Abstract
Introduction
Adherence to adjuvant therapy is crucial for effective disease management in patients with resected melanoma. This study assessed patient-reported adherence to adjuvant therapy and identified behavioral/belief constructs associated with adherence in patients with resected melanoma.
Methods
Patients with resected stage III/IV melanoma were recruited through the Melanoma Research Foundation and a patient panel to complete an online survey. Patient characteristics, medical history, and adherence to therapy were captured. In accordance with the theory of planned behavior (TPB), the survey measured behavioral, normative, and control beliefs, and intention to adhere to therapy. Structural equation modeling (SEM) examined their relationships with adherence.
Results
Among all patients who received adjuvant therapy and completed the survey (n = 184), 69% received intravenous and 31% received oral therapy; the majority (85.3%) were somewhat involved in deciding to start therapy. Mean age was 45 years, 44% of patients were female, and 83% had stage III/IV disease at diagnosis. Patients had a mean disease duration of 1.5 years, a time since complete resection of 10 months, and an adjuvant therapy duration of 8 months. Adherence to adjuvant therapy was high overall and higher with intravenous than with oral therapy (98.4% versus 91.2%, P = 0.002). All underlying TPB constructs were significant in the SEM model, which explained 60.3% of the variance in intention to adhere. Control beliefs had the strongest association with intention to adhere (standardized estimate = 0.47, P < 0.001) and intravenous therapy was associated with greater adherence than oral therapy (standardized estimate = 0.26, P < 0.001).
Conclusions
This study found that patients with resected melanoma are highly engaged in the decision to initiate systemic adjuvant therapy, with an overall high adherence rate to prescribed adjuvant treatment. Enhancing patients’ view of their capability to adhere to treatments may further improve the adherence rate to melanoma adjuvant therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
An increasing number of patients with melanoma are being treated with complete surgical resection followed by adjuvant therapy, and adherence to therapies in the real-world setting may not be adequate. |
Understanding the extent of adherence to adjuvant therapy and patients’ considerations when receiving adjuvant therapy may improve decision-making to initiate adjuvant treatment and patient outcomes. |
What was learned from the study? |
Patients with resected melanoma were highly engaged in the decision to initiate systemic adjuvant therapy. |
Adherence to prescribed adjuvant treatment was generally high, with a higher proportion in patients treated with intravenous compared with oral therapy (98.4% versus 91.2%). |
Enhancing patients’ view of their capability to adhere to treatments (control beliefs) may further improve the adherence rate to melanoma adjuvant therapy. |
Introduction
Melanoma is a severe form of malignant skin cancer, with incidence rates rising in recent years. Estimates suggest an annual incidence of 287,700 cases worldwide [1], with 106,110 new cases, excluding in situ carcinomas, in the USA in 2021 [2]. Even with surgical excision as routine care for localized and regionally metastatic melanoma involving lymph nodes, patients remain at a high risk for disease recurrence after complete resection [3].
Systemic adjuvant therapy can lower the risk of recurrence of melanoma and consequently improve survival [4,5,6]. According to the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®), the recommended adjuvant therapy options for resected stage III or stage IV disease include the programmed death 1 (PD-1) inhibitors nivolumab or pembrolizumab, the BRAF plus MEK inhibitor combination of dabrafenib plus trametinib (for disease having a BRAF V600-activating mutation), and observation, among others [7]. Nivolumab and pembrolizumab are administered intravenously every 2 to 6 weeks, whereas dabrafenib and trametinib are taken orally. Two capsules of dabrafenib are taken twice a day and one tablet of trametinib is taken once daily 1 h before or 2 h after a meal. In addition to routine clinical follow-up, adherence to these treatment regimens is crucial for effective disease management. However, patients may not adhere to systemic therapy. Published data on adherence to adjuvant therapies in patients with stage III or stage IV resected melanoma are limited.
