Abstract
Introduction
Long-acting injectable antipsychotic agents have been suggested to improve adherence and patient outcomes in schizophrenia or schizoaffective disorder. The purpose of this study was to assess medication use patterns (i.e., medication adherence, persistence), hospital and emergency department readmissions, and total direct medical costs of Oklahoma Medicaid members with schizophrenia or schizoaffective disorder switching from an oral antipsychotic (OAP) to once-monthly paliperidone palmitate (PP1M) or to another OAP (OAP-switch).
Methods
A historical cohort analysis was conducted from 1 January 2016 to 31 December 2020 among adults aged ≥ 18 and ≤ 64 years with schizophrenia or schizoaffective disorder who were previously treated with an OAP. The first claim for PP1M or a new OAP defined the study index date. Members who transitioned from PP1M to 3-month formulation (PP3M) were included (i.e., PP1M/PP3M). Proportion of days covered (PDC), 45-day treatment gaps, 30-day readmissions to hospitals or emergency department, and total direct medical costs were assessed using multivariable, machine-learning least absolute shrinkage, and selection operator (Lasso) regressions controlling for numerous demographic, clinical, mental health, and provider characteristics.
Results
Among 295 Medicaid members meeting full inclusion criteria, 183 involved PP1M/PP3Ms (44 PP1M cases transitioned to PP3M) and 112 involved an OAP-switch. The multivariable-adjusted odds of readmission were significantly associated with a 45-day treatment gap (p < 0.05) and non-adherence (i.e., PDC < 80%) (p < 0.05). Relative to PP1M/PP3Ms, the multivariable analyses also indicated that OAP-switch was associated with an 18.5% lower PDC, 92.3% higher number of 45-day treatment gaps, and an approximately 90% higher odds of all-cause 30-day readmission (p < 0.05). The adjusted pre- to post-index change in cost was approximately 49% lower for OAP-switches versus PP1M/PP3Ms (p < 0.001), although unadjusted post-index costs did not differ between groups (p = 0.440).
Conclusion
This real-world investigation of adult Medicaid members with schizophrenia or schizoaffective disorder observed improved adherence and persistence with fewer readmissions with PP1M/PP3Ms versus OAP-switches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Persons with schizophrenia (SCZ) or schizoaffective disorder (SCD) often require switches in therapy. Compared with oral antipsychotic medications (OAP), long-acting injectable antipsychotic medications may be associated with improved adherence and persistence and reductions in hospitalizations, readmissions, and costs. |
This study assessed medication adherence, persistence, readmissions, and total comprehensive direct medical costs of Oklahoma Medicaid members with SCZ or SCD previously treated with an OAP who switched to once-monthly paliperidone palmitate (PP1M) or another OAP. |
What was learned from the study? |
Results from multivariable, machine-learning least absolute shrinkage, and selection operator (Lasso) regression observed significantly improved adjusted adherence and persistence, fewer readmissions, and a greater change in total costs for members switching to PP1M compared with those switching to another OAP. |
The presence of any 45-day gap in medication treatment was independently associated with a 2.7 times adjusted higher odds of hospital or emergency department readmission, whereas adherence (defined as 80% or greater proportion of days covered) was associated with a 65% lower adjusted odds of readmission. |
Targeted and supportive interventions are needed to minimize poor adherence and persistence and improve outcomes in this vulnerable population. |
Introduction
Schizophrenia (SCZ) is a severe psychiatric disorder with a substantial health, social, occupational, and economic burden [1]. In the USA, prevalence of SCZ is estimated to be between 0.25% and 0.64% [2, 3] and is one of the top 20 causes of disability [4]. SCZ is associated with an increased risk of substance abuse, suicide, and mortality compared with the general population [1, 5]. Schizoaffective disorder (SCD) is a psychiatric disorder characterized by mixed symptoms of SCZ and mood disorders [6]. The estimated lifetime prevalence of SCD is 0.3%, and the presence of SCD is associated with higher rates of hospitalization, suicide, and substance abuse compared with SCZ [6]. Cloutier et al. [7] estimated that the total annual economic burden of SCZ in the USA was $150 billion, with 24% involving direct patient care related to inpatient services, medications, and outpatient services [7]. Inpatient and emergency department (ED) care is estimated to account for 10% of total healthcare costs [7].
Antipsychotic agents are used in the management of acute episodes of SCZ and SCD, and in the continued management following recovery to prevent relapse [1, 8]. The American Psychological Association (APA) practice guidelines recommend treatment for patients to include initiating antipsychotic medication, continuing treatment once symptoms improve (e.g., adherence), and maintaining consistent treatment over time (e.g., persistence) [1]. Numerous oral antipsychotic agents (OAPs) have been approved specifically for use in SCZ and SCD [6, 9, 10]. Newer second-generation long-acting injectable antipsychotic agents (LAIs) have been introduced and are recommended by the APA in cases involving known non-adherence, or if substantial uncertainty surrounds medication-taking behavior [1]. Despite positive clinical outcomes of continued therapy to mitigate SCZ or SCD relapse, treatment non-adherence occurs in up to 50% of patients [11]. Several factors may contribute to non-adherence or poor persistence in SCZ and SCD, with management interventions often requiring a switch in OAP therapeutic agents or initiating LAIs [1, 12, 13].
Kane et al. [12] noted that switching among OAPs or initiating an LAI was an advocated clinical approach to address non-adherence, while Haddad et al. [13] stated that a trial of LAIs might assist clinicians to ascertain if potential treatment failure in SCZ could be due to either non-adherence or treatment resistance. APA guidelines recommend that patients with SCZ who have a history of poor or uncertain adherence receive LAI therapy [1]. A meta-analysis conducted by Lin et al. [14], which included Medicaid and claims-based analyses, reported that the utilization of LAIs was associated with an improved odds of medication adherence compared with OAPs. LAIs were also associated with a lower odds for hospitalization and fewer admissions to hospitals or EDs [14]. LAIs may also be associated with improved persistence relative to OAPs [15]. In a 2021 meta-analysis of real-world studies, the relative risk of treatment discontinuation was lower with an LAI formulation of risperidone versus several OAPs [15].
