Abstract
Introduction
The 2019 European Society of Cardiology and European Atherosclerosis Society (2019 ESC/EAS) guidelines stress the importance of managing low-density lipoprotein cholesterol (LDL-C) after myocardial infarction (MI) to reduce the risk of cardiovascular events. Information on guideline implementation is limited. The aim of this survey was to describe current clinical practice regarding LDL-C management in the first year post-MI across Europe, improving understanding of the role of ESC/EAS guidelines on clinical practice.
Methods
A qualitative web-based cross-sectional physician survey about the patient pathway and LDL-C management post-MI was conducted in 360 physicians from France, Italy, Germany, The Netherlands, Spain, and the UK (n = 60/country) between December 2019 and June 2020. Secondary and primary care physicians (SCPs/PCPs) described their experiences treating patients post-MI over the preceding 2 months.
Results
Physicians reported that on average 90.7% of patients not prescribed lipid-lowering therapy (LLT) before an MI initiated LLT as inpatients; for patients already taking LLT, treatment was intensified for 64.7% of inpatients post-MI. SCPs reported prescribing higher-intensity statins and/or ezetimibe for between 72.3% (Italy) and 88.6% (UK) of patients post-MI. More than 80.0% of SCPs and 51.2% of PCPs stated that they would initiate a change in LLT immediately if patients did not achieve their LDL-C treatment goal by 12 weeks post-MI; 82.0% of SCPs and 55.1% of PCPs reported referring to 2019 ESC/EAS guidelines for management of patients post-MI. Barriers to initiating PCSK9 inhibitors (PCSK9is) included prior prescription of a maximally tolerated dose of statin (49.4%) and/or ezetimibe (38.9%), requirement to reach threshold LDL-C levels (44.9%), and pre-authorization requirements (30.4%).
Conclusion
Differences in clinical practice post-MI were reported across the countries surveyed, including divergence between 2019 ESC/EAS and local guidelines. Increased use of innovative medicines to achieve LDL-C goals should reduce risk of subsequent cardiovascular events in very high-risk patients post-MI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The 2019 ESC/EAS guidelines define LDL-C treatment goals for patients regarded as at very high risk for cardiovascular events. |
Studies of how 2019 ESC/EAS guidelines impact lipid management practices in primary and secondary care for post-MI patients across Europe are limited. |
Findings from this physicians' survey indicate that lipid management practices as well as the extent to which primary and secondary care physicians follow the 2019 ESC/EAS guidelines during the first year after an MI differ across Europe. |
Clinical practice and 2019 ESC/EAS guidelines were reported to diverge in the areas of time to lipid measurement, LDL-C treatment goal, and treatment escalation. |
Reasons for following the 2019 ESC/EAS guidelines included differing national/regional guidelines, differing target LDL-C levels, and prescribing restrictions, highlighting that further effort is required to intensify management of lipids post-MI to improve patient cardiovascular outcomes across Europe. |
Introduction
Cardiovascular disease (CVD) remains the leading cause of mortality and a major cause of morbidity, causing 45% of all deaths in Europe [1], although mortality rates in patients with acute coronary syndrome have declined in recent years because of a greater use of early reperfusion therapy, primary percutaneous coronary intervention, modern antithrombotic therapy, and implementation of secondary prevention [2].
One of the key causal modifiable factors for atherosclerotic cardiovascular disease (ASCVD) and severe cardiovascular events, such as myocardial infarction (MI), is elevated low-density lipoprotein cholesterol (LDL-C) [3]. Currently, statins are recommended in all patients with MI, irrespective of cholesterol concentration at presentation [4]. High-intensity LLT should be started in these patients as early as possible as this is associated with early and sustained clinical benefits [5,6,7].
For post-MI patients, 2019 European Society of Cardiology and European Atherosclerosis Society (ESC/EAS) guidelines recommend targeting LDL-C levels below 1.4 mmol/l (55 mg/dl) and at least a 50% reduction from baseline [8]. A lower treatment goal of < 1.0 mmol/l (< 40 mg/dl) should be considered for patients who have a second vascular event within 2 years [5]. Guidelines recommend that very high-risk patients who do not achieve the recommended treatment goals, despite maximally tolerated statin therapy, should be prescribed supplemental LLT, such as ezetimibe or proprotein convertase subtilisin/kexin type 9 inhibitors (PCSK9i) [5, 9]. PCSK9is are capable of further reducing plasma LDL-C by 55–70% when used in combination with statins with or without ezetimibe [1]. PCSK9i use is associated with improved cardiovascular (CV) outcomes and a good safety profile [9, 10]. A meta-analysis of 26 randomized clinical trials including almost 170,000 participants has shown that lowering serum LDL-C level is associated with decreased risk of CV events [11]. While ESC/EAS guidelines recognize that total CV risk reduction should be individualized, they point out that having treatment goals may facilitate adherence to therapy as well as patient-physician communication. The guidelines further indicate that lowering LDL-C beyond the set goals may be associated with even lower risk of CV events [8].