A number of factors can affect patient adherence to adjuvant cancer therapy. For example, systematic reviews assessing adherence to adjuvant therapy in breast cancer showed that side effects, forgetfulness, inconvenience, cost, and beliefs about efficacy were associated with low adherence [8], whereas good patient–physician communication and self-efficacy for taking medication were associated with greater adherence [9]. In addition, adjuvant therapies differ in their route of administration, which may also affect patient adherence [10, 11]; however, the literature examining the direct impact of route of administration on adherence is sparse. Given the various factors that affect adherence, a theoretical social-behavioral model framework may offer a comprehensive guide for evaluating the impact of these factors among patients with resected melanoma.
In this study, we applied the theory of planned behavior (TPB) [12] to explore the factors associated with adherence to adjuvant therapy. The TPB suggests that the intention to engage in a behavior (e.g., medication adherence) results from the following three key underlying constructs: behavioral beliefs, normative beliefs, and perceived control beliefs, which can directly influence the actual behavior. Under this framework, TPB defines behavioral beliefs as a person’s positive or negative attitude toward performing the behavior, normative beliefs as the perception of other people (peers) approving or disapproving of the behavior, and perceived control beliefs as a person’s view of their capability to perform the behavior. The TPB has been previously used to assess adherence to medications for chronic conditions [13, 14], including cancer; for example, among patients with breast cancer, the TPB explained a substantial proportion of intentions to adhere to adjuvant endocrine therapy [15] and provided a useful framework for understanding adherence [16]. To the best of our knowledge, no previous study has applied the TPB to the adjuvant setting for resected melanoma.
Given the availability of several adjuvant therapies for resected melanoma, we conducted an online survey for patients with resected melanoma to assess patient-reported adherence to adjuvant therapies, as well as describe patients’ perceived barriers to adherence and identify constructs associated with adherence.
Methods
Study Participants
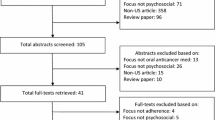
This cross-sectional survey was conducted in patients living in the USA who were members of the Melanoma Research Foundation, a patient advocacy group, or of a patient panel maintained by Dynata, a well-established market research firm that routinely carries out online healthcare surveys. Adult patients diagnosed with self-reported stage III or stage IV melanoma since January 2018 with no evidence of disease after complete surgical resection and without subsequent recurrence or metastases were included; eligible patients must have received adjuvant therapy for at least 2 months. Patients were further classified by the following routes of administration: intravenous therapy (nivolumab or pembrolizumab) or oral therapy (dabrafenib plus trametinib). Patients who were previously treated with other adjuvant therapies were also eligible. Patients were excluded if they were unable to read English or had participated in a clinical trial for melanoma within the past 2 years. The survey captured patients’ sociodemographic and clinical characteristics (including medical and treatment history related to melanoma, comorbidities, overall general well-being, and the extent of engagement when deciding to start adjuvant therapy following complete surgical resection), adherence to adjuvant therapy, and TPB constructs (behavioral, normative, and perceived control beliefs and intentions to adhere). Patients responded to the survey via a secure online portal between November 2019 and January 2020.
This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments and was granted an exemption from a full review by the New England Institutional Research Board. All patients consented to participate.
Measures
Adherence
Adherence to adjuvant therapy was self-reported according to the route of administration. Patients treated with oral adjuvant therapy self-reported how often they took their tablets or capsules on time and as instructed by their physician over the past 2 months, using the following categories: always (100%), almost all of the time (80–99%), just over half of the time (51–79%), about half of the time (50%), slightly less than half of the time (25–49%), or rarely (less than 25%). Patients treated with intravenous adjuvant therapy were asked to report the number of infusions missed over the entire duration of the therapy specified. The number of infusions received was calculated as the difference between the number of prescribed infusions and the number of self-reported missed infusions. Adherence was presented as a percentage, calculated by dividing the number of infusions received by the number of infusions prescribed, according to the dosing schedule. The calculated adherence to intravenous therapy was then characterized using the same categories as oral therapy to allow for comparisons among these measures.