Paliperidone palmitate is an LAI with a 1-month formulation (PP1M) approved by the US Food and Drug Administration (FDA) for both SCZ and SCD [16], and with 3-month (PP3M) and 6-month (PP6M) formulations approved specifically for SCZ [17, 18]. Research indicates that PP1M use is associated with a lower odds of hospital admission and potentially lower costs compared with OAPs in SCZ [19,20,21,22]. Building upon previous studies, a continued need exists to assess the association between PP1M/PP3M use on adherence, persistence, readmissions, and costs, particularly in applying more robust and extensive multivariable models to control for potential confounders of outcomes. Incorporating machine-learning algorithms, the objective of this study was to assess medication use patterns (i.e., medication adherence, persistence), readmissions, and total direct medical costs of Oklahoma Medicaid members with SCZ or SCD previously treated with an OAP and switching to PP1M or another OAP (OAP-switch).
Methods
This retrospective study utilized an historical cohort of comprehensive, transaction-level medical and pharmacy Oklahoma Medicaid administrative claims data from 1 January 2016 to 31 December 2019. More specifically, these data represented more than 750,000 Oklahoma Medicaid members and included information on demographics (e.g., age, sex, race, metro/urban residence), pharmacy claims (e.g., drug, date of transaction, quantity filled, days’ supply, prescriber, reimbursement amount), and medical claims (e.g., diagnoses, inpatient/outpatient/ED visits, long-term care, reimbursement amount). This study was defined as exempt by the Office of Human Research Participant Protection (institutional review board #12942) at the University of Oklahoma Health Sciences Center.
The study population comprised adult Medicaid members ≥ 18 and ≤ 64 years of age with one or more inpatient or two or more outpatient claims involving relevant SCZ or SCD diagnoses [based on International Classification of Diseases, Ninth or Tenth Revision, Clinical Modification (ICD-9-CM, ICD-10-CM) [23, 24] codes for SCZ (295.XX, F20.XX) or SCD (297.5, F25.9)] plus two or more prescription claims for an OAP within a 6-month period before switching to another OAP (for qualifying medications, see Supplementary Material Appendix S1). The study’s index date was defined as the initial PP1M prescription fill (following pre-index OAP use) or an OAP monotherapy switch (with the “OAP-switch” defined by the first claim of a new OAP following a pre-index OAP and also requiring two or more paid prescription claims for the new OAP within 60 days after the first claim). Inclusion criteria also required continuous Medicaid eligibility for a minimum of 12 months pre-index and at least 12 months post-index. Exclusion criteria included any use of clozapine across the study’s timeframe, any concomitant LAI use, dual Medicaid and Medicare eligibility (i.e., due to limited data availability), or any healthcare coverage within the Indian Health Service (i.e., also due to limited data availability). No index medication could be utilized within 6 months prior to the index date to ensure that members were naïve to an index medication.
Two comparative cohorts were defined via the index medication category as: (1) PP1M treatment initiation following pre-index OAP use (e.g., a switch from an OAP to PP1M defined as “PP1M initiation”) and (2) switching to a different OAP following pre-index OAP use (i.e., defined as “OAP-switch”). Members of the PP1M cohort were permitted to transition to PP3M; therefore, the PP1M initiation cohort also included those that extended treatment in the PP1M/PP3M group. A paid prescription claim for PP1M or PP3M required prior authorization from Oklahoma Medicaid throughout the study timeframe, and prior authorization criteria of a PP1M or PP3M were in congruence with FDA-approved indications for use [16, 17]. Thus, consistent with medical practice standards and medication labeling, Medicaid members could transition to PP3M only if they were adequately treated with PP1M. The rationale for the choice of comparators of PP1M/PP3M and OAP-switch was based on guideline recommendations that patients who are non-adherent to OAP therapy be switched to an LAI [1], though real-world clinical observations have indicated that many non-adherent cases are switched to another OAP rather than initiating treatment with an LAI [25].The study’s focus on paliperidone palmitate is, in part, due to its uniquely different indication within the therapeutic class—paliperidone is the only long-acting injectable antipsychotic (LAI) with a current indication that also includes schizoaffective disorder [16]. Overall, paliperidone palmitate (PP1M) as a focal LAI has received substantial attention by the clinical and scientific community, summarized across 25 studies within the meta-analysis conducted by Lin et al. [14]. The study’s outcomes of medication use patterns included adherence [defined via a continuous measure of proportion of days covered (PDC)] and persistence (defined as the continuous or count number of 45-day treatment gaps). Of note, PDC remains a recommended approach to measuring adherence, and is calculated as the number of days covered by the medication divided by the number of days in the study period following the index date until the end of follow-up (i.e., the number of days in the measurement period) [26]. Additional study outcomes included any all-cause 30-day readmission to the ED or hospital and costs, defined as total comprehensive direct medical costs from the perspective of a Medicaid payer (i.e., complete medical, ambulatory, inpatient, ED, procedure, pharmacy, home health, and other administrative claims).
