Abstract
Introduction
Treprostinil is a prostacyclin vasodilator widely used for the treatment of pulmonary arterial hypertension (PAH) and, in its inhaled form, for pulmonary hypertension associated with interstitial lung disease (PH-ILD). Treprostinil palmitil inhalation powder (TPIP) is a dry powder formulation of treprostinil palmitil (TP), an ester prodrug of treprostinil. TPIP is designed to provide sustained release of treprostinil in the lung over a prolonged period, potentially enabling a once-daily (QD) dosing regimen and significantly higher tolerated doses compared with currently available treprostinil formulations. This phase 1 study assessed the safety, tolerability, and pharmacokinetics of TP and treprostinil following single and multiple QD administrations of TPIP in healthy volunteers.
Methods
Healthy adults (aged 18–45 years) were randomized to receive single or multiple QD inhalation doses of TPIP. Participants in the single-dose phase received TPIP 112.5, 225, 450, or 675 µg (n = 6/dose) or placebo (n = 2). Participants in the multiple-dose phase received TPIP 225 µg QD for 7 days (n = 6), 112.5 µg QD for 4 days followed by 225 µg QD for 3 days (n = 6), or placebo for 7 days (n = 4).
Results
Overall, 41 of 42 participants (97.6%) completed the study. In the single-dose phase, 70.8% (n = 17/24) of TPIP-treated participants experienced a treatment-emergent adverse event (TEAE) vs 0% (n = 0/2) of placebo-treated participants; the most common TEAEs (≥ 20%) were cough (45.8%), dizziness (29.2%), and throat irritation (20.8%). In the multiple-dose phase, 83.3% (n = 10/12) of TPIP-treated participants experienced a TEAE vs 50.0% of placebo-treated participants (n = 2/4); the most common TEAEs were cough (58.3% TPIP vs 50.0% placebo), headache (50.0% vs 0%), nausea (33.3% vs 0%), chest discomfort (33.3% vs 0%), and dizziness (25.0% vs 0%). Most TEAEs were mild; only seven patients experienced a moderate TEAE, and no severe or serious TEAEs occurred. In the multiple-dose phase, participants whose doses were titrated from TPIP 112.5 µg QD to 225 µg QD experienced fewer TEAEs than those who received 225 µg QD at treatment initiation (66.7% vs 100.0%), and all TEAEs with dose titration were mild. After a single dose of TPIP, treprostinil elimination t1/2 was 8.67–11.6 h and exposure was dose proportional, with mean (CV%) Cmax 78.4–717 pg/mL (38.6–72.9%) and AUC0−∞ 1090–5480 pg·h/mL (11.5–30.0%). At steady state (TPIP 225 µg), the mean (CV%) of Cmax, Cmin, and AUCτ were 193–228 pg/mL (32.9–46.4%), 17.6–22.8 ng/mL (43.7–64.4%), and 1680–1820 pg·h/mL (28.7–36.6%), respectively. The elimination t1/2 was 6.84–8.82 h after repeat dosing. No steady-state accumulation was observed. Plasma concentrations of TP were below the limit of quantification (100 pg/mL) at all time points measured.
Conclusion
TPIP was well tolerated at the doses tested, and dose titration improved tolerability. Treprostinil pharmacokinetics were linear and supportive of a QD treatment regimen. These results support further development of TPIP in patients with PAH and PH-ILD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Treprostinil palmitil inhalation powder (TPIP), a treprostinil prodrug, was generally well tolerated in healthy adults. Adverse events were dose-related, and attenuated with uptitration in once-daily, multiple-dose administration |
Treprostinil pharmacokinetics showed both a much longer half-life and lower peak concentrations than currently available inhaled treprostinil formulations |
These findings support further evaluation of TPIP as a once-daily inhalation therapy in patients with pulmonary arterial hypertension and pulmonary hypertension associated with interstitial lung disease |
Introduction
Pulmonary arterial hypertension (PAH), a subtype of pulmonary hypertension associated with high morbidity and mortality rates, is a progressive disease characterized by high pulmonary arterial pressure due to occluded and/or constricted pulmonary vasculature that results in right-sided heart failure and death [1, 2]. Clinically, PAH is defined by a mean pulmonary arterial pressure (PAP) greater than 20 mmHg at rest in the setting of normal pulmonary arterial wedge pressure of at most 15 mmHg with pulmonary vascular resistance of at least 3 Wood units [3, 4]. On the molecular level, PAH is the result of an imbalance between vasodilatory and vasoconstrictive pathways, including nitric oxide, endothelin, and prostacyclins [5]. Although PAH is generally considered a rare disease, a recent systematic review of global national registries and databases found a wide range of the estimated incidence (1.5–32 patients per million) and prevalence (12.4–268 patients per million) of PAH in adults [2]. Patients with PAH typically present with nonspecific symptoms, including angina, fatigue, shortness of breath, and syncope [2].
