the treatment of post-transplant lymphoproliferative disorders (PTLD) following solid organ transplantation. Haematologica. 2007;92(2):273–4.
Kamble RT, Brown VI, Prockop S, et al. Post-transplant lymphoproliferative disorders arising after allogeneic hematopoietic cell transplantation: a comprehensive review. Ann Hematol Oncol. 2020;7(1):1279.
Allen UD, Preiksaitis JK, AST Infectious Diseases Community of Practice. Post-transplant lymphoproliferative disorders, Epstein-Barr virus infection, and disease in solid organ transplantation: guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019;33(9):e13652.
Shah N, Eyre TA, Tucker D, et al. Front-line management of post-transplantation lymphoproliferative disorder in adult solid organ recipient patients—a British Society for Haematology Guideline. Br J Haematol. 2021;193(4):727–40.
Styczynski J, van der Velden W, Fox CP, et al. Management of Epstein-Barr virus infections and post-transplant lymphoproliferative disorders in patients after allogeneic hematopoietic stem cell transplantation: Sixth European Conference on Infections in Leukemia (ECIL-6) guidelines. Haematologica. 2016;101(7):803–11.
National Comprehensive Cancer Network. Diffuse large B-cell lymphoma (Version 4.2020) 2020. https://www.nccn.org/patients/guidelines/content/PDF/nhl-diffuse-patient.pdf.
Uhlin M, Wikell H, Sundin M, et al. Risk factors for Epstein-Barr virus-related post-transplant lymphoproliferative disease after allogeneic hematopoietic stem cell transplantation. Haematologica. 2014;99(2):346–52.
Fox CP, Burns D, Parker AN, et al. EBV-associated post-transplant lymphoproliferative disorder following in vivo T-cell-depleted allogeneic transplantation: clinical features, viral load correlates and prognostic factors in the rituximab era. Bone Marrow Transplant. 2014;49(2):280–6.
Watson C, Barlev A, Worrall J, Duff S, Beckerman R. Exploring the burden of short-term CHOP chemotherapy adverse events in post-transplant lymphoproliferative disease: a comprehensive literature review in lymphoma patients. J Drug Assess. 2020;10(1):18–26.
Trappe R, Oertel S, Leblond V, et al. Sequential treatment with rituximab followed by CHOP chemotherapy in adult B-cell post-transplant lymphoproliferative disorder (PTLD): the prospective international multicentre phase 2 PTLD-1 trial. Lancet Oncol. 2012;13(2):196–206.
Trappe RU, Dierickx D, Zimmermann H, et al. Response to rituximab induction is a predictive marker in B-cell post-transplant lymphoproliferative disorder and allows successful stratification into rituximab or R-CHOP consolidation in an international, prospective, multicenter phase II trial. J Clin Oncol. 2017;35(5):536–43.
Gonzalez-Barca E, Capote FJ, Gomez-Codina J, et al. Long-term follow-up of a prospective phase 2 clinical trial of extended treatment with rituximab in patients with B cell post-transplant lymphoproliferative disease and validation in real world patients. Ann Hematol. 2021;100(4):1023–9.
Gonzalez-Barca E, Domingo-Domenech E, Capote FJ, et al. Prospective phase II trial of extended treatment with rituximab in patients with B-cell post-transplant lymphoproliferative disease. Haematologica. 2007;92(11):1489–94.
Zimmermann H, Trappe RU. Therapeutic options in post-transplant lymphoproliferative disorders. Ther Adv Hematol. 2011;2(6):393–407.
Ocheni S, Kroeger N, Zabelina T, et al. EBV reactivation and post transplant lymphoproliferative disorders following allogeneic SCT. Bone Marrow Transplant. 2008;42(3):181–6.
Styczynski J, Gil L, Tridello G, et al. Response to rituximab-based therapy and risk factor analysis in Epstein Barr virus-related lymphoproliferative disorder after hematopoietic stem cell transplant in children and adults: a study from the Infectious Diseases Working Party of the European Group for Blood and Marrow Transplantation. Clin Infect Dis. 2013;57(6):794–802.