Adherence Barriers
Barriers to adherence were identified through a series of 15 items, which listed reasons for previous and expected future nonadherence, as identified in the literature [17]. These items included the following categories: forgetfulness (forgot the infusion appointment or to take the oral medication), safety and side effect concerns (worried about potential side effects, did not want to become dependent on the medication, on a break from therapy due to side effects), affordability (not covered by insurance or high out-of-pocket costs), avoidance (did not want to be reminded of melanoma, melanoma was out of one’s control, melanoma was not bothering respondent, wanted to take a break from treatment), concerns about efficacy, inconvenience, time constraints (childcare or work-related), and other.
Constructs in the TPB
The survey questions were designed on the basis of targeted literature reviews [12,13,14, 18], patient focus group discussions, and a clinical expert interview. Specifically, to identify the relevant constructs within the melanoma adjuvant therapy setting, the literature review focused on systemic adjuvant therapy options for patients with completely resected melanoma, factors affecting treatment adherence, adherence among patients with cancer treated with adjuvant therapy (with resected melanoma or with other types of advanced cancer), applications of social/behavioral models for adherence in the cancer adjuvant setting, and specific applications of TPB in patients receiving cancer adjuvant therapies. The initial list of constructs was subsequently developed and facilitated the development of semi-structured interview guides for focus group discussions. The applicability of TPB among this patient population was confirmed in the focus group discussions, and direct inputs/feedback from the patients were used to develop the items for each of the constructs.
The question development for TPB constructs were guided by the TPB framework [12]. Responses to all TPB questions used the 5-point Likert scale (e.g., strongly disagree, disagree, neither agree nor disagree, agree, or strongly agree) on behavioral, normative, and perceived control beliefs related to adjuvant therapy and their intent to adhere. Intent to adhere to adjuvant therapy was assessed using the following two items: “I have every intention to follow the dosing schedule for my adjuvant therapy exactly as prescribed” and “In general, how likely are you to take your medication(s) or receive treatments as prescribed?” The draft survey was pretested among two patients who met the same eligibility criteria as study participants.
Statistical Analysis
All analyses were performed using SAS Enterprise Guide software, Version 7.15 of the SAS system for Unix (Copyright© 2017 SAS Institute Inc., Cary, NC, USA). Categorical and continuous variables were summarized descriptively for all participants and for route of administration (intravenous versus oral). Comparisons between cohorts were made using chi-square tests for categorical variables and Wilcoxon rank-sum tests for continuous variables.
Structural equation modeling (SEM) with maximum likelihood estimation was used to evaluate the TPB for factors associated with adherence and to assess the relationship between route of administration (i.e., intravenous versus oral) and adherence. The following two models were run: a base model that examined core TPB concepts and an expanded model that incorporated the route of administration. First, exploratory factor analysis was used to select items that best described the TPB latent constructs. Second, confirmatory factor analysis was used to confirm that the selected items represented the intended factors. These models also included age, sex, race, and education as control variables. Fit indices were used to evaluate model validity (i.e., goodness of fit index [GFI], adjusted GFI, chi-square, Bentler comparative fit index [CFI], root mean square error of approximation [RMSEA], and standardized root mean square residual [SRMR]).
Results
Patient Characteristics
A total of 184 patients completed the survey, including 127 (69.0%) recently/currently treated with intravenous adjuvant therapy (86 with nivolumab and 41 with pembrolizumab) and 57 (31.0%) with an oral adjuvant combination therapy (dabrafenib plus trametinib) (Table 1). The mean age was 44.9 years at the time of the survey, 44.0% of patients were female, and 21.7% were non-White, followed by 9.8% black/African American. On average, participating patients had a disease duration from the initial diagnosis of 18 months, time since complete surgical resection of 10.3 months, and adjuvant treatment duration of 8.1 months. Stage III or stage IV disease at first diagnosis was reported by 83% of patients, and stage III disease at the time of complete resection surgery was reported by 65.8% of patients. Sociodemographic and clinical characteristics were mostly similar between the two cohorts of patients who were treated with intravenous compared with oral combination adjuvant therapy, except for education and employment status. Most patients (81.0%) reported that they felt “good,” “very good,” or “excellent” about their overall well-being. The most commonly self-reported comorbidity among patients was anxiety (11.4%), followed by depression (9.8%).
