Abstract
Introduction
Large-bore chest tubes are usually applied after thoracic surgery. Recently, small-bore tubes have been increasingly considered owing to the extensive use of video-assisted thoracoscopic surgery (VATS). This study assessed the differences in outcomes between large-bore and small-caliber drainage tubes in patients undergoing surgical stabilization of rib fractures (SSRF) with VATS.
Methods
Overall, 131 patients undergoing SSRF with VATS were prospectively enrolled, including 65 patients receiving 32-Fr chest tubes (group 1) and 66 patients receiving 14-Fr pigtail catheters (group 2) for postoperative drainage. The clinical characteristics and perioperative outcomes of the patients were compared.
Results
All patients underwent SSRF with VATS within 4 days after trauma. After the operation, the mean duration of chest tubes was longer than that of pigtail catheters, with statistical significance (5.08 ± 2.47 vs 3.11 ± 1.31, P = 0.001). Length of stay (LOS) was also longer in group 1 (10.38 ± 2.90 vs 8.18 ± 2.44, P = 0.001). After multivariate logistic regression, the only independent factors between the two groups were duration of postoperative drainage (adjusted odds ratio [AOR] 1.746; 95% confidence interval [CI] 0.171–10.583, P = 0.001) and hospital LOS (AOR 1.272; 95% CI 0.109–4.888, P = 0.027).
Conclusion
After reconstruction of the chest wall and lung parenchyma, small-caliber drainage catheters could be easily and safely applied to reduce hospital LOS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
After reconstruction of the chest wall and lung parenchyma through surgical stabilization of rib fractures (SSRF) and video-assisted thoracoscopic surgery (VATS), small-caliber drainage catheters could be easily and safely applied with little cost to shorten hospital stay. |
Pigtail catheters yielded superior outcomes to chest tubes in patients undergoing SSRF with VATS. |
With negative low-pressure suction, small-bore pigtail catheters exhibited drainage performance similar to that of large-bore chest tubes. |
Introduction
Blunt chest trauma frequently causes injuries such as hemothorax, pneumothorax, and rib fractures [1]. Surgical fixation for rib fractures is an effective and now routine procedure for patients with unstable chest wall injuries [2, 3]. Following surgery, suitable drainage for eliminating any residual hemothorax or pneumothorax is required. Adequate drainage combined with low-pressure suction is critical to maintaining full expansion of the lung parenchyma [4, 5].
Chest tubes are the most common tools used to facilitate drainage after thoracic surgery [6, 7]. Traditionally, large-bore chest tubes such as 28-French (Fr) and 32-Fr tubes, with outer diameters typically more than 1.0 cm (Fig. 1a), have been considered effective owing to their large size, which prevents obstruction of the lumen. They are also easy to insert and cost-effective. However, large-caliber tubes entail large wounds, which can cause considerable discomfort [6, 8]. Numerous complications often occur with more chest tissue damage, such as malposition, wound infection, and increased risk of empyema [6, 9].
Recent advances in catheter design have allowed the use of small-caliber drainage catheters (pigtail catheter, COOK, Wayne Pneumothorax Cather Set, USA); Fig. 1b) for chest drainage [10, 11]. Several studies have indicated that pigtail drainage could be successfully applied in the treatment of pneumothorax [12,13,14], but only a few studies have focused on its use in hemothorax [10, 11]. The use of pigtail catheters for drainage in patients receiving video-assisted thoracoscopic surgery (VATS) has yet to be reported. In this study, we applied pigtail catheters for drainage in patients receiving surgical stabilization of rib fractures (SSRF) with VATS. We hypothesized that pigtail catheters would perform similar drainage functions as chest tubes, and furthermore, because of their smaller caliber, pigtail catheters would be better tolerated by patients than larger chest tubes.
Methods
Patient Population
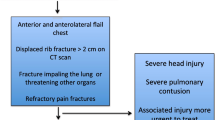
This prospective observational study was conducted at Kaohsiung Veterans General Hospital, a level 1 trauma center in southern Taiwan that receives approximately 15,000 emergency trauma visits per year. Patients aged 18 years and older were enrolled from March 2018 to May 2021; the inclusion criterion was blunt chest trauma as the major injury site. No patient had bleeding tendencies or coagulation disorders before the operation; none had anticoagulant medication history. All patients had at least three bicortical rib fractures combined with hemothorax, pneumothorax, or lung contusions. The abbreviated injury score (AIS) of the chest ranged between 3 and 4. Some patients underwent tube thoracostomy with 32-Fr chest tubes during the first evaluation at the emergency department (ED). The decision to insert a chest tube was based on the emergency physician’s subjective judgment. Secondary evaluation to identify associated injuries was also performed at the ED. Patients were excluded if their AISs for associated sites were higher than 2. Patients were also excluded (1) if they had acute respiratory failure within 24 h after trauma, requiring positive pressure ventilator support that may prolong admission; (2) if they had hemodynamic instability indicating emergent thoracotomy; and (3) if they had severe medical disease or cancer of any stage. The algorithm of patient selection is illustrated in Fig. 2.