In clinical practice, LDL-C management remains suboptimal, and target LDL-C levels in post-MI patients often remain above the treatment goals recommended by the 2019 ESC/EAS guidelines, despite treatment with statins and/or ezetimibe [8, 12]. According to the EUROASPIRE V survey (27 countries), 80% of patients who had experienced acute coronary symptoms or who required revascularization or coronary artery bypass surgery were on statins but 71% had LDL-C ≥ 1.8 mmol/l (≥ 70 mg/dl), the 2016 ESC/EAS guideline treatment goal applicable when EUROASPIRE V was conducted [12]. The DA VINCI study (18 European countries) identified that among patients with established ASCVD, the 2019 ESC/EAS guideline treatment goal for very high-risk patients (LDL-C < 1.4 mmol/l) was achieved by 18% of patients, and this proportion increased to 22% for those patients receiving high-intensity statins or to 37% for those receiving ezetimibe in combination with a statin therapy [13].
A structured literature review of lipid management across Europe in the real-world setting reviewed 53 real-world observational studies in high- or very-high-risk patients and observed that statins were the most common LLT. Patients without familial hypercholesterolemia (FH) mostly received high- or moderate-intensity LLT. Patients with FH mostly received high-intensity LLT. In patients without FH, the proportion of patients receiving ezetimibe was low overall (1–22%), and use of PCSK9i therapy was limited as well. LDL-C goal attainment was suboptimal irrespective of LLT [14].
This cross-sectional survey of primary (PCPs) and secondary care physicians (SCPs) aimed to understand the patient pathway and treatment patterns during the first year post-MI across the six countries surveyed: France, Germany, Italy, The Netherlands, Spain, and the UK. The primary objective of this survey was to understand the proportion of primary and secondary care physicians who review or make changes to LLT in post-MI patients. Secondary objectives were to determine how practice varied by country or healthcare setting, characterizing LLT patterns, improving understanding of lipid management practices and post-MI patient care. Practices were compared with recommendations from the 2019 ESC/EAS guidelines for management of dyslipidemias. The findings from this survey are based on the opinions of surveyed physicians, and the data presented are qualitative in nature.
Methods
Study Objectives
The primary objectives were to understand the proportion of primary and secondary care physicians who reviewed or made changes to LLT post-MI in the scope European countries.
Secondary objectives were to determine how practice varied by country or healthcare setting, identifying where post-MI patients are discharged, estimating rates of LLT review for patients not achieving LDL-C goals, and characterizing treatment patterns in post-MI patients. Practices were compared with recommendations from the 2019 ESC/EAS guidelines.
Study Design
The study was a qualitative cross-sectional survey of primary and secondary care physicians involved in the management of post-MI patients in six countries (France, Germany, Italy, The Netherlands, Spain, the UK) carried out from December 2019 to June 2020. A stratified sample of 60 physicians was surveyed in each country. The number of primary and secondary care physicians varied across countries to reflect their role in management of post-MI patients during the first year after the event in each country (Table 1). A review of literature, local guidelines, and country-specific guidelines was conducted to define the survey questions. Data were then collected using a structured web-based survey developed using Streiner and Norman methods [15]. A screener questionnaire was used to select physicians who satisfied the inclusion and exclusion criteria for the survey.
The main body of the questionnaire related to various aspects of LDL-C management with some questions specific to one of the physician types. Two case studies featuring fictitious patients at very high risk of CV events were presented: patient A (a 55-year-old female presenting with a first MI, non-smoker, LDL-C = 250 mg/dl, not taking LLT) and patient B (a 67-year-old male, presenting with MI and recent history of previous MI, recently quit smoking, LDL-C = 100 mg/dl, currently on atorvastatin 80 mg). The case studies contained a series of questions to collect information on LLT decisions.
The study was approved by the research ethics committee of the University of Technology, Sydney, Australia, on 7 November 2019 (application no. PRMA4149_2019 UTS HREC ref no. ETH18-2910). This study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments. All participants provided informed consent to participate in the study.
Study Population and Inclusion Criteria
Primary and secondary care physicians from each of the scope countries were surveyed. To be eligible for the survey, the respondents could be:
-
SCPs: hospital-based cardiologists or (Germany only) cardiac rehabilitation specialists (working in a rehabilitation center for ≥ 20% of their time), practicing for at least 2 years since completion of specialty training, who had managed at least 20 patients admitted as a hospital inpatient with an MI in the previous 2 months
-
PCPs: general practitioners or office-based cardiologists, practicing for at least 2 years, who had been involved in the care of at least four patients with an MI in the previous year.
