Abstract
Aims
To evaluate the efficacy and safety of elobixibat in patients with diabetes and concomitant chronic constipation.
Methods
This was a single-center, single-arm study. Thirty-three patients with diabetes and chronic constipation, as defined by the Rome IV criteria, were treated with elobixibat (10 mg/day) for 8 weeks. Patients recorded stool properties, including spontaneous bowel movements (SBMs) and stool consistency, according to the Bristol Stool Form Scale (BSFS). Quality of life for constipation was evaluated with the Japanese version of the Patient Assessment of Constipation Quality of Life (JPAC-QOL).
Results
Of the 33 eligible patients, 30 completed the study. Elobixibat significantly increased the median (interquartile range) frequency of SBMs per week, from 5.0 (3.0–7.0) at baseline to 6.0 (4.0–7.0] at week 8 (p = 0.030). After 8 weeks, the BSFS score approached 4; the score for normal stool consistency and the JPAC-QOL score significantly improved from 1.05 ± 0.40 at baseline to 0.94 ± 0.53 (p = 0.048); and glycated albumin and serum lipid profiles significantly improved. Stratified analysis revealed that SBMs increased especially in patients with low SBM frequency, in particular in women, older adults, patients without overweight, patients with a long duration of constipation, and patients with diabetic neuropathy. No serious adverse events occurred.
Conclusions
Among patients with diabetes who met the Rome IV criteria for constipation, elobixibat was effective, especially in those with few SBMs at baseline. Improvements in lipid profiles could be an advantage of elobixibat compared with other laxatives.
Clinical Trial Registry
Japan Registry of Clinical Trials registration number: jRCTs031190092
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
To evaluate the efficacy and safety of elobixibat in the treatment of chronic constipation in patients with diabetes. |
The effect of elobixibat on glycolipid metabolism was also investigated because elobixibat increases glucagon-like peptide-1, one of the incretin hormones that stimulates insulin secretion. |
What was learned from the study? |
The results showed that elobixibat increased spontaneous bowel movements and improved lipid profiles in patients with diabetes. |
These results may help physicians to select the optimum laxative for patients with diabetes and concomitant chronic constipation. |
Introduction
Diabetes is a metabolic disorder characterized by chronic hyperglycemia due to defects in insulin secretion or action. Chronic exposure to hyperglycemia causes microvascular complications, such as neuropathy, retinopathy, and nephropathy. Also, patients with diabetes often develop chronic constipation, the prevalence of which in patients with diabetes has been reported to range from 10% to 60%, depending on the country and the definition of constipation applied [1,2,3,4,5]. In recent years, chronic constipation has been reported to increase overall mortality and cardiovascular events [6]. Although the mechanism by which chronic constipation develops in diabetes is not fully understood, diabetic enteric neuropathy due to neurodegeneration caused by apoptosis, oxidative stress, and decreased neuronal growth factor might be associated with its pathophysiology [7, 8].
Diet and exercise therapy are initially recommended for the treatment of chronic constipation. However, the limited efficacy of these lifestyle modifications often results in the introduction of various laxatives as the next-step treatment [9]. In Japan, pharmacological treatment of chronic constipation often comprises stimulant laxatives, such as senna compounds and sodium picosulfate, and salt laxatives, such as magnesium oxide [10]. Although it has been reported that long term use of stimulant laxatives rarely causes tolerance [11], magnesium oxide use can cause hypermagnesemia [12].
Elobixibat, a novel treatment for chronic constipation, was approved in January 2018 in Japan. It is the world's first inhibitor of ileal bile acid transporter (IBAT), also called apical-dependent bile acid transporter. Elobixibat inhibits IBAT at the terminal ileum and suppresses the reabsorption of bile acids, which interrupts the enterohepatic circulation and upregulates hepatic bile acid synthesis [13]. The increased bile acids flowing into the large intestine accelerate colonic transit by stimulating water and electrolyte secretion [14] and inducing high-amplitude colon contraction waves [15]. Because of these dual functions, which are completely different mechanisms from those of existing therapeutic agents, elobixibat represents a new treatment option for constipation. The Japanese phase III trial of elobixibat confirmed that the drug improves the number of spontaneous bowel movements (SBMs) compared with placebo in patients with chronic constipation [16]. However, the efficacy and safety of elobixibat in the treatment of chronic constipation in patients with diabetes have not yet been investigated.