Several targeted treatments for PAH are available, including endothelin receptor antagonists, phosphodiesterase type 5 inhibitors, prostaglandin receptor agonists, and soluble guanylate cyclase activators, all of which reduce PAP by increasing pulmonary vasodilation [1, 5]. Treprostinil, a vasodilatory tricyclic benzidine analogue of prostacyclin, is a prostaglandin receptor agonist and, along with epoprostenol, iloprost, and beraprost, it is one of the four prostacyclin analogues approved in various countries for the treatment of PAH [1]. Binding of treprostinil to various relaxant prostaglandin receptors (IP, EP2, EP4, and DP1 receptors) on the surface of smooth muscle cells activates adenylate cyclase to produce cyclic adenosine monophosphate, altering intracellular calcium levels and promoting vasodilation [1, 6, 7]. Nonclinical studies have also shown that treprostinil potentially inhibits remodeling of the pulmonary vasculature [6, 8]. Treprostinil is available in many countries for the treatment of PAH as an injection for intravenous or subcutaneous use (Remodulin) and in the USA as an inhalation solution (Tyvaso) and extended-release oral tablet (Orenitram). Treprostinil inhalation solution is also approved in the USA for the treatment of pulmonary hypertension associated with interstitial lung disease (PH-ILD). Treprostinil has proven to be efficacious but is rapidly eliminated from the circulation and requires either frequent administration or continuous infusion to maintain efficacy. With an elimination half-life (t1/2) of 26–54 min, treprostinil treatment requires frequent inhalation (e.g., four times per day) or continuous intravenous/subcutaneous infusion. Orally administered treprostinil has a more prolonged elimination, but still requires dosing 2–3 times per day [9]. In addition, high systemic levels of treprostinil are associated with dose-limiting adverse events (AEs) [10]. In patients with PAH, inhaled treprostinil is associated with headache, nausea, cough, throat irritation, flushing, and syncope [11,12,13,14].
Treprostinil palmitil (TP) is a hexadecyl ester prodrug of treprostinil. TP does not interact with prostanoid receptors and inflammatory mediators, but it is hydrolyzed slowly in the lung via endogenous esterases to form treprostinil [1, 10, 15, 16]. In rat and dog models of pulmonary hypertension, TP provided sustained treprostinil release in the lung and demonstrated prolonged reduction of pulmonary arterial pressures [15]. A phase 1 study of a previous formulation of TP (treprostinil palmitil inhalation suspension [TPIS]) confirmed fewer AEs compared with inhaled treprostinil at comparable doses [13, 17]. Following a single dose of TPIS 85, 170, or 340 µg, treprostinil exposure was dose proportional and the elimination t1/2 was 5.7–7.6 h. Participants in the 85 µg cohort also received a single dose of inhaled treprostinil 54 µg (equivalent dose to TPIS 85 µg), 24 h prior to TPIS dosing. Compared with inhaled treprostinil 54 µg, TPIS 85 µg produced approximately tenfold lower maximum observed plasma concentration (Cmax) (89 vs 958 pg/ml), similar area under the plasma concentration–time curve (AUC) (614 vs 872 ng·h/ml), and approximately tenfold longer elimination t1/2 (5.7 vs 0.49 h) [13, 17]. Treprostinil palmitil inhalation powder (TPIP), which was developed to improve convenience over TPIS, is in clinical development for PAH and PH-ILD.
In this phase 1 study, the safety, tolerability, and pharmacokinetics (PK) of single and multiple daily doses of TP delivered as TPIP were evaluated in healthy adults. TPIP doses for the study presented here were selected on the basis of safety, tolerability, and PK findings from the previous phase 1 study of TPIS administered to healthy adults [13, 18, 19].
Methods
Study Design
This was a randomized, double-blind, placebo-controlled, phase 1 study that was conducted sequentially in two parts, with two cohorts in each phase (four cohorts in total). The primary objective was to evaluate the safety and tolerability of single and multiple doses of TPIP, and the secondary objective was to evaluate the PK of TP and treprostinil in healthy volunteers. PPD Phase I Clinic (Austin, TX, USA) generated the randomization schedule, and each cohort was independently assigned by a qualified individual who was not involved in study conduct, data management, or data analysis. All participants entered the study after a 27-day screening period.