Data Collection
For the pilot phase, five respondents for the UK and three in each of the other countries were recruited (20 in total), and these responses were not included in the main dataset. For the main phase, a total of 360 respondents (60 respondents in each of the scope countries) were recruited stratified by specialty. This sample size was calculated at the design stage to be sufficient to address the study objectives with acceptable precision. The questionnaire was translated into local languages with two-step verification; participants completed their responses in their native language. Responses were obtained using a structured questionnaire, administered between December 2019 and June 2020. Descriptive analyses of the main phase data were conducted overall (for the primary endpoints) and for each country individually.
Data Validation and Statistical Analyses
The study was descriptive. The questionnaire included closed questions whenever possible permitting respondents to answer only within a pre-specified range of options. Questions with continuous numerical values had a wide permitted range to ensure that all logical options were available to the respondents. Values were immediately checked for plausibility by the software; the responder was notified if their response was outside the plausible range and asked to provide a plausible value. The respondents were not asked to consult medical records when completing the questionnaire but where appropriate were prompted to limit responses to patients seen over the preceding 2 months. For missing survey data, no imputation of the data was attempted; statistics were calculated omitting those data.
Continuous variables were summarized using the mean and standard deviation as well as the median and interquartile range to understand the distribution of results. For categorical variables, the number and percentage of respondents were calculated for each category. For the primary analyses, the data were analyzed collectively across all countries. Findings for each scope country were analyzed and reported separately. Results were summarized by clinician type and were reported separately for PCPs and SCPs. Data were analyzed using SAS® (version 9.4, SAS Institute, Cary, NC, USA).
Results
Respondent Characteristics
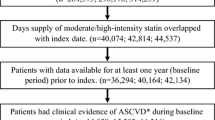
Of 360 physicians surveyed, 233 (64.7%) were SCPs (cardiologists) and 127 (35.3%) were PCPs (general practitioners or office-based cardiologists). Most physicians surveyed had practiced for > 10 years, and the majority worked in teaching hospitals or urban practices. Respondent characteristics are summarized in Table 1.
Lipid Management in Primary and Secondary Care Settings Post-MI
Prescription of LLTs Post-MI in Secondary Care
Secondary care physicians reported that on average across the six participating countries 90.7% of patients who were not on LLT prior to having an MI did have LLT initiated during their hospital stay. This proportion ranged from 87.5% in Spain to 96.4% in The Netherlands (Fig. 1a). Only 64.7% of patients who were on LLT prior to having an MI, had their LLT intensified after the event. Among the surveyed countries that proportion was lowest in The Netherlands (46.5%) and highest in Italy (73.4%; Fig. 1b).
Secondary care physician reported rates of LLT prescribing during inpatient stay post-MI including (a) LLT initiation for patients not taking LLT at admission and (b) LLT intensification for patients taking LLT at admission. LLT lipid-lowering therapy, MI myocardial infarction, SCP secondary care physician
Cardiac Rehabilitation Post-MI
Physicians reported that between 38.3% (Italy) and 84.0% (The Netherlands) of patients were referred to cardiac rehabilitation after an MI (Fig. 2). Ten percent of Spanish physicians and 15.6% of Italian doctors reported not having access to cardiac rehabilitation programs, but overall, physicians across all countries surveyed reported having access to cardiac rehabilitation programs without restrictions. In Italy, it was reported that 78.9% of patients attending cardiac rehabilitation first attend directly after discharge from secondary care following their MI. Across the other surveyed countries patients were reported to start their rehabilitation programs on average between 2.0 and 5.8 weeks after discharge from the hospital.
LDL-C Management Post-MI
Secondary care: SCPs reported an average time from hospital discharge post-MI until LLT review ranging from 6.2 weeks in Italy to 10.5 weeks in the UK (Fig. 3). The proportion of patients that SCPs reported underwent LLT review in the first 12 weeks post discharge following an MI ranged from 48.0% in the UK to 77.4% in The Netherlands (Fig. 4).
Primary care: Following discharge from secondary outpatient to primary care, PCPs reported that they requested assessment of LDL-C levels for between 58.8% (UK) and 69.0% (France) of post-MI patients at their first consultation following the discharge. PCPs reported that they review LLT in the first consultation for between 46.4% (Italy) and 69.9% (Germany) of post-MI patients (Fig. 4). Between 8.3% (The Netherlands) and 36.7% (France) of PCPs reported requesting assessment of LDL-C levels for all post-MI patients at first consultation after the patients were transferred to their care.