This study was approved by the Institutional Review Board of Kaohsiung Veterans General Hospital (reference number VGHKS17-CT12-13) and was conducted in accordance with the Declaration of Helsinki, Ethical Guidelines for Medical and Health Research Involving Human Subjects, and Taiwan’s laws and regulations. All patients provided informed consent by completing an online consent form before they could participate in the study.
Data Collection
Basic demographic data of all patients were prospectively collected, including age, gender, number of fractured ribs, pulmonary contusion score, and trauma mechanism. The AIS of each associated injury was also collected, and injury severity scores (ISSs) were calculated. The duration of chest tube use, rates of infection, total dose of analgesics, and hospital length of stay (LOS) were also recorded. During follow-up periods, any evidence of angle blunting detected on chest X-rays was also collected. This radiologic finding was regarded as a mild fibrothorax (Fig. 3).
Video-Assisted Thoracoscopic Surgery and Surgical Fixation of Fractured Ribs
After detailed evaluations, patients were admitted to the intensive care unit. Surgical fixation was indicated for total displacement of fractured ribs. In our hospital, VATS is performed simultaneously with SSRF [15, 16], and both procedures are arranged within days after trauma. General anesthesia with single-lung ventilation is also required during the operation. For SSRF, titanium plates with locking screws (Rib Locking Plate, Aplus Biotechnology Corporation Limited, Taiwan) were applied at the outer surface of fractured ribs. Surgical incisions were designed according to fracture sites that were localized through VATS. These fractured sites were approached using the chest wall muscle-sparing method of Hasenboehler [17]. After SSRF, evacuation of retained hemothorax and repair of lung lacerations were performed via VATS. Most patients did not need decortication or lavage because we performed the fixation within 5 days after trauma.
Postoperative Drainage
The chest tube inserted at ED was removed during operation. All patients who underwent VATS with SSRF received postoperative chest drainage. Before January 2020, patients received 32-Fr plastics chest tubes with multiple drainage fenestrations (Fig. 1) after SSRF; we designated this cohort as group 1. After January 2020, patients received 14-Fr pigtail drainage; we designated this cohort as group 2. Both types of drainage were connected to low-pressure suction (− 15 cmH2O) to reduce residual pleural effusions. After the operation, endotracheal tubes were immediately removed when patients regained consciousness, and routine follow-up chest X-rays were arranged. The criteria for drainage tube removal were absence of air leaks, fluid drainage of less than 100 mL per day, and completely expanded lung. Residual pleural effusions were estimated using chest X-rays and sonography. Once the residual pleural collection was greater than 300 mL, this postoperative complication was managed with secondary VATS.
After discharge, patients were regularly followed up at the outpatient clinic. Chest X-rays were regularly obtained. The follow-up period lasted at least 6 months after trauma.
Statistical Analysis
We used a descriptive analysis for all variables to determine frequencies and averages in each group. Continuous variables are presented as means (± standard deviation) and categorical variables as frequencies. Chi-square and Fisher’s exact tests were used in this study to assess associations between categorical variables. Analysis of variance was used to analyze variation in continuous variables. Multivariate logistic regression was used to assess the associated variables of postoperative drainage. Logistic regression analysis with a running entry model was applied to control confounders. Subsequently, all independent variables were entered into the multivariate logistic regression analysis to detect the independent variables of postoperative drainage methods. The Hosmer–Lemeshow test was used to assess goodness of fit for logistic regression models. Significant associations between the independent and dependent variables were assessed using 95% confidence interval (CIs) and adjusted odds ratios (AORs). P < 0.05 was considered as statistically significant. Data were analyzed using SPSS 20.0. This study had a 99.7% power to detect a significant difference in hospital LOS between patients and controls (two-sided equality, two-sample) by using a sample size of 131 patients (α = 5%; sampling ratio = 65/66).
Results
A total of 131 patients who underwent SSRF combined with VATS were included in this study. Of these, 65 patients (group 1) received 32-Fr chest tubes, and 66 patients (group 2) received 14-Fr pigtail catheters for postoperative drainage. The basic demographic characteristics of the two groups are presented in Table 1. The mean age of the patients was 56 years. The sex distribution of both groups was similar. The mean of fractured ribs, percentage of flail chest, and lung contusion scores were also similar between both groups. Likewise, chest AISs and ISSs did not differ significantly between the two groups. However, the rate of tube thoracostomy for hemothorax and pneumothorax at the ED was higher in group 1 (38.5% vs 21.2%, P = 0.031). Overall, both groups were satisfactorily matched and could be compared on the basis of their similar characteristics.