A previous study confirmed that elobixibat increases the plasma concentration of glucagon-like peptide-1 (GLP-1) [17], one of the incretin hormones that stimulates insulin secretion in a glucose-dependent manner. In addition, elobixibat was found to decrease plasma cholesterol levels [18, 19].
Therefore, the purpose of this study was to investigate the efficacy and safety of elobixibat in patients with diabetes and chronic constipation. The study also aimed to explore whether elobixibat affects glycolipid metabolism.
Methods
Study Design
This was an 8-week, prospective, single-center, single-arm study. Participants were recruited between October 2019 and January 2021 at the outpatient clinic of the St. Marianna University Hospital (Kawasaki, Japan). The certified review board (Hattori Clinic, Tokyo, Japan; reference number: CRB3180027) reviewed and approved this study protocol, which complies with the revised ethical guidelines of the 1964 Declaration of Helsinki. This study was registered with the Japan Registry of Clinical Trials (registration number: jRCTs031190092). Written informed consent was obtained from all patients.
Participants
Outpatients who met all of the following criteria were eligible for inclusion: (1) man or woman aged ≥ 20 years; (2) diagnosis of diabetes (irrespective of diabetes type); (3) chronic functional constipation as defined by the Rome IV criteria [20] (i.e., subjective symptoms have been present for > 6 months, and [i] at least two of the following six criteria were met in the last 3 months: straining for more than one-fourth of bowel movements; a sensation of anorectal obstruction/blockage or difficulty with evacuation for more than one-fourth of bowel movements; lumpy or hard stools for more than one-fourth of bowel movements; manual maneuvers or enemas/suppositories to facilitate evacuation for more than one-fourth of bowel movements; sensation of incomplete evacuation for more than one-fourth of the bowel movements; and fewer than three SBMs per week; [ii] loose stools are rarely present without the use of laxatives; and [iii] insufficient criteria for a diagnosis of irritable bowel syndrome).
The exclusion criteria were as follows: (1) history of hypersensitivity to elobixibat; (2) confirmed or suspected intestinal obstruction due to tumor, hernia, etc.; (3) severe liver dysfunction (aspartate aminotransferase and/or alanine aminotransferase levels more than threefold the upper limit of the normal range); (4) suspected biliary obstruction or decreased bile secretion; (5) suspected organic constipation; (6) in women, pregnancy, possible pregnancy, planned pregnancy, or breastfeeding; (7) treatment with ursodeoxycholic acid, chenodeoxycholic acid, aluminum-containing preparations (sucralfate hydrate, aldioxa, etc.), bile acid sequestrants (cholestyramine, colestimide), digoxin, dabigatran etexilate, or midazolam; (8) any change in oral antidiabetic therapy within the 12 weeks before recruitment; (9) variation in hemoglobin A1c (HbA1c) by ≥ 0.5% during the 12 weeks before recruitment; (10) a history of hospitalization to improve glycemic control within the past 6 months; and (11) considered to be ineligible for other reasons at the discretion of the attending physician.
Procedures
To avoid the effects of previous treatment, all patients participated in a 12-week run-in period, the last 2 weeks of which were defined as the baseline period. All medications, including laxatives, were continued without dose changes during the study period. Participants were informed by telephone to start keeping a daily stool diary 2 weeks before the first visit. At the first visit, patients underwent abdominal ultrasonography to confirm that no biliary obstruction was present and were instructed to take a 10-mg dose of elobixibat (2 tablets of 5 mg) orally once daily before breakfast from the next day for 8 weeks. The dose of elobixibat could be adjusted or withdrawn depending on the symptoms, but, according to the package insert, the maximum dose was 15 mg/day. For each bowel movement, patients continued to use their stool diary to record the following stool properties: presence or absence of sensation of incomplete evacuation; stool consistency assessed with the 7-point Bristol Stool Form Scale (BSFS) [21]; bowel movement time; and daily dose of elobixibat. The diaries were reviewed at the start of treatment and at 4 and 8 weeks after initiation of therapy. At each visit, blood and urine tests were performed, patients were weighed, and quality of life (QOL) for constipation was evaluated with a validated Japanese version of the Patient Assessment of Constipation Quality of Life (JPAC-QOL: Mapi Research Trust, Lyon, France) [22]. The JPAC-QOL consists of four subscales (worries and concerns, physical discomfort, psychosocial discomfort, and satisfaction with bowel habits) with a total of 28 questions, which are rated by patients on a 5-item Likert scale; the lower the score, the better the QOL. During the dosing phase, side effects and treatment compliance were recorded by patients in their stool diary and evaluated by the study investigators.
