Abstract
Introduction
Smoking prevalence is twice as high among patients admitted to hospital because of the acute condition of aneurysmal subarachnoid hemorrhage (aSAH) as in the general population. Smoking cessation may improve the prognosis of aSAH, but nicotine replacement therapy (NRT) administered at the time of aSAH remains controversial because of potential adverse effects such as cerebral vasospasm. We investigated the international practice of NRT use for aSAH among neurosurgeons.
Methods
The online SurveyMonkey software was used to administer a 15-question, 5-min online questionnaire. An invitation link was sent to those 1425 of 1988 members of the European Association of Neurosurgical Societies (EANS) who agreed to participate in surveys to assess treatment strategies for withdrawal of tobacco smoking during aSAH. Factors contributing to physicians’ posture towards NRT were assessed.
Results
A total of 158 physicians from 50 nations participated in the survey (response rate 11.1%); 68.4% (108) were affiliated with university hospitals and 67.7% (107) practiced at high-volume neurovascular centers with at least 30 treated aSAH cases per year. Overall, 55.7% (88) of physicians offered NRT to smokers with aSAH, 22.1% (35) offered non-NRT support including non-nicotine medication and counselling, while the remaining 22.1% (35) did not actively support smoking cessation. When smoking was not possible, 42.4% (67) of physicians expected better clinical outcomes when prescribing NRT instead of nicotine deprivation, 36.1% (57) were uncertain, 13.9% (22) assumed unaffected outcomes, and 7.6% (12) assumed worse outcomes. Only 22.8% (36) physicians had access to a local smoking cessation team in their practice, of whom half expected better outcomes with NRT as compared to deprivation.
Conclusions
A small majority of the surveyed physicians of the EANS offered NRT to support smoking cessation in hospitalized patients with aSAH. However, less than half believed that NRT could positively impact clinical outcome as compared to deprivation. This survey demonstrated the lack of consensus regarding use of NRT for hospitalized smokers with aSAH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A small majority of the surveyed physicians of the European Association of Neurosurgical Societies (EANS) offered nicotine replacement therapy (NRT) to support smoking cessation in patients admitted to hospital because of the acute condition of aneurysmal subarachnoid hemorrhage (aSAH). | |
Physicians from the surveyed high-volume neurovascular centers were more experienced with combined NRT regimes and tended to expect a beneficial effect of NRT. | |
Those who did not routinely support smoking cessation were rather uncertain about the clinical outcome of NRT. | |
There is no established consensus guideline to manage tobacco withdrawal during aSAH. |
Introduction
Smoking is one of the most important risk factors of cardiovascular disease [1, 2]. Compared to non-smokers, smokers had higher risks of cerebral aneurysm formation [3], rupture [4, 5], and vasospasm [6], and inferior survival rates [7,8,9] when admitted to hospital because of the acute condition of aneurysmal subarachnoid hemorrhage (aSAH). Globally, 37.1–62% of patients hospitalized with aSAH are active smokers, compared to 22% in the general population [10,11,12,13].
Among aSAH survivors, active cigarette smoking may be the most important modifiable risk factor for mortality [9]. Smoking cessation may reduce the severity of aSAH and improves long-term prognosis [9, 14,15,16,17,18]. Thus, smoking cessation counseling for hospitalized smokers with aSAH with use of nicotine replacement therapy (NRT) has been recommended in a number of intensive care units worldwide, such as in the USA [19,20,21,22], the Netherlands [23], and Australia and New Zealand [24]. However, in the absence of clinical trials, there is no established consensus guideline to manage tobacco withdrawal during aSAH. As such, administration of NRT remains controversial because of concerns of potential side effects including cerebral vasospasm [12, 25,26,27,28]. The Swiss agency for therapeutic products identified stroke as a precaution to the use of NRT. They advised that addicted smokers, who suffered a recent stroke should be encouraged to quit smoking through non-pharmacological means while reserving NRT for situations which are refractory to counseling alone. In addition, two recently published observational studies of patients with aSAH reported better clinical outcomes among smokers compared to non-smokers giving birth to the smokers’ paradox [11, 29, 30], which was attributable to neuroprotective properties of nicotine [11]. However, this hypothesis was revised after the inclusion of patients with sudden death after aSAH who never reached hospital [7].
In this controversial context, Turgeon et al. conducted a survey in 2017 that included 14 neurosurgeons from Canada [12]. Six of them reported to sometimes order NRT in aSAH. We wanted to assess whether use of NRT during aSAH is internationally applied and to what extent this practice is standardized. Therefore, we conducted a worldwide survey among the physicians of the European Association of Neurosurgical Societies (EANS), in order to assess the attitudes and treatment strategies concerning withdrawal of tobacco smoking during aSAH.