Treatment Decisions Reported by Physicians for Patients Who Did Not Achieve LDL-C Treatment Goals
More than 80.0% of SCPs in each of the participating countries stated that they would initiate a change in LLT immediately if patients did not achieve their LDL-C treatment goal by 12 weeks after an MI, with < 20% reporting that they would delay action. In the UK, 10.0% of SCPs reported that they would not take further action to change LLT if LDL-C levels were above the treatment goal (Fig. 5a).
Among PCPs, an average of 51.2% stated that they would initiate a change in LLT immediately if patients did not achieve their LDL-C treatment goal by 12 weeks post-MI, ranging from 30.0% in France to 80.0% in Spain. Germany was the only country where 2.6% of PCPs reported that they would take no action in this situation. From 20.0% (Spain) to 70.0% (France) of PCPs reported that they would wait before changing LLT in these patients (Fig. 5). Treatment decisions reported by physicians for patients who did not achieve LDL-C treatment goals
LDL-C Level Treatment Goals
The majority of SCPs from Spain (72.0%), Germany (70.0%), France (66.7%), and Italy (57.8%) reported using treatment goals recommended by the 2019 ESC/EAS guidelines for very high-risk patients (1.4 mmol/l and at least 50% from the baseline level). In The Netherlands and the UK, more physicians reported that they targeted an LDL-C level of < 1.8 mmol/l or at least a 50% reduction of the baseline LDL-C level (the LDL-C treatment goals recommended by 2016 ESC/EAS guidelines; Fig. 6a).
Physician-reported LDL-C levels considered most appropriate for post-MI patients. aOther includes: at least 50% reduction of LDL-C level, LDL-C < 100 mg/dl (2.6 mmol/l) or at least 50% reduction of LDL-C level; LDL-C < 130 mg/dl (3.3 mmol/l) or at least 50% reduction of LDL-C level; at least 50% reduction in LDL-C from the level before treatment; LDL-C level as low as possible with the most intensive lipid-lowering therapy regimen; 40% reduction in non-HDL from the level before treatment; other. HDL high-density lipoprotein, LDL-C low-density lipoprotein cholesterol, MI myocardial infarction
Up to 40.0% of those surveyed in Germany and Spain reported using the treatment goals to reduce LDL-C to < 1.4 mmol/l and by \(\le \) 50% from the baseline level. In France, Germany, Italy, The Netherlands, and Spain, most PCPs reported that they targeted an LDL-C of 1.8 mmol/l or ≤ 50% reduction of the baseline LDL-C level. Three-quarters of UK PCPs reported a range of other treatment goals including 15% who reported targeting the lower threshold of 1.0 mmol/l associated with multiple cardiac events (Fig. 6b).
The most common way of intensifying LLT post-MI reported by SCPs was increasing statin intensity and/or addition of ezetimibe. This modification was reported to be suitable for between 72.3% (Italy) and 88.6% (UK) of post-MI patients. Use of PCSK9i, with or without additional modification of the LLT regimen, was reported to be appropriate for between 9.8% of patients in the UK and 23.8% of patients in Italy (Fig. 7). When asked what guidelines are used in their day-to-day practice, 82.0% of SCPs across the scope countries stated that they refer to 2019 ESC/EAS guidelines for management of post-MI patients. Among PCPs, this proportion was 55.1%. Similarly, 55.1% of PCPs reported that they consulted national guidelines.
Secondary care physician-reported proportion of patients who receive each treatment option during treatment intensification. aThis category represents the combined values reported for the following therapeutic regimen modifications: increase statin intensity and add PCSK9i, decrease statin intensity and add PCSK9i; add ezetimibe and PCSK9i; increase statin intensity with addition of ezetimibe and PCSK9i; reduce statin intensity with addition of ezetimibe and PCSK9i
Prescribing Decisions Made by Physicians Reviewing Very High-Risk Fictitious Case Studies
To evaluate their LDL-C treatment practices, the physicians were presented with two hypothetical case studies of very high-risk fictitious patients. Case study A described a 55-year-old woman who was presenting with her first MI, was a non-smoker, had an LDL-C level of 250 mg/dl, and had not been prescribed LLT. Case study B described a 67-year-old man presenting with an MI and previous history of MI 7 months ago, who had recently quit smoking, had an LDL-C level of 100 mg/dl, and had been prescribed atorvastatin 80 mg. Both fictitious cases were designed such that it was not possible to achieve LDL-C treatment goals recommended by the 2019 ESC/EAS guidelines by a combination of a high-intensity statin and ezetimibe. In both these situations, the current guidelines recommend adding a PCSK9i.
