Abstract
Introduction
The objective was to use the evidence-based medicine metrics of number needed to treat, number needed to harm, and likelihood to be helped or harmed to appraise the clinical efficacy and tolerability of sublingual dexmedetomidine in adults with agitation associated with schizophrenia or bipolar disorder.
Methods
Sublingual dexmedetomidine data for this post hoc analysis were obtained from two similarly designed, double-blind, randomized, placebo-controlled studies of adults with schizophrenia or bipolar disorder. Response to treatment was defined as a ≥ 40% reduction from baseline in the Positive and Negative Syndrome Scale-Excited Component (PEC). Tolerability was assessed by evaluating rates of adverse events.
Results
The number needed to treat (95% confidence interval) estimate versus placebo for PEC response at 2 h post-dose was 3 (2, 3) for the sublingual dexmedetomidine 180-µg group (n = 125) and 3 (3, 4) for the 120-µg group (n = 129) in the study of patients with schizophrenia and 3 (2, 3) for the sublingual dexmedetomidine 180-µg group (n = 126) and 4 (3, 6) for the 120-µg group (n = 126) in the study of patients with bipolar disorder. Number needed to harm values versus placebo were greater than 10 for all adverse events except somnolence, where the number needed to harm (95% confidence interval) was 7 (5, 10) for all doses pooled from both studies. In all instances, likelihood to be helped or harmed values were greater than 1 for efficacy versus applicable tolerability outcomes.
Conclusions
The number needed to treat, number needed to harm, and likelihood to be helped or harmed of sublingual dexmedetomidine support a favorable benefit–risk profile in adults with acute agitation associated with schizophrenia or bipolar disorder.
Trial Registration
ClinicalTrials.gov, https://clinicaltrials.gov/ct2/show/NCT04268303, NCT04268303. ClinicalTrials.gov, https://clinicaltrials.gov/ct2/show/NCT04276883, NCT04276883.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Episodes of acute agitation associated with schizophrenia or bipolar disorder are common and challenging for patients, caregivers, and healthcare providers. |
Ideal treatments are needed that are effective, noninvasive, and calming without sedating. |
This post hoc analysis calculated the number needed to treat and harm for a recently approved treatment based on two similarly designed phase 3 clinical trials. |
Number needed to treat values versus placebo were consistent with a potent beneficial effect for sublingual dexmedetomidine, and number needed to harm values indicated that sublingual dexmedetomidine is reasonably tolerable. |
The likelihood to be helped or harmed was greater than 1 when contrasting clinical response versus any tolerability challenge, indicating a favorable benefit–risk profile for sublingual dexmedetomidine in the treatment of acute agitation in adults with schizophrenia or bipolar disorder. |
Introduction
Episodes of acute agitation that occur in individuals with schizophrenia and bipolar disorder can present a substantial challenge for patients, families, and healthcare professionals [1,2,3]. Nonpharmacological approaches are recommended as initial management of agitation, including verbal de-escalation and environmental management; however, pharmacological therapy may be needed if these techniques are not sufficient to avoid escalation [1, 2, 4,5,6]. An ideal drug for treating acute agitation should be noninvasive, easy to administer by healthcare professionals or the patient, provide a rapid onset of action within 30 min, produce calmness without excess sedation, and be safe and well tolerated [4].
Selecting a medication for acute agitation can be challenging, especially when treatment decisions involve agents that may be unfamiliar to clinicians and patients. Although findings from randomized controlled clinical trials provide the most reliable information, the statistical significance of a drug relative to placebo (i.e., P value) is insufficient as the sole basis for clinical decision-making because it provides no information about the size of treatment effects [7]. To complement tests of significance and refine the process of drug selection, clinically intuitive measures of effect size can be used, including number needed to treat (NNT), which quantifies benefit (therapeutic response), and number needed to harm (NNH), which quantifies undesirable outcomes such as adverse events (AEs) or discontinuation due to AEs [8,9,10]. The ratio of NNH to NNT is called the likelihood to be helped or harmed (LHH) [10]. These metrics have been used to evaluate other agents used for the treatment of agitation [11,12,13], as well as other new medications [14,15,16], and help clinicians understand the potential place in therapy of novel interventions.
