Abstract
Introduction
We aimed to assess the efficacy and safety of lixisenatide and basal insulin (BI) according to timing of treatment initiation, treatment compliance, and number of concomitant daily injections in Japanese individuals with type 2 diabetes (T2D).
Methods
Each substudy analyzed subgroup data from the 3-year post-marketing surveillance PRANDIAL study. Endpoints included glycated hemoglobin (HbA1c), postprandial glucose, treatment response (HbA1c < 7.0% at week 24 and 156), and safety. Changes in HbA1c levels were analyzed using paired t tests; between-group comparisons were made using analysis of variance (ANOVA).
Results
Of 2679 participants, 46.5% initiated BI before lixisenatide, 12.0% the same day, 2.7% between 1 and 90 days, and 2.8% at 91 or more days after lixisenatide; 36.0% did not receive BI. Overall, 85.4% of patients were compliant with lixisenatide treatment. The majority of patients (52.4%) received two injections/day (one was lixisenatide). Compared with other subgroups taking BI and lixisenatide, the subgroup starting them simultaneously had a mean change in HbA1c of − 0.69% [8 mmol/mol] (vs + 0.07% [0.8 mmol/mol] to − 0.79% [9 mmol/mol]) and numerically higher treatment response (21.0% vs 8.3–18.7%), but more hypoglycemia (8.1% vs 2.3–2.8%).
Conclusions
Japanese people with T2D achieved better glycemic control by simultaneous as opposed to sequential initiation of lixisenatide and BI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Japanese people with type 2 diabetes treated with basal insulin or glucagon-like peptide 1 receptor agonists alone have a diminishing probability of achieving glycemic control; however, addition of lixisenatide to basal insulin demonstrates significant improvements. |
Reported here are the results of three substudies of a 3-year post-marketing surveillance study conducted in Japan, assessing the effectiveness and safety of lixisenatide according to the sequence of therapy initiation, the level of treatment compliance, and the number of daily injections. |
What was learned from the study? |
Simultaneous initiation of lixisenatide and basal insulin on the same day resulted in significant improvements in both glycated hemoglobin and postprandial plasma glucose and was associated with the highest treatment response rate among subgroups receiving both agents. |
No relationship between the number of daily injections and glycemic control was observed; however, treatment response rates were higher in participants receiving only one injection daily. |
Although development of adverse drug reactions appeared to be unrelated to timing of insulin initiation, the long-term relationship between drug compliance, glycemic control, and adverse drug reactions warrants further investigation. |
Introduction
In Japanese people, type 2 diabetes (T2D) is characterized by deterioration of pancreatic β-cell functional capacity, which leads to a predominant defect in insulin secretion with pronounced postprandial plasma glucose (PPG) excursions [1,2,3]. Glucagon-like peptide 1 (GLP-1) is secreted postprandially by cells in the intestine, leading to stimulation of insulin release and the suppression of glucagon; however, in Japanese people, endogenous GLP-1 levels are low and meal-induced secretion of GLP-1 is negligible, suggesting an underlying GLP-1 deficiency [4,5,6], which may have a genetic origin.
GLP-1 receptor agonists (GLP-1 RAs) improve fasting and postprandial hyperglycemia, have a low risk of hypoglycemia [7, 8], and may be particularly useful in Japanese people with T2D [5, 6, 9,10,11]. Recent real-world evidence from a retrospective analysis of data from the Japan Diabetes Clinical Data Management Study Group (JDDM) indicates that GLP-1 RA therapy for Japanese people with T2D is associated with favorable clinical outcomes, such as improved HbA1c, reductions in body weight, and improved lipid profiles, as well as high treatment persistence rates (80.5% at 6 months and 66.2% at 12 months) [12].
First-line treatment of T2D generally involves lifestyle modifications and oral antidiabetic drugs (OADs) as appropriate, but regimen intensification through addition of an injectable agent (GLP-1 RA or basal insulin) to OADs is often required in real-world practice to achieve glycemic control [7]. If an individual requires further glucose-lowering therapy despite treatment with a GLP-1 RA or basal insulin, an additional injectable agent can be added [7, 8, 13].
A database analysis of Japanese people with T2D recently found that the probability of achieving glycemic control diminished over time among those who initiated BI or GLP-1 RA therapy after failing to achieve glycemic control with OAD therapy [14]. Real-world evidence from the USA indicates that early combination therapy or simultaneous initiation of insulin and GLP-1 RAs leads to better glycemic control than delayed combination therapy/sequential initiation [15,16,17].
Lixisenatide, a once-daily short-acting GLP-1 RA, has been evaluated as add-on therapy to basal insulin ± sulfonylurea as part of the multinational phase 3 GetGoal clinical trial program [18,19,20,21]. Compared with placebo, add-on lixisenatide consistently improved glycemic control, with a pronounced postprandial effect, in the predominantly Caucasian T2D populations of the GetGoal-L and GetGoal-Duo 1 trials [18, 19], and the overall mixed Asian population and Japanese subpopulation of the GetGoal-L-Asia trial [20, 21]. Lixisenatide is a safe and effective option for the treatment of T2D in Japanese people in routine clinical practice according to results of a 3-year post-marketing surveillance (PMS) study [22].
Here, we report on three substudies of the 3-year PMS study, which assessed the efficacy and safety of lixisenatide according to the sequence of therapy initiation, the level of treatment compliance, and the number of daily injections. Patterns of adverse drug reactions (ADRs) across subgroups were also assessed.