Patients treated with intravenous therapy compared with those treated with oral therapy were more likely to be employed full-time (66.9% versus 47.4%, P = 0.012) and to have commercial insurance (75.6% versus 47.4%, P < 0.001) (Table 1). A higher proportion of patients treated with oral therapy compared with those treated with intravenous therapy had a higher educational attainment (P = 0.030) and reported involvement in the decision-making process to start adjuvant therapy (P = 0.005; 40.4% versus 23.6% reported a great deal of involvement, and 42.1% versus 31.5% reported quite a bit of involvement) (Table 1).
Adherence to Adjuvant Therapy
The majority of patients (90.2%; 166 of 184) were receiving adjuvant therapy (112 were treated with intravenous therapy and 54 were treated with oral therapy). Self-reported adherence to adjuvant therapy was high, with 96.2% of patients following their regimens always or almost all of the time (Table 2). Adherence was higher in patients treated with intravenous therapy than in those treated with oral therapy (P = 0.002), with 98.4% and 91.2% of patients, respectively, following their regimens always or almost all of the time. In this analysis, 19% of patients treated with intravenous therapy reported missing an infusion compared with 42% of those treated with oral therapy reporting not always following their regimens as instructed (P < 0.001).
Among patients with low adherence (less than 80%), the most common reason for nonadherence was forgetfulness (50.0%) followed by safety and side effect concerns (35.4%; Table 2). Only patients with oral therapy expressed concerns about affordability (45.8% versus 0% in those with intravenous therapy, P < 0.001). A substantial proportion of patients (39.8% overall, 36.6% with intravenous therapy, and 46.3% with oral therapy) anticipated not being able to follow their regimens as prescribed in the future. The largest barriers to adherence in the future were expected to be safety and side effects (66.7%) and affordability (59.1%). A higher proportion of patients treated with oral therapy compared with those treated with intravenous therapy had expected that forgetfulness would be a reason for nonadherence (28.0% versus 4.9%, P = 0.021).
Constructs in the Theory of Planned Behavior
Overall, on a scale from 1 to 5 (strongly agree), patients indicated strong agreement with respect to the importance of behavioral beliefs, including actively managing their melanoma (mean, 4.5 [standard deviation, 0.6]), receiving adjuvant therapy (4.2 [0.7]), and following instructions exactly as prescribed (4.6 [0.6]; Table 3). Patients also strongly agreed with the value of perceived control beliefs, such as having the capability (4.1 [0.8]), having the necessary resources (4.2 [0.8]), and planning ahead (4.3 [0.8]) to follow instructions for adjuvant therapy. Respondents were less concerned about normative beliefs (views of peers), as follows: other patients similar to them have had adjuvant therapy (3.7 [0.9]) and follow therapy exactly as prescribed (3.9 [0.9]). Patients generally showed strong intentions to follow instructions (4.3 [0.8]) and take medications or receive treatments as prescribed (4.7 [0.6]). Patients responded similarly to items of the underlying TPB constructs, except that more patients treated with intravenous therapy indicated, “I plan ahead to make it easier to follow instructions for adjuvant therapy,” than those treated with oral therapy (4.4 [0.7] versus 4.1 [1.0], P = 0.012).
The base model and the expanded model examining the TBP concepts showed acceptable fit. CFIs were 0.95 and RMSEAs were less than 0.08 (0.0604 and 0.0586, respectively). The base and expanded models had SRMRs of 0.0491 (Fig. 1a) and 0.0484 (Fig. 1b), respectively. All coefficients were positive and significant in both models. In the base model, behavioral, normative, and perceived control beliefs explained a substantial proportion of the variance in intention to adhere to adjuvant therapy (60.3%), and all were significantly associated with intention to adhere. Perceived control beliefs were more strongly associated with intention (standardized estimate = 0.47, P < 0.001) than behavioral and normative beliefs (standardized estimates = 0.30 and 0.24, respectively, P < 0.05 for both). Stronger intention to adhere was significantly associated with higher adherence (standardized estimate = 0.23, P < 0.05). In the expanded model, results between the theoretical constructs were consistent with the base model. Additionally, route of administration had a significant impact on adherence, with intravenous administration being associated with greater adherence than oral administration (standardized estimate = 0.26, P < 0.001).