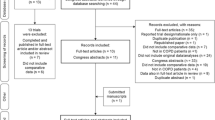
In the single-dose phase, the first cohort of participants was randomized 1:1:1 to receive an inhaled dose of TPIP (112.5 µg, 225 µg, or 450 µg), and the second cohort of participants was randomized 3:1 to receive TPIP 675 µg or placebo (Fig. 1). Participants were admitted to the clinic for 4 days, during which a single dose of assigned treatment was administered on day 1 followed by 3 days of assessments and observations. Safety data were collected for 72 h after dosing. A blinded safety review was conducted before dose escalation. On the basis of the review of safety data, the sponsor and investigator could have chosen to repeat a dose level, administer a dose higher or lower than the previous dose, escalate to a dose that was higher or lower than the next planned dose, and/or change the number of participants to be randomized to receive placebo. Participants were discharged on day 4 and contacted via telephone for a safety follow-up approximately 30 days after dosing.
Study design. All doses were administered using 112.5-μg single-actuation capsules. d day, PK pharmacokinetics, QD once daily, Scn screening, TPIP treprostinil palmitil inhalation powder. aBlood samples for PK assessments in the single-dose phase were collected within 15 min before dosing and at 0.25, 0.5, 1, 1.5, 2, 4, 6, 8, 10, 12, 24 (day 2), 36 (day 2), 48 (day 3), and 72 (day 4) hours after administration of TPIP or placebo; blood samples for PK assessments in the multiple-dose phase were collected within 30 min before dosing and at 0.25, 0.5, 1, 1.5, 2, 4, 6, 8, 10, and 12 h after dosing on day 1, before dosing only on days 2, 3, 4, 5, and 6, and before dosing on day 7 and 0.25, 0.5, 1, 1.5, 2, 4, 6, 8, 10, 12, 24 (day 8), 48 (day 9), and 72 (day 10) hours after day 7 dosing
In the multiple-dose phase, the first cohort of participants was randomized 3:1 to receive an inhaled dose of TPIP 225 µg once daily (QD) or placebo QD for 7 days. In the second cohort, participants were randomized 3:1 to receive TPIP 112.5 µg QD for 4 days followed by 225 µg QD for 3 days (titrated group) or placebo QD for 7 days (Fig. 1). Safety results from the two cohorts of participants in the single-dose phase were used to determine the titration step. Participants were admitted to the clinic for 10 days, during which daily doses of TPIP or placebo were administered for the first 7 days followed by 3 days of assessments and observations. Participants were discharged on day 10 and contacted via telephone for a safety follow-up approximately 30 days after the last dose.
The study was carried out in accordance with the ethical principles derived from international guidelines, including the Declaration of Helsinki and the Council for International Organizations of Medical Sciences International Ethical Guidelines, International Council for Harmonisation Good Clinical Practice Guideline, and applicable local regulatory requirements and laws. Before study entry, all participants provided written informed consent in compliance with US Title 21 Code of Federal Regulations, Part 50, which was submitted by the investigator to the institutional review board for the study site.
Participants
Healthy male and female nonsmokers aged 18 to 45 years who had a body mass index from 19.0 to 32.0 (calculated as weight in kilograms divided by height in meters squared) and no clinically significant abnormal findings from medical history, physical examination, vital sign measurements, 12-lead electrocardiogram, or clinical laboratory tests were eligible. Participants were excluded if they had a documented history of anaphylaxis or hypersensitivity to any drug including treprostinil and TPIP excipients, abnormal renal function (estimated glomerular filtration rate less than 60 mL/min/1.73 m2 by the Chronic Kidney Disease Epidemiology Collaboration equation), HIV infection, surgery requiring general anesthesia within 90 days, or malignancy within 5 years (excluding nonmelanoma skin cancer) before screening. Use of prescription medication (excluding hormonal birth control) or over-the-counter medications within 14 days of the first dosing day or throughout the study was not permitted. Concomitant medications deemed necessary for the welfare of the participant during the study were allowed at the investigator’s discretion. The complete list of inclusion and exclusion criteria are provided in Online Resource 1.
Study Drug Treatment
Dosing of TPIP (7.5 mg dry powder per capsule packaged in a single actuation capsule containing 112.5 µg TP) or matching placebo occurred after an overnight fast for at least 10 h. Water was permitted except for 1 h before and 1 h after study drug administration when serial PK samples were collected. Study drug was administered via an actuated device held by study staff. Participants performed up to two inhalations per capsule over a period up to 15 min and remained seated or standing for at least 1 h after dosing. Active drug and placebo were identical in appearance, and all participants within their cohort were dosed with the same number of capsules. When multiple dose levels were required, the number of capsules administered was determined by the number of capsules required to achieve the highest desired dose level, and other dose levels were achieved by an appropriate mix of active and placebo capsules. An unblinded pharmacist dispensed the capsules in a manner consistent with maintaining the blinding.