Methods
Study Design and Population
Individuals with T2D who initiated treatment with lixisenatide between March 2014 and June 2017 were prospectively registered in an observational, multicenter, open-label PMS study, called Post-maRketing surveillANce in patients with type 2 DIAbetes mellitus to evaluate the long-term safety and effectiveness of Lixisenatide (PRANDIAL). The study was conducted in accordance with the Japanese Ministerial Ordinance on Good Post-Marketing Study Practice (Ministry of Health, Labour and Welfare Ordinance No. 171, December 20, 2004) and the ethical guidelines for medical and health research involving human subjects. Under the Japanese regulations for PMS studies, requirement to conform with the Declaration of Helsinki was not applicable for this study and there was no requirement for review or approval by the ethics committee of the participating medical institutions nor for collection of informed consent from study participants. All data were collected anonymously to protect personal information; the study sponsor had no access to individual participant medical records. Full details of the parent study design have been described previously [22].
Briefly, data were collected from electronic case report forms for 3 years after initiation of lixisenatide treatment. The date of initiating lixisenatide was defined as the index date, and baseline measurements were defined as those most recently taken within 2 months before and leading up to the index date. Effectiveness endpoints included changes in parameters of glycemic control (i.e., glycated hemoglobin [HbA1c] and PPG), and the proportion of participants with HbA1c < 7.0% at week 24 and 156 by subgroup. ADRs were defined as adverse events for which a causal relationship with lixisenatide could not be ruled out by the treating physician. Only those occurring in at least 1% of the total analysis population (n = 2679) are reported here; ADRs of special interest for this report included hypoglycemia (Medical Dictionary for Regulatory Activities [MedDRA] preferred term [PT]), administration site reactions (MedDRA PT), gastrointestinal disorders (MedDRA System Organ Class [SOC] term), and laboratory tests (MedDRA SOC term).
Substudies
In the first substudy, a post hoc analysis, study participants were classified on the basis of the time interval between the start of lixisenatide therapy (index date) and initiation of basal insulin (see Fig. S1 in the Supplementary Material for details): basal insulin started prior to the start of lixisenatide, both started on the same day, basal insulin started between 1 and 90 days after lixisenatide, basal insulin started at least 91 days after lixisenatide, or no concomitant basal insulin.
In the second substudy, study participants were grouped according to compliance with lixisenatide therapy at 6 months after starting treatment, where compliance was defined as using lixisenatide as directed. Assessment of compliance was pre-specified in the study protocol and reported in a subjective manner by physicians, such that they qualitatively evaluated how participants were able to comply with the daily injection over 6 months. The three subgroups were compliance ≥ 75% (“compliant”), ≥ 50% and < 75% (“sometimes non-compliant”), and < 50% (“not compliant”).
The third substudy, a post hoc analysis, grouped participants on the basis of the number of injections per day at the start of lixisenatide therapy: lixisenatide injection once daily (OD) only, lixisenatide OD plus one other injectable medication OD (total of two injections daily), and lixisenatide OD plus at least two other injections daily, which may have included insulin preparations (i.e., long-acting, intermediate, premixed, rapid-acting, or other).
Statistical Analysis
The effectiveness analysis set comprised all study participants with T2D who received lixisenatide in accordance with the approved product label (subcutaneous injection, 10–20 µg administered within 1 h before breakfast [23]) for whom efficacy data were available and who had received their first dose of lixisenatide within 15 days of registration. Safety data were also assessed in this analysis set.
Summary statistics included mean ± standard deviation (SD) for continuous measures, and counts and proportions for categorical measures. Paired t tests were used to test changes in HbA1c from baseline. Between-group comparisons were made using analysis of variance (ANOVA) for the change from baseline in HbA1c in the compliance and injection number analyses. All tests were conducted with a significance level of 5%. Data were calculated using the last observation carried forward (LOCF) approach.
Results
Study Participants
In total, 3177 participants were registered at 516 sites and electronic case report forms were available for 3083 participants (Fig. S2 in the Supplementary Material). This report includes fewer participants than were included in the overall analysis of the PMS [22] because data extraction for the current analysis was conducted prior to collection of electronic case report forms from all eligible participants. The overall effectiveness analysis set included 2679 participants. Exclusion from the effectiveness analysis set was mainly because no data were collected after lixisenatide was first administered (n = 348).
Within the effectiveness analysis set, 1714 (64.0%) study participants received concomitant basal insulin prior to lixisenatide or at a known starting date after lixisenatide initiation (Fig. S2 in the Supplementary Material). In the basal insulin timing substudy, most of these individuals began basal insulin prior to starting treatment with lixisenatide (n = 1245; 46.5%). The next largest subgroup were those individuals who initiated lixisenatide and basal insulin treatment on the same day (n = 322; 12.0%). Among participants who started basal insulin only after starting treatment with lixisenatide, 72 (2.7%) individuals began basal insulin between 1 and 90 days after lixisenatide, and 75 (2.8%) began basal insulin at least 91 days after lixisenatide. Concomitant basal insulin was not used in 965 (36.0%) study participants.
In the treatment compliance substudy, most participants were included in the compliant subgroup (n = 2289; 85.4%); far fewer participants were in the sometimes noncompliant (n = 305; 11.4%) and not compliant subgroups (n = 85; 3.2%) (Fig. S2 in the Supplementary Material).
In the daily injection number substudy, most participants had two injections daily, one of which was lixisenatide (n = 1405; 52.4%), and the next largest subgroup were those receiving only lixisenatide OD (n = 993; 37.0%) (Fig. S2 in the Supplementary Material).