Independent variables of interest assessed during the pre-index period included age, sex, race, residence (i.e., urban, micropolitan/rural), SCZ diagnosis type (i.e., paranoid, disorganized, catatonic, undifferentiated/simple, residual, other), SCD diagnosis, presence of mental health comorbidities [i.e., bipolar disorder, major depressive disorder, and post-traumatic stress disorder (PTSD)], Deyo–Charlson Comorbidity Index (D-CCI) [27], and the number of years since initial SCZ or SCD diagnosis. Clinical independent variables included the use of an OAP, pre-index ED or inpatient admission [28], pre-index total comprehensive direct medical costs [29], provider type (i.e., primary care/generalist, specialist physician including psychiatrist, nurse practitioner, physician assistant), and index year. Importantly, the analysis also included control for potential differences in post-index follow-up time (i.e., among members with eligibility and treatment extending beyond 12 months). As a predictor variable, a PDC ≥ 80% was used as a dichotomous marker for adherence, which is commonly used in real-world evidence research and has been validated in predicting hospital admissions associated with SCZ [30]. The presence of any 45-day treatment gap as a predictor variable was used as a dichotomous measure for persistence. Owing to inherent collinearity that is present between the measures (i.e., correlation between variables), the PDC ≥ 80% and presence of any 45-day treatment gap variables were incorporated into separate regression models for the outcomes of SCZ or SCD resource utilization (i.e., readmissions) and costs. A complete list of regression variables is presented in Supplementary Material Appendix S2.
Bivariable statistical comparisons between PP1M/PP3M and OAP-switch cohorts were conducted using independent-group t-tests or chi-squared tests, as appropriate. A multivariable, machine-learning least absolute shrinkage and selection operator (Lasso) regression was specified for the main inferential analysis, providing a validated and robust statistical framework to analyze high-dimensional models with numerous predictors [31,32,33,34]. In more detail, a cross-fit partialing-out Lasso was employed via a: (1) linear regression with a Napierian logarithmic-transformed outcome used for the continuous measure of PDC; (2) Poisson regression for the count number of 45-day gaps; (3) logistic regression for the presence of any 30-day readmission; and (4) linear regression for the Napierian logarithmic-transformed total direct comprehensive medical costs from the perspective of a Medicaid payer [29, 31,32,33,34,35]. All Lasso regressions were specified with Lasso penalty parameter optimization via a plugin iterative formula, repeat sample splitting ten times, tenfold within each split for cross-fitting, and Eicker–Huber–White heteroscedasticity-robust standard error estimation [31,32,33,34, 36,37,38]. The use of Napierian logarithms was warranted owing to the skewed nature of both PDC and cost outcomes, and was required to ensure minimum variance unbiased estimators (MVUE); these transformations were validated through extensive residual diagnostics [35]. Outcomes were reported as exponentiated beta estimates (exp(βestimate)) for PDC and costs, incidence rate ratios (IRR) for the number of 45-day treatment gaps, and odds ratios (OR) for readmissions based on linear, Poisson, or logistic regressions, respectively, with associated 95% confidence intervals (CIs) [29, 35]. Of note, the coefficient estimates obtained from log-transformed continuous outcomes may also be interpreted as semi-elasticities, and a log–log transformation of both continuous outcome and continuous predictor may be interpreted as a constant or full elasticity [35]. Given the potential for differences that may have occurred owing to interruptions in care associated with the coronavirus disease 2019 (COVID-19) pandemic, sensitivity analyses were also conducted to evaluate the index year of 2019; explicit control for this potential confounder was retained within all Lasso regression analyses, irrespective of this sensitivity analysis. All analyses were performed using SAS version 9.4 (Cary, NC) or Stata MP version 17.0 (College Station, TX).
Results
Descriptives
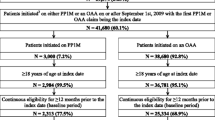
Overall, 295 Medicaid members met full inclusion criteria; 62.0% (n = 183) were in the PP1M/PP3M cohort and 38.0% (n = 112) in the OAP-switch cohort (Fig. 1). Twenty-four percent (44 of 183) of members who received PP1M transitioned to PP3M treatment during the post-index period. The average duration of post-index follow-up was 1.5 ± 0.8 years.
The average age across both cohorts was 39.7 ± 12.6 years; 48.1% of the population was female, and 22.7% was African American or Black (Table 1). The D-CCI had an overall mean and standard deviation of 1.13 ± 1.84. There were no significant differences observed in the proportions of SCZ or SCD members in the PP1M/PP3M versus OAP-switch cohorts (p ≥ 0.05). The OAP-switch cohort was generally older (42.0 ± 13.2 versus 38.4 ± 12.0 years), had a higher proportion of females (55.4% versus 44.8%), and had a higher proportion of white race (74.1% versus 61.8%) compared with the PP1M/PP3M cohort (p < 0.05 for all comparisons). In addition, OAP-switch members had higher D-CCI scores than the PP1M/PP3M cohort (1.5 ± 2.1 versus 0.9 ± 1.6, p < 0.01), though neither score was necessarily indicative of numerous other chronic conditions [27]. To illustrate, OAP-switch members had higher proportions of comorbid bipolar disorder (50.0% versus 35.0%) and comorbid PTSD (61.6% versus 42.1%) than the PP1M/PP3M cohort (p < 0.05). Concerning baseline OAP medication use, 28.0% were prescribed risperidone overall, while 22.3% were prescribed olanzapine. OAP-switch members were associated with a higher proportion of baseline quetiapine (23.2% versus 13.9%, p < 0.05) than the PP1M/PP3M cohort. An index year of 2017 was more common in the OAP-switch cohort than in the PP1M/PP3M cohort (49.1% versus 33.9%, p = 0.01).
Unadjusted results indicated that adherence was low irrespective of treatment cohort, with an average PDC of 66.7 ± 29.8 overall and some 48.5% reaching a PDC of 80% or greater (Table 2); no significant difference between cohorts was observed in unadjusted measures of adherence (p ≥ 0.05). Concerning persistence, OAP-switches had a higher proportion of unadjusted post-index 45-day treatment gaps compared with PP1M/PP3M members (24.1% versus 18.7%, p = 0.037). Of the members incurring a 45-day treatment gap, OAP-switches had a higher proportion of two or more gaps (9.0% versus 2.1%, p = 0.008). The OAP-switch cohort had higher unadjusted pre-index total direct medical costs relative to the PP1M/PP3M cohort ($31,634 ± 32,534 versus $16,125 ± 19,151, p < 0.001), although post-index costs were similar between groups ($52,963 ± 65,276 versus $48,998 ± 43,791, p = 0.440). Lastly, the OAP-switch cohort had a higher proportion of any 30-day post-index readmission compared with the PP1M/PP3M cohort (42.0% versus 33.3%, p = 0.042).