The clinical outcomes of both groups are outlined in Table 2. All patients underwent SSRF with VATS within 4 days after trauma. Most patients had their drainage tubes removed within 5 days after SSRF. After the operation, the mean duration of chest tubes in group 1 was slightly but significantly longer than that of pigtail catheters in group 2 (5.08 ± 2.47 vs 3.11 ± 1.31, P = 0.001). Hospital LOS was also longer in group 1 (10.38 ± 2.90 vs 8.18 ± 2.44, P = 0.001). Doses of analgesics for pain management in both groups were also equal (55.09 ± 15.44 vs 57.06 ± 19.37, P = 0.522). Discomfort at the drain tube site was slightly higher in group 1 (1.28 ± 0.52 vs 1.08 ± 0.27, P = 0.006).
Binary logistic regression was used to test the associated factors; the results are displayed in Table 3. After multivariate logistic regression, the only independent factors between the two groups were duration of postoperative drainage (AOR 1.746; 95% CI 0.171–10.583, P = 0.001) and hospital LOS (AOR 1.272; 95% CI 0.109–4.888, P = 0.027). These results indicate a significant association between the type of drain used after SSRF and LOS. Calibration of the final model was assessed using the Hosmer–Lemeshow goodness of fit test. A P value of 0.206 (χ2 = 10.928) suggested that the model was accurate.
Five patients (four in group 1 and one in group 2) had residual pleural collection greater than 300 mL, which required secondary VATS. All cases of secondary VATS were performed smoothly without complications. Despite a higher percentage of secondary VATS in group 1, no statistical significance was observed (6.2% vs 1.5%, P = 0.166). Drains were removed 2 to 3 days postoperatively.
Patients were regularly followed at the outpatient clinic for at least 6 months. Seventeen patients had mild fibrothorax, with angle blunting visible on chest X-rays, during the follow-up period. Group 1 had a higher percentage of mild fibrothorax cases after SSRF, with statistical significance (20% vs 6.1%, P = 0.018). No case of mild fibrothorax influenced the patient’s activities of daily living.
Discussion
Residual pleural collection can compress lung parenchyma, thereby precipitating clinical infection [9, 18]. Therefore, adequate drainage is critical to preventing fluid accumulation after thoracic surgical procedures. Tube thoracostomy combined with closed low-pressure suction is necessary during chest surgery, especially for chest trauma, to prevent the collapse of lung parenchyma [5]. Traditionally, large-bore chest tubes have been used after chest surgery. Because of their larger diameter, chest tubes have been thought to provide better drainage than pigtail catheters. However, large-bore chest tubes may cause more pain or discomfort because of larger wounds. In this study, we observed that pigtail catheters produced better outcomes than chest tubes in patients undergoing SSRF with VATS.
Recently, 14-Fr pigtail catheters have been widely used for spontaneous pneumothorax [12, 13]. The pigtail could also be used in chest fluid collection, but its use for the drainage of trauma-derived hemothorax remains controversial [8, 11]. In this study, we applied pigtail drainage after SSRF. We observed that with negative low-pressure suction, small-bore pigtail catheters could provide comparable drainage ability as large-bore chest tubes.
Blunt chest trauma typically induces multiple rib fractures accompanied by hemothorax and pneumothorax. In line with the treatment methods employed in our hospital, complete management of both the chest wall and lung parenchyma is vital to the management of blunt chest trauma [19]. In our hospital, nearly all fractured ribs are fixed, hemothorax is evacuated, and lung lacerations are repaired using VATS. SSRF can reduce oozing from the bone marrow, and lung repair can reduce micro-air leakage from injured lung parenchyma. Together, these procedures could reduce residual hemothorax and pneumothorax. Because residual pleural collection decreases after surgery, small-caliber drainage could reduce the pain and discomfort experienced from the tube wound.
In this study, the duration of postoperative drainage was much shorter in the pigtail group; the main reason might have been the numerous side holes that pigtail catheters have, despite their small caliber. In our previous study, we observed that traumatic hemothorax or pneumothorax could be drained successfully using 14-Fr pigtail catheters instead of large-bore chest tubes [20]. Pigtail drain tubes contain more than 20 side holes, enabling a better capillary effect than that of large-bore chest tubes. Combined with negative pressure suction, pigtail catheters could provide excellent drainage [10]. We observed that the postoperative duration was longer with chest tubes than with pigtail catheters. As a result, the total LOS comprising the entire period from admission to discharge was also longer.