Dexmedetomidine is a potent and selective agonist of the α2-adrenergic receptor, which is a key regulator of sympathetic hyperarousal via inhibition of norepinephrine release from adrenergic neurons [17]. Sublingual dexmedetomidine, (BioXcel Therapeutics, New Haven, CT, USA) was recently approved by the US Food and Drug Administration to treat acute agitation in adults with schizophrenia and bipolar disorder. Sublingual or buccal administration of sublingual dexmedetomidine bypasses first-pass metabolism, results in increased absorption compared to oral administration, and evidences a rapid onset of action [18]. Sublingual dexmedetomidine represents a novel mechanism of action and route of administration for treating acute agitation associated with schizophrenia or bipolar disorder.
The efficacy and tolerability of 120-µg and 180-µg doses of sublingual dexmedetomidine were evaluated in two similarly designed, randomized, double-blind, placebo-controlled, phase 3 trials in the treatment of acute agitation associated with schizophrenia [19] and bipolar disorder [20]. Efficacy in both studies was measured from 10 min through 24 h post-dose using the 5-item Positive and Negative Syndrome Scale-Excited Component (PEC), a validated and commonly used research instrument for evaluating acute agitation and aggression in patients with different psychiatric pathologies [21]. Participants with schizophrenia or bipolar disorder who were treated with sublingual dexmedetomidine, 120 µg or 180 µg, had symptomatic improvements from baseline to 2 h post-dose compared to placebo, and treatment effects began at 20 or 30 min post-dose [19, 20, 22]. Sublingual dexmedetomidine was well tolerated, with mild or moderate somnolence as the most common AE [16]. While these statistically significant results are essential to the evidence base for sublingual dexmedetomidine, they have limited value in appraising its potential clinically relevant value in the treatment of patients with agitation associated with schizophrenia or bipolar disorder. A description of effect sizes is required in order to place this potential intervention into clinical perspective. The objective of this post hoc analysis of data from two randomized controlled clinical trials was to use the evidence-based medicine metrics of NNT, NNH, and LHH to provide a clinically meaningful estimate of the efficacy and tolerability of sublingual dexmedetomidine in adults with agitation associated with schizophrenia or bipolar disorder.
Methods
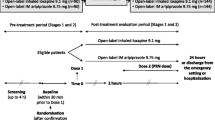
Data were taken from two similarly designed, randomized, double-blind, placebo-controlled studies that evaluated the effects of sublingual dexmedetomidine on acute agitation in patients with schizophrenia (NCT04268303) or bipolar disorder (NCT04276883) [19, 20]. The studies were conducted between January and May 2020 at clinical sites in the United States. Each study was conducted in accordance with Good Clinical Practices and the Declaration of Helsinki, and were approved by the institutional review board or ethics committee at each participating site. All patients provided written informed consent before any study procedures were undertaken.
Conduct
All study participation was voluntary, and participants were free to withdraw from the study at any time and for any reason. Acutely agitated patients could be identified in outpatient clinics, and by mental health, psychiatric, or medical emergency services, including medical/psychiatric observation units, as newly admitted to hospital settings for acute agitation, or already in hospital for underlying conditions. Participants remained in hospital or were domiciled in clinical research settings under medical supervision during screening procedures. The protocol allowed a maximum of three overnights from the time of admission to the clinical research unit to discharge. Each study included a Screening Visit, Treatment Visit (Day 1), Follow-Up Visit (Day 2), Discharge (Day 3), and End of Study Visit (Day 7). To obtain data through 2 days post-dose, participants remained in the clinical unit until the morning of Day 3. Day 7 (+ 2) was the final study visit during which blood and urine were collected for clinical laboratory tests, vital signs were repeated, and concomitant medications and AEs were recorded.