Base model examining core TPB concepts; R-square = 0.603 for intention and 0.081 for adherence (a) and expanded model that incorporated route of drug administration; R-square = 0.580 for intention and 0.144 for adherence (b). Standardized path estimates shown. Errors were modeled for all observed indicators and the dependent latent variable (i.e., disturbance is modeled for intention). Covariances were also modeled among all exogenous variables (i.e., variables that only influence another parameter). Errors and covariances not shown. Covariates, including age, sex, white race, education (college graduate versus less than college graduate) were also included but not shown. TBP theory of planned behavior. *P < 0.05. **P < 0.01. ***P < 0.001
Discussion
This study conducted an in-depth evaluation of the use of adjuvant therapy among real-world patients with resected melanoma. Self-reported adherence to adjuvant therapy was high for patients with resected melanoma. These results differed from those reported in a systematic review of breast cancer survivors, in which adherence to adjuvant endocrine therapy was suboptimal (41–72%) [8]. There are multiple potential reasons for the lower adherence reported among breast cancer survivors, such as the overall drug profile differences between adjuvant therapy for breast cancer versus that for melanoma, the perceived risk–benefit profile, and in particular a much longer recommended adjuvant treatment course for breast cancer (more than 5 years versus up to 1 year for melanoma).
This study also showed that the route of administration was significantly associated with patients’ adherence to treatment. Patients treated with intravenous adjuvant therapy reported higher adherence than those treated with oral adjuvant therapy. This finding is similar to results in patients with metastatic colon cancer; for instance, claims data showed that adherence to chemotherapy was significantly higher with treatments administered intravenously than orally [19]. In the current study, this difference in adherence may be attributable to several factors. First, the oral combination adjuvant therapy comprises two capsules of dabrafenib taken twice a day in combination with one tablet of trametinib taken once a day 1 h before or 2 h after a meal. In addition, trametinib must be refrigerated in the original bottle. These complexities may make it challenging for some patients to adhere to the oral treatment schedule. A review of current literature and clinical experience identified greater regimen complexity as a major barrier to adherence of oral therapies for melanoma, especially in the adjuvant setting, due to the different dosing schedules and storage requirements of dabrafenib and trametinib [10]. These findings appear to align with our results in that only patients treated with oral therapy reported inconvenience as a barrier to adherence, despite the apparent ease of administration. Second, oral medications may require higher co-pays than intravenous therapies, since they are covered under prescription insurance plans instead of major medical plans [10, 20]. This is consistent with our results, which showed that patients treated with oral therapy indicated affordability as a common barrier to adherence, whereas those treated with intravenous therapy did not. Third, patients treated with intravenous therapy may interact with their healthcare providers more frequently as a result of treatment administration, which may enhance feelings of accountability to adhere. In contrast, for patients who are prescribed oral therapy, the responsibility and management of treatment shifts from the clinical team to the patient, which may affect adherence. Although more patients in this study treated with oral therapy anticipated not being able to follow future treatments as instructed, this difference was not statistically significant.
As this study did not evaluate clinical outcomes and their association with adherence rates, it is difficult to speculate whether the difference in adherence rates between intravenous and oral therapy (98.4% versus 91.2%, respectively) would influence clinical outcomes. On the other hand, results from indirect treatment comparisons suggest that intravenous adjuvant therapy with the PD-1 inhibitors nivolumab or pembrolizumab may be more effective than oral adjuvant therapy with the BRAF plus MEK inhibitor combination of dabrafenib plus trametinib, especially over the long term [21, 22]. Therefore, in the real-world setting, the small improvement in adherence with intravenous versus oral therapy may augment the apparent superior treatment effect with PD-1 inhibitors versus the BRAF plus MEK inhibitor.