Methods
Recruitment and Survey
The study was a survey of physicians of the EANS community, working in 50 European and non-European countries. The questionnaire consisted of 15 standardized questions. To assess acceptability of the survey, we conducted a test with four eligible physicians, who were subsequently excluded from the survey. We used a single-staged sample via the MailChimp (Ponce City Market, Atlanta, GA, USA) electronic mail distribution software to track access. Included was a quick response (QR)-Code and the link, leading to the SurveyMonkey (Inc., San Mateo, CA, USA) questionnaire. One reminder email was sent once for those who did not respond 10 days after the first email. The number of unique visitors was provided by the email distribution software. Multiple participation was checked through correlation of the geographical location of the transferred Internet Protocol (IP) address with the corresponding designated country of employment. There were no cases of double or multiple participation.
Only the completed questionnaires of invited responders between August 29, 2018 and August 29, 2019 were included in this final analysis. The datasets generated or analyzed during the current study are available from the corresponding author on reasonable request. The authors confirm that the study obtained consent from all study participants to participate in the survey/study and also consent for their responses/survey results to be published. The survey/study participants are aware that the results of the study would be published.
All participating physicians consented to receive emails with requests for surveys. They were additionally informed in the email invitation on the study and subsequent studies and that it focuses on patients with intracranial aneurysms and aneurysmal subarachnoid hemorrhage and that the data will only be used confidentially and anonymously.
In human research, a distinction is drawn in Switzerland between projects that require authorization and those that do not. This study qualifies as anonymized research, because the data was sent via an online question tool and no one can trace who has given the answers. This study is not research involving patients, embryos, etc. and is therefore a project that does not comply with the Human Research Act (HRA) because it is anonymous research (https://www.fedlex.admin.ch/eli/cc/2013/617/en). Anonymous research is neither reviewed nor approved by a local ethics commission. This study did not qualify for ethics approval; however, approval was granted by the Scientific Liaison of the EANS Board.
Smoking Cessation and NRT
Support for smoking cessation was defined as any stated medical action to mitigate withdrawal that was sometimes or routinely offered, including NRT, non-nicotine medication, and verbal support. Verbal support was defined as psychological or educational counseling. NRT was defined as the substitution of nicotine-containing pharmacological products during smoking cessation. Non-nicotine medication to support smoking cessation was defined as non-nicotine-containing pharmacological products. Non-NRT support was defined as verbal support including psychological support, educational support or counselling, or non-nicotine-containing pharmacological products such as bupropion or varenicline.
Two non-nicotine-containing pharmacological products were specifically included in the questionnaire. Varenicline has both agonistic and antagonistic properties at the nicotinic receptor. Bupropion is a nicotinic receptor antagonist. Bupropion is also a selective norepinephrine and dopamine reuptake inhibitor and serves as an option for management of nicotine withdrawal [31]. Physicians who “never offered any support for smoking cessation” were defined as physicians who did not offer support for smoking cessation for smokers who suffered aSAH. Physicians that “would offer NRT” were defined as those physicians who specified at least one product of NRT that they would offer to support smoking cessation during aSAH. Physicians who “would not offer NRT” were defined as those physicians who reported that they would not offer NRT to support smoking cessation. Tobacco withdrawal was defined by the physical and psychological effects a person experiences when attempting to cease tobacco smoking.
Covariates
The definition of caseload was based on the number of annual aSAH cases at each physician’s practicing centers. High volume was defined as an annual caseload of at least 30 cases and low volume as fewer than 30 [12, 32]. Level of practice was defined by the level of training of the surveyed physicians that were classified as residents, consultants, and senior physicians. Health economic data was collected for the year 2018, and if not available, the most recent year’s data was used. Data was compared to the average value from the Organisation for Economic Co-operation and Development (OECD) [33,34,35]. The data is reported as percentage (number).
Data Analysis and Statistical Methodology
Stratified analysis was done for physicians practicing at high-volume and low-volume neurovascular centers, to assess the influence of caseload on NRT prescription [36, 37]. To assess geographic variation in practice, each responding physician was assigned to the respective country in which they practiced. Similarly, a stratified analysis according to the health economic situation of each country was performed. Correlation analysis was performed for each country accounting for physicians who offered NRT and the average national health expenditure per capita above or below OECD average. An association between OECD average costs of national health care systems and the predisposition to offer NRT after aSAH was graphically represented.
The number of samples, the right-tailed probability of the chi-squared distribution, and type of test statistic tests were indicated. The p value was reported with a statistical level of significance of less than 0.05. Data was analyzed using the SPSS software (IBM SPSS Statistics 25; Armonk, New York, USA).