For case study A, between 46.7% (Spain) and 76.7% (France) of physicians (SCP and PCP) reported that they would initiate a statin for this patient. The proportion of physicians who selected LLT regimens including PCSK9is ranged from 5.0% in France to 11.7% in the UK. For case study B, across the countries surveyed, between 41.7% (The Netherlands) and 73.3% (Germany) chose to add ezetimibe. The proportion of physicians who selected LLT regimens including PCSK9i ranged from 5.0% in Germany to 25.1% in the UK.
Barriers to PCSK9i Use
Among the main barriers to prescribing a PCSK9i identified by the physicians surveyed were the requirements for a minimum LDL-C threshold before PCSK9i treatment can be prescribed (44.9%), the requirement for patients to already be on the maximally tolerated statin dose (49.4%) or ezetimibe (38.9%), and a requirement for the patient to be pre-authorized for the PCSK9i therapy (30.4%) (country-specific data are provided in Table 2). Physicians were asked whether PCSK9is were included on their formulary. For all participating countries, 68.6% of physicians reported that PCSK9is were included on their formulary and 31.4% reported that they were not included. This proportion varied substantially by the physician’s specialty. Among SCPs, 84.1% reported that PCSK9i were included in their formulary, while this proportion among PCPs was only 40.2%. The largest differences in availability between primary and secondary care were observed in Spain, The Netherlands, and the UK. The main barriers to achieving LDL-C treatment goals more generally identified by prescribers were adverse events of LLTs, poor adherence, and lack of patient education about LDL-C, lifestyle, and diet changes (Table 2).
Discussion
This study showed that there are differences across the European countries surveyed in the management of dyslipidemia and the proportion of physicians who review or make changes to LLT in post-MI patients. This can be attributed in part to differing patient pathways and healthcare systems. However, adherence to local guidelines, differences in formulary-based restrictions, and varying interpretations of the treatment goals post-MI contribute to some of the differences being reported in practice.
The 2019 ESC/EAS guidelines recommend: (1) high-intensity statin use to the highest tolerated dose required to achieve lipid level goals; (2) addition of ezetimibe for people not achieving treatment goals; (3) combination with PCSK9i for primary and secondary prevention in patients who are at very high risk for CV events and who are not achieving their treatment goal on existing treatment regimens [5]. While LLT is initiated in most patients who did not have any LLT prior to their MI, lower rates of intervention are seen in those patients who were on LLT before their event. From 26.6% (Italy) to 45.5% (Germany) of patients who were on LLT prior to their MI did not have their LLT regimen intensified after the event. Although this proportion may include some patients already at goal LDL-C, EUROASPIRE V and DA VINCI studies have found that the majority of ASCVD patients in Europe have LDL-C levels higher than those recommended by the ESC/EAS guidelines [13, 16]. There is potential for improvement in how 2019 ESC/EAS guidelines are implemented with respect to LLT intensification and use of the full spectrum of prescribing options to achieve target LDL-C levels in post-MI patients.
Physician-estimated referral rates of post-MI patients to cardiac rehabilitation varied widely across the six countries surveyed (from 38.3% in Italy to 84.0% in The Netherlands). The process surrounding discharge to primary care or to a cardiac rehabilitation program is often unclear, and the management protocols for post-MI follow-up are not clearly defined [17,18,19]. The low levels of referral to cardiac rehabilitation reported for some countries may reflect that not all post-MI patients are considered for rehabilitation in every country, with selection for rehabilitation reflecting the severity or type of the MI (ST-elevation vs. non-ST-elevation MIs). Higher levels of referral to cardiac rehabilitation in the UK may reflect that this is a quality standard for secondary prevention after an MI, against which primary care organizations can be assessed. In some countries, such as France, guidelines are available that cover the care pathway from admission to rehabilitation, but implementation is often variable [20]. This means that the opportunity to optimize LDL-C management may often be missed. Improved care transition between clinicians and physicians involved in early outpatient follow-up post-MI is required.
In primary care, few physicians reported reviewing LLT or requesting LDL-C level checks on the first consultation post-MI. Following discharge, many patients do not have their LLT reviewed by SCPs within 12 weeks post-MI (up to 52.0% of patients in the UK, Fig. 4). This variation may be in part due to differences in healthcare systems across the surveyed countries. In Spain, most post-MI patients remain in the care of SCPs for > 12 weeks following discharge. In The Netherlands, SCPs care for the patient for 1 year post-MI, and PCPs do not see these patients during that period. In France, both SCPs and PCPs manage post-MI patients. In the UK, NICE guidelines for secondary prevention recommend that physicians measure lipids at admission and at 3 months after the start of high-intensity statin treatment. Physicians in the UK often refer to the NICE guidelines and review the LLT at 3 months and not at 12 weeks as it is recommended by the ESC/EAS guidelines. Further country-specific observations include that Spanish physicians more commonly reported targeting LDL-C levels recommended by 2019 ESC/EAS guidelines and demonstrated proactive LLT management overall. Physicians across the countries surveyed cited adverse events, poor adherence, and lack of patient education about LDL-C as barriers to achieving LDL-C treatment goals. Recent studies have indicated that the true frequency of adverse events caused by LLT may be lower than that reported because of the perception that this drug class is associated with adverse events [21].