Outcomes
Primary Outcome
The primary outcome was the change from baseline to 8 weeks in the weekly frequency of SBMs as recorded in the patient’s daily stool diary. An SBM was defined as a bowel movement that occurred without the use of laxative suppository, enema, or digital evacuation.
Secondary Outcomes
Secondary outcomes included endpoints for constipation, glycolipid metabolism, and safety.
Endpoints for constipation were weekly changes from baseline to 8 weeks in the time required for the first SBM after administration of elobixibat, in the BSFS score, and in the frequency of weekly complete SBMs (a completed SBM was defined as a bowel movement with no sense of remaining stool without the use of a laxative suppository, enema, or digital evacuation); changes from baseline to 4 or 8 weeks in the JPAC-QOL score; and the proportion of patients who had the first SBM within 24 or 48 h after the initial administration of elobixibat.
Endpoints for glycolipid metabolism were changes from baseline to 8 weeks in fasting plasma glucose (FPG), HbA1c, glycated albumin (GA), cholesterol (total, low-density lipoprotein-cholesterol [LDL-C], and high-density lipoprotein-cholesterol [HDL-C]), and triglyceride levels.
Safety endpoints were the incidence of adverse drug reactions and adverse events (AEs), which were recorded throughout the study period and assessed by investigators regarding the type, severity, and causal relationship with the treatment.
Statistical Analysis
The normality of data was checked with the Shapiro-Wilk test. Results are reported as mean ± standard deviation (SD) or median (interquartile range [IQR]) depending on the data distribution. The determination of sample size was based on a previous study of lubiprostone, a laxative in one of the other new classes of laxatives, in patients with diabetes [23]. We recruited 46 patients in case of dropouts. The change from baseline to the end of the intervention at week 8 and the 95% confidence interval of the difference were calculated. Paired t tests and Wilcoxon signed rank tests were used to evaluate changes from before to after the intervention.
Stratified exploratory analyses were performed to identify patients with diabetes who were suitable for treatment with elobixibat and to assess the confounding of risk factors with or without diabetic complications, in particular autonomic neuropathy and sensory neuropathy. Autonomic neuropathy was defined by orthostatic hypotension; we used the most widely accepted definition of orthostatic hypotension (i.e., a decline in systolic blood pressure ≥ 20 mmHg or in diastolic blood pressure ≥ 10 mm Hg from sitting to standing within 3 min) [24]. Sensory neuropathy was assessed by Achilles’ tendon reflex, Semmes-Weinstein monofilament tests (i.e., if patients could not perceive the monofilament size ≥ 3.61), and tuning fork tests (i.e., if patients could not perceive the vibrations of C 128-Hz tuning forks for > 10 s).
A two-sided t test was also performed as an exploratory analysis to compare the changes from baseline to 8 weeks between each of the stratified groups.
All analyses were performed with SAS 9.4 software (SAS Institute Inc., Carey, NC, USA) by an independent contract research organization (Satt Co Ltd., Tokyo, Japan). Significance was accepted for p values < 0.05.
Results
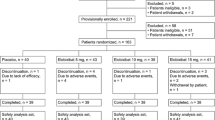
Figure 1 shows the flowchart of participant enrollment in the study. Informed consent was obtained from 46 patients, but 12 of these were excluded because it was determined that they were not eligible for the study. Of the 34 eligible patients who were enrolled in the study, one withdrew consent before the administration of elobixibat. Thus, data from 33 patients were analyzed as the full analysis set (FAS) and safety analysis set. Three patients were determined to have deviated from the protocol because they took elobixibat too infrequently and forgot to take it on the starting date. Consequently, the per-protocol set (PPS) included 30 patients. Because neither the FAS nor the PPS analysis showed a statistically significant difference, the results for all endpoints except the primary one were described only in the PPS.