Results
Sample Population
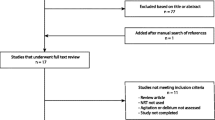
The EANS membership during the period of sampling from August 29, 2018 to August 29, 2019 consisted of 1367 individual members from 38 European countries and 621 members of 67 countries outside Europe. A total of 1425 physicians agreed to participate in surveys and were contacted by email; 188 unique visitors opened the survey link (click rate 13%) and 158 completed the survey (response rate 11%) (Fig. 1).
European physicians were the most represented group with 74.7 (118) respondents working in 27 nations. Overall responses were available for physicians from 50 countries including three in Africa, two in North America, four in Central and South America, 10 in Asia, and 27 in Europe; 22.8% (36) physicians practiced in 19 non-European countries. The remaining 2.5% (4) physicians practiced in countries that were considered Eurasian, namely Cyprus, Georgia, Russian Federation, and Turkey.
Of the responding physicians, 30.4% (48) were residents, 32.9% (52) consultants, and 36.7% (58) senior physicians consisting of 15.8% (25) senior consultants and 20.8% (33) chief physicians.
Management of Smoking Cessation
Of 158 physicians, 81.6% (129) routinely enquired about tobacco consumption when treating patients with aSAH; 51.2% (81) routinely enquired about cumulative pack-years (Fig. 2). Overall 60.1% (95) of 158 physicians offered support for smoking cessation to smokers with aSAH, out of which 65.3% (62) stated that they would offer NRT, whereas 34.7% (33) would not offer NRT (Fig. 3). Among the 62 physicians who offered NRT, 12.9% (8) additionally offered non-NRT; and among the 33 physicians who would not offer NRT, 18.2% (6) would offer non-NRT [(χ2 (1, N = 14) = 3.84, p = 0.52].
Management of smoking cessation. Percentage (n) of n = 158 physicians who would have (a) asked patients with aSAH about tobacco-smoking habits. (b) Asked patients with aSAH about the desire to quit smoking. (c) Offered support for smoking cessation to patients with aSAH. (d) Offered NRT for a patient with aSAH who smokes during the hospital stay and wishes to stop smoking. (e) Offered NRT for a patient with aSAH who wants to stop smoking and who gave written consent for NRT knowing about the “warnings and precautions”. (f) Offered NRT for a patient with aSAH, who is confused, has delirium, and expresses the wish for either NRT or smoking tobacco. *The answer “routinely” corresponds in the patient cases (d), (e), and (f) to support voluntary/intentional tobacco cessation, the answer “never” corresponds in the same cases to forced tobacco withdrawal due to hospitalization. aSAH patients admitted to hospital because of the acute condition of aneurysmal subarachnoid hemorrhage, NRT nicotine replacement therapy
Support of smoking cessation or NRT for patients with aSAH among physicians of the EANS. The lower part depicts the surveyed physicians’ expected clinical outcome of hospitalized smokers with aSAH when using NRT compared to deprivation. *Indicates a significant difference between the physicians who offer NRT or do not offer NRT. aSAH patients admitted to hospital because of the acute condition of aneurysmal subarachnoid hemorrhage, EANS European Association of Neurosurgical Societies, NRT nicotine replacement therapy
Out of the 39.8% (63) of 158 physicians who did not offer support for smoking cessation for smokers with aSAH, 41% (26) would consider offering NRT for smokers with aSAH. Overall, 88 of 158 (56%) physicians offered NRT to smokers with aSAH as depicted in Fig. 3. Figure 3 also reflects the expected impact of NRT during aSAH on clinical outcome. There was a significant difference in the expected better outcome with NRT [54.5% (n = 48 of 88) vs. 27.1% (n = 19 of 70)] and in the expected uncertain outcome with NRT [29.5% (n = 26 of 88) vs. 44.3% (n = 31 of 70)] according to the predisposition to offer NRT [χ2 (1, N = 67) = 20.8, p < 0.00001 and χ2 (1, N = 57) = 6, p = 0.01, respectively]. The subgroup of physicians that expected better outcome differed significantly from the physicians that expected unchanged outcome with NRT [11.4% (n = 10 of 88) and 17.1% (n = 12 of 70)] and those who expected worse outcome with NRT [4.5% (n = 4 of 88) and 11.4% (n = 8 of 70)] according to the predisposition to offer NRT [χ2 (1, N = 22) = 7.42, p = 0.006 and χ2 (1, N = 12) = 8.7, p = 0.003, respectively].
Stratified Analysis
A total of 78 physicians were practicing in 14 nations with health expenditure per capita above the OECD average of 2018, and 80 physicians were practicing in 36 countries with health expenditure per capita below the OECD average [33,34,35]. Of the 78 physicians practicing in a nation with health expenditure per capita above OECD average, 66.7% (52) offered NRT, as compared to 45% (36) of 80 physicians practicing in a nation with health expenditure per capita below the OECD average [χ2 (1, N = 80) = 16.9, p < 0.0001].