The reported target LDL-C treatment goal varied substantially by country and physicians’ specialty and often diverged from the treatment goal recommended by 2019 ESC/EAS guidelines [8]. Not surprisingly, the proportion of physicians who were targeting the LDL-C treatment goal recommended by the current guidelines was higher among SCPs as they were specialist cardiologists. But even among SCPs the variation across countries was apparent: while > 57% of SCPs in Germany, Spain, France, and Italy targeted the LDL-C treatment goal recommended by 2019 ESC/EAS guidelines in their practice, only 10.4% of Dutch and 27.5% of UK SCPs targeted this goal. The proportions of PCPs who targeted the LDL-C goals recommended by the most recent guidelines were much lower and never exceeded 40.0% (reported in Germany and Spain). Substantial proportions of physicians, both SCPs and PCPs, were still targeting the LDL-C treatment goals recommended by 2016 ESC/EAS guidelines, which were outdated at the time of the survey. It is worth noting, however, that the 2019 guidelines had come out only a few months before the survey began, and many physicians probably did not have sufficient time to adopt them in their practice. Another reason for the variability observed may be that in some countries the physicians refer to local guidelines, which are not always harmonized with the most recent ESC/EAS guidelines.
SCPs in each of the surveyed countries reported that the appropriate way to intensify LLT in more than half of their post-MI patients who have not reached LDL-C treatment goals was to increase statin intensity with or without addition of ezetimibe. This is aligned with the recommendations of the 2019 ESC/EAS guidelines. However, the guidelines make further recommendations to consider PCSK9is for patients who need further LLT intensification. The physicians estimated that adding a PCSK9is would be appropriate in no more than 17.2% of their post-MI patients. The results observed by EUROASPIRE IV and DA VINCI studies suggest that a far greater proportion of post-MI patients would benefit from adding a PCSK9i [12, 13].
A conservative approach towards intensive LDL-C lowering was observed in the LDL-C management decisions selected for the fictitious MI cases. Both fictitious cases were designed such that it was not probable that their LDL-C would be brought below the treatment goals recommended by 2019 ESC/EAS guidelines using a combination of high-intensity statins and ezetimibe. The combination of these two medications was, however, sufficient to bring LDL-C in these fictitious cases below the treatment goals recommended by the 2016 guidelines. In each of the participating countries, 11% of physicians or fewer chose to use a PCSK9i for case study A, and fewer than 25% chose this treatment option for case study B. Most physicians chose to initiate a statin in case study A, and to add ezetimibe to case study B, a patient already being treated with a high-intensity statin. Hypotheses for why physicians selected these treatment options include: (1) physicians may have not considered use of PCSK9is because of concerns related to their reimbursement criteria; (2) physicians may not have been familiar with the new guidelines and may have been following the 2016 ESC/EAS guidelines or their local guidelines; (3) physicians may have selected the next step in the LLT intensification pathway, with the intention to observe the effect and subsequently evaluate whether further LDL-C lowering is necessary. The 2019 ESC/EAS guidelines recommend that in patients at very high risk of cardiovascular events, LDL-C should be lowered as quickly as possible with high-intensity LLT necessary to bring the LDL-C under the recommended treatment goal. Use of PCSK9is where appropriate may result in patients avoiding unnecessary risk of further cardiovascular events associated with sustained high LDL-C levels.
PCSK9i therapies as a second-line treatment have been found to be very effective at reducing LDL-C. Physicians reported that multiple barriers hinder initiation of treatment with PCSK9is in patients who need this therapy. The requirements for patients to have been treated with the maximally tolerated dose of statin, to have been prescribed ezetimibe, and the application of a minimum LDL-C threshold (in some countries multiple tests above the threshold are required) for the patient to qualify for a PCSK9i therapy were among the most common barriers reported (Table 3). These requirements delay the recommended treatment of patients with LDL-C above the threshold recommended by the guidelines.
The 2021 ESC guidelines on cardiovascular disease prevention in clinical practice focus on achieving LDL-C levels as close as possible to treatment goals, approaching treatment intensification in a stepwise manner to help physicians and patients pursue treatment goals in a way that fits patient profiles and preferences. For patients at very high risk the physician can proceed directly to treatment escalation to achieve the low LDL-C target of < 1.4 mmol/l (55 mg/dl) [22].