Eligible participants were randomly assigned (1:1:1) to sublingual dexmedetomidine 180 µg, sublingual dexmedetomidine 120 µg, or matching placebo film; randomization was stratified by age (< 65, ≥65 years). Participants were instructed on sublingual administration of the study drug, which was self-administered under the supervision of a trained staff member. In the event of persistent or recurrent agitation, a repeat dose of 90 µg or 60 µg sublingual dexmedetomidine (ie, one half of the originally administered dose) could be given after the 2-h time point. The maximum number of repeat doses was 2 during the 12 h after the first dose. Participants and study site personnel were blinded to study assignment.
Participants
Eligible participants were aged 18–75 years and had acute agitation associated with (1) schizophrenia, schizoaffective, or schizophreniform disorder [19] or (2) bipolar I or II disorder [20] regardless of polarity (eg, mania or depression). The diagnoses of schizophrenia and bipolar disorder were based on the criteria in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition [23]. At screening and baseline, participants were required to have a PEC total score of at least 14 and a score of 4 or more on at least 1 of the 5 PEC items (poor impulse control, tension, hostility, uncooperativeness, and excitement, each rated from 1 [absent] to 7 [extreme]), consistent with the presence of actionable agitation. [21]
Assessments
In both studies, response to treatment was defined as a reduction of at least 40% from baseline on the PEC total score [21] and was calculated using the following formula: ([PEC postbaseline] − [PEC baseline])/(PEC baseline − 5). The 40% threshold for response to treatment was based on the validation study finding that PEC improvement of 38% or greater from baseline corresponded to a CGI-I improvement of “much improved” [21], and has been used as the definition of treatment response in similar registrational studies of intramuscular olanzapine, intramuscular aripiprazole, and inhaled loxapine for the treatment of agitation [11, 12]. The PEC was administered at screening, pre-dose (within 15 min before dosing), and at 10, 20, 30, and 45 min, and 1, 1.5, 2, 4, 6, 8, and 24 h post-dose. Both studies also used an alternate definition of response: achieving a score of 1 (very much improved) or 2 (much improved) on the Clinical Global Impressions-Improvement (CGI-I) Scale. [24] Agitation and potential sedation were further assessed using the Agitation-Calmness Evaluation Scale (ACES) [25, 26], where 1 = marked agitation, 2 = moderate agitation, 3 = mild agitation, 4 = normal behavior, 5 = mild calmness. 6 = moderate calmness, 7 = marked calmness, 8 = deep sleep, and 9 = unarousable. The ACES was administered at pre-dose, 2, 4, and 8 h post-dose.
Statistical Analysis
The efficacy (intent-to-treat population) population included all participants who received a dose of the study drug and had baseline and post-dose PEC total score assessments. The AE population included all participants who received a dose of the study drug; AEs of special interest included bradycardias, cardiac/vascular disorders, hypotension, and somnolence. The pooled efficacy population included all participants in both studies who received a dose of the study drug and had baseline and post-dose PEC total score assessments.
The NNT values for response were calculated using 1/Absolute Risk Reduction (ARR), where ARR was the rate of response in the sublingual dexmedetomidine treatment group minus the rate in placebo group in the efficacy population. Values for the NNH were calculated using the incidence rates for AEs occurring in at least 2% of participants in the safety population, as well as AEs of special interest, regardless of the percentage of participants reporting them. The NNH analysis examined AEs occurring within 2 h of initial study drug administration (acute) versus those occurring more than 2 h after initial study drug administration (delayed). By convention, NNT and NNH values were rounded up to the closest integer [27]. The association between mean ACES scores and the onset of somnolence (as measured by the presence or absence of drowsiness, sleepiness, or somnolence) was also evaluated. Generally, a low NNT (i.e., at least 10% better than placebo, resulting in an NNT < 10) with a higher associated NNH (no more than a 10% disadvantage, resulting in an NNH > 10) is preferred. The likelihood to be helped or harmed (LHH) was calculated as the ratio of NNH to NNT; in general, LHH values > 1 suggest an intervention is more likely to help patients than to harm them. [10]
Values for NNT and NNH, with their respective 95% confidence intervals (CIs), for sublingual dexmedetomidine versus placebo were computed for each outcome. When the NNT or NNH estimate was not statistically significant at the P < 0.05 threshold (as noted when the 95% CI would contain infinity), the notation of not significant (ns) was provided. The terms statistically significant and not statistically significant are used descriptively and not inferentially, as PEC response was an exploratory endpoint that was not adjusted for multiplicity in the studies; all reported P values in this analysis are nominal. Results from the two studies are presented individually and as a pooled population.