Overall 67.7% (107) of physicians were practicing in high-volume neurovascular centers and 32.3% (51) were practicing in low-volume neurovascular centers. Use of NRT by the volume of neurovascular centers is reported in Table 1. Of the 107 physicians from high-volume neurovascular centers, 23.4% (25) offered support for smoking cessation routinely compared with 9.8% (5) of 51 physicians from low-volume neurovascular centers [χ2 (1, N = 30) = 4.84, p = 0.03].
Type of NRT
The most frequently used NRT product was a nicotine patch, which was preferred by 43% (68) of all physicians. Practice was heterogenous in that NRT was offered as monotherapy or in combination with other NRT products or non-nicotine medication as depicted in Table 2. In case of no routine smoking cessation support, both “nicotine chewing gum” with 28.1% (n = 36 of 128) and “non-nicotinic medication only” with 5.4% (n = 7 of 128) were the only means of support that were more frequently offered compared to routine smoking cessation support with 20% (n = 6 of 30) and 3.3% (1 of 30), respectively. All other forms of NRT products, as well as varenicline and bupropion and verbal support were most frequently offered by physicians who supported smoking cessation routinely and were employed in high-volume neurovascular centers.
Case-Specific NRT
For a patient who is aware of warnings and precautions of NRT use after a cerebrovascular event and gives written informed consent to NRT, 61.4% (97) of the surveyed physicians would have prescribed NRT (Fig. 2). For a patient in the acute phase of aSAH who is confused, has delirium, and expresses the wish for either NRT or smoking tobacco, 53.2% (84) physicians would have allowed NRT, 38.6% (61) would have forbidden both tobacco smoking and NRT, and 8.2% (13) would have allowed smoking tobacco. None of the last 13 physicians expected a worse clinical outcome with NRT compared to deprivation. The physician’s willingness to prescribe NRT was more pronounced in patients who gave written consent compared to delirious patients [χ2 (1, N = 158) = 4.36, p = 0.04].
Smoking Cessation Team
Overall 22.8% (36) of the physicians had access to a smoking cessation team in their hospital, 63.9% (101) stated there was no such team available in their hospital, while 13.3% (21) had no knowledge of such a team. Overall, 55.1% (87) thought that a smoking cessation intervention during aSAH was more successful compared to a smoking cessation intervention after discharge. Of the 12 physicians who expected a worse clinical outcome with NRT, 12 did not have access to or were unaware of a smoking cessation team. Of the 36 physicians who had access to a smoking cessation team in their hospital, 50% reported to expect a better clinical outcome with NRT, 16.6% (6) expected unaffected outcome, and 33.3% (12) were uncertain about the impact of NRT on outcome. None expected a worse clinical outcome. There was a significant difference in the expected worse clinical outcome according to access to a local smoking cessation team (0% (0 of 36) with access vs. 11% (12 of 101) without, [χ2 (1, N = 12) = 3.93, p = 0.04].
Discussion
Among surveyed physicians of the EANS working worldwide, about half offered NRT routinely to support smoking cessation in hospitalized patients with aSAH, although a majority of them enquired about tobacco consumption. Offering NRT correlated with the physician’s predisposition to support smoking cessation, independently of the methods of support. Physicians who would not offer NRT managed tobacco withdrawal with no specified care or, equally frequently, with non-NRT support, which consisted predominantly of verbal support and to a lesser degree of non-nicotinic medication. Physicians working in high-volume neurovascular centers offered NRT more regularly and with a more comprehensive range of various nicotinic and non-nicotinic products, compared to those of low-volume neurovascular centers. Physicians with a workplace in a country with national health expenditure per capita above the OECD average offered NRT more often as well.
Current approaches for smokers with aSAH include three options: (I) smoking cessation with NRT to mitigate tobacco withdrawal; (II) smoking cessation without NRT, with or without non-nicotine medication; and (III) continued smoking. Physicians treating smokers with aSAH face the challenge of nicotine withdrawal on a daily basis. Often such cases are discussed individually and the treating physicians finally decide for option (I), (II), or (III) and derive personal experiences from it. Despite this regular clinical issue, only a few studies have weighed NRT vs. tobacco withdrawal [25,26,27, 38]. These studies evaluated several outcomes including duration of hospitalization, duration of neurosurgery intensive care stay, occurrence of vasospasm, delayed cerebral ischemia, delirium, use of antipsychotic medication or physical restraint, 30-day mortality, 3-month mortality, or other medical complications. None of these published studies were randomized controlled trials. Therefore, many expert reviews underlined the low level of evidence for or against NRT in aSAH and expressed the need for randomized controlled trials for more robust recommendations [12, 23, 28, 39, 40]. Our survey found that physicians who offered NRT expected a better clinical outcome than those who have not offered NRT. Furthermore, uncertainty about the outcome when using NRT for aSAH was higher among physicians who would not offer NRT.