The strengths of this study include that it evaluated treatment practices across both PCPs and SCPs in six European countries, covering a broad range of treatment decisions. The data were collected consistently across all countries, allowing comparison of the results across the countries. The study was robust, with minimal missing data. An inherent limitation of this survey is that physicians were not asked to consult medical records; therefore, the answers physicians provide about their practice are based on recall and therefore cannot be independently validated. Steps were taken to mitigate the recall bias: the physicians were asked to limit their responses to reflect the previous 2 months. Physicians may feel obliged to report treatment procedures based on what is recommended in clinical guidelines; therefore, the full extent of potential variance between what should happen and what does happen may not be detected. To reduce this potential information bias, the survey restricted reference to guidelines. The sampling process was based on the panel held by the recruitment agency and, against that list, a set of screening criteria was applied with the aim to recruit physicians with experience of the post-MI patient pathway. This creates a potential selection bias, as the physicians who choose to be on these panels may not be representative of all physicians. For example, physicians in senior positions or involved in administration, research, or teaching may be less likely to participate because of their busy schedule. However, the physician panels used to recruit participants have been used in previous studies and include many physicians, which should limit the impact of any potential bias arising from the selection of physicians. No cardiac rehabilitation specialist was recruited from France, which is a limitation of this study.
Conclusions
Our results show that there is substantial variation in patient pathways and LDL-C management across six major European countries, which leads to inconsistencies in medical care of post-MI patients. It takes time for harmonization of local guidelines to adopt changes in ESC/EAS guidelines for management of hyperlipidemia. This, in combination with multiple administrative barriers, hinders prescription of innovative and highly effective lipid-lowering drugs, substantially reducing physicians’ ability to lower LDL-C in post-MI patients below the recommended treatment goals and leaving patients at excess risk of subsequent cardiovascular events. Steps towards elimination of administrative barriers enabling quicker intensification of LLT, optimization of LDL-C management pathways, and harmonization of local guidelines for treatment of hyperlipidemia would benefit post-MI patients in Europe.
References
ESC. CVD in Europe and ESC Congress figures. https://www.escardio.org/The-ESC/Press-Office-Fact-sheets/.
Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77. https://doi.org/10.1093/eurheartj/ehx393.
Ference B, Ginsberg H, Graham I, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society consensus panel. Eur Heart J. 2017;38(32):2459–72. https://doi.org/10.1093/eurheartj/ehx144.
Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366(9493):1267–78. https://doi.org/10.1016/S0140-6736(05)67394-1.
Knuuti J, Wijns W, Saraste A, et al. 20119 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407–77. https://doi.org/10.1093/eurheartj/ehz425.
Danchin N, Ferrieres J, Puymirat E, et al. Association between lipid lowering regimen intensity at discharge and long-term mortality in optimally-treated patients with acute myocardial infarction. The FAST-MI programme. In. ESC Congress 2020 - The digital experience; 2020.
Schubert J, Lindahl B, Melhus H, et al. Low-density lipoprotein cholesterol reduction and statin intensity in myocardial infarction patients and major adverse outcomes: a Swedish nationwide cohort study. Eur Heart J. 2020;00:1–10. https://doi.org/10.1093/eurheartj/ehaa1011.
Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–88. https://doi.org/10.1093/eurheartj/ehz455.
Drexel H, Coats AJS, Spoletini I, et al. An expert opinion paper on statin adherence and implementation of new lipid-lowering medications by the ESC Working Group on cardiovascular pharmacotherapy: barriers to be overcome. Eur Heart J Cardiovasc Pharmacother. 2020;6(2):115–21. https://doi.org/10.1093/ehjcvp/pvz079.
Saborowski M, Dolle M, Manns MP, et al. Lipid-lowering therapy with PCSK9-inhibitors in the management of cardiovascular high-risk patients: effectiveness, therapy adherence and safety in a real world cohort. Cardiol J. 2018;25(1):32–41. https://doi.org/10.5603/CJ.a2017.0137.
Cholesterol C, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670–81.
Kotseva K, De Backer G, De Bacquer D, et al. Lifestyle and impact on cardiovascular risk factor control in coronary patients across 27 countries: results from the European Society of Cardiology ESC-EORP EUROASPIRE V registry. Eur J Prevent Cardiol. 2019;26(8):824–35. https://doi.org/10.1177/2047487318825350.
Ray KK, Molemans B, et al. EU-wide cross-sectional observational study of lipid-modifying therapy use in secondary and primary care: the DA VINCI study. Eur J Prevent Cardiol. 2021;28:1279–89. https://doi.org/10.1093/eurjpc/zwaa047.