Safety Analyses
Safety was assessed via monitoring and recording of AEs (including treatment-emergent AEs [TEAEs] and serious AEs), clinical laboratory test results (hematologic assessments, serum chemistry, and urinalysis), vital sign measurements (blood pressure, pulse rate, respiratory rate, and body temperature), and physical examination findings. Clinical laboratory testing occurred at screening, check-in, and day 4 in the single-dose phase and at day 8 and day 10 in the multiple-dose phase. On dosing days, vital signs were measured at screening, check-in, 15 min before dosing, and 0.5, 1, 2, 4, 8, and 12 h after dosing. Vital signs were also measured on nondosing days at times that coincided with those on dosing days (i.e., time-matched intervals at 4, 8, and 12 h after scheduled dosing).
AEs (defined as any untoward medical occurrence regardless of whether it is considered drug related) were coded by preferred term and system organ class using the Medical Dictionary for Regulatory Activities (MedDRA) v23.0. TEAEs were defined as any event that was not present before exposure to study drug or any event that worsened in intensity or frequency after exposure. AEs were assessed from administration of the first dose until participants were discharged from the clinic and up to approximately 30 days after the last dose. All AEs were followed up until they were resolved, stable, or judged clinically insignificant by the investigator.
PK Analyses
PK samples were analyzed by a validated liquid chromatography coupled with tandem mass spectrometry assay for treprostinil and TP in plasma samples with potassium EDTA as coagulant. The treprostinil analysis methods consisted of a BetaSil C8 Column (5 µm; ThermoFisher Scientific), [13C2D1]treprostinil as an internal standard, and a mobile-phase gradient of 5 mM ammonium bicarbonate and methanol. Treprostinil and its internal standard were detected under a negative ionization mode at m/z 389.2 → 331.1 and 392.1 → 332.1, respectively. The TP analysis method consisted of a C18 column (Poroshell 120 EC-C18 30 × 3.0 mm, 2.7 μm [Agilent]), TP-d4 as an internal standard, and a mobile-phase gradient of 0.1% trifluoroacetic acid in 10 mM ammonium acetate and acetonitrile. TP and its internal standard were detected under electrospray-positive ionization at m/z 632.5 → 355.3 and 636.5 → 355.3, respectively. The quantitation limits for treprostinil and TP were 10 pg/mL and 100 pg/mL, respectively.
In the single-dose phase, serial blood samples were collected on day 1 before dosing and 0.25, 0.5, 1, 1.5, 2, 4, 6, 8, 10, 12, 24, 36, 48, and 72 h after dosing. In the multiple-dose phase, serial blood samples were collected on day 1 before dosing and 0.25, 0.5, 1, 1.5, 2, 4, 6, 8, 10, and 12 h after dosing; before dosing only on days 2, 3, 4, 5, and 6; and before dosing on day 7 and 0.25, 0.5, 1, 1.5, 2, 4, 6, 8, 10, 12, 24, 48, and 72 h after dosing.
PK parameters derived from plasma samples were calculated using a noncompartmental analysis with Phoenix WinNonlin version 8.0 or higher (Certara, Inc) or SAS version 9.4 or higher (SAS Institute Inc), including the time to maximum plasma concentration (Tmax), Cmax, AUC from time 0 to the last time with quantifiable concentration (AUClast), AUC from time 0 to 24 h (AUCτ), AUC from time 0 to infinity (AUC0−∞), t1/2, total drug clearance following extravascular administration (CL/F), and volume of distribution at the terminal phase (Vd/F).
Statistical Analyses
Plasma concentrations below the limit of quantification (BLQ) were treated as zero for descriptive statistics. For PK parameter calculations, predose data on day 1 were treated as zero. All postdose BLQ values were considered missing.
Dose proportionality was assessed in the single-dose phase using the power regression model for AUCs and Cmax defined by ln[PK parameter] = β0 + β1ln[dose]. The null hypothesis was that AUCs and Cmax were dose proportional, or slope (β1) was equal to 1. Dose proportionality was concluded if the 90% confidence interval (CI) of the slope β1 was entirely within [1 + ln(0.5)/ln(r), 1 + ln(2)/ln(r)], where r was a ratio of highest dose to lowest dose that described the dose range. Steady state was tested in the multiple-dose phase by visual inspection of individual plasma trough levels from days 1 to 7.