Results
Participants in the two studies had a mean age of 45.6 (SD 11.52; range 18–71); 46% identified as female, 67% identified as black or African American, and 30% identified as white (Table 1).
PEC Response
Baseline PEC and item scores are provided in Table 2. In participants with schizophrenia (n = 380), PEC response rates at 2 h in the sublingual dexmedetomidine 180-μg and 120-μg dose groups were significantly higher than with placebo [88.8% (111/125) and 79.1% (102/129), respectively, vs. 40.5% (51/126), P < 0.0001 vs. placebo for both doses]. In participants with bipolar disorder (n = 278), PEC response rates at 2 h in the sublingual dexmedetomidine 180-μg and 120-μg groups were also significantly higher than with placebo [90.5% (114/126) and 77.0% (97/126) vs. 46.0% (58/126), P < 0.0001 vs. placebo for both doses].
Number Needed to Treat
In participants with schizophrenia, the NNT (95% CI) versus placebo for response at 2 h post-dose was 3 (2, 3) for the sublingual dexmedetomidine 180-µg group and 3 (3, 4) for the sublingual dexmedetomidine 120-µg group (Table 3). The NNT (95% CI) was 5 (4, 10) for the sublingual dexmedetomidine 180-µg group at 20 min post-dose, and it remained between 3 and 6 at all subsequent time points from 30 min post-dose through 24 h post-dose. In the sublingual dexmedetomidine 120-µg group, the NNT was below 10 starting at 45 min, and remained between 3 and 6 at subsequent time points through 24 h.
In participants with bipolar disorder, the NNT (95% CI) relative to placebo for 2-h response was 3 (2, 3) for the sublingual dexmedetomidine 180-µg group and 4 (3, 6) for the 120-µg group (Table 4). The NNT was below 10 starting at 30 min post-dose and remained between 3 and 5 from 45 min post-dose through 24 h post-dose for the sublingual dexmedetomidine 180-µg group, and from 45 min post-dose through 24 h post-dose for the sublingual dexmedetomidine 120-µg group.
In the pooled population (n = 506), efficacy data for both sublingual dexmedetomidine doses in both studies resulted in an NNT (95% CI) versus placebo of 3 (3, 3) at 2 h post-dose. The time course of NNT, which shows benefits in participants treated with sublingual dexmedetomidine from baseline through 2 h post-dose, is presented in Fig. 1. The range for pooled NNT remained between 3 and 6 from 45 min post-dose through 24 h post-dose (Table S1).
When response was defined using CGI-I, effect sizes were similar to those observed when PEC was used to define response (Table S5). The NNTs for PEC and CGI-I response were consistent with the magnitude of effect size, as measured by Cohen’s d for the PEC change score versus placebo (Table S6).
Number Needed to Harm
In participants with schizophrenia, the NNH versus placebo was greater than 10 for both doses of sublingual dexmedetomidine for all acute AEs, except for somnolence (Table 5). For somnolence, the NNH (95% CI) was 8 (5, 23) and 8 (5, 22) for the sublingual dexmedetomidine 180-µg and 120-µg groups, respectively. Headache was reported more frequently in the placebo group than in the dexmedetomidine groups, hence resulting in a “negative” estimate for NNH. The LHH was 5.7 or greater when contrasting response versus all AEs except somnolence, where it was 2.7 for both sublingual dexmedetomidine treatment groups. Most [92.7% (51/55)] somnolence events occurred within 2 h of dosing, and most [91.7% (44/48)] were mild (Table S2). One somnolence event occurred beyond 4 h post-dose. The mean (SD) (range) ACES score associated with somnolence was 2.5 (0.94) (2.0, 4.3), and there were no observed ACES scores greater than 7.