Residual pleural collection may induce lung collapse which may cause pneumonia or empyema in the short term after trauma or surgery. In the long term, unresolved pleural collection may evolve into fibrothorax [21]. Fibrothorax can reduce not only the elasticity of the lungs but also chest wall expansion capacity. These chronic complications can reduce lung function, which may cause difficulty in breathing. Activities of daily living may also be affected. In this study, no patient had severe fibrothorax after a follow-up of 6 months. However, some patients had mild fibrothorax that appeared as lateral costophrenic angle blunting on chest X-rays during the follow-up period. Because pigtail catheters offer excellent drainage and less irritation owing to their smaller caliber, inflammation is reduced. Group 2 had a much lower percentage of mild fibrothorax than did group 1.
One of the main goals after SSRF is pain reduction. In our previous study, SSRF dramatically reduced pain [15, 16], and the analgesic dose was significantly reduced compared with patients who did not undergo SSRF. In this study, because all patients underwent SSRF, the analgesic dose was similar between both groups. The only difference was pain at the drain tube site. Discomfort at the drain wound site was clearly higher in the chest tube group. This means that despite SSRF reducing most pain in all patients, tube size might still influence pain. Pigtail catheters are much smaller than chest tubes; therefore, they should cause less discomfort.
This study has limitations. First, the number of cases was small: only 131 patients were enrolled. Multiple rib fractures are frequently diagnosed, but less than one-third of patients require SRF. Nevertheless, the demographic characteristics of the two groups in this study were not significantly different. This study, however, had a 99.7% power to detect a significant difference in hospital LOS between the two groups. The only difference was pleural drainage before SSRF. Although group 1 had a higher rate of tube thoracostomies at the ED, binary logistic regression did not reveal any statistical difference (AOR 2.323; 95% CI 0.530–2.530, P = 0.112). This indicates that the choice of tube thoracostomy at the ED was not a confounding factor between the two groups. Second, the study protocol of the pigtail group was prospective, but patient selection in the chest tube group was based on retrospective data collected from the trauma registry database of our hospital. However, the variations between both groups did not present significant confounding or bias. All surgical procedures were performed by the same team, and to avoid surgical confounding bias, the same surgeons made all decisions regarding SSRF. Third, pain or discomfort was subjectively reported by patients. To prevent subjective bias due to single-blind data collection, we ensured nursing staff rather than trauma surgeons recorded the pain scores. In future studies, we intend to focus on hemodynamically stable patients with traumatic hemopneumothorax. Direct VATS with SSRF without initial chest tube insertion could become the new strategy for managing chest wall and lung parenchyma injuries.
Conclusion
After reconstruction of chest wall and lung parenchyma through SSRF and VATS, small-caliber drainage catheters could be easily and safely applied with little cost to shorten lengths of hospital stay.
References
Dogrul BN, Kiliccalan I, Asci ES, Peker SC. Blunt trauma related chest wall and pulmonary injuries: an overview. Chinese J Traumatol = Zhonghua chuang shang za zhi. 2020;23:125–38.
Zhang D, Zhou X, Yang Y, et al. Minimally invasive surgery rib fracture fixation based on location and anatomical landmarks. Eur J Trauma Emerg Surg. 2021. https://doi.org/10.1007/s00068-021-01676-2.
Majeed FA, Zafar U, Imtiaz T, Ali Shah SZ, Ali A, Mehmood U. Rib fixation versus conservative management of rib fractures in trauma patients. J Ayub Med Coll Abbottabad. 2018;30:576–84.
Chou Y-P, Lin H-L, Wu T-C. Video-assisted thoracoscopic surgery for retained hemothorax in blunt chest trauma. Curr Opin Pulm Med. 2015;21:393–8.
Feenstra TM, Dickhoff C, Deunk J. Systematic review and meta-analysis of tube thoracostomy following traumatic chest injury; suction versus water seal. Eur J Trauma Emerg Surg. 2018;44:819–27.
Kwiatt M, Tarbox A, Seamon MJ, et al. Thoracostomy tubes: a comprehensive review of complications and related topics. Int J Crit Illn Inj Sci. 2014;4:143–55.
Porcel JM. Chest tube drainage of the pleural space: a concise review for pulmonologists. Tuberc Respir Dis (Seoul). 2018;81:106–15.
Kulvatunyou N, Bauman ZM, Zein Edine SB, et al. The small (14 Fr) percutaneous catheter (P-CAT) versus large (28–32 Fr) open chest tube for traumatic hemothorax: a multicenter randomized clinical trial. J Trauma Acute Care Surg. 2021;91:809–13.