To the best of our knowledge, this is the first study that utilized a social behavioral model, the TPB, to systematically evaluate underlying factors associated with adherence to adjuvant therapy in patients with resected melanoma. The proposed models had satisfactory fit indices, indicating that the TPB can be useful in understanding medication adherence in patients with resected melanoma. It is a valid theoretical framework for this context, as behavioral, normative, and perceived control beliefs explained a substantial proportion of intention to adhere to adjuvant therapy [15], and intention was significantly associated with actual adherence [16]. These results align with previous findings, which showed that knowledge, attitudes, beliefs, perceptions, and expectations of patients with cancer regarding the course of the disease and their capability to manage their illness and treatment regimen can affect adherence [23, 24].
We found that perceived control beliefs (a patient’s perceived capability to perform a behavior) had the strongest association with intention to adhere, followed by behavioral beliefs, and then normative beliefs, similar to previous findings [15, 16, 18]. Other studies have found behavioral beliefs or attitudes to be the strongest predictor of intention [13, 25]. In the adjuvant setting for breast cancer, self-efficacy, attained through more knowledge about taking the medication, has been associated with increased odds of self-reported adherence [9]. It is worth noting that the majority of patients in our study felt their general well-being was good or very good regardless of adjuvant treatment and that they had been involved in the decision-making process about whether or not to start adjuvant therapy. It is possible that the high adherence observed in this study is in part due to patients’ high level of involvement in the decisions related to their care and a positive attitude toward their health (feeling good about general well-being). When patients feel empowered in their ability to take control of their care, they have more intention to adhere to treatment, which could lead to a greater adherence. This may imply that, in clinical practice, communication that increases a patient’s sense of control can be an effective channel for improving adherence. Examples of such approaches have been incorporated in patient-tailored counseling at the initiation of adjuvant therapy to help patients overcome perceived barriers and establish treatment routines through goal setting and confidence-building [9].
Despite the strengths of this study, including the collection of patient-reported data to inform adjuvant therapy patterns and beliefs in patients with melanoma, there were several limitations. First, all measures were self-reported and may have been subject to recall biases. As a result of social desirability bias, for instance, adherence may have been overestimated by patients. Second, the adherence measures differed by route of administration: in patients treated with intravenous therapy, missed infusions were considered; whereas, in those treated with oral therapy, adherence was based on estimates of taking medication on time and as instructed. Third, results might not be generalizable to all patients with melanoma treated with adjuvant therapies in the USA. The sample may have been subject to selection bias: patients who were able and willing to participate could have differed from those who were not able to participate because of factors such as patient engagement and internet access. In particular, this group of patients may represent those who are highly engaged in advocacy for their care because of their affiliation with the Melanoma Research Foundation. In addition, this sample includes a limited representation of racial/ethnic minorities and was, on average, younger than other populations of patients with resected melanoma [4, 5, 26]. Assessing adherence in a patient population with a broader range of characteristics would provide greater insights as poorer clinical outcomes with melanoma have been associated with older age, certain racial/ethnic groups (e.g., African Americans), and lower socioeconomic status [27,28,29]. Finally, we found that while intention to adhere significantly contributed to adherence, this construct explained a limited proportion of the variation observed in adherence. This suggests that there are factors not currently captured in our study that warrant further research to fully appreciate adherence behavior in these patients.
Conclusion
Results from this study indicate that patients with resected melanoma are highly engaged in the decision to initiate systemic adjuvant therapy, with an overall high adherence rate to prescribed adjuvant treatment. Intravenous administration and enhanced patient perception of control are associated with better adherence. Future studies are warranted to fully evaluate factors associated with adherence to adjuvant therapy, as well as the impact that adherence may have on safety and long-term outcomes among patients with completely resected melanoma.
References
Ferlay J, Colombet M, Mathers C, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144:1941–53.
American Cancer Society. Cancer facts & figures 2021. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2021/cancer-facts-and-figures-2021.pdf. Accessed 09 February 2021.
Romano E, Scordo M, Dusza SW, Coit DG, Chapman PB. Site and timing of first relapse in stage III melanoma patients: implications for follow-up guidelines. J Clin Oncol. 2010;28:3042–7.
Eggermont AMM, Chiarion-Sileni V, Grob J-J, et al. Adjuvant ipilimumab versus placebo after complete resection of high-risk stage III melanoma (EORTC 18071): a randomised, double-blind, phase 3 trial. Lancet Oncol. 2015;16:522–30.