The reluctance of using NRT during aSAH may be explained by concerns that nicotine products might induce vasospasm [12, 26, 41]. Despite this, only 12 of the reported physicians (8%) expected a poor outcome from NRT (Fig. 3). Among them, there was on the one hand none who knew about a smoking cessation team in the respective clinic. On the other hand, none of the 36/158 physician with access to a local smoking cessation team reported to assume worse outcome. Access to a smoking cessation team therefore seemed to promote the expectation of a favorable outcome. Overall, only 8.2% (13) of physicians, mainly senior physicians, favored continued smoking (Fig. 2). None of these physicians expected a worse clinical outcome with NRT compared to deprivation. It seemed therefore as if they did not fear the adverse effects of NRT, but rather the adverse effects of tobacco withdrawal. Continued smoking may be justified by reports of the smokers’ paradox [11, 13, 30]. Better outcomes were thereby reported for smokers compared to nonsmokers after aSAH and had been attributed to potentially neuroprotective properties of nicotine [13, 30, 42]. However, in contrast to these studies, other authors reported worse outcomes for smokers after aSAH, as compared to nonsmokers [6, 9]. These paradoxical results may be explained by exclusion of patients with sudden death after aSAH who never reached a hospital [7]. Overall, the proven benefits of smoking cessation on neoplastic, vascular, respiratory, and other diseases ultimately outweighed the risks of continued smoking after aSAH [1, 7, 9, 43].
Furthermore, the National Institute for Health and Care Excellence (NICE) guidelines from England note that smoking can be a risk factor for an initial subarachnoid haemorrhage [caused by a ruptured aneurysm]. They agreed that smoking cessation interventions, in addition to benefiting general health, may also reduce the risk of recurrent subarachnoid haemorrhage [44].
Concerning the general population, reducing tobacco consumption is essential for both improving the population’s health and reducing health care costs [45]. For these reasons the guidelines recommend that clinicians advise all smokers to stop using tobacco and provide behavioral interventions and pharmacotherapy [46]. Behavioral interventions and pharmacotherapy during the hospital stay with a supportive contact after discharge significantly increase smoking cessation [46, 47]. A systematic review of the literature on NRT in patients with aneurysmal subarachnoid hemorrhage concludes that clinicians may consider use of NRT in smokers hospitalized for aSAH who present with signs of nicotine withdrawal, or who are stable for discharge [12].
The current clinical practice of initiating a brief intervention in case of aSAH is also recommended in the NICE guidelines [44]. In line with this, the majority 81.6% (129) of the surveyed physicians routinely initiated the brief intervention by asking the smoking status and 60.1% (95) assisted smoking cessation. The surveilled physicians have gradually taken less account of the further steps of the brief intervention as depicted in Fig. 2. Optimally, all patients with aSAH need a brief intervention; however, not all patients who smoke need pharmacotherapy.
The controversy in offering NRT for smoking cessation to patients with aSAH reflects that there are guidelines such as the NICE guidelines [44], but these are not uniformly applied by clinicians. Slettebø et al. stated that NRT had been very uncommon at the Department of Neurosurgery of the Oslo University Hospital in Norway in the year 2011 [13].
Turgeon et al. surveyed high-volume neurovascular surgeons from Canada regarding NRT in hospitalized patients with aSAH [12]. Eight of 14 responders (57%) reported to follow “local standard of care” as a rationale to offer NRT. Local standard of care had prompted half of these physicians to never offer NRT, whereas the other half offered NRT sometimes. Another four of these 14 surveyed physicians (29%) reported “training” and merely two (14%) reported “evidence” as a rationale to consider NRT. About half of the responders in that survey offered NRT. In our international study, we found comparable results, which corroborates the external validity of the compiled data on administering NRT in smokers with aSAH. Our study moreover identified previously unreported sources of physician’s confidence in offering NRT: previous experience with any kind of smoking cessation support, access to a smoking cessation care team, and a workplace in a high-volume neurovascular center or in a country with comparatively high per capita health care expenditure.
Some limitations apply to our study. Physicians had been assured anonymity before participating in the survey, which could have affected response rates and answers. The response rate was 11% and only EANS members were included. While the response rate appears to be in the lower range of comparable studies with 6.5–40%, it is not sufficient to be generalizable [12, 48]. European physicians were the most represented group with 118 (75%) respondents working in 27 countries. This precludes generalizations about the entire EANS membership and the sample may not be representative of the international population and thus limits the external validity of the study. The personal smoking history of the surveyed physicians is a potential confounder that was not assessed in this survey, while previous findings on this are controversial. Pipe et al., on the one hand, found that physicians who smoke were less likely to initiate a smoking cessation intervention with their patients than nonsmoking physicians were [49]. Shields et al., on the other hand, found that physicians who smoke were more likely to offer a test to tailor their patients’ treatment for smoking cessation [50]. We furthermore compared the smoking prevalence by nation [51] as a potential confounder with the rate of surveyed physicians who offered nicotine replacement therapy during aSAH. There seemed to be no relevant association between estimated national smoking prevalence and the rate of physicians who offered NRT during aSAH [χ2 (1, N = 50) = 3.84, p = 0.57].