Karmy-Jones R, Holevar M, Sullivan RJ, Fleisig A, Jurkovich GJ. Residual hemothorax after chest tube placement correlates with increased risk of empyema following traumatic injury. Can Respir J. 2008;15:255–8.
Orlando A, Cordero J, Carrick MM, et al. Comparing complications of small-bore chest tubes to large-bore chest tubes in the setting of delayed hemothorax: a retrospective multicenter cohort study. Scand J Trauma Resusc Emerg Med. 2020;28:56.
Bauman ZM, Kulvatunyou N, Joseph B, et al. Randomized clinical trial of 14-French (14F) pigtail catheters versus 28–32F chest tubes in the management of patients with traumatic hemothorax and hemopneumothorax. World J Surg. 2021;45:880–6.
Fang M, Liu G, Luo G, Wu T. Does pigtail catheters relieve pneumothorax? A PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore). 2018;97:e13255-e.
Riber SS, Riber LP, Olesen WH, Licht PB. The influence of chest tube size and position in primary spontaneous pneumothorax. J Thorac Dis. 2017;9:327–32.
Rasihashemi SZ, Ramouz A, Amini H. Comparison of the therapeutic effects of a pigtail catheter and chest tube in the treatment of spontaneous pneumothorax: a randomized clinical trial study. Turk Thorac J. 2021;22:459–65.
Lin HL, Tarng YW, Wu TH, Huang FD, Huang WY, Chou YP. The advantages of adding rib fixations during VATS for retained hemothorax in serious blunt chest trauma—a prospective cohort study. Int J Surg. 2019;65:13–8.
Wu TH, Lin HL, Chou YP, Huang FD, Huang WY, Tarng YW. Facilitating ventilator weaning through rib fixation combined with video-assisted thoracoscopic surgery in severe blunt chest injury with acute respiratory failure. Critical Care. 2020;24:49.
Hasenboehler EA, Bernard AC, Bottiggi AJ, et al. Treatment of traumatic flail chest with muscular sparing open reduction and internal fixation: description of a surgical technique. J Trauma. 2011;71:494–501.
Zeiler J, Idell S, Norwood S, Cook A. Hemothorax: a review of the literature. Clin Pulm Med. 2020;27:1–12.
Chou YP, Kuo LC, Soo KM, et al. The role of repairing lung lacerations during video-assisted thoracoscopic surgery evacuations for retained haemothorax caused by blunt chest trauma. Eur J Cardio-thorac Surg. 2014;46:107–11.
Lin HL, Chou YP. 14-French pigtail catheters for traumatic hemothorax/hemopneumothorax: size does not matter. World J Surg. 2018;42:2686.
Davies HE, Davies RJO, Davies CWH. Management of pleural infection in adults: British Thoracic Society pleural disease guideline 2010. Thorax. 2010;65:ii41–53.
Acknowledgements
The authors thank the patients, their families, and all investigators involved in the study.
Funding
No funding was received for this study. The journal’s Rapid Service and Open Access fees were paid by Jung-Fang Chuang.
Editorial Assistance
Rasheed O. and Ian Fritz from Wallace Academic Editing assisted with the re-editing of the article and was funded by Jung-Fang Chuang.
Author Contributions
Yuan-Yuarn Liu, Fong-Dee Huang, Yi-Pin Chou and Chieh-Jen Wu assisted with data analysis and interpretation. Yi-Pin Chou planned and conducted the study. Yih-Wen Tarng and Jung-Fang Chuang drafted the manuscript. All authors participated in the preparation of the report and approved the final version.
Disclosures
Chieh-Jen Wu, Yuan-Yuarn Liu, Yih-Wen Tarng, Fong-Dee Huang, Yi-Pin Chou and Jung-Fang Chuang have declared that no conflict of interest or financial ties to disclose.
Compliance with Ethical Guidelines
This study was approved by the Institutional Review Board of Kaohsiung Veterans General Hospital (reference number VGHKS17-CT12-13) and was conducted in accordance with the Declaration of Helsinki, Ethical Guidelines for Medical and Health Research Involving Human Subjects, and Taiwan’s laws and regulations. All patients provided informed consent by completing an online consent form before they could participate in the study.
Data Availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wu, CJ., Liu, YY., Tarng, YW. et al. It is Time to Replace Large Drains with Small Ones After Fixation of Rib Fractures: A Prospective Observational Study. Adv Ther 39, 3668–3677 (2022). https://doi.org/10.1007/s12325-022-02182-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02182-6