The safety population consisted of participants who received at least one dose of TPIP or placebo. The PK population consisted of participants who received at least one dose of TPIP and had at least one measurable postdose plasma concentration. Sample sizes were not based on a formal statistical power calculation but were chosen to obtain reasonable evidence of safety and tolerability without exposing an undue number of participants to TP during this phase 1 study. The sample size was based on previous experience in phase 1 studies and not a formal statistical power calculation. All analyses were performed using SAS version 9.4 or higher (SAS Institute Inc).
Results
Participants
A total of 42 participants ranging from 21 to 44 years of age were randomized, 26 in the single-dose phase and 16 in the multiple-dose phase. A total of 97.2% (35 of 36) of participants who received at least one dose of TPIP and 100% (6 of 6) of those who received placebo completed the study. The first participant was enrolled on September 17, 2020, and the study was completed (i.e., the last participant contacted) on January 12, 2021. The mean participant age was 31.8 years in the single-dose group and 35.0 years in the multiple-dose group. In the single-dose group, baseline characteristics across treatment groups were generally similar, with slight variations with respect to sex, race, and ethnicity (Table 1). In the multiple-dose group, baseline characteristics across treatment groups varied slightly with respect to age, sex, race, and ethnicity (Table 1).
Safety
In the single-dose phase, TEAEs were reported in 70.8% (17 of 24) of TPIP-treated participants and 0% of placebo-treated participants. The most common TEAEs (15% or greater overall) among those treated with a single dose of TPIP were cough, dizziness, throat irritation, nausea, and hypotension (Table 2). Most TEAEs were mild. Four participants experienced a moderate TEAE: one participant in the TPIP 225 µg group (nausea and vomiting) and three participants in the TPIP 675 µg group (hypotension, n = 2; chest discomfort, oxygen saturation decreased, and dyspnea, n = 1). Treatment for chest discomfort and dyspnea was provided, and all TEAEs resolved.
In the multiple-dose group, 83.3% (10 of 12) of participants treated with multiple doses of TPIP experienced a TEAE compared with 50% (2 of 4) of placebo-treated participants. The most common TEAEs (15% or greater overall) among participants treated with multiple doses of TPIP were cough, headache, nausea, chest discomfort, and dizziness (Table 2). Most TEAEs were mild and occurred more frequently among those who did not undergo titration. Three participants, all in the TPIP 225 µg nontitrated group, experienced a moderate TEAE that resolved (throat irritation, n = 1; syncope, n = 1; chest discomfort, n = 1). The participant who experienced syncope experienced the AE approximately 8 h after the first dose (TPIP 225 µg), soon after a blood draw, and continued with dosing through completion. The participant who experienced moderate chest discomfort discontinued the study after two doses. Fewer participants in the TPIP multiple-dose group whose doses were titrated from TPIP 112.5 µg QD to 225 µg QD (66.7% [n = 4]) experienced TEAEs compared with those who received 225 µg QD at treatment initiation (100.0% [n = 6]); all TEAEs experienced with TPIP titration were mild (Table 2).
In both the single- and multiple-dose phases, no severe or serious TEAEs were reported, and no deaths occurred. No clinically significant findings from laboratory assessments or physical examinations were reported. Overall, vital signs observed after dosing were similar to those at baseline, except for mean decreases in diastolic and systolic blood pressure and increased mean pulse rate (greater than 10 beats per minute) observed mostly in the single-dose phase among participants treated with TPIP 675 µg, and mean decreases in diastolic and systolic blood pressure in those in the multiple-dose group, mostly among those whose doses were titrated from TPIP 112.5 µg QD to 225 µg QD. Changes in these vital signs among participants treated with a single dose of TPIP occurred within 8 h and started to resolve by 12 h post dosing. In those treated with multiple doses, mean diastolic blood pressure was lowest at 0.5 h after dosing on day 1, while the lowest mean systolic blood pressure occurred at 0.5 h after dosing on day 7. Importantly, any changes in either diastolic or systolic blood pressure began to resolve within an hour of dosing.
PK
TP plasma concentrations after single and multiple dosing were BLQ (less than 100 pg/mL) in all participants at all time points. Treprostinil plasma concentrations were dose dependent and measurable within 15 min and up to 72 h after TPIP dosing. Peak concentrations occurred 1.00 to 3.00 h after dosing, followed by exponential decline (Fig. 2). Elimination phases were parallel across all TPIP doses, and a moderate elimination rate was observed; t1/2 ranged from 8.67 to 11.6 h in participants treated with single TPIP doses (Table 3). In the multiple-dose group, mean steady-state elimination was 8.82 h with TPIP 225 µg QD for 7 days and 6.84 h with TPIP 225 µg QD when titrated from 112.5 µg (Table 4), and mean treprostinil plasma concentrations were BLQ by 48 h after day 7 dosing.