Dharnidharka V, Thirumalai D, Jager U, et al. Clinical outcomes of solid organ transplant patients with Epstein-Barr virus-driven (EBV+) post-transplant lymphoproliferative disorder (PTLD) who fail rituximab plus chemotherapy: a multinational, retrospective chart review study. Blood. 2021;138:2528.
Sanz J, Storek J, Socie G, et al. Clinical outcomes of patients with Epstein-Barr virus-driven post-transplant lymphoproliferative disease following hematopoietic stem cell transplantation who fail rituximab: a multinational, retrospective chart review study. Blood. 2021;138:1454.
Shahid S, Prockop SE. Epstein-Barr virus-associated post-transplant lymphoproliferative disorders: beyond chemotherapy treatment. Cancer Drug Resist. 2021;4:646–64.
Brown BB. Delphi process: a methodology used for the elicitation of opinions of experts. ASTME Vectors. 1968:1–18.
Vernon W. The Delphi technique: a review. Int J Ther Rehabil. 2009;16(2):69–76.
DeStefano CB, Desai SH, Shenoy AG, Catlett JP. Management of post-transplant lymphoproliferative disorders. Br J Haematol. 2018;182(3):330–43.
Jagadeesh D, Woda BA, Draper J, Evens AM. Post transplant lymphoproliferative disorders: risk, classification, and therapeutic recommendations. Curr Treat Options Oncol. 2012;13(1):122–36.
Kumarasinghe G, Lavee O, Parker A, et al. Post-transplant lymphoproliferative disease in heart and lung transplantation: defining risk and prognostic factors. J Heart Lung Transplant. 2015;34(11):1406–14.
Murukesan V, Mukherjee S. Managing post-transplant lymphoproliferative disorders in solid-organ transplant recipients: a review of immunosuppressant regimens. Drugs. 2012;72(12):1631–43.
Simakachorn L, Tanpowpong P, Lertudomphonwani C, et al. Various initial presentations of Epstein-Barr virus infection-associated post-transplant lymphoproliferative disorder in pediatric liver transplantation recipients: case series and literature review. Pediatr Transplant. 2019;23(2):e13357.
Absalon MJ, Khoury RA, Phillips CL. Post-transplant lymphoproliferative disorder after solid-organ transplant in children. Semin Pediatr Surg. 2017;26(4):257–66.
Lauro A, Arpinati M, Pinna AD. Managing the challenge of PTLD in liver and bowel transplant recipients. Br J Haematol. 2015;169(2):157–72.
Sullivan BJ, Kim GJ, Sara G. Treatment dilemma for survivors of rituximab-induced bowel perforation in the setting of post-transplant lymphoproliferative disorder. BMJ Case Rep. 2018;11(1):e226666.
Styczynski J, Einsele H, Gil L, Ljungman P. Outcome of treatment of Epstein-Barr virus-related post-transplant lymphoproliferative disorder in hematopoietic stem cell recipients: a comprehensive review of reported cases. Transpl Infect Dis. 2009;11(5):383–92.
Watson C, Gadikota H, Barlev A, Beckerman R. A review of the risks of long-term consequences associated with components of the CHOP chemotherapy regimen. J Drug Assess. 2022;11(1):1–11.
Smith C, Khanna R. Adoptive cellular immunotherapy for virus-associated cancers: a new paradigm in personalized medicine. Immunol Cell Biol. 2017;95(4):364–71.
Cantrill JA, Sibbald B, Buetow S. The Delphi and nominal group techniques in health services research. Int J Pharm Pract. 1996;4(2):67–74.
Delbecq AL, Van de Ven AH, Gustafson DH. Group techniques for program planning: a guide to nominal group and Delphi processes. Glenview: Scott Foresman; 1975.
Acknowledgements
Funding
Atara Biotherapeutics, Inc. sponsored this study and the journal’s Rapid Service and Open Access fees.
Medical Writing, Editorial, and Other Assistance
Writing assistance was provided by Cindy Chiu, PhD, and Folabomi Oladosu, PhD, from AMICULUM USA, funded by Atara Biotherapeutics, Inc. The authors thank Endpoint Outcomes, Inc. (now Lumanity, Inc.) for conducting the surveys.