Our results may be also subject to sample size bias, as some of the analyzed subgroups differed relevantly in size.
However, we believe our study can still provide a global overview of current clinical practice regarding use of NRT for smoking withdrawal among patients with aSAH.
Conclusions
Evidence-based recommendations for NRT administration are limited for patients admitted to hospital because of aSAH. In a worldwide survey, we reported that the majority of the responding physicians offered NRT to support smoking cessation in case of aSAH. However, this practice varied significantly between geographic territories. Most of the physicians from high-volume neurovascular centers were more experienced with combined NRT regimes and tended to expect a beneficial effect of NRT. Those who did not routinely support smoking cessation were more hesitant to offer combinations of NRT and non-nicotinic medication and rather uncertain about the clinical outcome of NRT.
References
Duncan MS, Freiberg MS, Greevy RA, et al. Association of smoking cessation with subsequent risk of cardiovascular disease. JAMA. 2019;322(7):642–50.
Erhardt L. Cigarette smoking: an undertreated risk factor for cardiovascular disease. Atherosclerosis. 2009;205(1):23–32.
Schatlo B, Gautschi OP, Friedrich CM, et al. Association of single and multiple aneurysms with tobacco abuse: an @neurIST risk analysis. Neurosurg Focus. 2019;47(1):E9.
Juvela S. Natural history of unruptured intracranial aneurysms: risks for aneurysm formation, growth, and rupture. In: Yonekawa Y, Sakurai Y, Keller E, Tsukahara T, editors. New trends in cerebral aneurysm management, vol 82. Vienna: Springer; 2002. p. 27–30.
Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006;354(4):387–96.
Weir BK, Kongable GL, Kassell NF, et al. Cigarette smoking as a cause of aneurysmal subarachnoid hemorrhage and risk for vasospasm: a report of the Cooperative Aneurysm Study. J Neurosurg. 1998;89(3):405–11.
Lindbohm JV, Kaprio J, Korja M. Survival bias explains improved survival in smokers and hypertensive individuals after aSAH. Neurology. 2019;93(23):e2105–9.
Futchko J, Starr J, Lau D, et al. Influence of smoking on aneurysm recurrence after endovascular treatment of cerebrovascular aneurysms. J Neurosurg. 2018;128(4):992–8.
Korja M, Silventoinen K, Laatikainen T, et al. Cause-specific mortality of 1-year survivors of subarachnoid hemorrhage. Neurology. 2013;80(5):481–6.
Tobacco smoking. 2016. Data retrieved on Aug 18, 2021. https://apps.who.int/gho/data/node.sdg.3-a-viz?lang=en.
Dasenbrock HH, Rudy RF, Lai PMR, et al. Cigarette smoking and outcomes after aneurysmal subarachnoid hemorrhage: a nationwide analysis. J Neurosurg. 2018;129(2):446–57.
Turgeon RD, Chang SJ, Dandurand C, et al. Nicotine replacement therapy in patients with aneurysmal subarachnoid hemorrhage: systematic review of the literature, and survey of Canadian practice. J Clin Neurosci. 2017;42:48–53.
Slettebø H, Karic T, Sorteberg A. Impact of smoking on course and outcome of aneurysmal subarachnoid hemorrhage. Acta Neurochir. 2020;162(12):3117–28. https://doi.org/10.1007/s00701-020-04506-3.
Korja M, Lehto H, Juvela S, et al. Incidence of subarachnoid hemorrhage is decreasing together with decreasing smoking rates. Neurology. 2016;87(11):1118–23.
Etminan N, Chang H-S, Hackenberg K, et al. Worldwide incidence of aneurysmal subarachnoid hemorrhage according to region, time period, blood pressure, and smoking prevalence in the population: a systematic review and meta-analysis. JAMA Neurol. 2019;76(5):588–97.
Connolly ES Jr, Poisik A, Winfree CJ, et al. Cigarette smoking and the development and rupture of cerebral aneurysms in a mixed race population: implications for population screening and smoking cessation. J Stroke Cerebrovasc Dis. 1999;8(4):248–53.
Woo D, Khoury J, Haverbusch M, et al. Smoking and family history and risk of aneurysmal subarachnoid hemorrhage. Neurology. 2009;72(1):69–72.