Treprostinil plasma concentration in healthy participants following a single TPIP dosing or b multiple QD TPIP dosing (PK population). d day, PK pharmacokinetics, QD once daily, TPIP treprostinil palmitil inhalation powder. aPre-dose samples were collected all days; serial post-dose samples were only collected on days 1 and 7
Treprostinil exposure was dose dependent, with low to moderate interindividual variability (Tables 3 and 4). No steady-state treprostinil accumulation was observed across all TPIP groups. Overall, treprostinil PK was linear within the dose range because CL/F, Vd/F, and t1/2 were comparable across TPIP treatment groups.
On the basis of a power model, treprostinil Cmax and AUC were proportionally correlated to the dose with slopes of 0.911 to 1.17 (Table 5).
Discussion
In this phase 1 study, single- and multiple-dose TPIP was generally well tolerated in healthy adults. The TEAEs reported by participants were dose related, mostly occurring in the highest single-dose TPIP groups (450 and 675 µg) and in the nontitrated multiple-dose group (TPIP 225 µg). Fewer TEAEs were reported in participants who received TPIP 112.5 µg for 4 days followed by 225 µg for 3 days compared with those who received TPIP 225 µg for 7 days. The uptitration approach appeared to improve TPIP tolerability. It is important to note that the doses in this study, which were informed by a phase 1 study of TPIS, were relatively high compared with the target dose of inhaled treprostinil (54–72 µg) in the currently approved product label for Tyvaso in the USA [10]. Even so, most TEAEs experienced with TPIP were mild, and all resolved.
In the present study, treprostinil PK in participants administered TPIP was linear, and systemic exposure was dose proportional. PK parameters were comparable among those treated with TPIP 225 µg, which was the most commonly used dose in the study as it was administered to two multiple-dose treatment groups and the single-dose group, indicating the reproducibility of the results despite different dosing schemes as well as a lack of effect of interindividual variability. Furthermore, no accumulation at steady state was observed.
Treprostinil exposure in this study was comparable to the exposure when treprostinil is administered as TPIS [13]. Compared with daily doses of available treprostinil products, treatment with TPIP 225 µg resulted in lower treprostinil systemic exposure (both Cmax and AUC) with a much longer elimination t1/2 due to the prolonged conversion from the prodrug TP. On the basis of in vitro data, TP is slowly converted to treprostinil in human lung tissues and then absorbed into systemic circulation [16]. Hence, the elimination of treprostinil with TPIP dosing is limited by its formation. On the basis of results from preclinical studies, the plasma half maximal effective concentration (EC50) of treprostinil was 60-fold (rats) and 550-fold (dogs) lower with inhaled TP than with treprostinil delivered via intravenous infusion [15]. These results suggest a considerable local effect of TPIP on the pulmonary vasculature that, if found to translate to patients, may provide a clinical benefit in PAH or PH-ILD, with relatively low systemic treprostinil exposure. Achieving high pulmonary exposure while maintaining low systemic exposure could allow for greater achievable efficacy through higher tolerated doses and a reduced risk for AEs that are associated with systemic delivery. Additionally, the prolonged conversion of treprostinil from TP after TPIP administration suggests the potential for QD administration.
If study results demonstrate efficacy, this could potentially provide an option that may be more tolerable and convenient than available inhaled treprostinil, which requires frequent administration because of rapid elimination from the circulation. High systemic treprostinil levels, additionally, are associated with dose-limiting AEs [10]. In fact, a phase 1 study showed greater tolerability of inhaled TP delivered as TPIS compared with inhaled treprostinil, as well as approximately tenfold lower Cmax, similar AUC, and approximately tenfold longer t1/2 [13, 17]. Given improved tolerability, it is conceivable that steady-state exposures of treprostinil from TPIP may approach what can be achieved through continuous intravenous or subcutaneous infusion of treprostinil. In that manner, TPIP may compare favorably to intravenous or subcutaneous administration of treprostinil in patients with PAH, with more convenient administration. Efficacy and tolerability of QD TPIP administration in patients with PAH and PH-ILD are currently being assessed in ongoing and planned phase 2 trials.