A summary of the baseline characteristics of the effectiveness analysis set, overall and in each subgroup for each of the three substudies, is shown in Table 1. Overall, the mean (SD) age was 58.9 (13.1) years, 38.5% were aged 65 years or older, 54% of participants were male, and the majority of participants were outpatients (82.9%). The mean (SD) baseline BMI was 28.7 ± 5.7 kg/m2 and the mean (SD) duration of T2D was 12.8 (8.6) years, with mean (SD) HbA1c of 8.7% (1.7%) [or 72 (19) mmol/mol] and baseline PPG of 210.4 (89.4) mg/dL.
There was some variability in baseline clinical parameters among the timing of basal insulin therapy subgroups: the highest mean HbA1c level (9.5% [80 mmol/mol]) occurred in the subgroup that received basal insulin between 1 and 90 days after initiating lixisenatide (p = 0.0097, across-groups ANOVA comparison). In the analysis of treatment compliance status, age (p = 0.0217), HbA1c (p = 0.0013), and PPG (p = 0.0092) were significantly different among subgroups at baseline (Table 1). All baseline parameters were significantly different among daily injection number subgroups. Mean T2D duration was the longest (16.0 years; p < 0.0001), and BMI (29.8 kg/m2; p < 0.0001), HbA1c (9.1% [76 mmol/mol]; p < 0.0001), and PPG (217.6 mg/dL; p = 0.0027) the highest in the subgroup receiving a lixisenatide OD injection plus at least two other injections daily.
The mean (SD) lixisenatide dosage was 16.1 (4.1) μg/day overall at week 156 (Table 1). In the basal insulin timing substudy, the subgroup that initiated basal insulin at least 91 days after starting lixisenatide reached the highest mean lixisenatide daily dosage (17.3 μg/day; p < 0.0001, across-groups ANOVA comparison). Lixisenatide dosage was also significantly different across treatment compliance subgroups, where the subgroup with the highest compliance rate reached the highest dosage (mean [SD] 16.3 [4.1] μg/day) and the lowest compliance subgroup had the lowest mean lixisenatide dosage (14.6 [4.1] μg/day; p < 0.0001, across-groups ANOVA comparison). Lixisenatide dosage did not vary significantly between daily injection number subgroups.
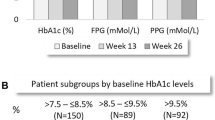
Change in Glycemic Parameters in the Basal Insulin Timing Substudy
Over the 3-year observation period, the HbA1c level decreased from baseline by a mean (SD) of − 0.69% (2.15%) [− 8 (24) mmol/mol] in the subgroup of participants who started lixisenatide and basal insulin simultaneously (p < 0.0001, LOCF) (Fig. 1a). There were also significant decreases in HbA1c from baseline in participants that began receiving basal insulin prior to the start of lixisenatide (mean [SD] change − 0.43% [1.87%], − 5 [20] mmol/mol; p < 0.0001) or between 1 and 90 days after starting lixisenatide (− 0.79% [2.28%], − 9 [25] mmol/mol; p = 0.0076). However, there was no significant change in HbA1c from baseline in participants who started basal insulin at least 91 days after initiating lixisenatide therapy. Participants who did not receive concomitant basal insulin experienced a significant improvement in HbA1c from baseline (mean [SD] change − 0.40% [1.60%], − 4 [18] mmol/mol; p < 0.0001). The changes in HbA1c at week 156 mirrored changes that had already been observed at week 24 (Fig. 1a). Figure 1b illustrates the change in HbA1c from baseline over the entire observation period in each subgroup for the basal insulin timing substudy.
Glycated hemoglobin (HbA1c) values in participants receiving lixisenatide according to the timing of initiation of basal insulin shown as a mean ± standard deviation (SD) change in HbA1c at week 24 and week 156, and b mean HbA1c over the 156-week observation period. Results are for the effectiveness analysis population (LOCF). ***p < 0.0001 vs baseline by paired t test. **p < 0.01 vs baseline by paired t test. *p < 0.05 vs baseline by paired t test. B/line baseline, BI basal insulin, Lixi lixisenatide, LOCF last observation carried forward, Wk week
In general, PPG improved from baseline at weeks 24 and 156, which reached statistical significance at the latter time point (Table S1 in the Supplementary Material), although these results are for only a small subset of participants who had PPG data available at both time points. Participants who started lixisenatide and basal insulin on the same day experienced the largest reduction in PPG from baseline at week 156 (mean [SD] change − 62.0 [87.1] mg/dL), followed by participants who had been receiving basal insulin prior to starting lixisenatide (− 52.0 [104.7] mg/dL).
Change in HbA1c in the Treatment Compliance Substudy
Significant decreases in HbA1c from baseline at week 156 were observed among participants in the compliant subgroup (mean [SD] change − 0.50% [1.84%], − 5 [20] mmol/mol; p < 0.0001), whereas there was no significant change in HbA1c in the sometimes noncompliant and not compliant subgroups (− 0.16% [1.67%], − 2 [18] mmol/mol; p = 0.1152 and + 0.13% [1.93%], + 1 [21] mmol/mol; p = 0.5843, respectively; Fig. 2a). A similar pattern of results was observed at week 24. Between-subgroup differences in the mean change in HbA1c from baseline at week 156 were significant (p = 0.0004; ANOVA).