For participants with bipolar disorder, the NNH versus placebo was greater than 10 for all acute AEs, except for somnolence (Table 6). For somnolence, the NNH (95% CI) was 6 (5, 12) and 7 (5, 13) for the sublingual dexmedetomidine 180-µg and 120-µg groups, respectively. Nausea was reported more frequently in the placebo group than in the dexmedetomidine groups, and headache was reported more frequently in the placebo group than in the dexmedetomidine 180-µg group, resulting in “negative” estimates for NNH. The LHH was 4.5 or greater when contrasting response versus all AEs except somnolence, where it was 2.0 and 1.8 for the sublingual dexmedetomidine 180-µg and 120-µg groups, respectively. In the bipolar disorder study, most (96.2% [51/53]) somnolence events occurred within 2 h of dosing, and 66.0% (35/53) were mild in severity (Table S2). The mean (SD) (range) ACES score associated with somnolence was 2.3 (0.85) (2.2, 4.5), and there were no observed ACES scores greater than 7.
The NNH versus placebo for delayed AEs was greater than 10 for all AEs of special interest for participants in both studies (Tables S3 and S4).
Discussion
This post hoc analysis was designed to use the evidence-based medicine metrics of number needed to treat, number needed to harm, and likelihood to be helped or harmed to provide a clinically meaningful estimate of the efficacy and tolerability of sublingual dexmedetomidine in adults with agitation associated with schizophrenia or bipolar disorder. The results using multiple measures of treatment response consistently demonstrated that the NNT, NNH, and LHH of sublingual dexmedetomidine support a favorable benefit–risk profile in adults with acute agitation associated with schizophrenia or bipolar disorder. The magnitude of the effect size with sublingual dexmedetomidine (1 standard deviation unit, as measured by Cohen’s d for the PEC change score vs. placebo) is considered large. [28]
Moreover, the pooled NNT estimate versus placebo of three compares favorably with similar analyses done for agents approved by the US Food and Drug Administration for agitation associated with schizophrenia and/or bipolar disorder, including intramuscular and inhaled formulations (Fig. 2).
Number needed to treat and 95% confidence intervals for response versus placebo for sublingual dexmedetomidine, 120 µg or 180 µg, inhaled loxapine, 5 or 10 mg, intramuscular ziprasidone, 10 or 20 mg, intramuscular olanzapine, 10 mg, and intramuscular aripiprazole, 9.75 mg. All data pooled from available studies as reported elsewhere. Not shown are data for haloperidol 6.5–7.5 mg or lorazepam 2 mg administered intramuscularly, where the NNT (95% CI) for response versus placebo has been reported as 4 (3, 5) and 4 (3, 7); refer to Fig. 1 in Citrome L. J Clin Psychiatry. 2007;68(12):1876–85
For NNH, values were greater than 10 for all AEs except somnolence, which indicates a low risk of harm from treatment with sublingual dexmedetomidine. In particular, the NNH for cardiac and vascular disorders, specifically hypotension, bradycardia, and orthostatic hypotension, were favorable for both doses of sublingual dexmedetomidine. Although somnolence was the most common AE, most occurrences were of mild severity, occurred within 2 h of dosing, and were associated with mean ACES scores of approximately 2.5; no sublingual dexmedetomidine-treated participants experienced deep sleep or were unarousable.
The metrics of NNT and NNH translate effect size into clinically meaningful information by quantifying how many patients need to be treated with an intervention versus placebo to encounter 1 additional outcome of interest. A rule of thumb is that single-digit NNTs (< 10) for efficacy measures suggest the intervention has potentially useful benefits, and that double-digit or higher NNHs (> 10) for AEs indicate that the intervention is potentially well tolerated [10]. Among adults with agitation associated with schizophrenia or bipolar disorder, where a delay in treatment can lead to escalation and injury for patients and clinicians, it is especially important that trial results be considered in terms of the clinical circumstances at hand, including urgency to treat and overall patient acceptability. By converting efficacy and safety results from clinical trials into ”patient units”, NNT and NNH also enable indirect, cross-study comparisons of interventions for agitation, as long as the studies are methodologically similar (i.e., similar populations and outcome measures).