Multivariable, Machine-Learning Lasso Regression Analyses
The multivariable Lasso regression analysis for adherence, persistence, resource utilization, and cost outcomes explicitly controlled for potential differences across demographics, clinical characteristics, provider types, index years, total number of years since initial SCZ or SCD diagnosis, and duration of follow-up (Table 3). Concerning adherence outcomes, OAP-switches were significantly associated with a lower adjusted PDC and a higher adjusted incidence of 45-day treatment gaps relative to PP1M/PP3M. More specifically, an OAP-switch was associated with a 18.5% lower PDC measure [exp(βestimate) = 0.815, CI 0.678–0.979, p = 0.030] and a 92.3% higher number of 45-day treatment gaps (IRR 1.923, CI 1.234–2.299, p = 0.004). Irrespective of treatment cohort, the presence of a pre-index ED visit or inpatient admission was associated with 59.9% more 45-day treatment gaps compared with members without any pre-index visit or admission (IRR 1.599, CI 1.051–2.433, p = 0.028).
When controlling for a PDC ≥ 80% as a dichotomous measure of adherence in the multivariable analysis of SCZ or SCD resource utilization, OAP-switches were significantly associated with an 87.4% higher adjusted odds of any 30-day readmission relative to PP1M/PP3Ms (OR 1.874, CI 1.031–3.411, p = 0.030). Additionally, a PDC ≥ 80% was associated with a 65.9% lower adjusted odds of any 30-day post-index readmission (OR 0.341, CI 0.180–0.644, p = 0.001). When controlling for the presence of any 45-day treatment gap as a dichotomous measure of persistence, OAP-switches were associated with a 91.1% higher adjusted odds of any readmission (OR 1.911, CI 1.071–3.410, p = 0.028), whereas the presence of any 45-day treatment gap was associated with 2.717 times higher adjusted odds of any readmission overall (CI 1.407–5.247, p = 0.003), irrespective of treatment cohort. Across both regressions, a pre-index admission was a significant predictor of any 30-day readmission, with an adjusted odds ratio of 4.863 when controlling for PDC ≥ 80% (CI 4.641–8.958, p < 0.001) and 5.227 when controlling for the presence of any 45-day treatment gap as a predictor (CI 2.728–10.015, p < 0.001).
The multivariable analysis of total comprehensive direct medical costs indicated that OAP-switches were associated with an adjusted pre- to post-index change of approximately −49% relative to PP1M/PP3M (exp[βestimate, PDC≥80% as a predictor] = 0.511 and exp[βestimate,treatment gap as a predictor] = 0.501, p < 0.001) (Table 3). Overall, a 25.2% increase in adjusted post-index costs was associated with PDC ≥ 80% (exp[βestimate] = 1.252, CI 1.020–1.537, p = 0.032), whereas the presence of any 45-day treatment gap was not associated with a pre- versus post-index change in costs (exp[βestimate] = 1.072, CI −0.841 to 1.366, p = 0.576). For each 1% increase in pre-index costs, a significant 0.31% increase was observed in adjusted post-index costs (exp[βestimate, PDC ≥ 80% as a predictor] = 1.306 and exp[βestimate,treatment gap as a predictor] = 1.312, p < 0.001), reflecting a full or constant cost elasticity [29].
Comprehensively, across all multivariable analyses, sensitivity analyses surrounding COVID-19 era cases did not suggest that any differences were present (p ≥ 0.05). Again, via the Lasso regression analyses, the overall analysis retained explicit control for any potential changes that may have occurred.
Discussion
The current historical cohort analysis of Oklahoma Medicaid members assessed medication use patterns, resource utilization/readmissions, and total comprehensive direct medical costs among 295 members with SCZ or SCD who switched to a PP1M from a pre-index OAP or switched to a different OAP medication. Machine-learning, multivariable Lasso regression analyses indicated that Medicaid members who underwent an OAP-switch had significantly lower adjusted medication adherence (i.e., 18.5% lower PDC measure) and lower persistence (i.e., 92.3% higher number of 45-day treatment gaps) compared with those who initiated PP1M/PP3Ms (p < 0.05). The multivariable analysis also indicated that OAP-switches were associated with an 87.4% or 91.1% higher adjusted odds of any readmission controlling for PDC ≥ 80% or the presence of any 45-day treatment gap, respectively (p < 0.05). The multivariable-adjusted change in costs from pre- to post-index was approximately 49% lower for OAP-switch (p < 0.05), although the total overall unadjusted post-index costs did not differ between the PP1M/PP3M versus OAP-switch cohorts (p = 0.440). While treatment adherence defined by PDC ≥ 80% was associated with a 25.2% higher pre- to post-index change in adjusted costs (p = 0.032), fewer than half achieved a threshold of PCD ≥ 80% overall.
The current study builds on previous work in several important ways, with a key strength afforded by utilizing high-dimensional, machine-learning, multivariable statistical approaches to incorporate multiple predictors in a robust manner. Therein, Lasso regression analyses simultaneously controlled for numerous demographics, SCZ diagnosis types, providers, mental health comorbidities, clinical case mixes, longitudinal attributes, and health system characteristics, and included robust standard error estimations to ensure that potential violations required for statistical inference were mitigated. Lasso regression, overall, is a particularly useful machine-learning approach to estimate coefficients under conditions of small sample inference in the presence of numerous and extensive covariate control [39]. An additional strength of the current study is the uniqueness of Oklahoma Medicaid data, in that the program operates under a fee-for-service model to afford full transparency relative to several other Medicaid programs [40]. To illustrate, fee-for-service Medicaid programs do not generally operate under federal waivers, with Oklahoma’s program affording no mental health carve-outs [40].