Eggermont AMM, Chiarion-Sileni V, Grob J-J, et al. Prolonged survival in stage III melanoma with ipilimumab adjuvant therapy. N Engl J Med. 2016;375:1845–55.
Gibney GT, Kudchadkar RR, DeConti RC, et al. Safety, correlative markers, and clinical results of adjuvant nivolumab in combination with vaccine in resected high-risk metastatic melanoma. Clin Cancer Res. 2015;21:712–20.
Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Melanoma: Cutaneous V.3.2022. © National Comprehensive Cancer Network, Inc. 2022. All rights reserved. Accessed 25 April 2022. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
Murphy CC, Bartholomew LK, Carpentier MY, Bluethmann SM, Vernon SW. Adherence to adjuvant hormonal therapy among breast cancer survivors in clinical practice: a systematic review. Breast Cancer Res Treat. 2012;134:459–78.
Moon Z, Moss-Morris R, Hunter MS, Carlisle S, Hughes LD. Barriers and facilitators of adjuvant hormone therapy adherence and persistence in women with breast cancer: a systematic review. Patient Pref Adherence. 2017;11:305–22.
Kottschade LA, Lehner RM. Promoting oral therapy adherence: consensus statements from the faculty of the melanoma nursing initiative on oral melanoma therapies. Clin J Oncol Nurs. 2017;21(4 suppl):87–96.
Eek D, Krohe M, Mazar I, et al. Patient-reported preferences for oral versus intravenous administration for the treatment of cancer: a review of the literature. Patient Pref Adherence. 2016;10:1609–21.
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Processes. 1991;50:179–211.
Manning M, Bettencourt BA. Depression and medication adherence among breast cancer survivors: bridging the gap with the theory of planned behaviour. Psychol Health. 2011;26:1173–87.
Lin C-Y, Updegraff JA, Pakpour AH. The relationship between the theory of planned behavior and medication adherence in patients with epilepsy. Epilepsy Behav. 2016;61:231–6.
Hurtado-de-Mendoza A, Carrera P, Parrott WG, Gómez-Trillos S, Perera RA, Sheppard VB. Applying the theory of planned behavior to examine adjuvant endocrine therapy adherence intentions. Psychooncology. 2019;28:187–94.
Moon Z, Moss-Morris R, Hunter MS, Hughes LD. More than just side-effects: the role of clinical and psychosocial factors in non-adherence to tamoxifen. Br J Health Psychol. 2017;22:998–1018.
Peh KQE, Kwan YH, Goh H, et al. An adaptable framework for factors contributing to medication adherence: results from a systematic review of 102 conceptual frameworks. J Gen Intern Med. 2021;36:2784–95.
Rich A, Brandes K, Mullan B, Hagger MS. Theory of planned behavior and adherence in chronic illness: a meta-analysis. J Behav Med. 2015;38:673–88.
Seal BS, Anderson S, Shermock KM. Factors associated with adherence rates for oral and intravenous anticancer therapy in commercially insured patients with metastatic colon cancer. J Manag Care Spec Pharm. 2016;22:227–35.
Schneider SM, Adams DB, Gosselin T. A tailored nurse coaching intervention for oral chemotherapy adherence. J Adv Pract Oncol. 2014;5:163–72.
Toor K, Middleton MR, Chan K, Amadi A, Moshyk A, Kotapati S. Comparative efficacy and safety of adjuvant nivolumab versus other treatments in adults with resected melanoma: a systematic literature review and network meta-analysis. BMC Cancer. 2021;21:3.
Lorenzi M, Arndorfer S, Aguiar-Ibañez R, Scherrer E, Liu FX, Krepler C. An indirect treatment comparison of the efficacy of pembrolizumab versus competing regimens for the adjuvant treatment of stage III melanoma. J Drug Assess. 2019;8:135–45.