The analysis presented here has several strengths. The estimates of NNT and NNH were obtained from rigorously conducted placebo-controlled trials that were conducted to support regulatory approval of sublingual dexmedetomidine. The efficacy outcome itself (therapeutic response as defined by a 40% or greater reduction from baseline on the PEC total score) has been used in other studies examining agitation, thus making indirect comparisons possible. A focus on effect size allows for the appraisal of the clinical significance of the study findings. Benefit–risk is further quantified by the metric of LHH.
This study has several limitations. First, the NNT in this post hoc analysis was based on a dichotomous outcome (PEC response) that was an exploratory endpoint in the source studies, with no adjustment for multiplicity. However, the effect size based on this outcome was consistent using an alternate outcome measure assessing clinical response (CGI-I) and other analytical techniques (calculation of Cohen’s d for the PEC change score). Second, while the findings reported here are consistent with those of other studies of pharmacological therapy for treating acute agitation in adults with schizophrenia and bipolar disorder [11, 12], they may not be generalizable to nonresearch patients who may differ from patients who participate in clinical trials.
Conclusions
In this post hoc analysis of two Phase 3 studies of sublingual dexmedetomidine in patients experiencing acute agitation episodes associated with schizophrenia or bipolar disorder, NNT values versus placebo were consistent with a potent beneficial effect, and NNH values versus placebo indicated that sublingual dexmedetomidine is reasonably tolerable. The LHH for both studies contrasting efficacy with tolerability was greater than 1, indicating a favorable benefit–risk profile for sublingual dexmedetomidine in the treatment of acute agitation in adults with schizophrenia or bipolar disorder.
Change history
31 October 2022
A Correction to this paper has been published: https://doi.org/10.1007/s12325-022-02350-8
References
Garriga M, Pacchiarotti I, Kasper S, et al. Assessment and management of agitation in psychiatry: expert consensus. World J Biol Psychiatry. 2016;17(2):86–128.
Sacchetti E, Valsecchi P, Tamussi E, Paulli L, Morigi R, Vita A. Psychomotor agitation in subjects hospitalized for an acute exacerbation of Schizophrenia. Psychiatry Res. 2018;270:357–64.
Alderfer BS, Allen MH. Treatment of agitation in bipolar disorder across the life cycle. J Clin Psychiatry. 2003;64(Suppl 4):3–9.
Martinez-Raga J, Amore M, Di Sciascio G, et al. 1st International experts’ meeting on agitation: conclusions regarding the current and ideal management paradigm of agitation. Front Psychiatry. 2018;9:54.
Pacciardi B, Calcedo A, Messer T. Inhaled loxapine for the management of acute agitation in bipolar disorder and schizophrenia: expert review and commentary in an era of change. Drugs R D. 2019;19(1):15–25.
Patel MX, Sethi FN, Barnes TRE, et al. Joint BAP NAPICU evidence-based consensus guidelines for the clinical management of acute disturbance: de-escalation and rapid tranquillisation. J Psychiatric Intensive Care. 2018;14(2):89–132.
Wasserstein RL, Lazar NA. The ASA Statement on p-values: context, process, and purpose. Am Stat. 2016;70(2):129–33.
Laupacis A, Sackett DL, Roberts RS. An assessment of clinically useful measures of the consequences of treatment. N Engl J Med. 1988;318(26):1728–33.
Altman DG. Confidence intervals for the number needed to treat. BMJ. 1998;317(7168):1309–12.
Citrome L, Ketter TA. When does a difference make a difference? Interpretation of number needed to treat, number needed to harm, and likelihood to be helped or harmed. Int J Clin Pract. 2013;67(5):407–11.
Citrome L. Comparison of intramuscular ziprasidone, olanzapine, or aripiprazole for agitation: a quantitative review of efficacy and safety. J Clin Psychiatry. 2007;68(12):1876–85.
Citrome L. Inhaled loxapine for agitation revisited: focus on effect sizes from 2 Phase III randomised controlled trials in persons with schizophrenia or bipolar disorder. Int J Clin Pract. 2012;66(3):318–25.