The baseline characteristics of the patients are shown in Table 1. All participants were Japanese, and 19 (63.3%) were women. The mean (± SD) age was 63.3 ± 12.3 years, mean body mass index (BMI) was 25.9 ± 4.0 kg/m2, and mean duration of diabetes was 14.0 ± 9.5 years. Twenty-nine (96.7%) patients had type 2 diabetes, while only one patient (3.3%) had type 1 diabetes. The mean HbA1c and GA were 7.0% ± 0.9% [52 ± 14 mmol/mol] and 18.9% ± 4.5%, respectively. Regarding diabetic complications, eight (26.7%) patients had autonomic neuropathy and 19 (63.3%) had sensory neuropathy. A total of 14 patients (46.7%) used other laxatives. The mean weekly dose of elobixibat was ≤ 5 mg in five patients; > 5 mg, ≤ 10 mg in 15 patients; and > 10 mg ≤ 15 mg in ten patients. None of the patients had biliary obstruction as assessed by abdominal ultrasonography.
Primary Outcome
The primary outcome of the change in weekly SBMs showed a significant increase at the end of the study in both the FAS, from a median of 5.0 (IQR 3.0–7.0) at baseline to 6.0 (IQR 4.0–7.0) at 8 weeks (p = 0.030) and the PPS, from a median of 5.0 (IQR 3.0–7.0) at baseline to 6.0 (IQR 4.0–7.0) at 8 weeks (p = 0.017) (Fig. 2).
Changes from baseline to week 8 (end of study) in the weekly frequency of spontaneous bowel movements with elobixibat treatment. The left side of the bar graphs shows the results for the full analysis set (n = 33), and the right side of the bar graphs show the results for the per protocol set (n = 30). Data are expressed as the median, and the bars represent the interquartile range. The asterisk indicates a significant difference from baseline at *p < 0.05. SBMs Spontaneous bowel movements
Secondary Outcomes
Constipation-Related Parameters
The frequency of SBMs per week and of complete SBMs per week both increased significantly 1 week after the initiation of elobixibat; the frequency of SBMs per week was significantly higher also in weeks 2, 5, 7, and 8, and the frequency of complete SBMs per week was significantly higher every week until week 8 (Fig. 3a, b). Although the BSFS score did not show a significant change after 8 weeks of treatment, it did increase significantly up to 4 weeks, then decreased and approached 4, the score for normal stool consistency (Fig. 3c). In each week, the mean time from taking elobixibat to the first SBM was about 20 h (Fig. 3d). The proportions of patients with the first SBM within 24 and 48 h after the initial administration of elobixibat were 78.1% and 93.8%, respectively.
Treatment effect of elobixibat each week for 8 weeks. a Frequency of SBMs per week, b frequency of complete SBMs per week, c Bristol Stool Form Scale score, d time required for the first SBM after initiation of elobixibat treatment. Data are expressed as the mean ± standard deviation. Asterisks indicate a significant difference from baseline at *p < 0.05, **p < 0.01
Table 2 shows the effect of elobixibat on the JPAC-QOL score. The total score showed a nonsignificant decrease at 4 weeks and a significant decrease at 8 weeks (p = 0.136 and p = 0.048, respectively). Furthermore, the satisfaction score decreased significantly after both 4 and 8 weeks (p = 0.040 and p = 0.027, respectively), indicating an improvement in QOL.
Glycolipid Metabolism-Related Parameters
Table 3 shows the effects of elobixibat on glycolipid metabolism. Although no significant difference was observed in HbA1c, GA decreased significantly, and FPG tended to decrease. After 8 weeks of treatment with elobixibat, serum LDL-C was significantly decreased and serum HDL-C was significantly increased, but no significant differences were observed in serum total cholesterol or triglyceride. In this study, no exclusion criteria for lipid-related parameters were defined. During the study period, lipid medications were not changed except in one patient. However, the statistical significance was still present (p = 0.036), even when this patient was excluded from the analysis.
Supplementary Data
The tables in the electronic supplementary material (ESM) show the data obtained from the analyses stratified by sex (ESM Table S1), age (ESM Table S2), BMI (ESM Table S3), duration of chronic constipation (ESM Table S4), presence or absence of autonomic neuropathy (ESM Table S5), and presence or absence of sensory neuropathy (ESM Table S6). Patients with a low SBM frequency at baseline, i.e., women, older people, and patients without overweight, with a long duration of constipation, and with autonomic neuropathy and sensory neuropathy, showed a significant (ESM Tables S1, S2, S3, and S4) or near-significant (ESM Table S5 and S6) increase in SBM frequency. Patients who exhibited significant increases in BSFS score, i.e., men or patients without overweight or with autonomic neuropathy, showed no significant improvement in JPAC-QOL scores (ESM Tables S1, S3, and S5).