Bor ASE, Rinkel GJ, van Norden J, et al. Long-term, serial screening for intracranial aneurysms in individuals with a family history of aneurysmal subarachnoid haemorrhage: a cohort study. Lancet Neurol. 2014;13(4):385–92.
Mayer SA, Chong JY, Ridgway E, et al. Delirium from nicotine withdrawal in neuro-ICU patients. Neurology. 2001;57(3):551–3. https://doi.org/10.1212/wnl.57.3.551.
Stefan MS, Pack Q, Shieh M-S, et al. The association of nicotine replacement therapy with outcomes among smokers hospitalized for a major surgical procedure. Chest. 2020;157(5):1354–61.
Rincon F. Neurologic: traumatic and non-traumatic. In: Dries DJ, Zanotti-Cavazzoni SL, Latenser BA, Martinez EA, Rincon F, Zwank MD, editors. Year Book of Critical Care Medicine 2012. Philadelphia; 2012. pp. 275–6.
Agarwal S, Dangayach N. Aneurysmal subarachnoid hemorrhage. In: Colosimo C, Gil-Nagel A, Gilhu NE, Rapoport A, Williams O, editors. Handbook of neurological therapy, chap. 8. Oxford: Oxford University Press; 2014. p. 85.
de Jong B, Schuppers AS, Kruisdijk-Gerritsen A, et al. The safety and efficacy of nicotine replacement therapy in the intensive care unit: a randomised controlled pilot study. Ann Intensive Care. 2018;8(1):70.
McGain F, Bates S, Meyer J, et al. Smoking cessation therapy in Australian and New Zealand intensive care units: a multicentre point prevalence study. Crit Care Resusc. 2018;20(1):68.
Panos NG, Tesoro EP, Kim KS, et al. Outcomes associated with transdermal nicotine replacement therapy in a neurosurgery intensive care unit. Am J Health Syst Pharm. 2010;67(16):1357–61.
Carandang RA, Barton B, Rordorf GA, et al. Nicotine replacement therapy after subarachnoid hemorrhage is not associated with increased vasospasm. Stroke. 2011;42(11):3080–6.
Seder DB, Schmidt JM, Badjatia N, et al. Transdermal nicotine replacement therapy in cigarette smokers with acute subarachnoid hemorrhage. Neurocrit Care. 2011;14(1):77–83.
Wilby KJ, Harder CK. Nicotine replacement therapy in the intensive care unit: a systematic review. J Intensive Care Med. 2014;29(1):22–30.
Western E, Sorteberg A, Brunborg C, et al. Prevalence and predictors of fatigue after aneurysmal subarachnoid hemorrhage. Acta Neurochir. 2020;162(12):3107–16.
Cockroft KM. A smoker’s paradox: does being a smoker really lead to a better outcome after aneurysmal SAH? J Neurosurg. 2017;129(2):442–5.
Motooka Y, Matsui T, Slaton RM, et al. Adverse events of smoking cessation treatments (nicotine replacement therapy and non-nicotine prescription medication) and electronic cigarettes in the Food and Drug Administration Adverse Event Reporting System, 2004–2016. SAGE Open Med. 2018;6:2050312118777953.
Hattori N, Katayama Y, Abe T. Case volume does not correlate with outcome after cerebral aneurysm clipping: a nationwide study in Japan. Neurol Med Chir. 2007;47(3):95–101.
OECD data—health spending per capita. https://data.oecd.org/healthres/health-spending.htm. 2018. Accessed 18 Aug 2020.
Current health expenditure per capita. https://data.worldbank.org/indicator/SH.XPD.CHEX.PP.CD. Accessed 18 Aug 2020.
Albania. https://www.who.int/countries/alb/en/. Accessed 23 July 2020.
Macdonald RL, Schweizer TA. Spontaneous subarachnoid haemorrhage. Lancet. 2017;389(10069):655–66.
Boogaarts HD, Amerongen MJV, Vries JD, et al. Caseload as a factor for outcome in aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. J Neurosurg JNS. 2014;120(3):605. https://doi.org/10.3171/2013.9.jns13640.
Lee H, Perry JJ, English SW, et al. Clinical prediction of delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage. J Neurosurg. 2018;130(6):1914–21.
Ng K, Gillies M, Griffith D. Effect of nicotine replacement therapy on mortality, delirium, and duration of therapy in critically ill smokers: a systematic review and meta-analysis. Anaesth Intensive Care. 2017;45(5):556–61.
Kerr A, McVey J, Wood A, et al. Safety of nicotine replacement therapy in critically ill smokers: a retrospective cohort study. Anaesth Intensive Care. 2016;44(6):758–61.
Jackson M. Cerebral arterial narrowing with nicotine patch. Lancet. 1993;342(8865):236–7.
Hammer A, Steiner A, Ranaie G, et al. Impact of comorbidities and smoking on the outcome in aneurysmal subarachnoid hemorrhage. Sci Rep. 2018;8(1):1–7.