Across previous studies using multi-state Medicaid populations to assess adherence, the proportion of members with a PDC ≥ 80% using PP1M has been reported to be significantly greater than comparator groups based upon multivariable analyses [19,20,21,22, 40]. Previous studies have also reported, via propensity score matching, that inpatient admissions were more frequent in cohorts that had lower PDC [19,20,21,22, 40]. In the current work, the bivariable analysis of both the continuous measure of PDC and dichotomous measure of PDC ≥ 80% versus < 80% (i.e., adherent versus nonadherent) was not observed to significantly differ between PP1M/PP3Ms and OAP-switches. However, in the multivariable Lasso regression analysis, OAP-switches were significantly and independently associated with an 18.5% lower PDC compared with PP1M/PP3M after controlling for other factors (p = 0.030). Whereas the current study’s inclusion criteria included Medicaid members with either SCZ or SCD, other research that compared PP1M/PP3Ms with OAPs have applied varying inclusion criteria. To illustrate, the comparator groups of Manjelievskaia et al. [40], Pesa et al. [20], Pilon et al. [21], and Xiao et al. [22] included Medicaid members with any use of OAP and were limited to an SCZ diagnosis alone, while Patel et al. [19] additionally required a hospitalization relapse following a medication’s index date. Prior investigations have also utilized data from multiple, and structurally different, Medicaid programs. Manjelievskaia et al. [40] used Truven MarketScan Medicaid Multi-State data to include 439 members with PP1Ms ranging from 18 to 35 years of age, Pesa et al. [20] used Medi-Cal data to include 1939 members with PP1Ms, Pilon et al. [21] used Medicaid healthcare claims data from New Jersey, Iowa, Mississippi, Missouri, and Kansas to include 1107 members with PP1Ms, and Xiao et al. [22] used New Jersey, Iowa, Missouri, and Kansas Medicaid data to include 952 members with PP1Ms.
The current work assessed both the number and presence of 45-day treatment gaps in therapy for members initiating PP1Ms after a pre-index OAP versus those switching to another OAP. Controlling for other factors, the number of 45-day treatment gaps was 92.3% higher in OAP-switches compared with PP1M/PP3Ms (p = 0.004). Two prior studies using multi-state Medicaid populations assessed various treatment gaps in patients with SCZ receiving an LAI or OAP [41, 42]. Marcus et al. [41] utilized Truven MarketScan Medicaid Multi-State data, including both first- and second-generation LAIs, and observed that LAIs were associated with a 55% lower adjusted odds of a 60-day treatment gap compared with OAPs (CI 0.34–0.60, p < 0.001). That study, which included 940 members using LAIs, also compared outcomes for paliperidone palmitate versus OAPs in a subgroup analysis, wherein paliperidone palmitate was associated with a 27% lower adjusted odds of rehospitalization (CI 0.54–0.99, p < 0.041) after controlling for several variables, including a 60-day treatment gap [41]. Pilon et al. [42] also compared second-generation LAIs to OAPs among 3307 Medicaid members from Iowa, Kansas, Missouri, and New Jersey. In a subgroup analysis of 2182, paliperidone palmitate was significantly associated with a higher persistence [i.e., a lack of 60-day therapy gaps (OR 1.53, p < 0.001)], with no significant differences in inpatient admissions, ED visits, or overall medical costs (p > 0.05) [42]. Of note, the current study also observed that a lower number of 45-day treatment gaps was significantly associated with PP1M/PP3Ms versus OAP-switches (p < 0.05).
With regard to acute care readmissions, Lafeuille et al. [43] analyzed the risk of any all-cause inpatient readmission or ED revisit in patients recently hospitalized for SCZ that received either PP1M or an OAP during their initial inpatient stay. The authors utilized hospital-level data from the Premier Perspective Comparative Hospital Database and included patients from multiple third-party payers, including Medicaid [43]. Using multivariable analysis, PP1Ms were associated with a 39% lower adjusted risk of all-cause readmission to a hospital or ED compared with OAPs (p < 0.001) [43]. Xiao et al. [44] compared adherence, inpatient admissions or ED visits), and costs across Medicaid members receiving PP1Ms or OAPs, reporting a significantly reduced risk of inpatient admission with PP1Ms (IRR 0.96, p < 0.01), coupled with a reduced risk of 30-day readmissions (OR 0.89, p < 0.05) and no significant difference in total healthcare costs (p > 0.05). Tidmore et al. [45] observed among 2532 Oklahoma Medicaid members that LAI initiation in those with SCZ and/or BP was associated with significantly higher adjusted odds of admissions and readmissions compared with those initiating OAPs, also involving higher overall adjusted costs (p < 0.023). Among those discharged from acute care settings, Tidmore et al. also reported that LAIs were subsequently associated with lower adjusted costs and shorter durations to psychiatry-related follow-up (p < 0.05) [45]. As previously stated, the current study observed that PP1M/PP3M use was associated with a lower adjusted odds of all-cause readmissions compared with OAP-switches, with an OAP-switch incurring an 87.4% higher adjusted odds after controlling for PDC ≥ 80% (p = 0.003) or a 91.1% higher odds when controlling for the presence of any 45-day treatment gap (p = 0.028). Multivariable analyses also indicated that any 45-day treatment gap was associated with 2.717 times higher adjusted odds of any readmission (p = 0.003), whereas a PDC ≥ 80% was associated with a 65.9% lower adjusted odds of readmission (p = 0.001), which, overall, may be suggestive of important clinical intervention points to mitigate SCZ or SCD resource utilization.