Regarding safety endpoints, no serious AEs occurred during the study period. One patient was withdrawn from the study because of diarrhea as a possible AE (1/33, 3.0%), and the diarrhea improved promptly after the administration of elobixibat was discontinued.
Discussion
In the present study, we evaluated the effects of elobixibat, a novel laxative that inhibits IBAT, in Japanese patients with diabetes and concomitant chronic constipation. We obtained four main findings. First, administration of elobixibat significantly increased the weekly frequency of SBMs as the primary outcome. Second, after 8 weeks of treatment with elobixibat, stool form became normal and the total JPAC-QOL score improved significantly because of improvement in the satisfaction domain. Third, although no significant changes were observed in glucose metabolism, significant improvements were observed in lipid metabolism. Fourth, stratified analysis revealed that the increase in the weekly frequency of SBMs was observed in particular in patients with a low frequency of SBMs at baseline. No serious AEs occurred in this study. This is the first report showing the efficacy and safety of elobixibat in patients with diabetes and concomitant chronic constipation.
Although elobixibat increased the weekly frequency of SBMs, the increase of 1.0 SBM per week was small. This result is not surprising because the baseline frequency of SBMs was not low and participants’ treatment, including laxatives, was not changed during the study period. In the phase 2b trial of elobixibat, the mean changes in SBMs after 1 week of treatment at the doses of 5, 10, and 15 mg/day were 3.5, 5.7, and 5.6 per week, respectively [25]. Also in the phase 3 trial of elobixibat, the mean change in SBMs after 2 weeks of treatment was 5.0 per week [16]. These differences between the present study and the earlier studies were probably due to the difference in the inclusion criteria in each study. In the phase 2b and 3 trials described above, in addition to the Rome III criteria, the inclusion criteria limited SBMs to < 3 per week. However, in accordance with the Rome IV criteria, which were published in 2016 [20], we did not set an upper limit on the SBM frequency in the present study. Moreover, in the earlier studies, no other laxatives were permitted, and a washout period was used; however, in our study we did not change patients’ treatment, including laxatives. Thus, our study results more closely reflect the situation in a clinical setting.
After 4 weeks of treatment, the BSFS score significantly increased, but the total JPAC-QOL score did not change. However, after 8 weeks of treatment, the BSFS score approached the normal value of 4 and the total JPAC-QOL score significantly improved. The stratified analyses revealed that in men, patients with a BMI < 25 kg/m2, and patients with autonomic neuropathy, the total JPAC-QOL scores did not significantly improve even though the BSFS scores increased significantly. These results suggest that an increase in the BSFS score to > 4 may not improve QOL, probably because a BSFS score of 4 indicates a normal stool consistency. This hypothesis is consistent with the results of a previous study in which improvement of the PAC-QOL score was observed in patients with a BSFS score of 4, whereas more than half of patients with a BSFS score of 6 or 7 reduced their intake of elobixibat because of excessive effects [26].
Regarding glucose metabolism, we expected that elobixibat may improve glucose control in patients with diabetes because it was reported to increase plasma GLP-1 levels [17]. However, in the present study no significant difference was observed in FPG or HbA1c. The previous study used an elobixibat dose of ≥ 15 mg, whereas the mean elobixibat dose in our study was 10 mg, which might have been insufficient to improve FPG and HbA1c. However, GA, which is considered to represent the mean blood glucose level over the last 2–3 weeks [27, 28], decreased significantly in the present study. Previously, we reported that GA, but not HbA1c, was decreased when postprandial hypoglycemic drugs were given to patients with well-controlled type 2 diabetes [29]. Thus, elobixibat may improve glucose metabolism by reducing postprandial plasma glucose. A further study with a larger sample size and longer duration is needed to reveal the effect of elobixibat on glucose metabolism.
Regarding lipid metabolism, elobixibat is known to decrease serum LDL-C levels by inhibiting bile acid reabsorption in the ileum [17,18,19]. In this study, elobixibat not only decreased LDL-C levels but also increased HDL-C levels significantly. The underlying mechanism for this effect is unknown. Diabetes, low HDL-C, and high LDL-C are known to be important, independent risk factors for future cardiovascular events [30, 31]. Furthermore, constipation is also known to increase cardiovascular events [32]. Thus, because elobixibat improves both serum lipid profiles and constipation, it may help to decrease the risk of cardiovascular disease in patients with diabetes and concomitant chronic constipation and dyslipidemia.