Mean change ± standard deviation (SD) in glycated hemoglobin (HbA1c) from baseline at week 24 and week 156 in the a treatment compliance subgroups and b daily injection number subgroups. Results are for the effectiveness analysis population (LOCF). For the 3 participants for whom daily injection number data were missing (not shown), the mean (SD) change from baseline in HbA1c was + 0.63% (0.62%) [+ 7 (7) mmol/mol] (p = 0.2144 vs baseline). ***p < 0.0001 vs baseline by paired t test. **p < 0.01 vs baseline by paired t test. *p < 0.05 vs baseline by paired t test. Lixi lixisenatide, LOCF last observation carried forward, OD once daily
Change in HbA1c in the Daily Injection Number Substudy
HbA1c was significantly decreased in each of the subgroups based on the number of daily injections received at baseline. Mean (SD) changes from baseline in HbA1c at week 156 were − 0.43% (1.70%) [− 5 (19) mmol/mol] in the lixisenatide OD only subgroup (p < 0.0001), − 0.50% (1.93%) [− 5 (21) mmol/mol] in the lixisenatide OD plus one other injection OD subgroup (p < 0.0001), and − 0.27% (1.71%) [− 3 (19) mmol/mol] in the lixisenatide OD plus at least two other injections subgroup (p = 0.0139) (Fig. 2b). These changes mirrored those observed at week 24. However, between-subgroup differences in the mean change from baseline in HbA1c at week 156 were not statistically significant (p = 0.1732; ANOVA).
Lixisenatide Treatment Response
In the overall study population, the rate of lixisenatide treatment response (HbA1c < 7.0% [53 mmol/mol]) was 21.6% (LOCF analysis). With regard to timing of basal insulin initiation (Fig. S3 in the Supplementary Material), treatment response rates were 21.0% in the subgroup who initiated basal insulin and lixisenatide simultaneously and 18.7% in the subgroup who started basal insulin before lixisenatide. Numerically lower treatment response rates were observed in participants who started basal insulin after lixisenatide treatment, either between 1 and 90 days after lixisenatide (14.5%) or at least 91 days after lixisenatide (8.3%). The treatment response rate was highest in the participants who did not receive concomitant basal insulin (27.0%).
In the treatment compliance substudy, the treatment response rate was 23.2% in participants in the compliant subgroup, which was numerically higher than in participants in the other two subgroups (11.7% in the sometimes not compliant subgroup and 13.9% in the not compliant subgroup).
In the daily injection number substudy, participants whose only treatment was lixisenatide OD at the time of lixisenatide initiation had the highest rate of treatment response (26.2%) (Fig. S3 in the Supplementary Material). Response rates were 19.8% in participants receiving lixisenatide OD plus one other injection daily and 13.6% in those receiving lixisenatide OD plus at least two other daily injections.
Safety
Overall, 18.7% of participants experienced an ADR (Table 2). Of particular interest was hypoglycemia, for which events were classified as severe (serious or requiring assistance), documented symptomatic (plasma glucose ≤ 70 mg/dL), or nocturnal. Events were considered serious if they were life-threatening or important medical events, fatal ADRs, resulted in hospitalization or congenital defect, or required intervention. The overall incidence of hypoglycemia (any severity) was 2.8%, and of serious hypoglycemia was 0.07%. Few participants experienced an administration site reaction (1.0%; Table 2). The most common gastrointestinal-related ADR was nausea (8.1%).
Basal Insulin Timing Substudy
Across the basal insulin timing subgroups, ADRs occurred most commonly within the first 4 weeks of observation (Fig. 3a). The proportion of patients within each timing subgroup experiencing an ADR had dropped to below approximately 2.5% by weeks 28–32. By weeks 84–88, almost no patients experienced an ADR, with the exception of weeks 104–108 in the subgroup where basal insulin was started between 1 and 90 days after starting lixisenatide.
The proportion of study participants with a any adverse drug reaction (ADR) and b gastrointestinal ADRs, during the 156-week observation period by subgroup according the timing of basal insulin initiation relative to lixisenatide. Data are for the safety analysis population. BI basal insulin, Lixi lixisenatide
Hypoglycemia (any severity) occurred in 8.1% of participants who started lixisenatide and basal insulin simultaneously (Table 2). The incidence of hypoglycemia was less than 5% in the remaining subgroups, and the lowest incidence (1.8%) was in participants who did not receive concomitant basal insulin. There was no consistent pattern across basal insulin timing subgroups for the incidence of gastrointestinal-related ADRs (Table 2). The incidence of nausea was 9.3% in the subgroup of participants who started basal insulin prior to lixisenatide, and 4.0–7.8% in the subgroups of participants who started basal insulin at the same time as or after lixisenatide. Vomiting and abdominal discomfort were infrequent ADRs, occurring in 1.2–1.6% and 0.9–2.7% of participants across the subgroups, respectively. Figure 3b illustrates the proportion of patients in each basal insulin timing subgroup who had gastrointestinal-related ADRs across the 156-week observation period. Most gastrointestinal-related ADRs occurred with the first 4 weeks of observation, with the incidence decreasing rapidly thereafter.
Treatment Compliance Substudy
Participants in the not compliant subgroup had a numerically higher incidence of ADRs (28.2%) compared with the compliant subgroup (18.0%) and sometimes not compliant (21.3%) subgroups (Table 2). Hypoglycemia occurred in 3.1% of participants in the compliant subgroup, but in only 1.3% of those who were sometimes not compliant and 1.2% of those in the not compliant subgroup. With the exception of abdominal discomfort, gastrointestinal-related ADRs were reported most frequently in the not compliant subgroup. The subgroup with the lowest incidence of gastrointestinal-related ADRs was the compliant subgroup.