Bivariable analyses conducted by Patel et al. [19], Pesa et al. [20], Pilon et al. [21], and Xiao et al. [44] assessed differences in post-index total medical costs between PP1M and OAPs and reported no significant differences (p ≥ 0.05). Xiao et al. [22] employed marginal structural models, whereas both Manjelievskaia et al. [40] and Pilon et al. [42] utilized multivariable regression models and reported no significant differences in costs between groups (p ≥ 0.05). While the current study observed significantly lower unadjusted total medical costs in PP1M/PP3Ms compared with OAP-switches in both the pre-index ($16,125 ± 19,151 versus $31,634 ± 32,534, p < 0.001) and post-index periods ($46,998 ± 43,791 versus $52,962 ± 65,276, p < 0.05), the multivariable analysis of total costs indicated that OAP-switches were associated with an approximately 49% lower pre- to post-index change in costs relative to PP1M/PP3Ms (p < 0.001). Notably, in the current work, improved adherence (i.e., PDC ≥ 80%) was associated with a 25.2% increase in pre- versus post-index costs (p = 0.032) across the overall analysis and independent of treatment cohorts.
Certain limitations should be considered in interpreting the results of the current research endeavor. As with all nonrandomized observational studies, this work may have been subject to potential selection bias and residual confounding or confounding by indication, in part, owing to unmeasurable variables [29]. While proxies for case-mix severity and detailed disease categorization (e.g., SCZ type, year of initial SCZ or SCD diagnosis, comorbid mental health conditions) were included as covariates, no direct measure of disease severity is present within administrative claims (e.g., Positive and Negative Syndrome Scale) [46]. Additionally, measures of pre-index resource utilization and costs, demographics, provider types, and health system characteristics were included as potential predictors of outcomes. Without case notes and direct engagement of the provider and Medicaid member, the specific rationale or preferences surrounding medication switches at the clinical case level could not be measured, nor could the clinical appropriateness of treatment changes be assessed. The comprehensive economic burden surrounding SCZ and SCD includes substantial indirect costs [2], which could not be assessed. Owing to the separation of and inability to link full federal/national Medicare data and state-specific Medicaid data, this investigation summarily excluded persons above 64 years of age (i.e., “dual-eligibles”). The sequelae and natural history of SCD and SCZ remain complex, with interventions and resource utilization requiring consideration of advancing age [47,48,49]. Caution should be applied in extrapolating findings to other payers, patients, or other Medicaid programs.
Conclusion
This real-world multivariable investigation of adult Medicaid members with SCZ or SCD observed improved outcomes with PP1M/PP3Ms compared with OAP-switches. OAP-switches were also associated with poorer adjusted adherence, a greater adjusted number of treatment gaps, and a higher adjusted odds of any readmission. Medicaid members treated with PP1M/PP3M had significantly greater adherence and persistence and a lower odds of readmission relative to OAP-switches after controlling for numerous demographic, clinical, mental health, and provider characteristics. Although OAP-switches were associated with a lower change in adjusted pre- to post-index costs, the post-index total comprehensive direct medical costs did not differ between groups. Continued work should seek to assess and minimize poor adherence and persistence via targeted and supportive interventions in this vulnerable population.
References
Keepers GA, Fochtmann LJ, Anzia JM, et al. The American Psychiatric Association practice guideline for the treatment of patients with schizophrenia. Am J Psychiatry. 2020;177(9):868–72. https://doi.org/10.1176/appi.ajp.2020.177901.
Desai P, Lawson K, Barner J, Rascati K. Estimating the direct and indirect costs for community-dwelling patients with schizophrenia. J Pharm Health Serv Res. 2013;4:187–94. https://doi.org/10.1111/jphs.12027.
Wu EQ, Shi L, Birnbaum H, Hudson T, Kessler R. Annual prevalence of diagnosed schizophrenia in the USA: a claims data analysis approach. Psychol Med. 2006;36(11):1535–40. https://doi.org/10.1017/S0033291706008191.
Global Burden of Disease, 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–858. https://doi.org/10.1016/S0140-6736(18)32279-7.
Winklbaur B, Ebner N, Sachs G, Thau K, Fischer G. Substance abuse in patients with schizophrenia. Dialogues Clin Neurosci. 2006;8(1):37–43. https://doi.org/10.31887/DCNS.2006.8.1/bwinklbaur.
Lindenmayer JP, Kaur A. Antipsychotic management of schizoaffective disorder: a review. Drugs. 2016;76(5):589–604. https://doi.org/10.1007/s40265-016-0551-x.
Cloutier M, Aigbogun MS, Guerin A, et al. The economic burden of schizophrenia in the United States in 2013. J Clin Psychiatry. 2016;77(6):764–71. https://doi.org/10.4088/JCP.15m10278.
Marder SR, Cannon TD. Schizophrenia. N Engl J Med. 2019;381:1753–61. https://doi.org/10.1056/NEJMra1808803.
Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209–23. https://doi.org/10.1056/NEJMoa051688.
Scarff JR, Casey DA. Newer oral atypical antipsychotic agents: a review. Pharm Ther. 2011;36(12):832–8.
Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and risk factors for medication non-adherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63(10):892–909. https://doi.org/10.4088/jcp.v63n1007.
Kane JM, Kishimoto T, Correll CU. Non-adherence to medication in patients with psychotic disorders: epidemiology, contributing factors and management strategies. World Psychiatry. 2013;12(3):216–26. https://doi.org/10.1002/wps.20060.
Haddad PM, Brain C, Scott J. Nonadherence with antipsychotic medication in schizophrenia: challenges and management strategies. Patient Relat Outcome Meas. 2014;5:43–62. https://doi.org/10.2147/PROM.S42735.
Lin D, Thompson-Leduc P, Ghelerter I, et al. Real-world evidence of the clinical and economic impact of long-acting injectable versus oral antipsychotics among patients with schizophrenia in the United States: a systematic review and meta-analysis. CNS Drugs. 2021;35(5):469–81. https://doi.org/10.1007/s40263-021-00815-y.
Katona L, Bitter I, Czobor P. A meta-analysis of effectiveness of real-world studies of antipsychotics in schizophrenia: are the results consistent with the findings of randomized controlled trials? Transl Psychiatry. 2021;11(1):510. https://doi.org/10.1038/s41398-021-01636-9.