In the stratified analysis, elobixibat significantly increased SBM frequency in patients with low baseline SBMs, in particular women, older patients (≥ 65 years), patients without overweight (BMI < 25 kg/m2), patients with a long duration of constipation (≥ 10 years), and patients with autonomic neuropathy and sensory neuropathy. However, our findings in these subgroups are preliminary because of the relatively small number of participants in each stratum and possibly because of multiple tests.
Noteworthy is that participants in our study had fewer AEs than those in the other studies. In the phase 2b trial, diarrhea occurred in 8%, 6%, and 13% of patients in the 5-, 10-, and 15-mg elobixibat groups, respectively [25]. In the phase 3 trial, diarrhea and abdominal pain occurred in 30% of patients [16]. However, in the present study, diarrhea occurred in only 3% of participants, which is consistent with a recent interim report from a post-marketing surveillance study [33]. Thus, the inconsistent findings are probably due to differences between clinical trials and real-world settings.
The present study had a number of limitations, including the small sample size and single-center, open-label, single-arm design. Therefore, randomized controlled trials are needed to confirm the efficacy of elobixibat. Moreover, all patients were Japanese. Although the efficacy of elobixibat in White people and African Americans without diabetes has been confirmed [17,18,19], further research is needed to determine the efficacy in patients with diabetes among other races. Despite these limitations, the present results may help physicians to select the optimum laxative for patients with diabetes and concomitant chronic constipation.
Conclusion
We confirmed the efficacy and safety of elobixibat in patients with diabetes and concomitant chronic constipation. Among patients who met the Rome IV criteria, elobixibat appeared to be effective in those with low SBM frequency, in particular women, older adults, patients without overweight, patients with a long duration of constipation, and patients with diabetic neuropathy. In addition, improvements in lipid profiles could be an advantage of elobixibat compared with other laxatives.
References
Feldman M, Schiller LR. Disorders of gastrointestinal motility associated with diabetes mellitus. Ann Intern Med. 1983;98(3):378–84. https://doi.org/10.7326/0003-4819-98-3-378.
Janatuinen E, Pikkarainen P, Laakso M, Pyörälä K. Gastrointestinal symptoms in middle-aged diabetic patients. Scand J Gastroenterol. 1993;28(5):427–32. https://doi.org/10.3109/00365529309098244.
Enck P, Rathmann W, Spiekermann M, et al. Prevalence of gastrointestinal symptoms in diabetic patients and non-diabetic subjects. Z Gastroenterol. 1994;32(11):637–41.
Schvarcz E, Palmér M, Ingberg CM, Aman J, Berne C. Increased prevalence of upper gastrointestinal symptoms in long-term type 1 diabetes mellitus. Diabet Med. 1996;13(5):478–81. https://doi.org/10.1002/(SICI)1096-9136(199605)13:5%3c478::AID-DIA104%3e3.0.CO;2-5.
Maleki D, Locke GR 3rd, Camilleri M, et al. Gastrointestinal tract symptoms among persons with diabetes mellitus in the community. Arch Intern Med. 2000;160(18):2808–16. https://doi.org/10.1001/archinte.160.18.2808.
Sumida K, Molnar MZ, Potukuchi PK, et al. Constipation and risk of death and cardiovascular events. Atherosclerosis. 2019;281:114–20. https://doi.org/10.1016/j.atherosclerosis.2018.12.021.
Yarandi SS, Srinivasan S. Diabetic gastrointestinal motility disorders and the role of enteric nervous system: current status and future directions. Neurogastroenterol Motil. 2014;26(5):611–24. https://doi.org/10.1111/nmo.12330.
Yamada E, Namiki Y, Takano Y, et al. Clinical factors associated with the symptoms of constipation in patients with diabetes mellitus: a multicenter study. J Gastroenterol Hepatol. 2018;33(4):863–8. https://doi.org/10.1111/jgh.14022.
Prasad VG, Abraham P. Management of chronic constipation in patients with diabetes mellitus. Indian J Gastroenterol. 2017;36(1):11–22. https://doi.org/10.1007/s12664-016-0724-2.