Jha P, Ramasundarahettige C, Landsman V, et al. 21st-century hazards of smoking and benefits of cessation in the US. N Engl J Med. 2013;368(4):341–50. https://doi.org/10.1056/NEJMsa1211128.
National Institute for Health and Care Excellence. Guideline subarachnoid haemorrhage caused by a ruptured aneurysm: diagnosis and management. NICE guideline DRAFT 2021; February 2021.
Gilbert A, Cornuz J. Which are the most effective and cost-effective interventions for tobacco control? Copenhagen, WHO Regional Office for Europe. Health Evidence Network report; 2003. http://www.euro.who.int/document/e82993.pdf. Accessed 18 Aug 2021.
Krist AH, Davidson KW, Mangione CM, et al. Interventions for tobacco smoking cessation in adults, including pregnant persons: US preventive services task force recommendation statement. JAMA. 2021;325(3):265–79.
Rigotti NA, Clair C, Munafo MR, et al. Interventions for smoking cessation in hospitalised patients. Cochrane Datab Syst Rev. 2012;5(5):CD001837
Warren GW, Marshall JR, Cummings KM, et al. Addressing tobacco use in patients with cancer: a survey of American Society of Clinical Oncology members. J Oncol Pract. 2013;9(5):258–62.
Pipe A, Sorensen M, Reid R. Physician smoking status, attitudes toward smoking, and cessation advice to patients: an international survey. Patient Educ Couns. 2009;74(1):118–23. https://doi.org/10.1016/j.pec.2008.07.042.
Shields AE, Blumenthal D, Weiss KB, et al. Barriers to translating emerging genetic research on smoking into clinical practice: perspectives of primary care physicians. J Gen Intern Med. 2005;20(2):131–8.
Smoking rates by country 2018. 2018. https://worldpopulationreview.com/country-rankings/smoking-rates-by-country. Accessed 21 June 2022.
Acknowledgements
A special thank goes to the participants of the study. We thank the EANS and particularly the EANS office team including Amy Pinchbeck-Smith, Petra Koubova, and Beata Vasiliakova for distributing this survey to the EANS community. We would also like to thank Werner Z’Graggen from the Intermediate Care Unit and Nicole Söll, Department of Neurosurgery, University Hospital, Inselspital Bern as well as Coralie Wenger-Bonny, Center for Primary Care and Public Health, University of Lausanne, for review of earlier versions of the manuscript.
Funding
Open access funding provided by University of Lausanne. No funding was received for the study. The authors funded the journal’s Rapid Service Fee.
Author Contributions
David Nanchen: concept and design, critical comments, discussion. Bawarjan Schatlo: concept and design, critical comments. Jacques Cornuz: critical comments. Felice Burn: critical comments, discussion. Isabelle Jacot-Sadowski: concept and design, critical comments, discussion. Markus F. Oertel: design, critical comments, discussion. Philippe Herzog: statistical analysis, critical comments, discussion. Preci L. Hamilton: drafting the manuscript, critical comments, discussion. Christian V. Eisenring: drafting the manuscript, literature search, statistical analysis.
Disclosures
Christian V. Eisenring, Preci L. Hamilton, Philippe Herzog, Markus F. Oertel, Isabelle Jacot-Sadowski, Felice Burn, Jacques Cornuz, Bawarjan Schatlo, David Nanchen declare no conflict of interest.
Compliance with Ethics Guidelines
The authors confirm that the study obtained consent from all study participants to participate in the survey/study and also consent for their responses/survey results to be published. The survey/study participants are aware that the results of the study would be published.
All participating physicians consented to receive emails with requests for surveys. They were additionally informed in the email invitation on the study and subsequent studies and that it focuses on patients with intracranial aneurysms and aneurysmal subarachnoid hemorrhage and that the data will only be used confidentially and anonymously.
In human research, a distinction is drawn in Switzerland between projects that require authorization and those that do not. This study qualifies as anonymized research, because the data was sent via an online question tool and no one can trace who has given the answers. This study is not research involving patients, embryos, etc. and is therefore a project that does not comply with the Human Research Act (HRA) because it is anonymous research (https://www.fedlex.admin.ch/eli/cc/2013/617/en). Anonymous research is neither reviewed nor approved by a local ethics commission. This study did not qualify for ethics approval; however, approval was granted by the Scientific Liaison of the EANS Board.
Data Availability
The datasets generated or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Eisenring, C.V., Hamilton, P.L., Herzog, P. et al. Nicotine Replacement Therapy for Smokers with Acute Aneurysmal Subarachnoid Hemorrhage: An International Survey. Adv Ther 39, 5244–5258 (2022). https://doi.org/10.1007/s12325-022-02300-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02300-4