Pratts M, Citrome L, Grant W, Leso L, Opler LA. A single-dose, randomized, double-blind, placebo-controlled trial of sublingual asenapine for acute agitation. Acta Psychiatr Scand. 2014;130(1):61–8.
Citrome L, Juday T, Frech F, Atkins N Jr. Lemborexant for the treatment of insomnia: direct and indirect comparisons with other hypnotics using number needed to treat, number needed to harm, and likelihood to be helped or harmed. J Clin Psychiatry. 2021. https://doi.org/10.4088/JCP.20m13795.
Citrome L, DiBernardo A, Singh J. Appraising esketamine nasal spray for the management of treatment-resistant depression in adults: number needed to treat, number needed to harm, and likelihood to be helped or harmed. J Affect Disord. 2020;271:228–38.
Citrome L, Sánchez Del Rio M, Dong Y, et al. Benefit-risk assessment of galcanezumab versus placebo for the treatment of episodic and chronic migraine using the metrics of number needed to treat and number needed to harm. Adv Ther. 2021;38(8):4442–60.
Weerink MAS, Struys M, Hannivoort LN, Barends CRM, Absalom AR, Colin P. Clinical pharmacokinetics and pharmacodynamics of dexmedetomidine. Clin Pharmacokinet. 2017;56(8):893–913.
Preskorn SH, Risinger R, Kakar R, Yocca FD. Double-blind, placebo-controlled, single ascending dose, study to determine the efficacy, safety, and pharmacokinetics of a BXCL501 (sublingual dexmedetomidine) in agitation associated with schizophrenia or related. Neuropsychopharmacology. 2019;44:114.
Citrome L, Preskorn SH, Lauriello J, et al. Sublingual dexmedetomidine for the treatment of acute agitation in adults with schizophrenia or schizoaffective disorder: a randomized placebo-controlled trial. J Clin Psychiatry. (In Press)
Preskorn SH, Zeller S, Citrome L, et al. Effect of sublingual dexmedetomidine vs placebo on acute agitation associated with bipolar disorder: a randomized clinical trial. JAMA. 2022;327(8):727–36.
Montoya A, Valladares A, Lizán L, San L, Escobar R, Paz S. Validation of the Excited Component of the Positive and Negative Syndrome Scale (PANSS-EC) in a naturalistic sample of 278 patients with acute psychosis and agitation in a psychiatric emergency room. Health Qual Life Outcomes. 2011;9:18.
Citrome L. Dexmedetomidine sublingual film for agitation. Curr Psychiatry. 2022;21(6):34–8.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington: APA (American Psychiatric Association); 2013.
Guy W. ECDEU assessment manual for psychopharmacology. Rockville, MD: U.S. Dept. of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs; 1976.
Meehan KM, Wang H, David SR, et al. Comparison of rapidly acting intramuscular olanzapine, lorazepam, and placebo: a double-blind, randomized study in acutely agitated patients with dementia. Neuropsychopharmacology. 2002;26(4):494–504.
Battaglia J, Lindborg SR, Alaka K, Meehan K, Wright P. Calming versus sedative effects of intramuscular olanzapine in agitated patients. Am J Emerg Med. 2003;21(3):192–8.
Citrome L. Compelling or irrelevant? Using number needed to treat can help decide. Acta Psychiatr Scand. 2008;117(6):412–9.
Citrome L. Relative vs. absolute measures of benefit and risk: what's the difference? Acta Psychiatr Scand. 2010;121(2):94–102.
Acknowledgements
Funding
Sponsorship for this analysis, the clinical trials upon which the analysis is based, and the publisher’s Rapid Service and Open Access fees were funded by BioXcel Therapeutics, Inc, New Haven, CT.
Medical Writing and Editorial Assistance
The authors acknowledge the assistance of Chris Caiazza for medical writing and Alix Bennett, PhD of BioXcel Therapeutics for editing in the development of this manuscript. Support for this assistance was provided by BioXcel Therapeutics, Inc, New Haven, CT.