Mori H, Tack J, Suzuki H. Magnesium oxide in constipation. Nutrients. 2021;13(2):421. https://doi.org/10.3390/nu13020421.PMID:33525523.
Müller-Lissner SA, Kamm MA, Scarpignato C, Wald A. Myths and misconceptions about chronic constipation. Am J Gastroenterol. 2005;100(1):232–42. https://doi.org/10.1111/j.1572-0241.2005.40885.x.
Mori H, Suzuki H, Hirai Y, et al. Clinical features of hypermagnesemia in patients with functional constipation taking daily magnesium oxide. J Clin Biochem Nutr. 2019;65(1):76–81. https://doi.org/10.3164/jcbn.18-117.
Acosta A, Camilleri M. Elobixibat and its potential role in chronic idiopathic constipation. Therap Adv Gastroenterol. 2014;7(4):167–75. https://doi.org/10.1177/1756283X14528269.
Wingate DL, Krag E, Mekhjian HS, Phillips SF. Relationships between ion and water movement in the human jejunum, ileum and colon during perfusion with bile acids. Clin Sci Mol Med. 1973;45(5):593–606. https://doi.org/10.1042/cs0450593.
Bampton PA, Dinning PG, Kennedy ML, Lubowski DZ, Cook IJ. The proximal colonic motor response to rectal mechanical and chemical stimulation. Am J Physiol Gastrointest Liver Physiol. 2002;282(3):G443-9. https://doi.org/10.1152/ajpgi.00194.2001.
Nakajima A, Seki M, Taniguchi S, et al. Safety and efficacy of elobixibat for chronic constipation: results from a randomised, double-blind, placebo-controlled, phase 3 trial and an open-label, single-arm, phase 3 trial. Lancet Gastroenterol Hepatol. 2018;3(8):537–47. https://doi.org/10.1016/S2468-1253(18)30123-7.
Rudling M, Camilleri M, Graffner H, Holst JJ, Rikner L. Specific inhibition of bile acid transport alters plasma lipids and GLP-1. BMC Cardiovasc Disord. 2015;15:75. https://doi.org/10.1186/s12872-015-0070-9.
Simrén M, Bajor A, Gillberg PG, Rudling M, Abrahamsson H. Randomised clinical trial: the ileal bile acid transporter inhibitor A3309 vs. placebo in patients with chronic idiopathic constipation–a double-blind study. Aliment Pharmacol Ther. 2011;34(1):41–50. https://doi.org/10.1111/j.1365-2036.2011.04675.x.
Chey WD, Camilleri M, Chang L, Rikner L, Graffner H. A randomized placebo-controlled phase IIb trial of a3309, a bile acid transporter inhibitor, for chronic idiopathic constipation. Am J Gastroenterol. 2011;106(10):1803-12. https://doi.org/10.1038/ajg.2011.162. Erratum in: Am J Gastroenterol. 2014;109(5):782
Drossman DA, Hasler WL. Rome IV-functional GI disorders: disorders of gut-brain interaction. Gastroenterology. 2016;150(6):1257–61. https://doi.org/10.1053/j.gastro.2016.03.035.
Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997;32(9):920–4. https://doi.org/10.3109/00365529709011203.
Tsunoda A, Yamada K, Takano M, Kusanagi H. The translation and validation of the Japanese version of the patient assessment of constipation quality of life scale. Surg Today. 2016;46(4):414–21. https://doi.org/10.1007/s00595-015-1179-2.
Christie J, Shroff S, Shahnavaz N, et al. A Randomized, double-blind, placebo-controlled trial to examine the effectiveness of lubiprostone on constipation symptoms and colon transit time in diabetic patients. Am J Gastroenterol. 2017;112(2):356–64. https://doi.org/10.1038/ajg.2016.531.
Kaufmann H. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure and multiple system atrophy. Clin Auton Res. 1996;6(2):125–6. https://doi.org/10.1007/BF02291236.
Nakajima A, Seki M, Taniguchi S. Determining an optimal clinical dose of elobixibat, a novel inhibitor of the ileal bile acid transporter, in Japanese patients with chronic constipation: a phase II, multicenter, double-blind, placebo-controlled randomized clinical trial. J Gastroenterol. 2018;53(4):525–34. https://doi.org/10.1007/s00535-017-1383-5.
Ohkubo H, Yoshihara T, Misawa N, et al. Relationship between stool form and quality of life in patients with chronic constipation: an internet questionnaire survey. Digestion. 2021;102(2):147–54. https://doi.org/10.1159/000502815.