Timmers L, Boons CCLM, Verbrugghe M, van den Bemt BJF, Van Hecke A, Hugtenburg JG. Supporting adherence to oral anticancer agents: clinical practice and clues to improve care provided by physicians, nurse practitioners, nurses and pharmacists. BMC Cancer. 2017;17:122.
Wouters H, Stiggelbout AM, Bouvy ML, et al. Endocrine therapy for breast cancer: assessing an array of women’s treatment experiences and perceptions, their perceived self-efficacy and nonadherence. Clin Breast Cancer. 2014;14:460-467.e2.
DeMaria AL, Sundstrom B, Faria AA, Moxley Saxon G, Ramos-Ortiz J. Using the theory of planned behavior and self-identity to explore women’s decision-making and intention to switch from combined oral contraceptive pill (COC) to long-acting reversible contraceptive (LARC). BMC Womens Health. 2019;19:82.
Weber J, Mandala M, Del Vecchio M, et al. Adjuvant nivolumab versus ipilimumab in resected stage III or IV melanoma. N Engl J Med. 2017;377:1824–35.
Ribero S, Stucci LS, Marra E, et al. Effect of age on melanoma risk, prognosis and treatment response. Acta Derm Venereol. 2018;98:624–9.
Lam M, Zhu JW, Hu A, Beecker J. Racial differences in the prognosis and survival of cutaneous melanoma from 1990 to 2020 in North America: a systematic review and meta-analysis. J Cutan Med Surg. 2022;26:181–8.
Abdel-Rahman O. Prognostic impact of socioeconomic status among patients with malignant melanoma of the skin: a population-based study. J Dermatolog Treat. 2020;31:571–5.
Acknowledgements
We wish to thank the contribution from all of the study participants. We would like to acknowledge Georgia Grace Edwards, an employee of the Analysis Group, for analyzing these data. We would also like to acknowledge Matthew Burke, who was an employee of Bristol Myers Squibb during the conduct of this study, for his contribution to this project.
Funding
This study was funded by Bristol Myers Squibb. The journal’s Rapid Service and Open Access Fees were provided by Bristol Myers Squibb.
Editorial Assistance
Editorial assistance was provided by Kakoli Parai, Mark Palangio, and Michele Salernitano of Ashfield MedComms, an Ashfield Health company, funded by Bristol Myers Squibb.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Cassie Beisel, Tayla Poretta, Heather Sipsma, Eleanore Fuqua, Anthony Salvatore, and Min Yang contributed to the conception and design of this study. Heather Sipsma, Eleanore Fuqua, and Min Yang contributed to acquisition of these data. Tayla Poretta, Heather Sipsma, Eleanore Fuqua, and Min Yang contributed to analysis of these data. Cassie Beisel, Tayla Poretta, Vanessa B. Sheppard, Alejandra Hurtado-de Mendoza, Brian Stwalley, Anthony Salvatore, and Min Yang contributed to interpretation of these data.
Disclosures
Cassie Beisel is an employee of the Melanoma Research Foundation, which received consulting fees from Bristol Myers Squibb. Tayla Poretta is an employee of Bristol Myers Squibb and also reports personal fees from Rutgers University outside the submitted work. Vanessa B. Sheppard received consulting fees from Bristol Myers Squibb. Alejandra Hurtado-de Mendoza has no conflicts of interest. Heather Sipsma, Eleanore Fuqua, and Min Yang. are employees of the Analysis Group, Inc., which received consulting fees from Bristol Myers Squibb. Brian Stwalley and Anthony Salvatore are employees of Bristol Myers Squibb.
Compliance with Ethics Guidelines
This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments and was granted an exemption from a full review by the New England Institutional Research Board. All survey participants consented to participation in the study prior to proceeding to completing the survey questions.
Data Availability
Bristol Myers Squibb’s policy on data sharing is available at https://www.bms.com/researchers-and-partners/independent-research/data-sharing-request-process.html.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Beisel, C., Poretta, T., Sheppard, V.B. et al. Adherence to Adjuvant Therapy in Patients with Resected Melanoma: An Application of the Theory of Planned Behavior. Adv Ther 39, 4061–4075 (2022). https://doi.org/10.1007/s12325-022-02221-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02221-2