Daily Injection Number Substudy
Participants receiving only lixisenatide OD experienced the lowest incidence of ADRs (16.7%); the incidence of ADRs in participants who received lixisenatide OD plus one other injection or lixisenatide OD plus at least two other daily injections was 18.7–20.0% (Table 2). Hypoglycemia episodes (any severity) occurred in a smaller proportion of participants receiving only lixisenatide OD than in the other injection number subgroups (1.6% vs 3.6%). Nausea, vomiting, and abdominal discomfort were reported in 0.7–9.0% of participants across the three injection number subgroups, with nausea (6.9–9.0%) being the most frequent of these in all three subgroups.
Discussion
Three substudies of a 3-year PMS study of lixisenatide in Japanese people with T2D examined the efficacy and safety of lixisenatide according to the timing of its initiation in relation to starting basal insulin, different levels of treatment compliance, or the number of daily injections the participants received. When lixisenatide and basal insulin were started simultaneously, both HbA1c and PPG significantly improved from baseline, and these improvements were among the greatest observed across the four subgroups who received lixisenatide and basal insulin. Simultaneous initiation of lixisenatide and basal insulin was also associated with the highest rate of treatment response (21.0%) among subgroups receiving both agents. Study participants with good treatment compliance (at least 75%) experienced significant decreases in HbA1c from baseline that were significantly greater than those observed in the less compliant subgroups. The number of daily injections received at the time of starting lixisenatide appeared to have no effect on glycemic control (specifically reduction in HbA1c), but did appear to affect treatment response rates since participants receiving only one injection daily (lixisenatide OD) had the highest treatment response (26.2%) compared with those receiving two, or three or more, daily injections (19.8% and 13.6%, respectively).
Our results on the benefits of simultaneous (rather than sequential) initiation of lixisenatide plus basal insulin expand on findings from previous real-world studies in US populations. In a study by Peng et al., people with HbA1c ≥ 7.0% [≥ 53 mmol/mol] on OADs who initiated both basal insulin and GLP-1 RA treatment on the same day had numerically greater reductions in HbA1c and were more likely to achieve glycemic control (HbA1c < 7.0% [< 53 mmol/mol]) than those who initiated basal insulin first followed by a GLP-1 RA within 90 days or more than 90 days later [15]. In a study by Rosenstock et al., individuals with HbA1c ≥ 9.0% [≥ 75 mmol/mol] on OADs who initiated basal insulin and GLP-1 RAs within 30 days or up to 90 days were significantly more likely to achieve glycemic control (HbA1c < 7.0% [< 53 mmol/mol]) than those who initiated the two therapies 91–360 days apart [16]. Such evidence indicates that delaying the intensification of therapy while waiting to determine the effectiveness of existing treatments may not be the best approach [16].
A pronounced effect of lixisenatide plus basal insulin combination therapy on PPG improvements was observed in the current study, particularly when initiated simultaneously or when basal insulin was started prior to lixisenatide, and reflects the Japanese authors’ clinical experience. The effect on PPG is particularly important in Asia [5, 9, 11], where individuals with T2D are often prescribed short-term intensive insulin therapy to remove glucotoxicity first, followed by de-escalation of treatment and the introduction of GLP-1 RA therapy. Further, control of PPG is likely to be an important goal for individuals who are unable to achieve HbA1c targets [5, 9, 11]. A large proportion of our patient population initiated treatment with lixisenatide after being on basal insulin therapy, likely reflecting the clinicians’ attempts to address residual hyperglycemia, which is a well-recognized unmet need for those receiving basal insulin [24]. Our results indirectly support the simultaneous initiation of lixisenatide and basal insulin as an alternative approach. By reducing hyperglycemia, basal insulin enhances the effects of incretins on β-cell function [25], which augments the effect of a GLP-1 RA on PPG, while simultaneously reducing fasting plasma glucose [26].
As may be expected, participants with good compliance in the first 6 months of treatment experienced significantly better HbA1c reductions and treatment response rates than those with poorer treatment compliance, although these results must be interpreted with caution because of the small number of participants in the not compliant subgroup. While the relationship between treatment compliance and treatment outcomes in patients with T2D is well established [27], the importance of compliance in the first 6 months is not well studied, and further investigation is required to better characterize the clinical outcomes in patients with good early compliance. It is also reassuring that the majority of study participants (85.4%) had a compliance rate of at least 75% at 6 months after starting lixisenatide. This is broadly similar to the rate of treatment persistence at 6 months reported in a real-world Japanese study of GLP-1 RAs (approx. 80%) [12].
In our PMS substudies, the incidence of hypoglycemia was highest in participants who initiated basal insulin and lixisenatide simultaneously. The relatively higher incidence of hypoglycemia in this subgroup (8.1% vs 1.8% for the no concomitant basal insulin subgroup) was not unexpected, because hypoglycemia is more likely when lixisenatide is combined with antidiabetic medications that directly lower blood glucose, such as basal insulin [28, 29]. To mitigate the risk of hypoglycemia, dose reductions of either the GLP-1 RA or basal insulin may be considered [7]. Good treatment compliance was also associated with the highest incidence of hypoglycemia (3.1%), although still broadly similar to that observed in the overall population (2.8%). This may reflect the fact many patients are willing to take their medication as directed to achieve the optimal benefit, even at the expense of a slight increase in the risk of adverse events.