Ribeiro RT, Macedo MP, Raposo JF. HbA1c, fructosamine, and glycated albumin in the detection of dysglycaemic conditions. Curr Diabetes Rev. 2016;12(1):14–9. https://doi.org/10.2174/1573399811666150701143112.
Zendjabil M. Glycated albumin. Clin Chim Acta. 2020;502:240–4. https://doi.org/10.1016/j.cca.2019.11.007.
Ohta A, Ohshige T, Sakai K, et al. Comparison of the hypoglycemic effect of sitagliptin versus the combination of mitiglinide and voglibose in drug-naïve Japanese patients with type 2 diabetes. Expert Opin Pharmacother. 2013;14(17):2315–22. https://doi.org/10.1517/14656566.2013.842554.
Booth GL, Kapral MK, Fung K, Tu JV. Relation between age and cardiovascular disease in men and women with diabetes compared with non-diabetic people: a population-based retrospective cohort study. Lancet. 2006;368(9529):29–36. https://doi.org/10.1016/S0140-6736(06)68967-8.
Ference BA, Ginsberg HN, Graham I, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017;38(32):2459–72. https://doi.org/10.1093/eurheartj/ehx144.
Salmoirago-Blotcher E, Crawford S, Jackson E, Ockene J, Ockene I. Constipation and risk of cardiovascular disease among postmenopausal women. Am J Med. 2011;124(8):714–23. https://doi.org/10.1016/j.amjmed.2011.03.026.
Nakajima A, Fujimaki M, Arai Y, Emori K. Safety and Efficacy of Elobixibat, an Ileal Bile Acid Transporter Inhibitor, in Elderly Patients With Chronic Idiopathic Constipation According to Administration Time: Interim Analysis of Post-marketing Surveillance. J Neurogastroenterol Motil. 2022;28(3):431–41. https://doi.org/10.5056/jnm20263.
Acknowledgements
We thank the patients and investigators who participated in these trials. The authors are indebted to Yuko Yasuda for her expert assistance
Funding
This study was funded by EA Pharma Co., Ltd. and Mochida Pharmaceutical Co., Ltd.
Other Assistance
Yuko Yasuda, a medical staff of St. Marianna University Hospital (Kawasaki, Japan), participated in the data collection. The authors were fully responsible for all content and editorial decisions, were involved at all stages of development, and provided their approval on the final version.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. The authors did not receive payment for the development of this manuscript.
Author Contributions
YH participated in the conduct, data collection, and interpretation of the clinical trial and wrote the first draft. YN participated in the design, interpretation, and oversight of the clinical trial and edited the draft of the manuscript. HT, YN, and TN participated in the conduct of the clinical trial and data collection. SI and YT participated in application of ileal bile acid transporters (IBAT) in therapeutics in patients with diabetes and in designing and interpreting the clinical trial. MS participated in interpretation and oversight of the clinical trial. All authors had full access to the study data and approved the final draft of the manuscript to be published.
Disclosures
Yoshiaki Hishida and Yoshio Nagai have received research grants from EA Pharma Co., Ltd. and Mochida Pharmaceutical Co., Ltd. Hidekazu Tsukiyama, Yuta Nakamura, Tomoko Nakagawa, Yasushi Tanaka, and Masakatsu Sone declare that they have no competing interests. Sonoko Ishizaki is an employee of EA Pharma Co., Ltd. This study was funded by EA Pharma Co., Ltd., and Mochida Pharmaceutical Co., Ltd. The sponsor had no control over the interpretation, writing, or publication of this manuscript.
Compliance with Ethics Guidelines
The certified review board (Hattori Clinic, Tokyo, Japan; reference number: CRB3180027) reviewed and approved this study protocol, which complies with Clinical Trial Act and the revised ethical guidelines of the 1964 Declaration of Helsinki. This study was registered with the Japan Registry of Clinical Trials (registration number: jRCTs031190092). Informed consent to participate was received from all patients.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hishida, Y., Nagai, Y., Tsukiyama, H. et al. Effects of Elobixibat in Patients with Diabetes and Concomitant Chronic Constipation: an 8-week, Prospective, Single-center, Single-arm Study. Adv Ther 39, 4205–4217 (2022). https://doi.org/10.1007/s12325-022-02243-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02243-w