Authorship
All authors contributed to the conceptualization of this analysis, preparation and review of the manuscript, and decision to submit for publication. The analysis was conducted by Leslie Citrome and Heather Robison. All authors read and approved the final manuscript.
Author Contributions
Leslie Citrome—concept and design, statistical analysis, drafting the manuscript. Lavanya Rajachandran—concept and design, drafting the manuscript. Robert Risinger—concept and design, drafting the manuscript. Heather Robison—concept and design, statistical analysis, drafting the manuscript.
Prior Presentation
This analysis was previously presented at the Academy of Managed Care Pharmacists Nexus conference, October 20, 2021, Denver, CO, and abstract published in Citrome L, et al. Journal of Managed Care Specialty Pharmacy. 2021; 27(10-a): S60-61. Some of the data upon which this analysis is based have been published in the Journal of the American Medical Association, 2022; 327(8);727–736, are in press in the Journal of Clinical Psychiatry and have been have been presented previously at the American Psychiatric Association, May 3, 2021, Virtual; Society for Academic Emergency Medicine, May 11, 2022, New Orleans, LA; International Society of Bipolar Disorders, May 15, 2021, Virtual; International Society of Bipolar Disorders, June 10, 2022, Virtual; American College of Emergency Physicians, October 25, 2021, Boston, MA; Psych Congress, October 30, 2021, San Antonio, TX; Neuroscience Education Institute, November 5, 2021, Colorado Springs, CO; American Society of Health Systems Pharmacists, December 5, 2021, Virtual; and American Academy of Emergency Psychiatry, December 9, 2021, Las Vegas, NV.
Disclosures
Leslie Citrome, MD, MPH, reported serving as chair of the drug monitoring committee for the clinical trials upon which this analysis is based, and as consultant to AbbVie/Allergan, Acadia, Adamas, Alkermes, Angelini, Astellas, Avanir, Axsome, BioXcel, Boehringer Ingelheim, Cadent Therapeutics, Eisai, Enteris BioPharma, HLS Therapeutics, Impel, Intra-Cellular Therapies, Janssen, Karuna, Lundbeck, Lyndra, Medavante-ProPhase, Merck, Neurocrine, Novartis, Noven, Otsuka, Ovid, Relmada, Reviva, Sage, Sunovion, Supernus, Teva, University of Arizona, and one-off ad hoc consulting for individuals/entities conducting marketing, commercial, or scientific scoping research; speaker for AbbVie/Allergan, Acadia, Alkermes, Angelini, Eisai, Intra-Cellular Therapies, Janssen, Lundbeck, Neurocrine, Noven, Otsuka, Sage, Sunovion, Takeda, Teva, and CME activities organized by medical education companies such as Medscape, NACCME, NEI, Vindico, and Universities and Professional Organizations/Societies; stock ownership (small number of shares of common stock) in Bristol-Myers Squibb, Eli Lilly, J & J, Merck, Pfizer purchased > 10 years ago, stock options: Reviva; and royalties from Wiley (Editor-in-Chief, International Journal of Clinical Practice, through end 2019), UpToDate (reviewer), Springer Healthcare (book), Elsevier (Topic Editor, Psychiatry, Clinical Therapeutics). Robert Risinger, Lavanya Rajachandran, and Heather Robison are employees of BioXcel Therapeutics.
Compliance with Ethics Guidelines
The clinical trials upon which this analysis was based were conducted in accordance with Good Clinical Practices and the Declaration of Helsinki and were approved by the institutional review board or ethics committee at each participating site. All patients provided written informed consent before any study procedures were undertaken.
Data Availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original online version of this article was revised due to update in the article text.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Citrome, L., Risinger, R., Rajachandran, L. et al. Sublingual Dexmedetomidine for Agitation Associated with Schizophrenia or Bipolar Disorder: A Post Hoc Analysis of Number Needed to Treat, Number Needed to Harm, and Likelihood to be Helped or Harmed. Adv Ther 39, 4821–4835 (2022). https://doi.org/10.1007/s12325-022-02274-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02274-3