The findings of this study should be interpreted in light of the limitations that phase 1 studies carry; for this study, these limitations included the small number of study participants and that TPIP effects were assessed in healthy volunteers, not in patients with PAH or PH-ILD. Larger phase 2 studies to assess the safety and efficacy of TPIP in patients with PAH or PH-ILD are planned or in progress.
Conclusion
The findings from this phase 1 study demonstrated that TP delivered via TPIP was generally well tolerated, with a safety profile consistent with that of other prostanoid therapies, and that an uptitration strategy improved tolerability. Furthermore, the PK profile indicated the potential for QD administration, an important distinction from the currently approved inhaled PAH medications. Taken together, the PK and safety results from this phase 1 study support further evaluation of TPIP administered QD in patients with PAH and PH-ILD.
References
Leifer FG, Konicek DM, Chen KJ, et al. Inhaled treprostinil-prodrug lipid nanoparticle formulations provide long-acting pulmonary vasodilation. Drug Res (Stuttg). 2018;68:605–14. https://doi.org/10.1055/s-0044-100374.
Leber L, Beaudet A, Muller A. Epidemiology of pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension: identification of the most accurate estimates from a systematic literature review. Pulm Circ. 2021;11:2045894020977300. https://doi.org/10.1177/2045894020977300.
Coons JC, Pogue K, Kolodziej AR, Hirsch GA, George MP. Pulmonary arterial hypertension: a pharmacotherapeutic update. Curr Cardiol Rep. 2019;21:141. https://doi.org/10.1007/s11886-019-1235-4.
Simonneau G, Montani D, Celermajer DS, et al. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J. 2019;53:1801913. https://doi.org/10.1183/13993003.01913-2018.
Parikh V, Bhardwaj A, Nair A. Pharmacotherapy for pulmonary arterial hypertension. J Thorac Dis 2019;11:S1767–81. https://doi.org/10.21037/jtd.2019.09.14.
Corboz MR, Salvail W, Gagnon S, et al. Prostanoid receptor subtypes involved in treprostinil-mediated vasodilation of rat pulmonary arteries and in treprostinil-mediated inhibition of collagen gene expression of human lung fibroblasts. Prostaglandins Other Lipid Mediat. 2021;152:106486. https://doi.org/10.1016/j.prostaglandins.2020.106486.
Whittle BJ, Silverstein AM, Mottola DM, Clapp LH. Binding and activity of the prostacyclin receptor (IP) agonists, treprostinil and iloprost, at human prostanoid receptors: treprostinil is a potent DP1 and EP2 agonist. Biochem Pharmacol. 2012;84:68–75. https://doi.org/10.1016/j.bcp.2012.03.012.
Lambers C, Kornauth C, Oberndorfer F, et al. Mechanism of anti-remodelling action of treprostinil in human pulmonary arterial smooth muscle cells. PLoS ONE. 2018;13:e0205195. https://doi.org/10.1371/journal.pone.0205195.
LeVarge BL, Channick RN. Inhaled treprostinil for the treatment of pulmonary arterial hypertension. Expert Rev Respir Med. 2012;6:255–65. https://doi.org/10.1586/ers.12.23.
Chapman RW, Corboz MR, Malinin VS, et al. An overview of the biology of a long-acting inhaled treprostinil prodrug. Pulm Pharmacol Ther. 2020;65:102002. https://doi.org/10.1016/j.pupt.2021.102002.
LeVarge BL. Prostanoid therapies in the management of pulmonary arterial hypertension. Ther Clin Risk Manag. 2015;11:535–47. https://doi.org/10.2147/TCRM.S75122.
Channick RN, Voswinckel R, Rubin LJ. Inhaled treprostinil: a therapeutic review. Drug Des Devel Ther. 2012;6:19–28. https://doi.org/10.2147/DDDT.S19281.
Chapman RW, Corboz MR, Fernandez C, et al. Characterisation of cough evoked by inhaled treprostinil and treprostinil palmitil. ERJ Open Res. 2021;7:00592–2020. https://doi.org/10.1183/23120541.00592-2020.
Tyvaso [package insert]. Research Triangle Park, NC: United Therapeutics Corp., 2021.
Chapman RW, Li Z, Corboz MR, et al. Inhaled hexadecyl-treprostinil provides pulmonary vasodilator activity at significantly lower plasma concentrations than infused treprostinil. Pulm Pharmacol Ther. 2018;49:104–11. https://doi.org/10.1016/j.pupt.2018.02.002.
Corboz MR, Li Z, Malinin V, et al. Preclinical pharmacology and pharmacokinetics of inhaled hexadecyl-treprostinil (C16TR), a pulmonary vasodilator prodrug. J Pharmacol Exp Ther. 2017;363:348–57. https://doi.org/10.1124/jpet.117.242099.