As the number of daily injections increased, so did the overall ADR incidence, including the incidence of hypoglycemia (1.6% with lixisenatide OD only vs 3.6% in each of the other injection number subgroups). The additional daily injections were likely fast-acting or premixed insulin injections, which may explain this observation.
The most common ADRs with GLP-1 RAs, including lixisenatide, are nausea and vomiting [29, 30]. In the first 4 weeks of lixisenatide treatment, broadly similar proportions in the different basal insulin timing subgroups experienced a gastrointestinal ADR. The incidence of vomiting was low, with no obvious pattern related to the timing of basal insulin relative to lixisenatide treatment. The subgroup of patients who started basal insulin prior to starting lixisenatide had the highest incidence of nausea (9.3%) and those who started basal insulin at least 91 days after lixisenatide had the lowest (4.0%). The nausea incidence was intermediate in the subgroups where both agents were started simultaneously (7.8%) or participants did not receive concomitant basal insulin (6.9%). It is not immediately apparent why this pattern was observed. A previous study found that iGlarLixi, a fixed-ratio combination of insulin glargine 100 U/mL and lixisenatide, causes fewer gastrointestinal adverse events than lixisenatide alone, attributable to the more gradual titration of lixisenatide that can be achieved with this formulation [31], which supports the tolerability of starting these two agents on the same day. Further prospective studies of the relationship between the timing of treatment initiation (using narrower time intervals) and gastrointestinal tolerability are required.
Current Japanese guidelines state that OADs and/or GLP-1 RA therapy is to be given to noninsulin-dependent individuals in whom favorable glycemic control is not achievable with lifestyle modifications, and that insulin therapy is to be given to those in whom glycemic control targets are not achievable with OADs or GLP-1 RAs [7]. Our study of actual prescribing behavior in clinical practice during the study period seems to indicate that physicians are broadly consistent with Japanese guidelines, as we found that 36% of participants did not receive concomitant basal insulin, probably owing to their reasonable level of glycemic control (baseline HbA1c of 8.4%). Observations from a previous real-world study in Japan support this interpretation of our results: basal insulin was initiated in patients with higher baseline HbA1c than those who initiated GLP-1 RA (9.4% vs 8.8%) [14]. Of those who did receive concomitant basal insulin (n = 1714) in our study, 147 (8.6%) began basal insulin after starting treatment with lixisenatide. The majority started treatment on the same day as (322/1717; 18.8%) or prior to (1245/1714; 72.6%) lixisenatide. This is likely because we began registering subjects for this study in September 2013, and at this time, the only regimens that lixisenatide could be added to were either sulfonylurea ± biguanide or basal insulin ± sulfonylurea.
Although a multivariate analysis to examine the effects of comorbidities on glycemic outcomes was not conducted, the proportions of patients with some comorbidities showed significant variations across the study subgroups. For example, the proportion of patients with multiple comorbidities showed statistically significant differences in the cohort defined by the number of daily injections. The types of comorbidities with significant difference between subgroups were not always consistent across the three substudy cohorts; however, it is possible that some comorbidities may have affected study outcomes. Nonetheless, a multivariate analysis will be required to confirm this association.
A limitation of the current study is the wide cohort definitions in the timing substudy (i.e., starting basal insulin any time prior to lixisenatide, 1–90 days after lixisenatide, and at least 91 days after lixisenatide). Rosenstock et al., in the discussion of their own study of the relative timing of initiation of basal insulin and GLP-1 RAs [16], recommended focusing on participants who initiated therapies at most 30 days apart. Using narrow cohort brackets would provide a clearer time point cutoff for the perceived benefit of starting basal insulin close in time to the initiation of lixisenatide. Other limitations include the lack of an assessment of the effect of prior OAD use on glycemic outcomes, the fact that compliance with lixisenatide was assessed subjectively and only at 6 months, and that confounding factors, such as compliance with combination therapy and the type of insulin, were not assessed. In addition, as a result of the nature of our study design (PMS), collection of continuous glucose monitoring (CGM) data was not possible. It should also be noted that clinical use of CGM was not reimbursed for the wider population with T2D in Japan until April 2022. Lastly, small subgroup sizes may have introduced bias, for example in the subgroups in which basal insulin was initiated 1–90 days or at least 91 days after lixisenatide (n = 72 and n = 75, respectively). Similarly, missing data may not have occurred at random, so the LOCF method for imputation may also introduce a bias, leading to potential over- or underestimation of effectiveness [32].
Conclusion
Better glycemic control in Japanese people with T2D is provided when lixisenatide and basal insulin are initiated simultaneously rather than sequentially, as well as by good short-term treatment compliance to GLP-1 RA therapy. The long-term relationship between drug compliance and both glycemic control and ADRs warrants further investigation.
References
Inaishi J, Saisho Y. Ethnic similarities and differences in the relationship between beta cell mass and diabetes. J Clin Med. 2017;6:12.
Ma RC, Chan JC. Type 2 diabetes in East Asians: similarities and differences with populations in Europe and the United States. Ann N Y Acad Sci. 2013;1281:64–91.
Moller JB, Dalla Man C, Overgaard RV, et al. Ethnic differences in insulin sensitivity, beta-cell function, and hepatic extraction between Japanese and Caucasians: a minimal model analysis. J Clin Endocrinol Metab. 2014;99(11):4273–80.
Lee S, Yabe D, Nohtomi K, et al. Intact glucagon-like peptide-1 levels are not decreased in Japanese patients with type 2 diabetes. Endocr J. 2010;57(2):119–26.