Invega Sustenna®. Janssen Pharmaceuticals, Inc.: Titusville, NJ; 2021. Internet: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/022264s023lbl.pdf Accessed: 22 Feb 2022.
Invega Trinza®. Janssen Pharmaceuticals, Inc.: Titusville, NJ; 2021. Internet: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/207946s009lbl.pdf Accessed: 22 Feb 2022.
Invega HafyeraTM. Janssen Pharmaceuticals, Inc.: Titusville, NJ; 2021. Internet: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/207946s010lbl.pdf Accessed: 22 Feb 2022.
Patel C, Emond B, Morrison L, et al. Risk of subsequent relapses and corresponding healthcare costs among recently-relapsed Medicaid patients with schizophrenia: a real-world retrospective cohort study. Curr Med Res Opin. 2021;37(4):665–74. https://doi.org/10.1080/03007995.2021.1882977.
Pesa JA, Doshi D, Wang L, Yuce H, Baser O. Health care resource utilization and costs of California Medicaid patients with schizophrenia treated with paliperidone palmitate once monthly or atypical oral antipsychotic treatment. Curr Med Res Opin. 2017;33(4):723–31. https://doi.org/10.1080/03007995.2016.1278202.
Pilon D, Muser E, Lefebvre P, Kamstra R, Emond B, Joshi K. Adherence, healthcare resource utilization and Medicaid spending associated with once-monthly paliperidone palmitate versus oral atypical antipsychotic treatment among adults recently diagnosed with schizophrenia. BMC Psychiatry. 2017;17(1):207. https://doi.org/10.1186/s12888-017-1358-3.
Xiao Y, Muser E, Lafeuille MH, et al. Impact of paliperidone palmitate versus oral atypical antipsychotics on healthcare outcomes in schizophrenia patients. J Comp Eff Res. 2015;4(6):579–92. https://doi.org/10.2217/cer.15.34.
ICD-9-CM: International Classification of Diseases, 9th Revision, Clinical Modification. National Center for Health Statistics, U.S. Department of Health & Human Services: Washington, D.C; 2021.
ICD-10-CM: International Classification of Diseases, 10th Revision, Clinical Modification. National Center for Health Statistics, U.S. Department of Health & Human Services: Washington, D.C; 2022.
Shafrin J, Bognar K, Everson K, Brauer M, Lakdawalla DN, Forma FM. Does knowledge of patient non-compliance change prescribing behavior in the real world? A claims-based analysis of patients with serious mental illness. Clinicoecon Outcomes Res. 2018;10:573–85. https://doi.org/10.2147/CEOR.S175877.
Loucks J, Zuckerman AD, Berni A, Saulles A, Thomas G, Alonzo A. Proportion of days covered as a measure of medication adherence. Am J Health Syst Pharm. 2021;12:zxa392. https://doi.org/10.1093/ajhp/zxab392.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9. https://doi.org/10.1016/0895-4356(92)90133-8.
Donisi V, Tedeschi F, Wahlbeck K, Haaramo P, Amaddeo F. Pre-discharge factors predicting readmissions of psychiatric patients: a systematic review of the literature. BMC Psychiatry. 2016;16(1):449. https://doi.org/10.1186/s12888-016-1114-0.
Skrepnek GH, Olvey EL, Sahai A. Econometric approaches in evaluating costs and outcomes within pharmacoeconomic analyses. Pharm Policy Law. 2012;14(1):105–22. https://doi.org/10.3233/PPL-2011-0345.
Karve S, Cleves MA, Helm M, Hudson TJ, West DS, Martin BC. Good and poor adherence: optimal cut-point for adherence measures using administrative claims data. Curr Med Res Opin. 2009;25(9):2303–10. https://doi.org/10.1185/03007990903126833.
Belloni A, Chernozhukov V, Hansen CB. High-dimensional methods and inference on structural and treatment effects. J Econ Perspect. 2014;28:29–50. https://doi.org/10.1257/jep.28.2.29.
Belloni A, Chernozhukov V, Wei Y. Post-selection inference for generalized linear models with many controls. J Bus Econ Stat. 2016;34:606–19. https://doi.org/10.1080/07350015.2016.1166116.
Chernozhukov V, Chetverikov D, Demirer M, Duflo E, Hansen CB, Newey WK, Robins JM. Double/debiased machine learning for treatment and structural parameters. Econometrics J. 2018;21:C1-68. https://doi.org/10.1111/ectj.12097.
Chernozhukov V, Hansen CB, Spindler M. Post-selection and post-regularization inference in linear models with many controls and instruments. Am Econ Rev. 2015;105:486–90. https://doi.org/10.1257/aer.p20151022.
Skrepnek GH. Regression methods in the empirical analysis of health care data. J Manag Care Pharm. 2005;11(3):240–51. https://doi.org/10.18553/jmcp.2005.11.3.240.
Huber PJ. The behavior of maximum likelihood estimates under nonstandard conditions. In: Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability 1967;1:221–33
White H. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:817–38. https://doi.org/10.2307/1912934.
Eicker F. Limit theorems for regression with unequal and dependent errors. In: Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability. 1967;5:59–82
Hastie T, Tibshirani R, Wainwright M. Statistical learning with sparsity: the Lasso and generalizations. New York: CRC Press; 2015. https://doi.org/10.1201/b18401.
Manjelievskaia J, Amos TB, El Khoury AC, Vlahiotis A, Cole A, Juneau P. A comparison of treatment patterns, healthcare resource utilization, and costs among young adult Medicaid beneficiaries with schizophrenia treated with paliperidone palmitate or oral atypical antipsychotics in the US. J Med Econ. 2018;21(12):1221–9. https://doi.org/10.1080/13696998.2018.1527608.