Author Contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article. Sridhar Chaganti, Arie Barlev, Natalia Sadetsky, Anke Friedetzky, Dhanalakshmi Thirumalai and Ralf U. Trappe contributed to study conception and design, data analysis, and data interpretation. All authors revised the manuscript critically for relevant content, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosures
Sridhar Chaganti has served as a consultant for and received honoraria from AbbVie, Adicet Bio, Atara Biotherapeutics, Gilead Sciences, Gilead/Kite, Novartis, Orion Pharma, Pierre Fabre, Roche, and Takeda. Sophie Caillard has served as a consultant for AstraZeneca. Sylvain Choquet served as a consultant for Atara Biotherapeutics, AbbVie, Accord Healthcare, AstraZeneca, Biogaran, Gilead/Kite, Janssen, Pierre Fabre, Roche, Sandoz/Novartis, Takeda, and Viatris. Kate Cwynarski has served as a consultant for Atara Biotherapeutics, Celgene/BMS, Gilead/Kite, Incyte, Janssen, Roche, and Takeda; served on a speakers’ bureau for Gilead/Kite, Incyte, Roche, and Takeda; and have received travel support from BMS, Gilead/Kite, Janssen, Roche, and Takeda. Eva González-Barca has received honoraria from AbbVie, EUSA Pharma, Janssen, Takeda, Roche, Incyte; served as a consultant for AbbVie, BeiGene, EUSA Pharma, Gilead Sciences, Incyte, Janssen, Kiowa, Lilly, and Novartis; and received travel funds from EUSA Pharma and Janssen. Stefan Schneeberger has served as a consultant for Astellas, Atara Biotherapeutics, Merck, NefroHealth, Novartis, Sandoz, and Teva; received grants/research support from Bridge to Life, Chiesi, Neovii, Novartis, Organ Recovery Systems, and Sandoz; and speakers’ bureau/honoraria from Astellas, BMS, Chiesi, Novartis, OrganOx, and Sanofi. Pier Luigi Zinzani has served on advisory boards with AbbVie, Gilead Sciences, Incyte, Merck, Portola, Roche, Sanofi, Servier, and Takeda; has served as a consultant for BMS, BMS/Celgene, Celltron, EUSA Pharma, Gilead Sciences, Immune Design, Janssen-Cilag, Kyowa Kirin, Merck Sharp & Dohme, Roche, Sandoz, Verastem; received honoraria from AbbVie, ADC Therapeutics, BMS, Debiopharm, EUSA Pharma, Gilead Sciences, Incyte, Janssen, Kyowa Kirin, Merck, Roche, Servier, Takeda, TG Therapeutics, Verastem; received research funding from Portola; and served on a speaker’s bureau for AbbVie, ADC Therapeutics, BMS, BMS/Celgene, Celltron, EUSA Pharma, Gilead Sciences, Immune Design, Incyte, Janssen, Janssen-Cilag, Kyowa Kirin, Merck, MSD, Portola, Roche, Sandoz, Servier, Takeda, TG Therapeutics, and Verastem. Ralf Ulrich Trappe has served as a consultant for and has received travel funds and research funding from Atara Biotherapeutics. Dr. Trappe has also received travel funds from AbbVie, BMS/Celgene, GSK, Janssen, and Roche. Arie Barlev, Anke Friedetzky, and Dhanalakshmi Thirumalai are employees and shareholders of Atara Biotherapeutics. Natalia Sadetsky was an employee and shareholder of Atara Biotherapeutics during the development of the manuscript; her current affiliation is Gilead Sciences.
Compliance with Ethics Guidelines
This article is based on a modified Delphi panel study, which collated confidential online survey responses on a specific topic from eight clinicians who served as panelists. Approval from an ethics committee or an internal review board was not required as this study was considered as a consensus development technique and did not involve research on patients. All participating clinicians agreed to serve as panelists, agreed with the modified Delphi panel study objectives, participated in manuscript development, and agreed to the publication of this manuscript.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chaganti, S., Barlev, A., Caillard, S. et al. Expert Consensus on the Characteristics of Patients with Epstein–Barr Virus-Positive Post-Transplant Lymphoproliferative Disease (EBV+ PTLD) for Whom Standard-Dose Chemotherapy May be Inappropriate: A Modified Delphi Study. Adv Ther 40, 1267–1281 (2023). https://doi.org/10.1007/s12325-022-02383-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02383-z