Seino Y, Takami A, Boka G, Niemoeller E, Raccah D, investigators PDY. Pharmacodynamics of the glucagon-like peptide-1 receptor agonist lixisenatide in Japanese and Caucasian patients with type 2 diabetes mellitus poorly controlled on sulphonylureas with/without metformin. Diabetes Obes Metab. 2014;16(8):739–47.
Yabe D, Seino Y, Fukushima M, Seino S. β cell dysfunction versus insulin resistance in the pathogenesis of type 2 diabetes in East Asians. Curr Diab Rep. 2015;15(6):602.
Araki E, Goto A, Kondo T, et al. Japanese clinical practice guideline for diabetes 2019. Diabetol Int. 2020;11(3):165–223.
Levin PA, Nguyen H, Wittbrodt ET, Kim SC. Glucagon-like peptide-1 receptor agonists: a systematic review of comparative effectiveness research. Diabetes Metab Syndr Obes. 2017;10:123–39.
Chan WB, Luk A, Chow WS, Yeung VTF. What next after basal insulin? Treatment intensification with lixisenatide in Asian patients with type 2 diabetes mellitus. J Diabetes. 2017;9(6):562–74.
Kim YG, Hahn S, Oh TJ, Park KS, Cho YM. Differences in the HbA1c-lowering efficacy of glucagon-like peptide-1 analogues between Asians and non-Asians: a systematic review and meta-analysis. Diabetes Obes Metab. 2014;16(10):900–9.
Wang JS, Tu ST, Lee IT, et al. Contribution of postprandial glucose to excess hyperglycaemia in Asian type 2 diabetic patients using continuous glucose monitoring. Diabetes Metab Res Rev. 2011;27(1):79–84.
Ishigaki Y, Strizek A, Aranishi T, et al. Glucagon-like peptide-1 receptor agonist utilization in type 2 diabetes in Japan: a retrospective database analysis (JDDM 57). Diabetes Ther. 2021;12(1):345–61.
American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: Standards of Medical Care in Diabetes—2022. Diabetes Care. 2022;45(Suppl 1):S125–43.
Baxter M, Morimoto Y, Tamiwa M, et al. A real-world observational study evaluating the probability of glycemic control with basal insulin or glucagon-like peptide-1 receptor agonist in Japanese patients with type 2 diabetes. Diabetes Ther. 2020;11(7):1481–96.
Peng XV, Ayyagari R, Lubwama R, et al. Impact of simultaneous versus sequential initiation of basal insulin and glucagon-like peptide-1 receptor agonists on HbA1c in type 2 diabetes: a retrospective observational study. Diabetes Ther. 2020;11(4):995–1005.
Rosenstock J, Ampudia-Blasco FJ, Lubwama R, et al. Real-world evidence of the effectiveness on glycaemic control of early simultaneous versus later sequential initiation of basal insulin and glucagon-like peptide-1 receptor agonists. Diabetes Obes Metab. 2020;22(12):2295–304.
Tong L, Pan C, Wang H, Bertolini M, Lew E, Meneghini LF. Impact of delaying treatment intensification with a glucagon-like peptide-1 receptor agonist in patients with type 2 diabetes uncontrolled on basal insulin: a longitudinal study of a US administrative claims database. Diabetes Obes Metab. 2018;20(4):831–9.
Riddle MC, Aronson R, Home P, et al. Adding once-daily lixisenatide for type 2 diabetes inadequately controlled by established basal insulin: a 24-week, randomized, placebo-controlled comparison (GetGoal-L). Diabetes Care. 2013;36(9):2489–96.
Riddle MC, Forst T, Aronson R, et al. Adding once-daily lixisenatide for type 2 diabetes inadequately controlled with newly initiated and continuously titrated basal insulin glargine: a 24-week, randomized, placebo-controlled study (GetGoal-Duo 1). Diabetes Care. 2013;36(9):2497–503.
Seino Y, Ikeda Y, Niemoeller E, et al. Efficacy and safety of lixisenatide in Japanese patients with type 2 diabetes insufficiently controlled with basal insulin ± sulfonylurea: a subanalysis of the GetGoal-L-Asia study. Horm Metab Res. 2015;47(12):895–900.
Seino Y, Min KW, Niemoeller E, Takami A, Investigators EG-LAS. Randomized, double-blind, placebo-controlled trial of the once-daily GLP-1 receptor agonist lixisenatide in Asian patients with type 2 diabetes insufficiently controlled on basal insulin with or without a sulfonylurea (GetGoal-L-Asia). Diabetes Obes Metab. 2012;14(10):910–7.
Terauchi Y, Usami M, Inoue T. The durable safety and effectiveness of lixisenatide in Japanese people with type 2 diabetes: the post-marketing surveillance PRANDIAL study. Adv Ther. 2022;39(6):2873–88.
Sanofi K.K. Lixisenatide prescribing information (in Japanese). 2016. https://www.info.pmda.go.jp/go/pack/2499415G1024_1_07/. Accessed 20 Jul 2021.
Raccah D, Chou E, Colagiuri S, et al. A global study of the unmet need for glycemic control and predictor factors among patients with type 2 diabetes mellitus who have achieved optimal fasting plasma glucose control on basal insulin. Diabetes Metab Res Rev. 2017;33:3.
An Z, Prigeon RL, D’Alessio DA. Improved glycemic control enhances the incretin effect in patients with type 2 diabetes. J Clin Endocrinol Metab. 2013;98(12):4702–8.