Marcus SC, Zummo J, Pettit AR, Stoddard J, Doshi JA. Antipsychotic adherence and re-hospitalization in schizophrenia patients receiving oral versus long-acting injectable antipsychotics following hospital discharge. J Manag Care Spec Pharm. 2015;21(9):754–68. https://doi.org/10.18553/jmcp.2015.21.9.754.
Pilon D, Tandon N, Lafeuille MH, et al. Treatment patterns, health care resource utilization, and spending in Medicaid beneficiaries initiating second-generation long-acting injectable agents versus oral atypical antipsychotics. Clin Ther. 2017;39(10):1972-85.e2. https://doi.org/10.1016/j.clinthera.2017.08.008.
Lafeuille MH, Grittner AM, Fortier J, et al. Comparison of re-hospitalization rates and associated costs among patients with schizophrenia receiving paliperidone palmitate or oral antipsychotics. J Am Soc Health-Syst Pharm. 2015;72(5):378–89. https://doi.org/10.2146/ajhp140219.
Xiao Y, Muser E, Fu DJ, et al. Comparison of Medicaid spending in schizoaffective patients treated with once monthly paliperidone palmitate or oral atypical antipsychotics. Curr Med Res Opin. 2016;32(4):759–69. https://doi.org/10.1185/03007995.2016.1140634.
Tidmore LM, Keast SL, Waters HC, Pareja KL, Cothran T, Skrepnek GH. Readmissions, costs, and duration to subsequent outpatient visit after hospital discharge among Medicaid beneficiaries utilizing oral versus long-acting injectable antipsychotics in bipolar disorder or schizophrenia. Curr Med Res Opin. 2022;38(9):1621–30. https://doi.org/10.1080/03007995.2022.2101819.
Kay SR, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–76. https://doi.org/10.1093/schbul/13.2.261.
Freudenreich O. Natural history of schizophrenia. In: Psychotic disorders. Current clinical psychiatry. 2nd ed. Cham: Humana Press; 2020. https://doi.org/10.1007/978-3-030-29450-2_7.
Jeste DV, Maglione JE. Treating older adults with schizophrenia: challenges and opportunities. Schizophr Bull. 2013;39(5):966–8. https://doi.org/10.1093/schbul/sbt043.
Bartels SJ, Fortuna KL, Naslund JA. Serious mental disorders in older adults: schizophrenia and other late-life psychoses. In: Segal DL, Qualls SH, Smyer MA, editors. Aging and Mental Health. 3rd ed. Hoboken: Wiley Blackwell; 2018. p. 1–14. https://doi.org/10.1002/9781119133186.ch1051.
Centers for Medicare and Medicaid Services (CMS) Cell Suppression Policy. US Department of Health & Human Services: Washington, D.C.; 2022. https://www.hhs.gov/guidance/document/cms-cell-suppression-policy. Accessed 21 Sept 2022.
Acknowledgements
Funding
This research and the Journal’s Rapid Service and Open Access fees were funded by an unrestricted research award from Janssen Scientific Affairs, LLC to the University of Oklahoma Health Sciences Center. Also through the University of Oklahoma Health Sciences Center, Drs. Dickson, Nguyen, and Skrepnek were engaged in contractual work for the Oklahoma Health Care Authority. Dr. Skrepnek reports unrelated research grants from Pfizer Inc. and Otsuka Pharmaceuticals through the University of Oklahoma Health Sciences Center.
Medical Writing and Editorial Assistance
Manuscript writing support, funded by Janssen Scientific Affairs, LLC, was provided by Crystal Murcia, PhD of Inkwell Medical Communications LLC.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Conceptualization: Grant Skrepnek, Matthew Dickson, Michael Nguyen, Terry Cothran; Methodology: Grant Skrepnek, Matthew Dickson, Michael Nguyen, Charmi Patel, Shannon Grabich, Carmela Benson, Terry Cothran; Formal analysis and investigation: Grant Skrepnek, Matthew Dickson, Michael Nguyen, Charmi Patel, Shannon Grabich, Carmela Benson; Writing - original draft preparation: Matthew Dickson, Michael Nguyen, Charmi Patel, Shannon Grabich, Carmela Benson, Grant Skrepnek; Writing - review and editing: Grant Skrepnek, Matthew Dickson, Michael Nguyen, Charmi Patel, Shannon Grabich, Carmela Benson, Terry Cothran; Funding acquisition: Grant Skrepnek, Terry Cothran; Resources: Grant Skrepnek, Terry Cothran; Supervision: Grant Skrepnek.
Prior Presentations
Research abstracts based on this work were presented at the Academy of Managed Care Nexus 2021 on October 18-21, 2021, in Denver, CO, and at the US Psych Congress on October 29-November 1, 2021 in San Antonio, TX.
Disclosures
Matthew Dickson and Michael Nguyen have received unrelated research funding through the University of Oklahoma Health Sciences Center from Pfizer. Charmi Patel and Carmela Benson are employees of Janssen Scientific Affairs, LLC, and stockholders of Johnson & Johnson, Inc. Shannon Grabich was an employee of Xcenda, LLC at the onset of the investigation and is now an employee of Sarepta Therapeutics. Terry Cothran was an employee of the University of Oklahoma Health Science Center at the onset of the investigation, and is currently Director of Pharmacy at the Oklahoma Health Care Authority. Grant Skrepnek has received unrelated research funding through the University of Oklahoma Health Sciences Center from Pfizer and Otsuka.
Compliance with Ethics Guidelines
This study was defined as exempt by the Office of Human Research Participant Protection (Institutional Review Board #12942) at the University of Oklahoma Health Sciences Center.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Dickson, M.C., Nguyen, M.M., Patel, C. et al. Adherence, Persistence, Readmissions, and Costs in Medicaid Members with Schizophrenia or Schizoaffective Disorder Initiating Paliperidone Palmitate Versus Switching Oral Antipsychotics: A Real-World Retrospective Investigation. Adv Ther 40, 349–366 (2023). https://doi.org/10.1007/s12325-022-02354-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02354-4