Chapman RW, Corboz MR, Fernandez C, et al. Characterisation of cough evoked by inhaled treprostinil and treprostinil palmitil [supplemental appendix]. ERJ Open Res. 2021;7:00592–2020. https://openres.ersjournals.com/content/erjor/7/1/00592-2020/DC1/embed/inline-supplementary-material-1.pdf?download=true. Accessed Mar 17 2022.
Han D, Fernandez C, Sullivan E, et al. Single dose pharmacokinetics of C16TR for Inhalation (INS1009) vs treprostinil inhalation solution [PA2398]. Eur J Respir. 2016;48(suppl 60). Abstract PA2398. https://doi.org/10.1183/13993003.congress-2016.PA2398.
Han D, Fernandez C, Sullivan E, et al. Safety and pharmacokinetics study of a single ascending dose of C16TR for inhalation (INS1009). Eur J Respir. 2016;48(suppl 60). Abstract PA2403. https://doi.org/10.1183/13993003.congress-2016.PA2403.
Acknowledgements
The authors would like to thank the participants of the study, and would also like to acknowledge Dr. Shilpa Dhar Murthy for her contributions to this study.
Funding
This study was funded by Insmed Incorporated. The study sponsor also funded the journal’s Rapid Service and Open Access fees.
Medical Writing, Editorial, and Other Assistance
Monica Husby, PhD, and Kristen A. Andersen, PhD, of MediTech Media, Ltd provided medical writing assistance; editorial and creative support were also provided by MediTech Media, Ltd. Insmed Incorporated provided funding to MediTech Media, Ltd for these services. Clinical PK samples were analyzed by KCAS Bioanalytical & Biomarker Services, an Integris BioServices, LLC Company (Shawnee, KS, USA).
Author Contributions
All authors contributed to validation, writing, review and editing of the manuscript. Fraz A. Ismat conceptualized the research, conducted research investigations, developed methods, administered projects, curated data, and visualized data. Helen Usansky conceptualized the research, conducted research investigations, developed methods, and curated, analyzed, and visualized data. Raul Villa supervised research activities. Jun Zou curated, analyzed, and visualized data. Ariel Teper conceptualized the research, acquired funding, developed methods, and supervised research activities.
Disclosures
Fraz A. Ismat, Helen Usansky, Raul Villa, Jun Zou, and Ariel Teper are employees and stockholders of Insmed Incorporated.
Compliance With Ethics Guidelines
This study was carried out in accordance with the ethical principles derived from international guidelines, including the Declaration of Helsinki and the Council for International Organizations of Medical Sciences International Ethical Guidelines, International Council for Harmonisation Good Clinical Practice Guideline, and applicable local regulatory requirements and laws; and was approved by the Salus Institutional Review Board. Before study entry, all participants provided written informed consent in compliance with US Title 21 Code of Federal Regulations, Part 50, which was submitted by the investigator to the institutional review board for the study site.
Data Availability
The anonymized data generated and analyzed for the article are not publicly available, but can be made available upon review of reasonable requests.
Prior Presentations
Data reported here were previously presented at two conferences: An oral presentation at the 2021 European Society of Cardiology Congress. The abstract was published in the European Heart Journal: Ismat FA, Usansky H, Dhar Murthy S, Zou J, Teper A. Safety, tolerability, and pharmacokinetics (PK) of treprostinil palmitil inhalation powder (TPIP): a phase 1, randomised, double-blind, single- and multiple-dose study. European Heart Journal 2021;42(suppl 1):ehab724.1954. https://doi.org/10.1093/eurheartj/ehab724.1954. A poster presentation at the Pulmonary Hypertension Association’s (PHA) 2022 International PH Conference and Scientific Sessions: Ismat FA, Usansky H, Villa R, Zou J, Teper A. Safety, tolerability, and pharmacokinetics of treprostinil palmitil inhalation powder: a phase 1 randomized, double-blind, single and multiple dose study. Poster presented at: PHA 2022 International PH Conference and Scientific Sessions; June 10–12, 2022; Atlanta, GA, USA (poster 1043).
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ismat, F.A., Usansky, H.H., Villa, R. et al. Safety, Tolerability, and Pharmacokinetics of Treprostinil Palmitil Inhalation Powder for Pulmonary Hypertension: A Phase 1, Randomized, Double-Blind, Single- and Multiple-Dose Study. Adv Ther 39, 5144–5157 (2022). https://doi.org/10.1007/s12325-022-02296-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02296-x