Vora J. Combining incretin-based therapies with insulin: realizing the potential in type 2 diabetes. Diabetes Care. 2013;36(Suppl 2):S226–32.
Polonsky WH, Henry RR. Poor medication adherence in type 2 diabetes: recognizing the scope of the problem and its key contributors. Patient Prefer Adherence. 2016;10:1299–307.
Bodmer M, Meier C, Krähenbühl S, Jick SS, Meier CR. Metformin, sulfonylureas, or other antidiabetes drugs and the risk of lactic acidosis or hypoglycemia: a nested case-control analysis. Diabetes Care. 2008;31(11):2086–91.
Leon N, LaCoursiere R, Yarosh D, Patel RS. Lixisenatide (Adlyxin): a once-daily incretin mimetic injection for type-2 diabetes. P T. 2017;42(11):676–711.
McCarty D, Coleman M, Boland CL. Lixisenatide: a new daily GLP-1 agonist for type 2 diabetes management. Ann Pharmacother. 2017;51(5):401–9.
Watada H, Takami A, Spranger R, Amano A, Hashimoto Y, Niemoeller E. Efficacy and safety of 1:1 fixed-ratio combination of insulin glargine and lixisenatide versus lixisenatide in Japanese patients with type 2 diabetes inadequately controlled on oral antidiabetic drugs: the LixiLan JP-O1 randomized clinical trial. Diabetes Care. 2020;43(6):1249–57.
Lachin JM. Fallacies of last observation carried forward analyses. Clin Trials. 2016;13(2):161–8.
Acknowledgements
Funding
This study was funded by Sanofi K.K., including the journal’s Rapid Service Fee and open access fee associated with publication.
Medical Writing and Editorial Assistance
Editorial assistance in the preparation of this article was provided by Jo Dalton on behalf of inScience Communications, Springer Healthcare, who drafted the outline and by Tracy Harrison of inScience Communications, Springer Healthcare, who wrote the first draft of this manuscript. Support for this assistance was funded by Sanofi K.K. Assistance in data analysis was provided by Intage Healthcare Inc., Japan.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the study conception and design, performed some of the data analyses, and read, critically evaluated, and approved all drafts. Data acquisition was performed by Yoko Takahashi. All authors have read, critically evaluated and approved the final manuscript for submission.
Prior Presentations
These data have been previously presented at the 64th Annual Meeting of the Japan Diabetes Society (May 20–22, 2021; Toyama, Japan), in presentations titled “In combination with basal insulin in lixisenatide treatment, effect of timing on glycemic control: Subanalysis of post-marketing surveillance” (by Kaneto, H. Takahashi, Y, Ozaki A and Baxter M.), and “Effect of medication adherence and number of injections on glycemic control: Subgroup analysis of post-marketing surveillance of lixisenatide” (by Baxter M, Takahashi Y, Ozaki A and Terauchi Y).
Disclosures
Hideaki Kaneto has received honoraria for lectures, scholarship grants, and research grants from Novo Nordisk Pharma, Sanofi, Eli Lilly, Boehringer Ingelheim, Taisho Pharma, Sumitomo Dainippon Pharma, Takeda Pharma, Ono Pharma, Daiichi Sankyo, Mitsubishi Tanabe Pharma, Kissei Pharma, MSD, AstraZeneca, Astellas, Novartis, and Kowa. Mike Baxter was a full-time employee of Sanofi UK and affiliated with Swansea University, Swansea, Wales, UK at the time that the study was conducted; he is currently affiliated with Ashford and St Peter's Hospitals NHS Foundation Trust, Surrey and Swansea University, Swansea, Wales, UK. He declares no other competing interests. Yoko Takahashi is an employee of Sanofi K.K. Yasuo Terauchi has received honoraria for serving on advisory boards for MSD, Boehringer Ingelheim, Tanabe-Mitsubishi, Daiichi Sankyo, Novo Nordisk, Eli Lilly, Sanofi, Astellas Pharma, and AstraZeneca; honoraria for lectures from MSD, Ono, Boehringer Ingelheim, Takeda, Tanabe-Mitsubishi, Daiichi Sankyo, Sanwa Kagaku Kenkyusho, Novo Nordisk, Eli Lilly, Sanofi, Dainippon-Sumitomo, Shionogi, Bayer Yakuhin, Astellas and AstraZeneca; and research funding from MSD, Ono, Boehringer Ingelheim, Novartis, Takeda, Daiichi Sankyo, Novo Nordisk, Eli Lilly, Sanofi, and Dainippon-Sumitomo.
Compliance with Ethics Guidelines
The study was conducted in accordance with the Japanese Ministerial Ordinance on Good Post-Marketing Study Practice (Ministry of Health, Labour and Welfare Ordinance No. 171, December 20, 2004) and the ethical guidelines for medical and health research involving human subjects. Under the Japanese regulations for PMS studies, requirement to conform with the Declaration of Helsinki was not applicable and there was no requirement for review or approval by the ethics committee of the participating medical institutions nor for collection of informed consent from study participants. All data were collected anonymously to protect personal information; the study sponsor had no access to individual participant medical records.
Data Availability
The dataset generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kaneto, H., Baxter, M., Takahashi, Y. et al. Simultaneous Versus Sequential Initiation of Lixisenatide and Basal Insulin for Type 2 Diabetes: Subgroup Analysis of a Japanese Post-Marketing Surveillance Study of Lixisenatide (PRANDIAL). Adv Ther 39, 5453–5473 (2022). https://doi.org/10.1007/s12325-022-02311-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02311-1