Barrios V, Soronen J, Carter AM, et al. Lipid management across Europe in the real-world setting: a rapid evidence review. Curr Med Res Opin. 2021;37(12):2049–59. https://doi.org/10.1080/03007995.2021.1973396.
Streiner DL, Norman GR. Health measurement scales: a practical guide to their development and use. 4th ed. Oxford: Oxford University Press; 2008.
Reiner Z, De Backer G, Fras Z, et al. Lipid lowering drug therapy in patients with coronary heart disease from 24 European countries-findings from the EUROASPIRE IV survey. Atherosclerosis. 2016;246:243–50. https://doi.org/10.1016/j.atherosclerosis.2016.01.018.
De Luca L, Piscione F, Colivicchi F, et al. Contemporary management of patients referring to cardiologists one to three years from a myocardial infarction: the EYESHOT Post-MI study. Int J Cardiol. 2018;273:8–14. https://doi.org/10.1016/j.ijcard.2018.08.055.
Piepoli MF, Corra U, Dendale P, et al. Challenges in secondary prevention after acute myocardial infarction: a call for action. Eur Heart J Acute Cardiovasc Care. 2017;6(4):299–310. https://doi.org/10.1177/2048872616689773.
Schwaab B, Zeymer U, Jannowitz C, et al. Improvement of low-density lipoprotein cholesterol target achievement rates through cardiac rehabilitation for patients after ST elevation myocardial infarction or non-ST elevation myocardial infarction in Germany: results of the PATIENT CARE registry. Eur J Prev Cardiol. 2019;26(3):249–58. https://doi.org/10.1177/2047487318817082.
Haute Autorité de Santé. Clinical Practice Indicators Myocardial Infarction (MI) “From 1st symptoms to follow-up at 1 year. https://www.hassante.fr/portail/upload/docs/application/pdf/201308/cpi_mi_complete_document_fv.pdf.
Pedro-Botet J, Rubies-Prat J. Statin-associated muscle symptoms: beware of the nocebo effect. Lancet. 2017;389(10088):2445–6. https://doi.org/10.1016/S0140-6736(17)31163-7.
Visseren FLJ, Mach F, Smulders YM, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42(34):3227–337. https://doi.org/10.1093/eurheartj/ehab484.
Acknowledgements
The authors thank the study participants for their involvement in the study and Marie Chivers, Adella Peyton, and Max Thomas of PRMA Consulting Ltd, who provided medical writing services and editorial assistance in the preparation of this article respectively. Support for this assistance was funded by Amgen (Europe) GmbH.
Funding
Sponsorship for this study, open access and rapid service fee were funded by Amgen (Europe) GmbH.
Medical Writing and/or Editorial Assistance
Medical writing support was provided by Marie Chivers and editorial support was provided by Adella Payton and Max Thomas, employees of PRMA Consulting. Support for this assistance was funded by Amgen (Europe) GmbH.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Eduard Sidelnikov, Samara Ferguson and Christina Rowlands. The first draft of the manuscript was written by Marie Chivers and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Prior presentation
The abstract, methodology and preliminary results of this article were presented as a poster at Virtual ISPOR Europe, 16–19 November 2020.
Disclosures
Eduard Sidelnikov and Guillermo Villa are full-time employees of Amgen (Europe) GmbH. Samara Ferguson and Christina Rowlands are employees of PRMA Consulting Ltd at the time of conducting this research and do not have any conflicting interests. PRMA Consulting was paid by Amgen to conduct the study and contribute to the manuscript preparation, and receives professional fees from a number of companies. José R. González-Juanatey reports personal fees from Amgen, Bayer, Boehringer Ingelheim, MSD, Daiichi Sankyo-Lilly, Novartis, Novo Nordisk, Pfizer, Sanofi Aventis, and Servier.
Nadeem Qureshi, Sotiris Antoniou, Jan Cornel, Francois Schiele, Pasquale Perrone-Filardi and Johannes Brachmann declare that they have no competing interests.
Compliance with Ethics Guidelines
The study was approved by the research ethics committee of the University of Technology, Sydney, Australia, on 7 November 2019 (application no. PRMA4149_2019 UTS HREC ref no. ETH18-2910). This study was performed in accordance with the Helsinki declaration of 1964, and its later amendments. All participants provided informed consent to participate in the study.
Data Availability
The datasets generating during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Qureshi, N., Antoniou, S., Cornel, J.H. et al. European Physician Survey Characterizing the Clinical Pathway and Treatment Patterns of Patients Post-Myocardial Infarction. Adv Ther 40, 233–251 (2023). https://doi.org/10.1007/s12325-022-02344-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02344-6